Tuberculosis Epidemiologic Studies Consortium (TBESC)
Study 1: evaluating tests for tb infection, study 2: the latent tb infection care cascade, study 3: closing the gaps in the tb care cascade.
Study Sites
- California Department of Public Health
- Denver Health and Hospital Authority, Colorado
- Duke University, North Carolina and Tennessee
- Emory University, Georgia
- Hawaii Department of Health
- Public Health-Seattle and King County, Washington
- Maricopa County Department of Public Health, Arizona
- Maryland Department of Health and Mental Hygiene
- University of Florida
- University of North Texas Health Science Center
This first TBESC-II study was a head-to-head comparison of the three tests for TB infection in populations at high risk of latent TB infection and/or progression to TB disease.
Sub studies
- Repeatability and reproducibility of two interferon-gamma release assay (IGRA) blood tests– the QuantiFERON ® -TB Gold In-Tube (QFT-GIT), and T-SPOT ® . TB test (T-SPOT)
- Feasibility and cost of testing for prediabetes and diabetes in high-risk persons tested for TB infection
- Cost-effectiveness of TB infection testing in high-risk populations
The second study focused on describing and quantifying the steps in the TB prevention cascade of care within health department clinics. This included better understanding the proportions of patients with latent TB infection who are identified, offered treatment, accept treatment, and complete treatment.
- Developed algorithms to estimate latent TB infection prevalence at any county or state level.
- Developed tools for local TB programs to identify local clinicians who treat underserved populations at high risk, so they can partner with these groups to increase latent TB infection treatment.
- Used insurance billing codes to estimate the extent and magnitude of latent TB infection testing and treatment in commercial and community health sectors.
The third study focused on identifying barriers and facilitators to latent TB infection diagnosis and treatment at community health clinics (CHCs). Researchers collected and analyzed quantitative and qualitative data that can be used to inform development of interventions to improve targeted TB testing and latent TB infection treatment at CHCs.
To receive email updates about this page, enter your email address:

Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Tuberculosis articles from across Nature Portfolio
Tuberculosis (TB) is an infectious disease caused by strains of bacteria known as mycobacteria. The disease most commonly affects the lungs and can be fatal if not treated. However, most infected individuals show no disease symptoms. One third of the worlds population is thought to have been infected with TB.
Latest Research and Reviews

Age and sex influence antibody profiles associated with tuberculosis progression
Analysis of Mycobacterium tuberculosis -specific antibody responses in previously exposed South African cohorts reveals that profile features associated with progression to active tuberculosis are affected by age and sex.
- Leela R. L. Davies
- Chuangqi Wang
- Sarah M. Fortune
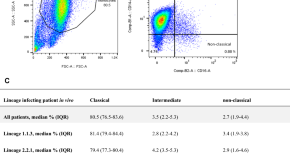
Bacterial diversity dominates variable macrophage responses of tuberculosis patients in Tanzania
- Hellen Hiza
- Michaela Zwyer
- Damien Portevin
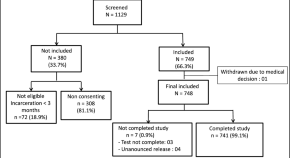
Prevalence of pulmonary tuberculosis and HIV infections and risk factors associated to tuberculosis in detained persons in Antananarivo, Madagascar
- Fanjasoa Rakotomanana
- Anou Dreyfus
- Rindra V. Randremanana
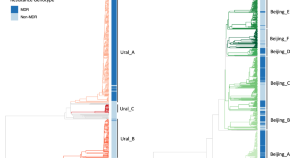
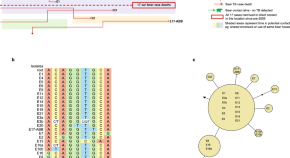
The recent rapid expansion of multidrug resistant Ural lineage Mycobacterium tuberculosis in Moldova
Chitwood et al. report on the rapid expansion of a Ural-lineage multidrug resistant strain of Mycobacterium tuberculosis in Moldova. This strain has an estimated reproduction number more than two times greater than otherwise similar drug susceptible strains.
- Melanie H. Chitwood
- Caroline Colijn
- Benjamin Sobkowiak
Genomic insights into anthropozoonotic tuberculosis in captive sun bears ( Helarctos malayanus ) and an Asiatic black bear ( Ursus thibetanus ) in Cambodia
- Kirsty Officer
- Timothy M. Walker
- Bethany Jackson

TOLLIP inhibits lipid accumulation and the integrated stress response in alveolar macrophages to control Mycobacterium tuberculosis infection
Toll-interacting protein (TOLLIP) prevents inflammation and lipid accumulation in alveolar macrophages to limit integrated stress response activation, macrophage necrosis and promote control of Mycobacterium tuberculosis .
- Sambasivan Venkatasubramanian
- Courtney R. Plumlee
- Javeed A. Shah
News and Comment
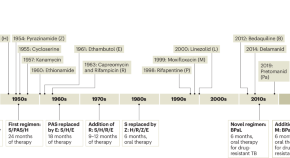
Restocking the tuberculosis drug arsenal
After many lean years, important progress has been made in updating the anti-tuberculosis drug armamentarium; a new drug that targets bacterial protein synthesis is one of several that could help transform the treatment of this neglected and deadly disease.
- Eric L. Nuermberger
- Richard E. Chaisson

Digital intervention improves tuberculosis treatment outcomes
An intervention that incorporates electronic pill boxes and remote adherence monitoring improved treatment success in patients with tuberculosis in Tibet — making this a promising strategy for low-resource settings.
- Karen O’Leary

A spotlight on the tuberculosis epidemic in South Africa
Tuberculosis is the leading cause of death from a single infectious agent, with over 25% of these occurring in the African region. Multi-drug resistant strains which do not respond to first-line antibiotics continue to emerge, putting at risk numerous public health strategies which aim to reduce incidence and mortality. Here, we speak with Professor Valerie Mizrahi, world-leading researcher and former director of the Institute of Infectious Disease and Molecular Medicine at the University of Cape Town, regarding the tuberculosis burden in South Africa. We discuss the challenges faced by researchers, the lessons that need to be learnt and current innovations to better understand the overall response required to accelerate progress.
