Appointments at Mayo Clinic
Stroke rehabilitation: what to expect as you recover.
Stroke rehabilitation is an important part of recovery after stroke. Find out what's involved in stroke rehabilitation.
Stroke rehabilitation is a program of different therapies designed to help you relearn skills lost after a stroke. Depending on the parts of your brain affected by the stroke, rehabilitation can help with movement, speech, strength and daily living skills. Stroke rehabilitation can help you regain independence and improve your quality of life.
There’s a wide range of complications from stroke — and how well each person recovers afterward. Researchers have found that people who participate in a focused stroke rehabilitation program perform better than most people who don't have stroke rehabilitation. Therefore, stroke rehabilitation is recommended for all people affected by stroke.

What's involved in stroke rehabilitation?
There are many approaches to helping people recover from stroke. But overall, rehabilitation is centered around specifically focused and repetitive actions — practicing the same thing over and over again. Your rehabilitation plan will depend on the part of the body or type of ability affected by your stroke.
Physical activities might include:
- Motor-skill exercises. Exercises can help improve muscle strength and coordination throughout the body. These can include muscles used for balance, walking and even swallowing.
- Mobility training. You might learn to use mobility aids, such as a walker, canes, wheelchair or ankle brace. The ankle brace can stabilize and strengthen your ankle to help support your body's weight while you relearn to walk.
- Constraint-induced therapy. An unaffected limb is restrained while you practice moving the affected limb to help improve its function. This therapy is sometimes called forced-use therapy.
- Range-of-motion therapy. Certain exercises and treatments can ease muscle tension (spasticity) and help you regain range of motion.
Technology-assisted physical activities might include:
- Functional electrical stimulation. Electricity is applied to weakened muscles, causing them to contract. The electrical stimulation may help reeducate your muscles.
- Robotic technology. Robotic devices can assist impaired limbs with performing repetitive motions, helping the limbs to regain strength and function.
- Wireless technology. An activity monitor might help you increase post-stroke activity.
- Virtual reality. The use of video games and other computer-based therapies involves interacting with a simulated, real-time environment.
Cognitive and emotional activities might include:
- Therapy for cognitive disorders. Occupational therapy and speech therapy can help you with lost cognitive abilities, such as memory, processing, problem-solving, social skills, judgment and safety awareness.
- Therapy for communication disorders. Speech therapy can help you regain lost abilities in speaking, listening, writing and comprehension.
- Psychological evaluation and treatment. Your emotional adjustment might be tested. You might also have counseling or participate in a support group.
- Medication. Your doctor might recommend an antidepressant or a medication that affects alertness, agitation or movement.
Therapies that are still being investigated include:
- Noninvasive brain stimulation. Techniques such as transcranial magnetic stimulation have been used with some success in a research setting to help improve a variety of motor skills.
- Biological therapies, such as stem cells, are being investigated, but should only be used as part of a clinical trial.
- Alternative medicine. Treatments such as massage, herbal therapy and acupuncture are being evaluated.
When should stroke rehabilitation begin?
The sooner you begin stroke rehabilitation, the more likely you are to regain lost abilities and skills.
It's common for stroke rehabilitation to start as soon as 24 to 48 hours after your stroke, while you're in the hospital.
How long does stroke rehabilitation last?
How long you need stroke rehabilitation depends on the severity of your stroke and related complications. Some stroke survivors recover quickly. But most need some form of long-term stroke rehabilitation. This could last for possibly months or years after their stroke.
Your stroke rehabilitation plan will change during your recovery as you relearn skills and your needs change. With ongoing practice, you can continue to make gains over time.
Where does stroke rehabilitation take place?
You'll probably begin stroke rehabilitation while you're still in the hospital. Before you leave, you and your family will work with hospital social workers and your care team to determine the best rehabilitation setting. Factors to consider include your needs, what insurance will cover, and what is most convenient for you and your family.
The options include:
- Inpatient rehabilitation units. These facilities are either freestanding or part of a larger hospital or clinic. You may stay at the facility for up to 2 to 3 weeks as part of an intensive rehabilitation program.
- Outpatient units. These facilities are often part of a hospital or clinic. You may spend a few hours at the facility a couple of days a week.
- Skilled nursing facilities. The type of care available at a nursing facility varies. Some facilities specialize in rehabilitation, while others offer less-intense therapy options.
- Home-based programs. Having your therapy at home allows greater flexibility than other options. But you likely won't have access to specialized rehabilitation equipment. Insurance coverage for home-based programs varies widely.
Talk to your doctor and family about the best option for you.
Who participates in your stroke rehabilitation team?
Stroke rehabilitation involves a variety of specialists.
Specialists who can help with physical needs include:
- Doctors. Your primary care doctor — as well as neurologists and specialists in physical medicine and rehabilitation — can guide your care and help prevent complications. These doctors can also help you to achieve and maintain healthy lifestyle behaviors to avoid another stroke.
- Rehabilitation nurses. Nurses who specialize in caring for people with limitations with activities can help you incorporate the skills you learn into your daily routines. Rehabilitation nurses can also offer options for managing bowel and bladder complications resulting from a stroke.
- Physical therapists. These therapists help you relearn movements such as walking and keeping your balance.
- Occupational therapists. These therapists help you lead more independent and active lives. They can help you relearn skills for dressing, bathing and household chores and return to driving. Occupational therapists can also help improve your ability to swallow and your cognitive ability with home and workplace tasks and overall safety.
Specialists who focus on cognitive, emotional and vocational skills include:
- Speech and language pathologists. These specialists help improve your language skills and ability to swallow. Speech and language pathologists can also work with you to develop tools to address memory, thinking and communication problems.
- Social workers. Social workers help connect you to financial resources, plan for new living arrangements if necessary and identify community resources.
- Psychologists. These specialists assess your thinking skills and help address your mental and emotional health concerns.
- Therapeutic recreation specialists. These specialists help you resume activities and roles you enjoyed before your stroke, including hobbies and community participation.
- Vocational counselors. These specialists help you address return-to-work issues if that is one of your goals.
What factors affect the outcome of stroke rehabilitation?
Stroke recovery varies from person to person. It's hard to predict how many abilities you might recover and how soon. In general, successful stroke rehabilitation depends on:
- Physical factors, including the severity of your stroke in terms of both cognitive and physical effects
- Emotional factors, such as your motivation and mood, and your ability to stick with rehabilitation activities outside of therapy sessions
- Social factors, such as the support of friends and family
- Therapeutic factors, including an early start to your rehabilitation and the skill of your stroke rehabilitation team
The rate of recovery is generally greatest in the weeks and months after a stroke. However, there is evidence that performance can improve even 12 to 18 months after a stroke.
Stroke rehabilitation takes time
Recovering from a stroke can be a long and frustrating experience. It's normal to face difficulties along the way. Dedication and willingness to work toward improvement will help you gain the most benefit.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Jankovic J, et al., eds. Neurological rehabilitation. In: Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Elsevier; 2022. https://www.clinicalkey.com. Accessed March 14, 2022.
- Kellerman RD, et al. Rehabilitation of the stroke patient. In: Conn's Current Therapy 2022. Elsevier; 2022. https://www.clinicalkey.com. Accessed March 16, 2022.
- AskMayoExpert. Stroke rehabilitation. Mayo Clinic; 2022.
- Choi MJ, et al. Digital therapeutics: Emerging new therapy for neurologic deficits after stroke. Journal of Stroke. 2019; doi:10.5853/jos.2019.01963.
- Cunningham DA, et al. Tailoring brain stimulation to the nature of rehabilitative therapies in stroke. Physical Medicine & Rehabilitation Clinics of North America. 2015; doi: 10.1016/j.pmr.2015.07.001.
- Stroke. Natural Medicines. https://naturalmedicines.therapeuticresearch.com/databases/comparative-effectiveness/condition.aspx?condition=Stroke. Accessed March 14, 2022.
- Bellamkonda E (expert opinion). Mayo Clinic. March 21, 2022.
- Post-stroke rehabilitation fact sheet. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Post-Stroke-Rehabilitation-Fact-Sheet. Accessed March 14, 2022.
- Hoenig H. Overview of geriatric rehabilitation: Program components and settings for rehabilitation. https://www.uptodate.com/contents/search. Accessed March 14, 2022.
- Hoenig H. Overview of geriatric rehabilitation: Patient assessment and common indications for rehabilitation. https://www.uptodate.com/contents/search. Accessed March 14, 2022.
- Schultz BA (expert opinion). Mayo Clinic. March 17, 2022.
- Edwardson MA, et al. Overview of ischemic stroke prognosis in adults. https://www.uptodate.contents/search. Accessed March 14, 2022.
- Winstein CJ, et al. Guidelines for adult stroke rehabilitation and recovery. Stroke. 2016; doi.org/10.1161/STR.0000000000000098.
Products and Services
- A Book: Future Care
- Assortment of Products for Independent Living from Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Antiphospholipid syndrome
- Arteriovenous fistula
- Assistive technology therapy
- Atrial septal defect (ASD)
- Behcet's disease
- Carotid angioplasty and stenting
- Carotid artery disease
- Carotid endarterectomy
- Carotid ultrasound
- Constraint-induced movement therapy
- Coronary angioplasty and stents
- CREST Trial
- Dietary fiber
- Echocardiogram
- Essential thrombocythemia
- Four Steps to Heart Health
- Functional electrical stimulation
- High blood pressure dangers
- Home enteral nutrition
- How your brain works
- Intermittent fasting
- Lisa M. Epp, RDN, LD, discusses home enteral nutrition
- Lisa M. Epp, RDN, LD, discusses how to remove your feeding tube at home
- Lisa M. Epp, RDN, LD, discusses the new enteral connectors
- Locomotor training
- Manpreet S. Mundi, M.D., discusses tube feeding
- Mayo Clinic Minute: Telestroke technology inside ambulances
- NSAIDs: Do they increase my risk of heart attack and stroke?
- Seeing inside the heart with MRI
- What is a stroke? A Mayo Clinic expert explains
- Stroke: First aid
- Strokes FAQ Neurologist Robert D. Brown, Jr. M.D., M.P.H., answers the most frequently asked questions about strokes.
- Stroke rehabilitation
- Stroke Robot
- Symptom Checker
- Telemedicine Advances
- Typing with Brain Waves
- Coronary angioplasty
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Stroke rehabilitation What to expect as you recover
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Stroke Helpline
Monday to Friday: 9 am to 5 pm
Saturday: 10 am to 1 pm
Sunday: Closed
Supporter Relations
Saturday: Closed
- Professionals
- Planning and problem-solving (executive function)
The information on this page can be accessed in the following formats:
- Download this information as a pdf or large print document.
- Order a printed copy from our shop
- To request a braille copy, email [email protected]
If a stroke affects your executive function, here is how it might impact you and some ways you can get help.
On this page
Problems with planning and problem-solving Signs of problems with planning and problem-solving What can I do about planning and problem-solving?
Problems with planning and problem-solving (executive function)
Many other thinking processes happen without us being aware of them, known as automatic processes. Together, many of these automatic processes are known as executive function.
Executive function is about planning and problem-solving. It includes all the things that allow us to organise, make decisions and know when we need to do something. It also involves the way we monitor what’s going on around us, and adjust what we think and do in response.
Signs of problems with planning and problem-solving
If a stroke affects your executive function, you may find it hard to:
- Work out how to do certain things. This could be a task that seems quite simple like changing the channel on the TV remote control, or it could be more complicated, like making a meal.
- Plan how to complete a task. You may not be able to think of all the steps that are needed to do something, such as making a cup of tea, or put the steps in the correct order.
- Begin or finish a task on your own. You may not realise that you need to do something, like get dressed, until someone tells you, or you may need someone to prompt you throughout a task to help you to complete it.
- Solve problems on your own. You may not be able to work out what to do if something goes wrong.
- Do more than one thing at a time (multi-task). You may find it hard to switch between tasks and remember where you were with each task.
What can I do about my planning and problem solving?
Practise, practise, practise.
- Planning and problem solving can be improved, but only with lots of practice. Your occupational therapist, clinical psychologist or clinical neuropsychologist can help you decide what activities to focus on, as it will be different for everyone.
- Once you’ve mastered one task, like making a sandwich, you’ll move on to more difficult ones, like cooking a meal.
Keep to a routine
- Dressing yourself in the same order every day will make it easier for you to relearn the steps and spot when you miss one.
- Developing a weekly routine can also help. If you know that Tuesday is laundry day or Wednesday is shopping day, it will prompt you to do these things.
- A daily timetable may also be useful. This can be especially helpful if you have problems getting motivated, also known as apathy, which is fairly common after a stroke.
Use prompts and reminders
- Write out instructions or checklists to follow when you do something.
- Stick up notes around the house to remind you of things that you may not think of on your own, like brushing your teeth.
- You could use brightly coloured stickers on the microwave or remote control, to remind you which buttons to press.
- Prompts do not have to be written down. Use pictures or recordings instead. Some people make up songs or acronyms to help them remember how to do things.
Talk it through
- It can help to talk through a task with someone before you do it, to go over the steps.
- Also think about what could go wrong, so that you know what to do if that happens.
- Concentration problems
- Memory problems
- Problems moving or controlling your body (apraxia)
- Problems with movement and finding your way around (visual perception)
- Confusion and denial (anosognosia)
- Problems noticing things on one side (spatial neglect)
Related pages
Have questions? We are here to help!
Give us a call today at (415) 881-1433
Or Contact Us Here