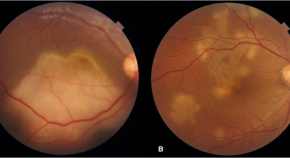
Presumed ocular tuberculosis – need for caution before considering anti-tubercular therapy
- Rohan Chawla
- Urvashi B. Singh
- Pradeep Venkatesh
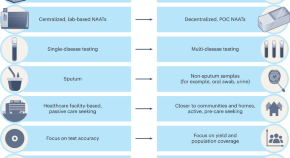
Transforming tuberculosis diagnosis
Diagnosis is the weakest aspect of tuberculosis (TB) care and control. We describe seven critical transitions that can close the massive TB diagnostic gap and enable TB programmes worldwide to recover from the pandemic setbacks.
- Madhukar Pai
- Puneet K. Dewan
- Soumya Swaminathan

B cells and T follicular helper-like cells within lung granulomas are required for TB control
We show a crucial protective function for T follicular helper (T FH )-like cells localized within granuloma-associated lymphoid tissue for Mycobacterium tuberculosis control in mouse models of tuberculosis. Antigen-specific B cells contribute to this strategic localization and the maturation of cytokine-producing T FH -like cells.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Correspondence
- Open access
- Published: 25 August 2016
Investments in tuberculosis research – what are the gaps?
- Mishal S. Khan 1 , 2 ,
- Helen Fletcher 1 ,
- London School of Hygiene and Tropical Medicine TB Centre Steering Committee &
- Richard Coker 1 , 3
BMC Medicine volume 14 , Article number: 123 ( 2016 ) Cite this article
5093 Accesses
12 Citations
21 Altmetric
Metrics details
Through decades of research, numerous studies have generated robust evidence about effective interventions for tuberculosis control. Yet, the global annual decline in incidence of approximately 1 % is evidence that current approaches and investment strategies are not sufficient. In this article, we assess recent tuberculosis research funding and discuss two critical gaps in funding and in scientific evidence from topics that have been left off the research priority agenda.
We first examine research and development funding goals in the 2011–2015 Global Plan to Stop Tuberculosis and analyze disbursements to different research areas by funders worldwide in 2014. We then summarize, through a compilation of published literature and consultation with 35 researchers across multiple disciplines in the London School of Hygiene and Tropical Medicine TB Centre, priorities identified by the tuberculosis research community. Finally, we compare researchers’ priority areas to the global funding agendas and activities.
Our analysis shows that, among the five key research areas defined in the 2011–2015 Global Plan - namely drugs, basic science, vaccines, diagnostics and operational research - drug discovery and basic science on Mycobacterium tuberculosis accounted for 60 % of the $2 billion annual funding target. None of the research areas received the recommended level of funding. Operational research, which had the lowest target, received 66 % of its target funding, whereas new diagnostics received only 19 %. Although many of the priority research questions identified by researchers fell within the Global Plan categories, our analysis highlights important areas that are not explicitly mentioned in the current plan. These priority research areas included improved understanding of tuberculosis transmission dynamics, the role of social protection and social determinants, and health systems and policy research.
While research priorities are increasingly important in light of the limited funding for tuberculosis, there is a risk that we neglect important research areas and encourage the formation of research silos. To ensure that funding priorities, researchers’ agendas and national tuberculosis control policies are better coordinated, there should be more, and wider, dialogue between stakeholders in high tuberculosis burden countries, researchers, international policymakers and funders.
The ancient scourge, tuberculosis, was the subject of the world’s first randomized controlled trial reported in 1949 [ 1 ], and since then numerous studies have generated robust evidence about effective interventions for tuberculosis control [ 2 ]. Although highly effective treatment regimens have been around for many decades [ 3 ], in 2014, tuberculosis killed 1.5 million people, surpassing HIV to become the leading cause of death from an infectious disease globally [ 4 ]. Tuberculosis evades control efforts for numerous reasons, including the lack of timely access to quality diagnostic and treatment services for vulnerable populations, which has contributed to the spread of drug-resistant tuberculosis. At the current rate of decline in incidence – just over 1 % per annum – it will take more than 150 years to meet the World Health Organization (WHO) targets of reducing tuberculosis deaths by 95 % and incidence by 90 % compared to rates in 2015 [ 5 ].
Recognizing the need for major improvements in our progress on tuberculosis control, the Stop TB Partnership’s Global Plan to End TB 2016–2020 calls for a paradigm shift [ 5 ]. While an acknowledgement of the need for a change in approach is promising, the tuberculosis control community has been criticized for failing to act effectively on the basis of existing knowledge and for constantly looking for ‘new’ solutions. Through his analysis of responses to tuberculosis in the twentieth century, historian Christian McMillan highlights a pattern of ‘repetition and rediscovery’ among researchers and policymakers, owing to a tendency to ignore lessons that have been learnt [ 6 ], resulting in a squandering of resources on repeatedly addressing already answered research questions. This view is echoed in a review of numerous studies carried out by the British Medical Research Council’s tuberculosis units between 1946 and 1986, which made the striking assertion: “[by the late 1980s] all of the measures necessary for successful programmes for the control of tuberculosis had been delineated ” [ 3 ]. On seeing the renewed calls for increased funding, some researchers have questioned whether we can justify being stewards of substantial funding for global health “ if we cannot manage a disease as well known as tuberculosis ” [ 7 ]. While the barriers to managing tuberculosis are numerous, including its association with poverty and the generation of drug resistance owing to inadequacies in health systems, these challenges are well defined; the balance between generating new knowledge and identifying strategies to implement proven solutions is thus being questioned.
In order to reflect upon, and learn from, our recent research activities and priorities, we look at the past 5 years of tuberculosis research funding and discuss two critical gaps in funding and in knowledge owing to essential topics being left off the research priority agenda.
We first extracted data on the funding goals for key research areas in the 2011–2015 Global Plan to Stop TB (Global Plan). The total annual funding goal for 2014, in US dollars, was identified in the report for individual research areas according to the classification used by the authors (drugs, basic science, vaccines, diagnostics, operational research). Data on the amount of funding actually allocated by global funding bodies in 2014 was extracted from the 2015 Treatment Action Group report [ 2 ], classified into the same five research areas as used by the Global Plan. Using these data, we expressed the allocated funding amount for each research area as a percentage of the Global Plan funding goal to assess how much of the funding goal was achieved for each research area. We then followed a two-step process to qualitatively compile priority topics identified by tuberculosis researchers. In the first step, we obtained the full text of articles on tuberculosis research priorities published by numerous groups between 2006 and 2010 [ 8 – 13 ]; we ensured that articles covered a wide range of possible research areas within tuberculosis, including childhood tuberculosis, drug resistance, diagnostics, vaccines and HIV, as well as papers looking more broadly across the whole spectrum of tuberculosis control. We extracted, from text and tables in these articles, research topics that the authors identified as being important. We classified research topics into the same five research areas used in the Global Plan, or into ‘others’ if they did not fit into any of the five research areas. In the second step, we updated the list of researchers’ priority topics compiled based on the literature, with additional priority research questions identified through an in-person consultation (short, structured, one-to-one interviews conducted in November 2015) with 35 researchers across multiple disciplines in the London School of Hygiene and Tropical Medicine (LSHTM) TB Centre [ 14 ]. The interviews were conducted at the annual TB Centre meeting under the supervision of a PhD student at LSHTM, and were recorded with respondents’ permission. Respondents were asked to identify their top research priorities for tuberculosis control. One of the authors (MSK) transcribed the interviews verbatim, and classified priority research topics identified by researchers into one of the five Global Plan research areas or ‘others’. Duplication between priority research topics emerging from the literature and from analysis of interviews was removed, and those classified under ‘others’ were grouped based on recurring themes or topics. Finally, we combined the quantitative and qualitative data into a single table (Table 1 ) to compare researchers’ priority topics with the global funding agendas and activities, highlighting key gaps. The priority research topics that did not fit into one of the five Global Plan research areas (identified from analyzing common themes among topics classified as ‘other’ in the qualitative analysis) were summarized into a separate table (Table 2 ).
Funding needs outlined in the Global Plan
The Global Plan to Stop TB 2006–2015 was launched in Davos, Switzerland, at the World Economic Forum in 2006 [ 15 ]. At $56 billion, the Stop TB Partnership’s forecasted total cost represented a three-fold increase in annual investment in tuberculosis control compared with the first Global Plan for 2001–2005 [ 16 ]. An update was provided for the 2011–2015 period in order to set out a clearer plan for reaching the Millennium Development Goals and Stop TB Partnership’s 2015 targets of halving tuberculosis prevalence and deaths compared with 1990 levels [ 16 ].
The research and development (R&D) component of the 2011–2015 Global Plan called for approximately $2 billion in annual funding to “ revolutionize the prevention, diagnosis and treatment of TB as the foundation for elimination of the disease ” [ 16 ]. Drug discovery and basic science were identified as the areas requiring the majority of investment (Table 1 ). With a target of $1.16 billion for 2014, these two areas accounted for 60 % of the recommended R&D funding. Basic science, which covers fundamental research about Mycobacterium tuberculosis and related organisms, was included as a separate research area in the updated plan, reflecting the fact that it underpins the development of all new technologies. The recommended level of R&D funding for basic science was set at $420 million per year. Similarly, operational research was included as a distinct research area in recognition of its essential role in ensuring uptake of new tools and efficient implementation of existing strategies. The funding allocated to operational research was, however, much lower than all other research areas, representing only 4 % of the 2014 target at $80 million.
How much funding was available?
Research funding disbursed by public funding agencies, philanthropic and academic organizations and industry groups over the 2011–2015 period fell far short of the Global Plan goals. By the end of 2014, only $2.7 billion had been invested in tuberculosis R&D since 2011, just over one-fourth of the $9.8 billion called for. None of the research areas were funded at the target levels in 2014 (Table 1 ). Operational research met two-thirds of its target, higher than any of the other research areas, possibly because it had the lowest target. The greatest discrepancy between targeted and achieved funding was for new diagnostics, which received less than one-fifth of the $340 million goal for 2014.
To put tuberculosis research funding levels into context, an analysis of research investments for UK institutions concluded that tuberculosis is underfunded in comparison to HIV and malaria, despite causing the most mortality; between 2011 and 2013, tuberculosis research received only 20 % of the total $344 million funding, whereas HIV and malaria received approximately 40 % each [ 17 ]. Similarly, the Global Fund to Fight AIDS, Tuberculosis and Malaria, a funder that mainly provides programmatic support of which a small proportion goes towards research, allocated the lowest amount of funding to tuberculosis; in 2015, disbursements were $15.5 billion for HIV, $7.2 billion for malaria and $4.1 billion for tuberculosis [ 18 ].
How well do research agendas match with researchers’ priority areas?
Within the individual research areas in the Global Plan, tuberculosis researchers’ priority objectives included developing better (more potent, less toxic, shorter duration of treatment) drugs for drug-resistant and drug-susceptible tuberculosis, identifying biomarkers for disease progression and immune responses, developing vaccines that are effective in adults and HIV-infected individuals, making accessible point of care diagnostics for all forms of tuberculosis and assessing strategies to optimize implementation of tuberculosis control strategies.