Brain Exercises For Stroke Recovery Patients: Improving Cognitive And Memory Functions
Christopher ravn.
- March 20, 2024

Key Takeaways
1. A stroke is a serious, life-threatening medical condition that happens when the blood supply to part of the brain is cut off. 2. Training and exercising a stroke survivor's brain is known as stroke rehabilitation. 3. Memory exercises are a fundamental part of stroke rehabilitation, helping to retrain the brain and improve cognitive function that may have been affected by the stroke.
Table of Contents
1. What Are The Best Brain Exercises For Stroke Recovery? 2. What Are The Benefits Of Cognitive Exercises For Stroke Patients? 3. How Do You Train And Exercise Your Brain After A Stroke 4. How Effective Are Brain Stroke Recovery Exercises? 5. What Are Cognitive Therapy Activities For Stroke Victims And Survivors? 6. What Cognitive Activities For Adults After Stroke Are Most Effective? 7. How Do Stroke Cognitive Rehabilitation Activities Work? 8. Frequently Asked Questions About Brain Exercises For Stroke Recovery
What Are The Best Brain Exercises For Stroke Recovery?
A stroke is a serious, life-threatening medical condition that happens when the blood supply to part of the brain is cut off. Strokes occur when a blood clot blocks the flow of blood and oxygen to the brain. These blood clots are typically the result of atherosclerosis, or arteries narrowed or blocked over time by fatty deposits. This is the most common type of stroke. Less common are hemorrhagic strokes, where a blood vessel supplying the brain bursts.
People who survive a stroke are often left with long-term problems caused by an injury to their brain . They will face challenges with thinking, reasoning, awareness, and memory. If help is obtained over time, the brain retains some function but needs to reorganize itself. This journey to recovery is arduous and involves relearning skills, improving physical coordination, and maintaining cognitive functions.
The best exercises for stroke recovery focus on cognitive rehabilitation, including problem-solving activities like puzzles and board games, which enhance cognitive flexibility and decision-making skills . These exercises play a crucial role in helping individuals regain cognitive functions affected by stroke, such as memory, problem-solving skills, processing speed, and attention span, ultimately aiding in their recovery journey.
What Does Science Say About Light Therapy?
Find a collection of academic research papers that we, together with top-tier academic research institutions. We are exceedingly proud of our work and incredibly grateful to collaborate with such wonderful research institutions.
What Are The Benefits Of Cognitive Exercises For Stroke Patients?
Cognitive exercises play a crucial role in the rehabilitation of stroke survivors, but they need to be practiced consistently to be most effective. Following a stroke, the brain is busy rewiring new pathways to bypass the affected areas – a process known as neuroplasticity. Functions are being rewired to new, healthy areas of the brain, to compensate for tissue damage sustained in the stroke.
How Do You Train And Exercise Your Brain After A Stroke
Training and exercising a stroke survivor’s brain is known as stroke rehabilitation . These typically are a program of different therapies, designed for the survivor to help them with movement, speech, strength, and daily living skills post-stroke. The aim is to help them regain their independence and quality of life.
What’s involved in stroke rehabilitation is speech and language therapy , focused on improving communication skills affected by the stroke and common post-stroke issues such as swallowing difficulties, otherwise known as dysphagia.
We Believe Prioritizing Brain Health Enhances Your Quality Of Life
Get to know our team, our mission and how our EVY LIGHT® can provide you and your loved ones with a fuller life, letting you breathe a little easier.
How Effective Are Brain Stroke Recovery Exercises?
According to the National Library of Medicine, approximately 40% of patients suffer from functional impairment after stroke onset, and 15–30% experience severe motor, sensory, cognitive, perceptual, and/or language impairments.
Rehabilitation is vital for stroke survivors, and those who undergo consistent and professional rehabilitation tend to recover quickly . Studies have shown that rehabilitation exercise regimens applied soon after a stroke are effective. The programs will need to be tailored to the survivor and how they were affected, so that the correct areas are given the necessary attention.
Cognitive issues are often the most debilitating and difficult-to-address consequences of a stroke. A stroke survivor with memory and attention issues who engages in cognitive therapy, including puzzles and memory games , could experience improvements in their memory and concentration, allowing them to better manage daily tasks and activities.
One may question what the difference is between regular exercises and those intended for stroke patients. The answer lies in their intention. Pre-stroke exercises are typically general and aim to maintain overall health and well-being – cardio, strength training, and muscle toning, for example. In contrast, post-stroke exercises are more targeted, focusing on the rehabilitation and recovery of specific functions affected by the stroke. Post-stroke exercises often involve intensive therapy tailored to individual needs, such as speech therapy, physical therapy, and cognitive exercises.
Studies have shown that brain stroke recovery exercises can be highly effective in improving functional outcomes and quality of life for stroke survivors. Studies published in the Journal of Stroke found that intensive rehabilitation programs significantly improved motor function and activities of daily living in stroke patients. Another study published in the Journal of Neurologic Physical Therapy showed that cognitive rehabilitation can lead to improvements in memory, attention, and executive function in stroke survivors.
What Are Cognitive Therapy Activities For Stroke Victims And Survivors?
Cognitive therapy is designed to improve cognitive functions affected by the stroke, for example, memory, processing speed, problem-solving, language, and executive functions . The aim is to challenge the brain in a supportive way.
Cognitive therapy would include memory exercises, e.g., card games to improve short-term working memory; puzzles, computer games, and reading and summarizing to improve their attention, concentration, and information processing; reading, writing, and conversation practice to help with communication; drawing; navigation tasks to help with visual-spatial orientation, planning, and awareness; and problem-solving tasks to help improve planning and organization skills.
What Cognitive Activities For Adults After Stroke Are Most Effective?
How do stroke cognitive rehabilitation activities work.
A 37-year-old stroke survivor participated in memory-based exercises as part of his rehabilitation program. He regularly played memory games and engaged in storytelling activities with his therapist. Over time, his short-term memory and cognitive function significantly improved . He was able to recall important information, make decisions more confidently, and communicate more effectively with his family and healthcare providers.
Family members can play a crucial role in implementing these activities and supporting stroke rehabilitation. They can be educated on the importance of consistency and patience, as progress may be gradual.
Short-Term Memory Loss Exercises To Train Your Brain After A Stroke
- Repetition: This involves repeating information or tasks multiple times to reinforce memory. For example, repeating a new phone number several times to remember it.
- Association: This technique involves linking new information with existing memories or concepts. For instance, associating a new face with a familiar name or place.
- Visualization: Creating mental images can aid memory recall. For instance, visualizing a grocery list as items in specific locations in your home.
- Chunking: Breaking down information into smaller, manageable chunks can make it easier to remember. For example, remembering a long number by grouping it into smaller sets.
- Memory Games: Playing memory games like matching cards or word recall can be fun and effective. These games challenge the brain and improve memory skills.
Music Stimulation Therapy For Stroke Survivors
Music stimulation therapy can benefit stroke survivors by engaging multiple areas of the brain. Listening to music activates the auditory cortex , which processes sound, while also stimulating areas responsible for memory and emotions. This stimulation can enhance cognitive functions such as memory, attention, and executive function. Additionally, music can evoke emotional responses that may help reduce stress and anxiety, which are common after a stroke.
Some examples of music-based exercises at home include listening to familiar music, such as the stroke survivor’s favorite songs or music from their past. This can evoke memories and emotions, stimulating cognitive function. Caregivers and guardians can sing along to these songs with the patient, to further engage the areas of the brain responsible for these functions.
Enhance your brain performance through the power of light.
Comfortable and easy to use 40Hz light therapy to support and improve your brain function.
Motor Skills Activities For Adults After A Stroke
- Finger Tapping: Tap each finger to your thumb in sequence, then reverse the order. This can improve individual finger movements
- Finger Stretching: Gently stretch your fingers and thumb apart, then bring them back together. Repeat several times to improve flexibility and control.
- Drawing: Encourage drawing simple shapes or patterns, progressing to more complex drawings. This can improve hand-eye coordination and fine motor skills.
- Painting: Use a brush or fingers to paint on paper or canvas. This activity can improve grip strength and coordination.
Practicing Games For Stroke Rehabilitation
- Lumosity: This brain training app offers a variety of games designed to improve memory, attention, and problem-solving skills. Games like “Train of Thought” and “Memory Matrix” are particularly effective for cognitive exercise.
- Nintendo Wii Fit: Games like “Balance Bubble” and “Table Tilt” can improve balance, coordination, and cognitive function through interactive gameplay.