Additional priority research areas (not explicitly included in the Global Plan for R&D funding at present) were also highlighted by researchers. Improved understanding of tuberculosis transmission dynamics was identified as a key research need in order to plan more targeted, effective prevention interventions. The role of social protection and social determinants in tuberculosis is another area that researchers directed attention towards; indeed, there is a danger that neglecting to tackle socioeconomic determinants of tuberculosis may justify criticisms about failing to learn lessons from the massive reduction in tuberculosis incidence in much of Europe, which was achieved without drugs, vaccines or technologically-advanced diagnostics [ 19 ]. Finally, health systems and policy research is not yet included as an independent research area in the Global Plan. Health systems and policy research is distinct from operational research as the latter focuses on optimizing implementation of tuberculosis control tools and strategies, whereas the former is concerned with factors influencing policymakers’ decisions, integration of tuberculosis control programs within the wider health system, and studies to inform optimal allocation of resources for tuberculosis control. Funding of both operational and health systems and policy research is essential for achieving maximum impact on tuberculosis control with limited resources, an aspect that the tuberculosis control community is currently struggling with. While most researchers cited priority research questions that were linked to their own work, those working on development of new drugs, vaccines and diagnostics recognized the importance of research to ensure that new tools can be accessed by tuberculosis patients in resource limited settings.
Funding priorities are essential for the effective allocation of limited resources and they can act as a focal point for driving financial investment. However, it is important to critically consider funding priorities that are being set and who is setting them. Policymakers and funders often prefer a biomedical approach to disease control and pay less attention to addressing more complex sociopolitical realities and their impact on the causal pathways of disease [ 20 ]. It is thus encouraging that the new Global Plan to End TB 2016–2020 recognizes that “ medical interventions alone will not be enough to end tuberculosis ” and stresses the importance of Universal Health Coverage and social determinants [ 5 ]. It is now vital to ensure that the R&D component of the Global Plan – which currently focuses on only three biomedical components: drugs, vaccines and diagnostics – prioritizes funding for research on health systems strengthening, translation of research into effective policies, addressing social determinants of tuberculosis, understanding transmission hotspots and analyses which inform optimal resource allocation.
We must also recognize that some funding streams may encourage researchers to restrict their activities to discrete silos, separating applied or implementation research from ‘hypothesis driven’ biomedical studies. We should therefore ensure greater support for cross-discipline research, which many funders are now emphasizing; for example, to explore the influence of poverty on immune correlates and to assess the impact of different investments (new drugs or vaccines, versus socioeconomic improvements versus Universal Health Coverage) on reductions in tuberculosis transmission and incidence.
Finally, there has to be flexibility in funding of priority areas identified by the research community and national tuberculosis programs themselves, such as health systems and policy research and studies on socioeconomic determinants, allowing researchers to be proactive and not only reactive to specific funding calls. Here, tuberculosis researchers must engage with funders and global policymakers to ensure that the research findings inform global tuberculosis control efforts more effectively. A pragmatic solution would be to support the formation of national bodies for setting research agendas, including key national stakeholders and researchers engaged in the country, which inform global funding priorities and play a role in evaluating research proposals in terms of applicability and potential impact on tuberculosis in high burden settings. Engaging local researchers would not only build research capacity and reduce costs from engaging primarily international teams, but also potentially aid dissemination and uptake of findings into policy.
Resource limitations did not allow us to expand the scope of our interviews to include researchers and policymakers in high tuberculosis burden countries; such a study would allow an important additional comparison of research priorities in international versus national institutions. Furthermore, we believe that a simple exercise in which national tuberculosis program representatives score the potential impact of findings from a number of recently completed studies would be very informative, and potentially surprising, for researchers and funders alike. Finally, interviews with representatives of key funding agencies would help to better understand why some diseases are funded disproportionately relative to disease burden (or potential public health impact), why narrow technology or biomedical approaches are often prioritized and how best to influence the research funding agenda.
Conclusions
There appears to be some disconnect between funding priorities, researchers’ agendas and global disease control strategies. Tuberculosis receives much less research funding than HIV and malaria despite causing more deaths globally, and the available funding is often channeled towards biomedical approaches; the 2011–2015 Global Plan recommended that far more funding be allocated to basic science and drug discovery than operational research to maximize the impact of new tools and, although the new Global Plan to End TB 2016–2020 highlights that biomedical interventions alone are not sufficient, the R&D component still focuses on drugs, vaccines and diagnostics. Improved coordination between stakeholders in high tuberculosis burden countries, researchers, international policymakers and funders would help to ensure that critical funding and knowledge gaps are addressed, and existing knowledge is acted upon more effectively.
Marshall G. Streptomycin in the treatment of pulmonary tuberculosis. A Medical Research Council investigation. BMJ. 1949;1:382–6.
Article Google Scholar
Frick M. 2015 Report on Tuberculosis Research Funding Trends, 2005–2014: A Decade of Data. New York: Treatment Action Group; 2015.
Google Scholar
Fox W, Ellard GA, Mitchison DA. Studies on the treatment of tuberculosis undertaken by the British Medical Research Council Tuberculosis Units, 1946–1986, with relevant subsequent publications. Int J Tuberc Lung Dis. 1999;3:S231–79.
CAS PubMed Google Scholar
World Health Organization. Global Tuberculosis Report 2015. Geneva: WHO; 2015.
Global Plan to End TB Paradigm Shift 2016–2020. Geneva: Stop TB Partnership; 2015
McMillen CW. Discovering Tuberculosis: A Global History 1900 to the Present. New Haven: Yale University Press; 2015.
Book Google Scholar
Upshur R, Singh J, Ford N. Apocalypse or redemption: responding to extensively drug-resistant tuberculosis. Bull World Health Organ. 2009;87(6):405–84.
Onyebujoh P, Rodriguez W, Mwaba P. Priorities in tuberculosis research. Lancet. 2006;367(9514):940–2.
Article PubMed Google Scholar
Donald P, Maher D, Qazi S. A research agenda to promote the management of childhood tuberculosis within national tuberculosis programmes. Int J Tuberc Lung Dis. 2007;11(4):370–80.
Hesseling AC, Cotton MF, Marais BJ, Gie RP, Schaaf HS, Beyers N, Fine PE, Abrams EJ, Godfrey-Faussett P, Kuhn L. BCG and HIV reconsidered: moving the research agenda forward. Vaccine. 2007;25(36):6565–8.