Other Activities That Help Retrain The Brain After A Stroke
An overall change in daily routines is crucial in stroke recovery to promote brain retraining and maximize rehabilitation outcomes.
The most important are physical activity and cognitive stimulation . Incorporating regular physical activity into daily routines can improve blood flow to the brain, promote neuroplasticity, and enhance overall brain health. Activities like walking, yoga, or tai chi can be beneficial.
As for mentally stimulating activities, these include reading, puzzles, or learning new skills, which can help retrain the brain and improve cognitive function . These activities should be challenging but achievable to promote brain plasticity.
Physical Activities In Cognitive Rehabilitation
- Walking: A safe and effective way to improve cardiovascular fitness and mobility. Start with short distances and gradually increase.
- Balance Exercises: Standing on one leg, heel-to-toe walking, and other balance exercises can improve stability and reduce the risk of falls.
Meditation And Relaxation Techniques For Cognitive Stimulation
- Focused Breathing: Sit comfortably and focus on your breath. Inhale deeply through your nose, hold for a moment, and exhale slowly through your mouth. Repeat for several minutes, focusing only on your breath.
- Guided Meditation: Use audio recordings or apps that guide you through a meditation practice, focusing on relaxation, gratitude, or mindfulness.
Social Participation As A Cognitive Exercise
- Support Groups: Joining a stroke support group allows individuals to connect with others who have experienced similar challenges, provide emotional support, and share coping strategies.
- Book Clubs or Discussion Groups: Participating in a book club or discussion group provides opportunities for intellectual stimulation and social interaction.
- You could also recommend light therapy for depression, as most would be negatively impacted by it.
Technology Aid In Stroke Rehabilitation Exercises
Apps and other digital tools can assist in cognitive rehabilitation post-stroke by providing accessible and engaging ways to improve cognitive functions. These tools can offer personalized exercises, real-time feedback, and progress tracking, making rehabilitation more efficient and effective .
View The Video Testimonials Of What Others Have Experienced
See how others have achieved a sharper mind by activating their gamma brainwaves in combination with maintaining a healthy lifestyle.
Frequently Asked Questions About Brain Exercises For Stroke Recovery
The best exercises for stroke recovery focus on cognitive rehabilitation, including problem-solving activities like puzzles and board games, which enhance cognitive flexibility and decision-making skills. These exercises play a crucial role in helping individuals regain cognitive functions affected by stroke, such as memory, problem-solving skills, processing speed, and attention span, ultimately aiding in their recovery journey.
What Are Cognitive Therapy Activities For Stroke Patients?
Receive notification when news, blogs, promotions, or other valuable information drops.

How To Deal With A Spouse With Memory Loss: Caring Tips For Living With Memory Loss & First Steps To Take
Mental Exercises For Mild Cognitive Impairment: Ideas For Improving And Preventing Mild Cognitive Decline

How To Help Someone With Cognitive Impairment: Caring & Communication Techniques To Improve The Quality Of Life Of Persons With MCI

How To Deal With Dementia In A Parent: Techniques To Help & Live With Dementia Parents At Home
How To Deal With Fixation In Dementia: Coping With Dementia Behavior Changes & Ideas To Focus Away From Fixation

How to Help Someone with Dementia Remember: A Comprehensive Guide for Caregivers and Families

Is Mild Cognitive Impairment A Disability? Legal Working Rights And Disability Benefits Advice

Living With A Spouse With Mild Cognitive Impairment: Caring Marital Relations To Adapt And Help A Spouse With MCI

How Long Does It Take For Light Therapy To Work: Duration & Frequency For Optimal Results & Benefits

How Long Can A Person With Dementia Live At Home: Setting Up A Safe Home Care Plan, Living Alone & Memory Care Considerations

How Fast Does Mild Cognitive Impairment (MCI) Progress: Turning Into Other Cognitive Decline, Risks Factors & Timeline

How Do Light Therapy Lamps Work? Best Ways To Maximize The Benefits & Timing Sessions

Brain Exercises For Seniors: Fun Ways Of Cognitive Training & How To Improve Mental Health In Older Adults

Sad Light vs Grow Light: How Different Are They?

Gifts for Dementia Patients: What’s a Good Presents Idea for Someone With Alzheimer’s & Memory Loss

Green Light Therapy Treatment & Its Health Benefits

How to Get Guardianship of an Elderly Parent With Dementia: Legal Steps

Meditation Light Therapy: How to Improve All Relaxation Techniques

Music Therapy for Dementia: Helping Patients Memory Functions

Sensory Activities for Dementia Patients: Improving Abilities & Quality of Life

How To Know When To Call Hospice For Dementia: Qualification Considerations

Which Sense Is Most Affected by Alzheimer’s Disease: Early Signs

What Is the Difference Between Memory Care vs Dementia Care?

Best Gifts for Seasonal Depression & Affective Disorder: Top Ideas

Speech Therapy Memory Activities for Adults: Enhancing Cognitive Skills

Light Therapy Treatment For Depression, SAD And Mood Disorders

How To Talk To Someone With Short-Term Memory Loss: Communication Strategies

Green Light Therapy Treatment For Depression, SAD And Mood Disorders

Brain Exercises To Prevent Alzheimer’s And Dementia: Types & The Best Ones

Transforming Lives: Melissa’s Journey with EVY LIGHT®

5 Warning Signs Of Early Alzheimer’s You Can’t Ignore

Crafting a Brain-Boosting Routine
How Learning Impacts The Brain

Thrive Together: Boosting Brain Health with Group Activities

Proactive Brain Health: Aging Gracefully with Science

Support Memory At All Stages of Life

Harnessing the Power of Dopamine for Keeping Mentally Energized

Strategies for Enhanced Focus: Unleash Your Productivity Potential

Move for Mind: The Link Between Exercise and Mental Health

The Vital Connection Between Your Sleep, Body, and Brain

Unlocking the Sunshine: 6 Tips to Banishing Brain Fog

Unveiling the Astonishing Energy Consumption of the Human Brain
Get exclusive content straight from the scientists who are rooting for you and your brain.
Comfortable Daily Use, Drug Free to Promote Focus, Clarity, and Mental Sharpness.
Privacy Preferences
When you visit our website, it may store information through your browser from specific services, usually in the form of cookies. Here you can change your Privacy preferences. It is worth noting that blocking some types of cookies may impact your experience on our website and the services we are able to offer.
10 Fun and engaging games for stroke patients
BY Anitha Thomas
8th Jun 2023 Health Conditions

"Games can provide a much-needed sense of normality and fun during a challenging time"
- Motor function: ability to move their body voluntarily
- Cognitive function: memory, learning, attention, decision making and language abilities
- Social interaction: conversations verbal or nonverbal
Board games

"Word games are a wonderful way to improve memory and language skills"
Music therapy
Storytelling games.

Adaptive sports
Sensory stimulation games.
"It's important to adapt the activities based on the individual's abilities"
- Start slowly and gradually increase the amount of time you spend playing the game over time.
- Listen to your body and stop if you feel pain .
- Find a quiet place where you can relax and focus on the game.
- Work your way through a Stroke Recovery Activity Book with a loved one or by yourself
- Take breaks throughout your sessions to rest your mind and body.
- Do activities with a friend or family member for support and motivation.
The world at your fingertips
Launched in 1922, Reader ' s Digest has built 100 years of trust with a loyal audience and has become the largest circulating magazine in the world
10 therapy tasks practiced most frequently by survivors of stroke
Stroke can impact all aspects of life—movement, communication, thinking, and autonomic functions such as swallowing and breathing. Research shows that early and specialized stroke rehabilitation can help to optimize an individual’s physical and cognitive recovery and enhance quality of life. Here, we identify the Constant Therapy tasks used most often by those recovering from stroke.
The goal of stroke therapy: help people regain lost skills
According to the Centers for Disease Control , about 87 percent of all strokes are ischemic strokes, in which blood flow to the brain is blocked. According to the American Speech-Language-Hearing Association, individuals with aphasia or other cognitive-communication issues represent up to 20 percent of the adult caseload for speech-language pathologists in the United States.
Typical goals of stroke therapy include:
- Restoring physical function and enhance the skills needed to perform daily activities
- Building strength, improving balance and regaining mobility
- Improving areas such as speech, language, cognition, or swallowing
- Developing new behavioral or compensatory strategies
Analysis: how is Constant Therapy being used with this population?
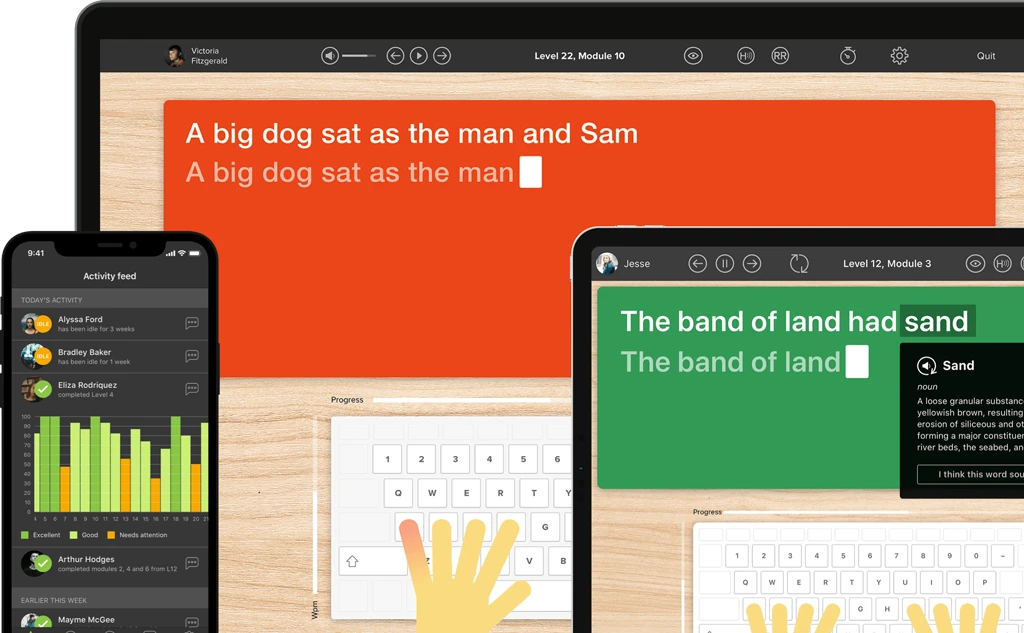
Constant Therapy uses artificial intelligence and data analytics to provide each user with a personalized brain exercise program targeting areas such as memory, attention, problem-solving, math, language, reading, writing, and many other skills. Research published in the Journal Frontiers in Human Neuroscience showed a significant improvement in standardized tests for survivors of stroke using the iPad-based rehabilitation technology of Constant Therapy.
An analysis of Constant Therapy users identified what tasks are assigned most frequently by clinicians working with survivors of stroke.
- We looked at data on 18,230 users who identified a diagnosis of stroke on the app.
- These 18,230 users completed an average of 572 tasks each
- Total tasks completed numbered 837,700.
The Constant Therapy tasks listed below are the 10 most frequently assigned by clinicians for their clients recovering from stroke.
The top 10 Constant Therapy exercises assigned by clinicians to patients recovering from stroke
1. Follow instructions you hear : Works on auditory memory and auditory comprehension through following directions . Individuals Assigned: 10,207 Percent of Users Identified As Recovering from Stroke 56%
2. Find the same symbols : Cognitive skills such as attention can be affected after a stroke. Find the same symbols targets a variety of skills which includes attention, visuospatial processing, and executive functioning . Individuals Assigned: 9,216 Percent of Users Identified As Recovering from Stroke: 51%
3. Put steps in order : For people recovering from a stroke, executive functioning skills may be affected. In this planning & organizing task , you are presented with steps of daily activities, and must drag these steps into the correct order. This is a great task for people working on sentence level reading comprehension too! Individuals Assigned: 8,814 Percent of Users Identified As Recovering from Stroke: 48%
4. Match pictures : For people with cognitive, speech, or language disorders, this task helps visual memory by matching pictures displayed on a grid. For people recovering from a stroke who are working on word retrieval, they can also practice naming the pairs of pictures that they match . Individuals Assigned: 7,629 Percent of Users Identified As Recovering from Stroke: 42%
5. Remember pictures in order (N-Back) : This memory task specifically targets an aspect of working memory called updating . There are 3 levels of difficulty. In Level 1, you must remember the order of the pictures from 1 picture ago. In level 3 you must recall 3 pictures ago. Want more N-Back Tasks? Do Remember spoken word order (N-Back) and Remember written words in order (N-back) , too! Individuals Assigned: 7,213 Percent of Users Identified As Recovering from Stroke: 40%
6. Do clock math : Stroke can affect number skills, math skills, and word finding. This task helps improve time-based calculation skills by answering math questions associated with clocks . Individuals Assigned: 6,701 Percent of Users Identified As Recovering from Stroke: 37%
7. Name Pictures : Helps improve word retrieval skills by speaking the name of presented images. There are 3 levels to this task, with each level increasing in word difficulty. Different cues include semantic, phonemic, graphemic, and whole word cues . Individuals Assigned: 6,635 Percent of Users Identified As Recovering from Stroke: 36%
8. Repeat a pattern : This task works on attention, visual working memory, and visuospatial skills . Individuals Assigned: 6,433 Percent of Users Identified As Recovering from Stroke: 35%
9. Understand voicemail : This functional task works on comprehension and memory of everyday language by answering questions about voicemails. Looking for a bigger challenge? Check out Infer from voicemail as well . Individuals Assigned: 6,085| Percent of Users Identified As Recovering from Stroke: 33%
10. Remember the right card : This task works on attention, disinhibition, and processing speed. The patient is asked to remember a playing card and tap on that card whenever it is presented in a series of cards . Individuals Assigned: 5,690 Percent of Users Identified As Recovering from Stroke: 31%
- Des Roches, C., Kiran, S. and Balachandran, I. (2015). Frontiers in Human Neuroscience, Effectiveness of an impairment-based individualized rehabilitation program using an iPad-based software platform , 2015 Jan 5. doi: 10.3389/fnhum.2014.01015.
- Centers for Disease Control and Prevention (2018). Stroke Facts .
- ASHA (2017). SLP Healthcare Survey: Caseload Characterisics .
Tackle your speech therapy goals, get top-notch support
Related articles, 11 comments.
Do you get this from the App Store? What is the cost?
Hi Lisa. Yes, check out the app store. Our monthly plan is $25 and an annual plan is $250 with a free tablet. If you want to set up a trial and need support, give us a call or email. 1-888-233-1399 or [email protected]
When I purchased a whole year package in 2023 I never received a free tablet. Is this something new?
Hi Todd, thank you so much for subscribing to Constant Therapy! Apologies for the confusion, this is an older comment and we discontinued this program back in 2019. If you have any questions or concerns about the device you use for Constant Therapy feel free to reach out to our Support Team at [email protected] .
What is the app name please?
- Constant Therapy
Thanks have learnt something. Am struggling with after stroke effects especially speech
Is there a way to have the math word problem questions read to you? My brother is working on math as well as re learning reading. He cannot read the questions yet to do the math problem…
Great question! This is a feature that we are working to add in the near future – keep an eye out for announcements in our weekly emails once we have that feature ready to use!
What exercises are recommended for people with primary progressive apraxia?
Hello Alberta, thank you for your question! We spoke with a Speech Language Pathologist and they said that difficulty levels will depend on the condition’s progression. You may be interested at looking into these exercises: Imitate Words, Imitate Sentences, Form and Say Active Sentences, and Form and Say Passive Sentences . These tasks will allow you practice with articulating speech at various levels of complexity. Hope this is helpful!

Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Constant Therapy Health
- Partner with us
- Try for free
- Request a Demo
- Conditions we support
- For clinicians
- For patients
- For veterans
Support + Resources
- Downloadable Resources
- Testimonials
Join the Conversation
For the majority of stroke patients, the road to recovery is a long one that includes many hours of therapy aimed at restoring both physical strength and language capacity. People who suffer a serious stroke may lose the ability to coordinate muscles and execute complex movements.
They can have trouble performing routine tasks including bathing, dressing and feeding themselves. Some will experience numbness or lose feeling in their limbs. Many will have difficulty understanding and producing language. While it is not always possible to recover completely from a stroke, with the right treatment plan quality of life can be improved.
According to the National Stroke Association, strokes are one of the top causes of long-term disability in adults. Damage can be irreversible and recovery may be affected by depression. This makes choosing the right treatment activities essential.
Keep in mind that every case is unique and no two stroke victims will need exactly the same type of therapy . Family and friends can provide emotional support and help reinforce coping strategies while specialized therapists will be able to suggest a recovery program, including tools and resources to try.
It’s important to remember that a stroke patient may be struggling with impairments but also grieving the loss of their former life, including their job, routine and independence. That’s why starting a recovery plan is key, even if progress isn’t immediately apparent.
Sticking to the programme over an extended period of time can bring about a change in attitude. It’s particularly useful to participate in activities that are both therapeutic and fun, to help stroke victims rebuild confidence and improve self-esteem.
What is a stroke?
Strokes are caused when blood supply to an area of the brain is cut off because of a clot or blood vessel that bursts. This results in the affected part of the brain not getting the oxygen it needs to function.
Depending on the severity and location of the blockage, as well as how long it lasts, a stroke can result in damage that impacts on physical and mental abilities – including language use and processing which may have short or long term consequences.
Common symptoms include: difficulty speaking and understanding language that was previously familiar and fluent, a left or right side weakness or paralysis including of facial muscles, numbness, muscle coordination and shaking and balance issues that make it hard to hold a pen or pencil or to move around, blurred vision which interrupts reading and causes seeing double (making it virtually impossible to look at certain kinds of screens), and slurred words and missing vocabulary that needs to be retrieved.
Note that while words become hard to reach, meaning is often still accessible which can result in a degree of frustration for stroke patients who know what they want to say but are unable to express themselves. It’s been described as a filing cabinet that has fallen over. The words are still there, but it can be difficult to find them and pull them out of the jumble.
Learn more about communication and language ability after a stroke .
Recovery activities for stroke patients
In addition to direct therapy at medical and rehabilitation centers, patients should beware of becoming isolated and try to engage in a handful of home-based and social activities throughout the week.
Get some exercise. Exercise in any form is important for rehabilitation. The coordination of movements brings about positive emotions thanks to endorphins. Even swaying side-to-side or rocking mobile parts of the body helps increase blood flow and is likely to make patients feel better.
Make art. The brain is a muscle and when its language centers are down you can stimulate it through color, texture and movement. If the fine motor skills required to hold a paintbrush are lacking, rethink your approach to art. Just arranging objects into collages and patterns or drawing in the sand with fingertips can be helpful.
Learn something new. You don’t have to go back to school, it might be you pick up a hobby like gardening or bird watching. You may also want to acquire a new skill—particularly one that helps with language recovery, such as practicing sign language or typing. Stimulating new areas of the brain gets things moving.
Satisfy your senses. Learning is enhanced through multi-sensory approaches in which you hear, see and feel material at the same time. Go to a greenhouse and smell the flowers, visit a museum or get a neck and shoulder massage. All of these activities stimulate your sensory systems.
Turn up the music. Hearing a rhythm can improve the attitude and outlook of stroke patients. It’s also a great way to maximize the potential for relearning coordinated movements and to work on balance. Express yourself in whatever way is possible, whether it be through syncopated tapping and conducting to the radio, or even just deep breathing in time to the music. Language and music are stored in different areas of the brain and someone who struggles with the spoken word may have no difficulty with singing a song. Singing is good exercise.
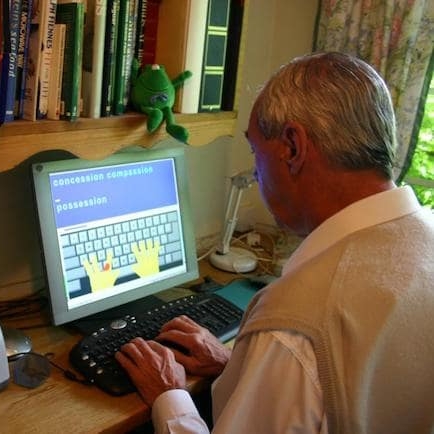
Try touch-typing. When writing by hand is too hard and speaking ability is inhibited, it can sometimes be easier to type messages on a computer or tablet. That’s because keyboarding trains muscle memory in the fingers to remember the spelling and help with word recovery. Repetitive drills reinforce learning and it is particularly helpful when the approach taken is multi-sensory – such as with Touch-type Read and Spell.
Engage your brain. Do some mental heavy lifting and try puzzles, audio books or even routine activities, such as making to-do lists. The idea is to work your reasoning, comprehension and problem solving skills. Meditation and clearing your mind afterwards can be a great way to wrap this type of activity up.
If you are putting together a plan for someone else, be creative as you consider the patient’s former hobbies and interests. As one illustrative example, a keen gardener may well appreciate a raised bed or bench that can be tended from a wheelchair. You may have to replace terra cotta pots with plastic ones so they are easier to lift and help with writing plant labels. Small tools with bigger handles are also a good idea.
Activities will vary greatly depending on the impact of the stroke and the patient’s recovery needs. Be aware that interacting with people is stressful and exhausting due to the communication required. Sometimes the stroke survivor just can’t keep up, and friendships may drift away.
People who have had a stroke and their carers can find great support in the company of others who’ve been there too. You may consider joining a local stroke support group. Being with others in the same boat can be both comforting and stimulating. In a context like this, group speech therapy sessions often prove popular and effective. Additionally, you can always suggest solo walks or encourage the person to sit outside to observe nature as part of a recovery plan that focuses on mindfulness.

TTRS as a resource
If you’re a therapist who works with stroke victims you’re probably aware of different solutions and online programs that can be used for language recovery.
Touch-type Read and Spell is a multi-sensory keyboarding program in which individuals hear letters and words, see them on the screen and then practice typing the correct keys. It focuses on repetition, sound-letter mapping and short spurts of multi-sensory activity and is ideal for those who may tire easily and need to take frequent breaks.
Individual modules can be repeated as often as necessary and the course provides plenty of feedback at each step, to enhance motivation and gradually build confidence and self-esteem for users. If you are a therapist you can help a person who’s had a stroke by working through the course with him or her at weekly sessions. Patients can then continue daily use of the course on their own, to reinforce learning.
Do you have any activities to add? Join the discussion in the comments!
When I used to do e-mails it was a nightmare, but now, what would take me half an hour I can do in five minutes. It's been two years since I started using the Touch-type Read and Spell course. In the beginning, one or two modules might have taken me half an hour and I’d try and do that every day. These days I’m much faster and I can do up to ten modules in one sitting. TTRS has given me confidence.
Brian, Retired engineer using TTRS
For stroke recovery
TTRS is a program that can support individuals who have had a stroke in recovering communicative ability.
Meredith Cicerchia

- Read more about Meredith Cicerchia
Chris Freeman

- Read more about Chris Freeman
Testimonials and reviews

Maria, Adult learner
Maria used to type with two-fingers, slowly and often inaccurately. Now she types faster, with fewer errors, more competently and professionally. This has boosted her confidence in the workplace tremendously. She now recognises individual sounds in words much better, due to the auditory aspect of the multi-sensory approach in TTRS. Her vocabulary has noticeably improved and she has found she can explain things and express herself more clearly in English after completing the course.
Read more of Maria’s story