Fauci AS, Group NTW. Multidrug-resistant and extensively drug-resistant tuberculosis: the National Institute of Allergy and Infectious Diseases Research agenda and recommendations for priority research. J Infect Dis. 2008;197(11):1493–8.
Marais B, Raviglione M, Donald P, Harries A, Kritski A, Graham S, El-Sadr W, Harrington M, Churchyard G, Mwaba P, et al. Scale-up of services and research priorities for diagnosis, management, and control of tuberculosis: a call to action. Lancet. 2010;375(9732):2179–91.
Wallis R, Pai M, Menzies D, Doherty T, Walzl G, Perkins M, Zumla A. Biomarkers and diagnostics for tuberculosis: progress, needs, and translation into practice. Lancet. 2010;375(9729):1920–37.
London School of Hygiene and Tropical Medicine. TB Centre Members. http://tb.lshtm.ac.uk/about-us/members/ . Accessed 22 February 2016.
The Global Plan to Stop TB 2006–2015. Geneva: Stop TB Partnership; 2006
The Global Plan to Stop TB 2011–2015: transforming the fight towards elimination of tuberculosis. Geneva: WHO; 2010.
Head MG, Fitchett JR, Derrick G, Wurie FB, Meldrum J, Kumari N, Beattie B, Counts CJ, Atun R. Comparing research investment to United Kingdom institutions and published outputs for tuberculosis, HIV and malaria: a systematic analysis across 1997–2013. Health Res Policy Syst. 2015;13:63.
The Global Fund to Fight Aids, Tuberculosis and Malaria: Financials. http://www.theglobalfund.org/en/financials/ . Accessed 22 February 2016.
Rasanathan K, Sivasankara Kurup A, Jaramillo E, Lönnroth K. The social determinants of health: key to global tuberculosis control. Int J Tuberc Lung Dis. 2011;15 Suppl 2:S30–6.
Tesh S. Hidden arguments: political ideology and disease prevention policy. New Brunswick: Rutgers University Press; 1988.
Download references
Acknowledgements
We gratefully acknowledge Katherine Horton’s support in collating information from the LSHTM TB Centre member consultation exercise.
Authors’ contributions
MSK led the conceptualization, analysis and writing of the manuscript. RC and HF contributed to writing the manuscript and all authors provided critical input. All authors read and approved the final manuscript.

Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
Not applicable.
Open Peer Review Reports
The author’s response to reviewers is available as Additional file 1 .
Author information
Authors and affiliations.
London School of Hygiene and Tropical Medicine, London, UK
Mishal S. Khan, Helen Fletcher & Richard Coker
Saw Swee Hock School of Public Health, National University of Singapore, Tahir Foundation Building, 12 Science Drive 2 #10-01, Singapore, 117549, Singapore
Mishal S. Khan
Faculty of Public Health, Mahidol University, Bangkok, Thailand
Richard Coker
You can also search for this author in PubMed Google Scholar
London School of Hygiene and Tropical Medicine TB Centre Steering Committee
Corresponding author.
Correspondence to Mishal S. Khan .
Additional file
Additional file 1:.
Response to reviewers. (DOCX 120 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Khan, M.S., Fletcher, H., London School of Hygiene and Tropical Medicine TB Centre Steering Committee. et al. Investments in tuberculosis research – what are the gaps?. BMC Med 14 , 123 (2016). https://doi.org/10.1186/s12916-016-0644-0
Download citation
Received : 26 February 2016
Accepted : 14 June 2016
Published : 25 August 2016
DOI : https://doi.org/10.1186/s12916-016-0644-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Research agendas
- Tuberculosis
BMC Medicine
ISSN: 1741-7015
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Afr Health Sci
- v.21(3); 2021 Sep
Prevalence and associated factors of HIV-TB co-infection among HIV patients: a retrospective Study
Associated data.
All data generated or analyzed during this study are available from the corresponding author on reasonable request.
TB/HIV co-infection is a major public health problem in many parts of the world. But the prevalence of co-infection was varies among countries.
This study was designed to assess prevalence of TB/HIV co-infection and to determine its factors.
A retrospective study was done among HIV-positive patients at Hiwot Fana hospital from December, 2014 to 2018. The study participants were selected by simple random sampling. Patients with incomplete chart reviews were excluded and demographic, clinical and laboratory information were analyzed using SPSS and STATA. Uni-vitiate and bivariate logistic regressions were applied.
Five hundred fourteen patients were enrolled in this study. Of these, 187(37.4%) had TB. Bivariate logistic analysis showed that HIV patients with regards to marital status[AOR = 2.6; 95%CI = 1.19–2.89], education status [AOR = 3.74; 95%CI = 2.47–5.66], weight less than 50kg [AOR = 2.54; 95% CI = 1.35 – 4.81], CD4 level < 200cells/mm 3 [AOR = 4.57; 95%CI = 2.38– 6.86] and patient who were at WHO clinical stage III [AOR = 7.8; 95%CI = 5.15 – 8.55] were significantly associated with TB/HIV co-infection.
The prevalence of TB among HIV patients was high and predicted by marital, education status, weight, CD4 cell count and WHO clinical stage III.
Introduction
TB and HIV co-infection is a major public health problem in many parts of the world. But the prevalence of TB/HIV co-infection was varies among countries. Exploring the reasons of the diversity of TB/HIV co-infection is important for public policy, planning and development of collaborative TB/HIV activities. 25
Tuberculosis is the most common presenting opportunistic infection and a major public health problem. It is the cause of death among infectious diseases for people living with HIV/AIDS worldwide 1 – 3 .
Worldwide, there were an estimated of 9 million incident cases of tuberculosis in 2013 with 13% co-infected with HIV. An estimated 1.5 million deaths were attributed to TB, excluding deaths among HIV-infected patients. Among infectious diseases, both tuberculosis (TB) and HIV/AIDS represent global public health emergencies. Their mutually detrimental effect on the individual patient and at the population level is most evident in sub-Saharan African countries 4 .
According to the World Health Organization report Ethiopia ranked as the 7th country among the 22 high burden countries with TB - HIV infection in the world 5 . TB and HIV/AIDS display a lethal bidirectional interaction, with major epidemic overlap. People living with HIV are almost 30 times more likely than HIV-uninfected people to develop TB, and the chronic immune stimulation resulting from active TB accelerates HIV/AIDS disease progression 6 – 8 .
Unlike other opportunistic infections, TB disproportionately affects people living with HIV even before any significant drop in CD4+ T cell counts. The key predictor of immune reconstitution inflammatory syndrome (IRIS) is the degree of HIV-induced immunosuppression (low CD4+ count) at ART initiation 9 .
The current increasing of HIV/AIDS associated tuberculosis shifted the clinical pattern of TB towards smear negative pulmonary TB (PTB) and extra-pulmonary TB (EPTB), which in turn, causes difficulties in the diagnosis and treatment of TB due to unusual clinical picture with increased smear negative acid fast bacilli (AFB) PTB, atypical finding on chest radiography and increased prevalence of EPTB 10 , 11 .
Several studies confirmed that the clinical manifestations of TB in people with HIV are quite different and generally show different patterns as a function of the CD4+ T cell count. In addition, TB can appear at any stage of HIV/AIDS infection, and its presentation varies with the WHO stage and CD4+ lymphocyte count, although it is more frequent when CD4+ T cell count is below 200 cells/mm 3 12 . Research findings indicated that some HIV-infectd people develop TB, while others do not. This idea implies that being HIV positive is not the only factor for being infected with TB, and there are various determinant factors that contribute to TB/ HIV co-infection 12 – 14 . Understanding the predictors of TB/HIV co-infections in the local context is critical point for Ethiopia to improve TB/HIV co-infected patients. In the study area, there were no relevant research done on the prevalence and determinants of TB-HIV co-infection.
The objective of this study was to determine the prevalence and factors associated with TB co-infection among HIV patients in Hiwot Fana hospital in Harar region, which will help to reduce the risk of death and its burden by taking early drug management in the local context.
Case Definitions
The TB case definitions below are based on the level of certainty of the diagnosis and on whether or not laboratory confirmation is:
Tuberculosis suspect. Any person who presents with symptoms or signs suggestive of TB. The most common symptom of pulmonary TB is a productive cough for more than 2 weeks.
Case of tuberculosis. A definite case of TB in which a health worker (clinician or other medical practitioner) has diagnosed TB and has decided to treat the patient with a full course of TB treatment. Any person given treatment for TB should be recorded as a case. Incomplete trial TB treatment should not be given as a method for diagnosis.
Definite case of tuberculosis. A patient with Mycobacterium tuberculosis complex identified from a clinical specimen, either by culture or by a newer method such as molecular line probe assay.
Study Design and Area
This study was a hospital based retrospective study addressing the prevalence of TB among HIV/AIDS. It used data from the HIV patients attending the ART clinic from December, 2014 to December, 2018 in Hiwot Fana hospital in Harari region, Ethiopia. Hiwot Fana Specialized University hospital serves as a referral hospital for the entire Eastern part of Ethiopia, including Eastern Oromia, Dire Dawa city administration, the Somali regional state and the Harari regional state. The facility is treats more than 2,097 HIV positive patients. It is a teaching hospital for Haramaya University health and medical sciences students. Hiwot Fana specialized University hospital obstetric department admits more than 3000 patients per year, with 2664 deliveries.
Sample size and sampling procedure
The sample size was determined by taking the estimated proportion (P) of TB15 among people with HIV positive ratio= 0.1, margin of error = 2 % and confidence level = 95%, and the required sample size became 864. The 4 years HIV/AIDS patients' case files were identified and the study participants were selected by simple random sampling which gives an equal chance for each subjects to be included in the study, since the nature of target population is heterogeneous, to increase the precision on the study findings. After excluding patients with incomplete medical records, and by adding 10 % to replace the excluded samples, 514 HIV patients who were under ART were considered as study samples to collect the data.
Data collection instruments and procedures
Data were collected from patients' chart files using a checklist which was prepared by adopting previous studies 16 – 18 . Pre-test was conducted for the check list before the actual data collection and some variables such as religion, employment status, functional status and alcohol intake were omitted because of incomplete medical records. Otherwise, the checklist was inclusive of the different socio-demographic variables (sex, age, education status, marital status, residence) and clinical characteristics (CD4 count, weight) which were assumed as possible determinants of TB occurrence among people with HIV. Data quality was assured by pre-tested data collection and by trained data collectors. Completeness and consistency of data was checked by professionals and data clerks before and after data entry.
Data Analysis
The data was collected and entered in-to the statistical package for social science (SPSS) version 23 and STATA version 14 were used. Frequency and percentage were determined for descriptive analysis of socio-demographic, clinical and laboratory profile of the study subjects. Multivariable logistic regression was used by entering all variables with p-value < 0.25 in the bivariate analysis. Finally, logistic regression with forward likelihood variable selection method with p-value < 0.05 was used to identify the determinant factors associated with TB/HIV co-infection. The Hosmer-Lemeshow test of goodness of fit was used to model diagnosis with p-value > 0.05 provided good fit for the model.
Socio-demographic characteristics
Medical records chart of 514 people living with HIV were used. The mean age of the study participants was 34.17 years with standard deviation (SD) of 3.6 years (34.71±3.6). Most of the participants were females 270(52.5%), aged greater than or equal 30 years were 296(57.6%), living in urban residents were 273(53.2%). Moreover, 282(54.9%) of the study participants were married and 310(60.3%) of the participant were educated ( Table 2 ).