Bolton College, Adult Education Program
At Bolton College we offer the TTRS course to self-study adult learners who have returned to education to improve their spelling, increase their familiarity with technology, and use word processors. We find that for many adult learners in our program, the conventional ‘look-cover-spell-check’ approach they were taught at school had a detrimental effect on their learning. In contrast, Touch-type Read and Spell provides a rewarding and positive experience for them when it comes to spelling.
Read more of Bolton College’s story
TTRS has a solution for you
An award-winning, multi-sensory course that teaches typing, reading and spelling
How does TTRS work?
Developed in line with language and education research
Teaches typing using a multi-sensory approach
The course is modular in design and easy to navigate
Includes school and personal interest subjects
Positive feedback and positive reinforcement
Reporting features help you monitor usage and progress
More realated articles from Read and Spell:
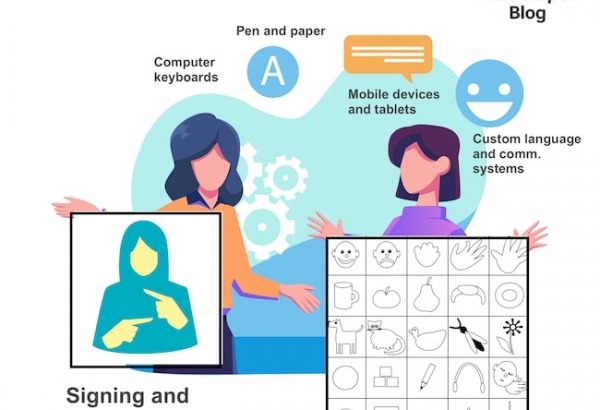
Augmentative and alternative communication
Augmentative and alternative communication is a general term used to refer to approaches, strategies, and tools, that enable children and adults with autism and speech and language disorders to communicate their wants, needs, thoughts, and emotions.
Augmentative and alternative communication is not appropriate for everyone with a speech or language disorder, but may be useful for people with apraxia of speech, stroke-related dysphasia and dysarthria, and other conditions that affect written expression and/or control of the muscles of the face, throat and mouth, such as cerebral palsy.
Sign language, pen and paper, and hand gestures are basic forms of augmentative and alternative communication, as is using a chart and pointing to pictures, letters, words or symbols.
Alternatives to speech can be as high-tech as specially fitted devices which allow people to communicate using custom buttons and pressure sensors, or as everyday as children and adults making use of a laptop computer and smartphone to meet their communication needs. On a computer or mobile device, written language can either be typed and displayed on screen or typed and read aloud by an automatized voice facilitated by text-to-speech technology.
Apraxia vs. aphasia: What’s the difference?
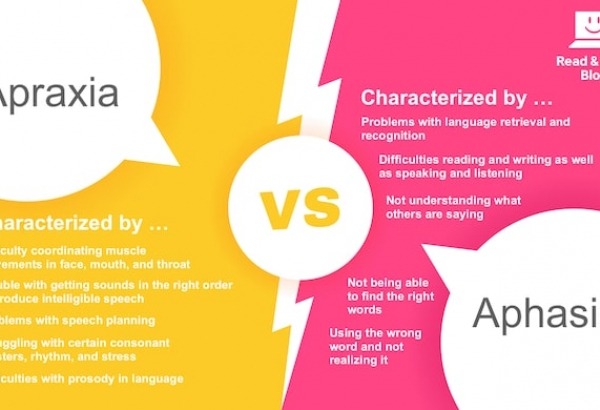
Both apraxia of speech and aphasia affect an individual’s ability to communicate – they just do so in different ways. Apraxia makes it hard to coordinate muscle movements and put sounds in the right order to produce intelligible speech. It may also impact speech planning. Individuals can struggle with consonant clusters, rhythm, and stress, and may generally experience difficulties with aspects related to the prosody of language.
On the other hand, aphasia is about language retrieval and recognition. People with aphasia or dysphasia may not be able to find the words they need to express themselves in speech or in writing, or they might use the wrong words and not realize it. Additionally, individuals with receptive aphasia don’t always understand what other people are saying and can finding listening and reading challenging.
If aphasia and apraxia of speech are the result of a stroke, a person may also experience difficulties with enunciation, referred to as dysarthria. This can present as trouble controlling the volume levels of speech, excessive drooling, or problems getting enough air while speaking. Dysarthria is caused by weakness or paralysis of the muscles of the lips, tongue, throat and face.

Regaining speech after a stroke
Communication difficulties following a stroke can take many forms. You may experience trouble finding the right word or have problems processing language that is directed at you – these conditions are commonly referred to as aphasia/dysphasia. When you struggle with speaking it’s referred to as productive aphasia and with understanding it’s receptive aphasia.
Aphasia and dysphasia are almost the same thing, except dysphasia is when you have partial access to language and aphasia is when you have none. Some individuals who have had a stroke find speaking difficult because of challenges with annunciation; this is called dysarthria. Speaking and breathing at the same time, or swallowing, may also be problematic with dysarthria.
It’s possible for paralysis, hemiplegia – one-sided paralysis - or hemiparesis - weakness on one side of the body following a stroke - to interrupt written modes of communication such as writing or typing. But just as every individual is unique, so is their recovery and it can be hard to put an exact estimate on the time it will take to regain communicative ability and/or how fully it will return.
Many people see the greatest gains in the first six weeks, as swelling in the brain goes down, and language processing areas which were temporarily affected come back online. However, it’s possible to see improvements for years after a stroke, particularly if an individual continues to receive speech therapy to strengthen and reinforce communication skills and confidence.

Aphasia recovery time following a stroke
One of the most common symptoms following a stroke is a disruption to language and communicative ability. This is a condition referred to as aphasia or dysphasia. The name aphasia implies a total loss of language, as compared to dysphasia , which is partial loss.
Nonetheless, the two terms are used somewhat interchangeably with dysphasia more common in Europe and the UK. Aphasia is a result of trauma to the brain, including when brain cells are deprived of oxygen or sustain damage due to internal bleeding. It can result in difficulty finding and retrieving words, producing intelligible speech, negotiating syntax (grammar), and sometimes even understanding what other people are saying.
Dysarthria vs. aphasia
While both dysarthria and aphasia can affect an individual’s ability to produce fluent and intelligible speech, they have very different causes. Dysarthria is an umbrella term used for disorders that impact the muscles used in speaking , including the lips, tongue, throat, vocal cords and diaphragm.
It causes a wide range of symptoms including breathy and nasal speech, drooling, uneven starts and stops, irregular volume, intonation and emphasis, and unclear articulation of words. Unlike brain-based conditions, language comprehension skills are typically not affected. On the other hand, aphasia is the result of injury to the brain. It has to do with understanding and producing language and symptoms will depend on the location and severity of the brain damage.

Stroke therapy at home
According to the Stroke Association in the United Kingdom and the American Stroke Association, there are over 8.2 million stroke survivors in the UK and the US. Many of these individuals undertake daily rehab activities in their own homes, either independently, or with the help of a friend, family carer or a trained specialist.
Stroke rehabilitation is many things including physical treatments that aim to improve gross and fine motor skills, language drills to restore communicative abilities, cognitive training to strengthen memory, occupational therapy to help with the performance of everyday tasks, and even emotional therapy to deal with any issues of depression or isolation that arise in the aftermath of a stroke.
Check out our most popular articles:
Learn to type. strengthen reading and spelling skills. boost confidence..
Discover multi-sensory typing with TTRS.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Dela J Public Health
- v.9(3); 2023 Aug
- PMC10494803