Socio-demographic characteristics of study participants in Hiwot Fana Referral Hospital (n = 514)
There were 514 participants in the study. Of these 187(37.4%) of them were had HIV/TB co-infection. Of the total, 187 TB/HIV co-infected, female respondents had higher proportion 108(57.8%) as compared to male respondents 79(42.2%). Patients whose CD4 count was less than 200cells/mm 3 had larger proportion 120 (64.4%) as compared to those CD4 count ≥ 200 cells/mm 3 67(35.6%). Furthermore, majority of TB/HIV co-infected patients 107 (57.2%) live in urban residence. From the same result among TB/HIV patients 95(50.8%) were married while 92(49.2%) were others (single, divorced and widowed). Moreover, out of TB/HIV co-infected patients, 76(40.6%), were found in WHO clinical stage of III, 73(39%) in WHO clinical stage of IV, 21(11.2%) under WHO clinical stage of III and 17(9.1%) in WHO clinical stage of I. In addition, more than half of co-infected patients 98(52.4%) but the remaining were illiterates ( Table 3 ).
Bivariate and Multivariable association of TB/HIV co-infection and independent factors
Others means(Single, divorced and Windowed)
The Hosmer-Lemeshow test provided good fit for the model (p-value =0.673)
Results in the bivariate analysis showed that the variable residence, WHO clinical stage, education status, marital status, CD4 counts and weight were associated with TB/HIV co-infection. Multivariate analysis in multiple logistic regression was used to determine factors of TB/HIV co-infection after adjusting other covariates. From this result, HIV patients whose marital status was different from married were 2.6 times more likely to develop TB than that of married [AOR= 2.6; 95 % CI = 1.19 – 2.89]. The illiterate patients were 3.74 times more likely to develop TB as compared to the educated patients [AOR = 3.74; 95% CI = 2.47 – 5.66]. Furthermore, patients whose CD4 cell level < 200 cell/mm 3 were 4.57 times more likely to develop TB as compared with cell level ≥ 200 cell/mm3 [AOR = 4.57; 95% CI = 2.38 – 6.86]. This implies low CD4 cell count is potential determinant for TB/HIV co-infection. Similarly, patients in WHO clinical stage III were 7.8 times more likely to develop TB as compared to that of patient in WHO clinical stage I[AOR = 7.8; 95%CI = 5.15 – 8.55] ( Table 3 ).
Tuberculosis is an opportunistic infection in patients with HIV. The prevalence of TB/HIV co-infection in this study was 37.4%. This in line studies in southern Ethiopia (36.9%) 19 , in Addis Ababa (33%) 20 and the study conducted in Keniya (35.6 %) 21 . However, the finding of this study was higher compared to the study result in Amhara region, Ethiopia (27.7%) 12 and a study reported from Nigeria (11%) 22 . The possible reasons for this large variation in TB/HIV co-infection across the world may be due to difference in study settings, sample size, diagnosis facility, HIV infection rate, study area and study time.
Being at WHO clinical stage III, having a CD4 level < 200 cells/mm 3 , were identified as risk factors for TB development among HIV patients. These finding is consistent with other Hospital-based studies in Ethiopia 12 , 19 and the study in Nigeria 23 . In my study patients with marital status (single, divorced and widowed) were morelikely to develop TB, which is in line with the study of 12 Mitku and others. The literate were less likely to develop TB. This finding is consistent with the results in Ethiopia 22 and Zambia 24 . In contrast, a study in western Ethiopia 12 and in Addis Ababa, confirms that high level of education was associated with TB. The contradiction may be possibly due to large proportion TB/HIV co-infection among illiterate patients in my study area.
In this study the prevalence of TB/HIV co-infection was high (37.4%). The risk of TB/HIV occurrence was found to be high among patients whose marital status being single, divorced & widowed, who was illiterate, whose weight was < 50kg, CD4 level were below 200celsl/mm 3 , and patients in WHO clinical stage III. The large ratio of TB cases among HIV patients requires a special attention for clinical and radiological investigation. Furthermore, since clinical variables were associated with TB/HIV co-infection, health professionals should care for patients who are in WHO clinical stage III, and patient who had lower CD4 counts.
Limitation of the study
Even though I endeavored to identify factors associated with TB/HIV co infection, the study was conducted in a single hospital with small number of patients, not include variables like viral load, TB before ART, sputum positivity and others, it is difficult to make generalizations about the population and community-based studies are needed to substantiate the study conclusions.
Variables used in the Study
Acknowledgment
The authors would like to acknowledge all staff members at Hiwot Fana Hospital, especially ART clinical staffs for their support and cooperation during the study.
Abbreviations
AFT: Acid Fast Bacilli; AOR: Adjusted Odds Ratio; CI: Confidence Interval; COR: Crude Odds Ratio; EPTB: Extra Pulmonary Tuberculosis; HIV: Human Immunodeficiency Virus; PTB: pulmonary Tuberculosis; TB: Tuberculosis; WHO: World Health Organization
No funding available for this study.
Availability of data and material
Authors' contribution.
Conceived, designed the study, analyzed the data, supervise the data collectors, wrote the manuscript and approved the final manuscript.
Ethics approval and consent to participate
Head Department of Statistics, wrote a letter to Hiwot Fana hospital and Chief Clinical Directorate Director of the hospital, read the content of proposal and approved the use of an anonymized dataset of routinely collected data for this study. As the data used in this analysis were collected from chart review, patients were not requested to provide informed consent for the use of their data. Confidentiality was ensured through the removal of patient identifiers prior to the analysis.
Conflict of interest
None declared.

IMAGES
VIDEO
COMMENTS
7. TB research and innovation. 7. TB research and innovation. Tuberculosis (TB) research and innovation is essential to achieve the global TB targets of the United Nations (UN) Sustainable Development Goals (SDGs) and the World Health Organization (WHO) End TB Strategy. The SDG target is to "end the epidemic" by 2030; more specific targets ...
Introduction. Tuberculosis (TB) continues to pose a major threat to global health , and research is a key component of the Global Plan to Stop TB2011-2015 .Research is particularly critical for developing new tools and approaches needed for eliminating TB by 2050 .Recognizing this, the Stop TB Partnership and the World Health Organization's (WHO) Stop TB Department have launched the TB ...
Tuberculosis research. Tuberculosis is the leading cause of death from a single infectious agent and remains a global health emergency. In 2018 alone, there were 1.5 million deaths and 10 million new cases globally, among whom half a million had rifampicin resistant TB. The annual rate of decline in TB incidence is still much lower than what ...
Research Plan. Strategic Priority 1: Improve Fundamental Knowledge of TB. Strategic Priority 2: Advance Research to Improve Diagnosis of TB. Strategic Priority 3: Accelerate Research to Improve TB Prevention. Strategic Priority 4: Support Research to Advance and Shorten Treatment of TB Strategic Priority 5: Develop Tools and Resources to ...
TB Trials Consortium. The TB Trials Consortium (TBTC) is a collaboration of North American and international clinical investigators whose mission is to conduct programmatically relevant research concerning the diagnosis, clinical management, and prevention of TB infection and disease.. Behavioral and Social Science Research. Behavioral and social science research has the potential to make a ...
To eliminate tuberculosis globally, a new, effective, and affordable vaccine is urgently needed, particularly for use in adults and adolescents in low-income and middle-income countries. We have created a roadmap that lists the actions needed to accelerate tuberculosis vaccine research and development using a participatory process. The vaccine pipeline needs more diverse immunological ...
Background. Worldwide, Tuberculosis (TB) is one of the top ten causes of death and continues to be a significant global health threat, which is the leading cause of a single infectious agent (above HIV/AIDS) [1, 2].In 2017, TB caused an estimated 1.3 million deaths (range, 1.2-1.4 million) among HIV-negative people [].TB is the central public health problem in low-income countries [3, 4 ...
Despite two decades of intensified research to understand and cure tuberculosis disease, biological uncertainties remain and hamper progress. However, owing to collaborative initiatives including ...
Policy guidance Research questions 1. Early detection of TB 3 1.1 Systematic screening for active tuberculosis: principles and recommendations 3 2. Diagnosing TB disease 35 2.1 Xpert MTB/RIF and Ultra assays for the diagnosis of pulmonary and extrapulmonary TB in adults and children and WHO Meeting Report of a Technical Expert Consultation: non ...
PRIORITIES FOR TUBERCULOSIS RESEARCH 7 Professor B. Xu Deputy Chair, Department of Epidemiology and Director, Tuberculosis Research Centre, School of Public Health, Fudan University, Shanghai, China. Professor C. Y. Yu Co-Chair, WHO Tropical Disease Reference Group (TB, Leprosy, Buruli Ulcer);
1. Introduction. Tuberculosis (TB) is a leading global public health problem, with high morbidity and mortality in humans. Until the COVID-19 pandemic, TB was still the leading cause of death from a single infectious agent, ranking above HIV/acquired immune deficiency syndrome [].The number of people newly diagnosed with TB fell from 7.1 million in 2019 to 5.8 million in 2020, and reduced ...
This first TBESC-II study was a head-to-head comparison of the three tests for TB infection in populations at high risk of latent TB infection and/or progression to TB disease. Sub studies. Repeatability and reproducibility of two interferon-gamma release assay (IGRA) blood tests- the QuantiFERON ® -TB Gold In-Tube (QFT-GIT), and T-SPOT ®.
Approximately 10·6 million people worldwide develop tuberculosis each year, representing a failure in epidemic control that is accentuated by the absence of effective vaccines to prevent infection or disease in adolescents and adults. Without effective vaccines, tuberculosis prevention has relied on testing for Mycobacterium tuberculosis infection and treating with antibiotics to prevent ...
Tuberculosis is the leading cause of death from a single infectious agent, with over 25% of these occurring in the African region. Multi-drug resistant strains which do not respond to first-line ...
High-quality research evidence is critical for improving global health and health equity, and for achieving the World Health Organization (WHO)'s objective of the attainment of the highest possible level of health by all peoples [1]. This need is most apparent when responding to complex epidemics such as tuberculosis (TB). TB is the leading killer among diseases caused by an infectious agent ...
Tuberculosis (TB) remains a significant global health challenge, with millions of new cases reported each year. Early detection and timely intervention are crucial in preventing the spread of the disease and reducing its impact on affected individuals and communities. This project proposal aims to implement a comprehensive strategy for the early detection and control of
other stakeholders to accelerate TB research and innovation, and improve equitable accessto the benefits of research. It will do so through clear objectives and recommendations, as set out below: (a) Create an enabling environment for high-quality TB research and innovation to increase capacity to conduct research and use its outcomes equitably, in
Introduction. Tuberculosis (TB) remains an important public health problem .With close to 10 million new cases per year, and a pool of two billion latently infected individuals, control efforts are struggling in many parts of the world (Figure 1).Nevertheless, the renewed interest in research and improved funding for TB give reasons for optimism.
Research funding disbursed by public funding agencies, philanthropic and academic organizations and industry groups over the 2011-2015 period fell far short of the Global Plan goals. By the end of 2014, only $2.7 billion had been invested in tuberculosis R&D since 2011, just over one-fourth of the $9.8 billion called for.
Background. Tuberculosis is an infectious airborne disease caused by Mycobacterium tuberculosis . It still remains a major public health problem which affects all age groups. Risk of exposure is higher in household contact than members of the general population. Objective. The aim of this study was to assess the prevalence and associated factors of tuberculosis among adult household contacts ...
3.3 Funding for TB research 11 4. The global TB research agenda 12 5. The Dutch TB research policy, global health themes and research areas 14 5.1 The Dutch TB research agenda and the Netherlands Science Policy Framework 14 5.2 The Dutch TB research agenda and other global health priorities 15 6. The Dutch areas of excellence explained 16
Research proposal examples. Writing a research proposal can be quite challenging, but a good starting point could be to look at some examples. We've included a few for you below. Example research proposal #1: "A Conceptual Framework for Scheduling Constraint Management" Example research proposal #2: "Medical Students as Mediators of ...
Tuberculosis is the most common presenting opportunistic infection and a major public health problem. ... Research findings indicated that some HIV-infectd people develop TB, while others do not. ... read the content of proposal and approved the use of an anonymized dataset of routinely collected data for this study. As the data used in this ...