Cognitive Rehabilitation Interventions for Post-Stroke Populations
As of 2023, stroke continues to be one of leading causes of significant long-term disability in the United States. 1 Cognitive deficits are a common component of post-stroke sequala, limiting or impacting participation in functional activities of daily living. In addition to having substantial impacts on the individual diagnosed with stroke, family members, caregivers, and society also absorb the impacts of post stroke cognitive impairment in acute and chronic phases of recovery. It is estimated that approximately 60% of individuals have cognitive impairments as a result of stroke in the acute stages of recovery (within one year of their stroke) and those who experience mild severity deficits have the highest occurrence of recovery. 2 , 3
Given the high incidence of stroke and resultant significant impacts of cognitive impairment, there is a substantial need for evidence-based interventions and multidisciplinary efforts to facilitate return to independence, work, and participation in functional aspects of daily living. 4 Cognitive rehabilitation addresses skills in the cognitive domains of attention, memory, and executive functioning and how they impact functionality and safety. In a course of cognitive rehabilitation, rehabilitative therapists commonly refer to more advanced activities of daily living that require increased cognitive demands as Instrumental Activities of Daily Living (IADLs). Examples of IADLs may include meal preparation, managing medications, housekeeping, managing financial responsibilities, time management for appointments, and self-care.
How Does Cognitive Rehabilitation Start?
Cognitive assessments and interventions that comprise cognitive rehabilitation are within the scope of practice of speech-language pathologists (SLP), occupational therapists, and neuropsychologists. In this review, assessment and intervention facilitated by SLPs in cognitive rehabilitation will be explained to inform members of interdisciplinary teams, patients, families, and communities of the beneficial impacts of cognitive rehabilitation for stroke.
The specific education and training of a speech-language pathologist provides expertise in evaluating and intervening on how cognitive deficits impact communication within the modalities of speaking, listening, reading, and writing, which are frequently included in the demands of IADLs. In many cases, the location of stroke or brain injury can largely assist in predicting the types of cognitive deficits to be expected, given the known function of that location in the brain. The impact of cognitive impairment on communication is described as cognitive-linguistic or cognitive-communication impairment, with further analysis of deficits provided in the areas of attention, memory, executive functioning, and language. SLP involvement in cognitive rehabilitation is noted to be separate from other types of rehabilitation interventions aimed at treating aphasia and motor speech disorders that also may result from stroke and can be addressed by a SLP.
Cognitive domains addressed in cognitive-linguistic interventions include attention, memory, and executive functioning, with each domain having further sub-divisions to more specifically describe skills. Skills in attention are recognized in a hierarchy, including focused, sustained, selective, alternating, and divided attention. Deficits in visual attention, commonly observed to be a unilateral neglect, are also recognized under the domain of attention and functionally impact reading and writing. In the context of post-stroke cognitive impairments, deficits in memory are commonly observed in subcategories of verbal and nonverbal memory, short term memory or delayed recall, working memory, and prospective memory. Executive functioning refers to skills and abilities for reasoning, judgement, problem solving, sequencing, inhibition, self-monitoring, information processing, and attention to detail. 5 , 6 The combination of skills in these domains interact for completion of IADLs.
Some cognitive-communication deficits are found to be specifically related to right hemisphere damage caused by stroke or acquired brain injuries. In addition to impairments in the aforementioned areas of cognition, right hemisphere damage may demonstrate more specific impacts on macrostructure components of verbal discourse and discourse comprehension. Skills in word retrieval, syntax, grammar, and phonological processing might not be negatively impacted as commonly seen in aphasia. 5 Additional impairments specific to right hemisphere damage also include reduced insight or awareness of deficits, known as anosagnosia, and visual neglects, typically causing one to ignore stimuli in left visual field. 7
SLPs, occupational therapists (OTs), and neuropsychologists have consistent roles in initial and ongoing assessment of cognitive functioning to inform cognitive rehabilitation programs across a variety of treatment settings, such as acute or sub-acute rehabilitation facilities or therapy provided in the home, outpatient, or community-based locations. Assessment begins with screening to determine appropriate options for more specific evaluation of cognitive domains, which can include formal and informal assessment procedures to inform clinical impression of skills in functional contexts. Assessment must also recognize culturally and linguistically relevant stimuli and input from the patient, patient’s family or support person, and interprofessional team as part of comprehensive approach. 5 With all components of current skills and prior level of functioning considered, severity ratings may be provided to further describe current level of functioning or degree of impairment. Not only are descriptive terms and severity ratings essential for tracking progress, but they are also informative in planning interventions and identifying needs for support in daily activities for self-care, independent living, or return to work.
Although assessment terminology is often centralized around identifying impairments or deficits, the consensus among evidence supporting cognitive rehabilitation intends to improve overall participation in personally relevant, functional tasks. Progress is measured in generalization and carryover of skills or strategies and participation in meaningful tasks. This motive also stems from the World Health Organization International Classification of Functioning, Disability, and Health (WHO-ICF) framework, which promotes capitalizing on strengths and addressing barriers to success. 4 Cognitive rehabilitation should provide simulations of how the different domains of cognition intricately interact in activities of daily living and patient specific goals to reduce disability.
What Do Cognitive Rehabilitation Interventions Entail?
Trends in literature continue to suggest the highest evidence support for cognitive rehabilitation is demonstrated when measured in patient reported outcomes concerning participation in functional tasks versus measured performance in specific, non-IADL functions within the different cognitive domains. 8 This trend continues to reiterate the goal of participation in cognitive rehabilitation and allows for recognizing the carryover of trained strategies that ultimately may require skills in more than one domain of cognition. In keeping with principles of neuroplasticity, interventions are also recommended to be high frequency, patient-specific, meaningful, and to promote for generalization. 5 , 6 The specific domains of cognition are, however, considered in development of treatment goals and activities and may be necessary to measure progress specifically as a result of interventions.
Like other concepts of rehabilitation, interventions in cognitive rehabilitation can be classified into restorative and compensatory approaches. Restorative approaches attempt to repair or restore an impaired function. Compensatory approaches teach and carryover new strategies, skills, or accommodations to compensate for deficits when original function may not be able be fully recovered. 5 , 6 Often, family members or a support person is not only beneficial, but essential in the success in carryover of new skills or strategies. Therefore, their participation in training within treatment sessions is highly encouraged and even required prior to discharge in some situations.
Efforts to increase the evidence base for cognitive rehabilitation are ongoing because of the heterogeneity of cognitive impairments post stroke as well as the heterogeneity of participants in supporting studies. Because of this, evidence-based practice for cognitive rehabilitation for post stroke impairments may also draw upon support for cognitive rehabilitation serving individuals with acquired or traumatic brain injuries (TBI).
Direct approaches to attention in therapeutic interventions may include addressing specific levels of attention. Focused attention is the most basic level of attention, with the ability to respond to stimuli in any form, including auditory, visual or tactile. Following focused attention is sustained attention, which describes abilities to maintain attention for a duration of time. Examples of sustained attention may include reading a book, brushing teeth, or listening to a lecture. Selective attention includes completing similar activities of sustained attention, but with an additional distractor present that would require active filtering of said distraction to remain on target. Alternating attention requires abilities to shift attention between stimuli, including pausing one task, starting another task, and returning to the first task. Lastly, divided attention entails completing two tasks or responding to and processing two types of stimuli simultaneously and accurately. This is considered the highest or most complex form of attention. Examples of divided attention may include having a conversation while cooking a meal or listening to music while responding to emails. 6
Based on performance within the different levels of attention, rehabilitation therapists may generate relevant, functional tasks to target these skills within restorative and compensatory techniques. Some restorative approaches with computer-based training and Attention Process Training (APT) have been studied in isolation with gains measured in their specific types of trained tasks, however, have not found to be significant in improving functional carryover to other tasks and patient perceived performance in IADLs. 8 , 9
However, these types of interventions provided in combination with additional compensatory strategy training demonstrated the most functional and positive outcomes of attention skills in carryover measures as well within increased white matter microstructural changes and redistribution of the cerebral attention network in neuroimaging following brain injury and stroke. 8 , 10 – 12 Specific examples of direct attention training can include cancellation tasks with single or alternating targets and completing tasks within presence or absence of a variety of distractors. Compensatory strategy training begins with education of potential distractors and their impact on overall accuracy in tasks to promote awareness or understanding for attentional strategies. Specific strategies might include managing internal and external distractions or segmenting tasks into smaller steps or shorter durations. Distractions can be present via auditory or visual stimuli as well as within physical symptoms, emotions, or internal thoughts. 5 , 6 Because attention skills are required for further information processing in memory and executive functioning tasks, basic or complex attention will be assessed and addressed to further improve performance in tasks that may initially be classified with memory or executive functioning demands.
Apart from the previously described levels of attention, cognitive rehabilitation may also address unilateral visual neglects under the domain of attention. Interventions provided by SLPs will specifically target increasing awareness of unilateral neglect and attention to the neglected side within communication tasks requiring reading and writing. Some examples of intervention include providing multimodal cueing or brightly colored materials to improve response to all stimuli in targeted visual field within describing pictures, reading, providing written instructions, or completing IADL tasks. 5
Intervention for memory skills in cognitive rehabilitation typically targets delayed recall or short term memory, working memory for short term information processing, and prospective memory, recall of a planned task or action. 5 , 6 Across all forms of memory in therapy targets, both restorative and compensatory approaches are again considered. Restorative approaches within evidence-based practice for cognitive rehabilitation may include trials of spaced or distributed practice or retrieval along with errorless learning, an instructional technique in which errors are minimized or avoided prior to advancing to the next step of a task. 13 – 16 These interventions would likely initially occur in a high-intensity format in therapy sessions directed by a speech-language pathologist, but could also be trained for family members or caregivers to replicate for carryover and memory benefit outside of therapy sessions.
There is a larger body of support for training of compensatory memory strategies across all severity ranges of impairments for memory. 8 Compensatory strategy training for memory can be further divided into internal and external strategies. Internal strategies may include use of mnemonics, visualizations or imagery, associations, rehearsal, repetition, and semantic elaborations, including using additional associations with pre-existing knowledge or identifying multiple salient features of the memory target. External compensatory memory strategies entail any use of external storage of information apart from the brain with examples including calendars, to-do lists, journals, recordings, labels, pictures, alarms, timers or use of technology for prospective reminders. 5 , 6 For moderate to severe memory deficits, recommendations for intervention include emphasis on errorless learning and external memory strategies. Internal memory strategies have demonstrated increased effectiveness with more mild severity memory deficits and for those with a considerable level of cognitive reserve, because of the additional executive functioning skills required for strategy carryover. 8 Participation in a course of cognitive rehabilitation with a SLP can help select which memory interventions would be suitable for patient specific goals.
Executive Functioning
Executive functioning skills are often required for successful carryover of memory and attention strategies, however, can also be also at risk for impairment in the setting of stroke. If executive functioning impairments are severe, interventions may need to target increasing awareness to cognitive impairment and training of individual functional tasks with understanding that skill acquisition may not carryover to untrained tasks. 8 , 17 Goals to address executive functioning skills in therapy may include improving accuracy in reasoning, attention to detail, problem solving, and sequencing with tasks mimicking demands for return to independent living or work. Maximum inclusion of scenarios, stimuli, or personally relevant information is recommended to facilitate carryover of improved accuracy and strategy use outside of therapy and in real life context.
For mild to moderate severity deficits in executive functioning, evidence supports metacognitive and compensatory strategy training. 5 , 8 Metacognition is the awareness of one’s own thought processes, which may include understanding specific changes in cognitive functioning and anticipating their impact. Applying metacognitive strategies evokes a “top down” approach in evaluating and adapting performance, specifically with cognitive demands, in everyday activities. 18 The first stage of metacognitive strategy training requires awareness of potential cognitive deficits. 19 This can be facilitated in therapy sessions, but is ultimately most successful or meaningful with personally relevant experiences or tasks. Following developed awareness, training in therapy would teach strategies for executive functioning or other domains of cognition and facilitate planning carryover of strategies. The final step would be self-evaluating one’s own performance in tasks to make improvements or adjustments to performance or task execution as needed. 5 , 19 Standardized or personal rating systems can allow for clear differentiation between expected or predicted accuracy and actual performance when used before, during, and following a task. 19 For example, these rating systems may evaluate for accuracy, perceived levels of difficulty, or time required to complete a task, or whatever the goal may be to address. These rating systems can also be helpful for fostering motivation when performance and progress is tracked, and in turn, encourage continued use of self-monitoring skills for a variety of untrained tasks not specifically targeted in therapy sessions.
Other metacognitive strategy approaches include learning to modify or control the environment to allow for carryover of trained strategies to support attention, memory, and additional executive functioning skills or to reduce potential distractions, ultimately improving accuracy or reducing difficulty. 5 , 6 Some individuals significantly benefit from use of graphic organizers, time management strategies, and any strategies to increase organization in the home, with medications, in the work place, or wherever necessary. Metacognitive strategy training has been observed to be effective in acute and chronic phases of recovery post stroke when specifically trained by rehabilitation therapists. 8 , 19 The overall goal of metacognitive strategies is again to reduce the negative impact of cognitive deficits on task execution or performance and increasing independence, with hopeful reduction in disability. 18
Although less supporting evidence is available in comparison to metacognitive strategy training post stroke, dual task training has some level of support for restorative approaches to executive functioning within trained tasks. 8 , 20 , 21 However, dual task training has been more specifically studied with diagnosis of TBI. Dual task training can involve any combination of motor and cognitive tasks that are completed simultaneously. 21 The demands of dual task training also simulate similar demands of divided attention, requiring completion of two tasks, at the same time. Dual task training is often applied in other rehabilitation therapies, such as physical therapy and occupational therapy, to address gait training with anticipated distractions present at home or in the community, using simple verbal reasoning tasks completed while walking. Examples of dual task training specifically for cognitive rehabilitation may include shopping while completing calculations, discourse or conversational tasks during cooking, listening and recalling a story while working on a simple or multi-step project. Limited carryover is appreciated for training executive functioning skills to improve further carryover of visual scanning strategies to address unilateral neglect across untrained tasks. 8 , 20 This interaction continues to demonstrate the complex interaction of cognitive skills that benefit from ongoing support by rehabilitative clinicians to facilitate patient specific needs.
Advancements in technology are beginning to find their way into new modalities for cognitive rehabilitation interventions. Virtual Reality (VR) is now being explored to provide simulations of activities of daily living (ADLs) by also targeting underlying cognitive skills in information processing, executive functioning, attention, memory, and language. Their ecological validity continues to be explored, however, shows promising results when used in combination with traditional compensatory strategy training provided by rehabilitative therapists for overall participation gains in ADLs and in some standardized cognitive assessments over short periods of time. 8 , 22
Cognitive rehabilitation may also include addressing how cognitive impairments negatively impact discourse skills, commonly caused by stroke in the right hemisphere of the brain. Effective communication involves cognitive skills in sustained attention, memory, and executive functioning. Skills in these domains allow for topic recognition, response generation or thought organization, recall of communication partner’s response, and awareness of errors and revisions. 5 , 23
Interventions are structured to target both verbal and comprehension goals and would also require some degree of metacognitive training or communication partner training. Deficits in executive functioning may contribute to increased verbosity, tangentiality, impulsivity, focusing on irrelevant details, and thought disorganization in conversation. 5 , 24 A combination of cognitive deficits can also limit understanding of abstract or figurative language, including information that can be interpreted in many ways requiring mental flexibility. This further can contribute to difficulty making inferences or understanding macrostructure components of conversations, such as the over overall topic or “big picture” of discussions. 25 , 26 Further, indirect forms communication information can become more difficult to decipher, such as emotions, jokes, irony and sarcasm. 5
In guidance provided by a speech-language pathologists, these types of discourse difficulties can be addressed with functional, patient specific goals, that may also need to be informed by family members or a support person if awareness to these challenges is reduced. Recommended therapeutic tasks would break down these macrostructure components into smaller units and prompting description of how items may be related to draw or recognize an inference. Examples of stimuli used to target these goals could include discussing news stories, having complex or opinionated discussions, organizing information into pictures to tell a story, or creating outlines for planned speaking tasks. 5
The overall goals of cognitive rehabilitation in the setting of stroke are to facilitate cognitive function for participation or independence in everyday tasks, to limit the impacts or severity of disability, and to improve quality of life. These needs may evolve over time based on progress, caregiver support, or different phases of recovery after stroke. However, chronicity of stroke recovery should not discourage individuals or families from seeking guidance from rehabilitation professionals to maximize participation in activities of daily living. Individuals and their support systems can benefit from cognitive rehabilitation throughout the stages of stroke recovery if there are functional, task-specific goals related to activities of daily living along with motivation.
Copyright (c) 2023 Delaware Academy of Medicine / Delaware Public Health Association.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License ( https://creativecommons.org/licenses/by-nc-nd/4.0/ ) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Study protocol
- Open access
- Published: 27 June 2013
The effectiveness of problem solving therapy for stroke patients: study protocol for a pragmatic randomized controlled trial
- Marieke M Visser 1 , 2 ,
- Majanka H Heijenbrok-Kal 1 , 2 ,
- Adriaan van ’t Spijker 3 ,
- Gerard M Ribbers 1 , 2 &
- Jan JV Busschbach 3
BMC Neurology volume 13 , Article number: 67 ( 2013 ) Cite this article
6694 Accesses
9 Citations
2 Altmetric
Metrics details
Coping style is one of the determinants of health-related quality of life after stroke. Stroke patients make less use of active problem-oriented coping styles than other brain damaged patients. Coping styles can be influenced by means of intervention. The primary aim of this study is to investigate if Problem Solving Therapy is an effective group intervention for improving coping style and health-related quality of life in stroke patients. The secondary aim is to determine the effect of Problem Solving Therapy on depression, social participation, health care consumption, and to determine the cost-effectiveness of the intervention.
Methods/design
We strive to include 200 stroke patients in the outpatient phase of rehabilitation treatment, using a multicenter pragmatic randomized controlled trial with one year follow-up. Patients in the intervention group will receive Problem Solving Therapy in addition to the standard rehabilitation program. The intervention will be provided in an open group design, with a continuous flow of patients. Primary outcome measures are coping style and health-related quality of life. Secondary outcome measures are depression, social participation, health care consumption, and the cost-effectiveness of the intervention.
We designed our study as close to the implementation in practice as possible, using a pragmatic randomized trial and open group design, to represent a realistic estimate of the effectiveness of the intervention. If effective, Problem Solving Therapy is an inexpensive, deliverable and sustainable group intervention for stroke rehabilitation programs.
Trial registration
Nederlands Trial Register, NTR2509
Peer Review reports
Stroke is an increasing public health problem in the Netherlands: every year, 41,000 people suffer from stroke and over 3% of the total health care costs are related to the treatment of stroke and its consequences [ 1 ]. The mortality rate after stroke is 30% and is likely to decrease, which will cause an increase in morbidity [ 2 ]. Almost 50% of stroke survivors experience consequences in daily life that result in a lowered health-related quality of life (HR-QoL) [ 1 ]. The World Health Organization Quality of Life (WHOQOL) Group defines quality of life as “individuals’ perceptions of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns [ 3 ]. HR-QoL refers to the health-related aspects of quality of life. On average, utility scores of HR-QoL after stroke range from 0.47 to 0.68 (a utility score equal to death is 0.0 and full health 1.0), which is substantially lower than the value of a healthy reference population (utility score of 0.93) [ 4 , 5 ]. HR-QoL after stroke is predicted by functional constraints, age, gender, and psychosocial factors, like socioeconomic status, depression, and coping style [ 4 , 6 – 8 ]. Functional constraints, age, gender, and socioeconomic status cannot or are difficult to change, but coping style could be targeted. The question then becomes if HR-QoL after stroke could be improved through a coping style intervention. If this is possible, a secondary question would be how such improvement relates to depression, health care consumption, and costs.
A common definition of coping style is someone’s preferred way of dealing with different situations. Several coping styles can be distinguished, such as active, passive, and avoidant coping. Wolters (2010) shows that in traumatic brain-injured (TBI) patients, higher HR-QoL in the long term is predicted by an increase in active problem-focused coping style and a decrease in passive emotion-focused coping style. Unfortunately, in this population of TBI patients the active coping decreases over time, while passive coping increases [ 9 ]. This suggests that if the decrease of active coping can be stopped, there is room for improvement in HR-QoL. Stroke patients make even less use of active, problem-oriented coping styles compared to other brain damaged patients [ 10 ]. Furthermore, Darlington (2007) shows that in stroke patients, coping becomes more important in determining HR-QoL over time, while the importance of general functioning decreases [ 11 ]. This would mean that long term HR-QoL could benefit from improved coping.
Coping styles can be influenced by several interventions. Backhaus (2010) shows that an intervention aimed at changing maladaptive coping styles positively influenced psychosocial functioning of TBI patients [ 12 ]. However, HR-QoL was not measured in this study. No research is found that investigated an intervention aimed at improving HR-QoL through the change of maladaptive coping styles in stroke patients. We therefore set out to investigate whether Problem Solving Therapy (PST), which aims at active problem-focused coping, might improve HR-QoL in stroke patients. PST has been proved effective in other patient populations [ 13 , 14 ]. In stroke patients, PST has been shown successful for the prevention of post stroke depression [ 15 ]. Effects on coping style and HR-QoL have not been investigated yet.
The primary aim of this study is to investigate whether PST is an effective group intervention for improving active problem-focused coping style and HR-QoL in stroke patients. The secondary aim is to determine the effect of PST on depression, social participation, health care consumption, and the cost-effectiveness of the intervention. The effectiveness of the therapy will be investigated in an open group design, which has not been used in PST research before. PST will be added to the standard care just before the end of the rehabilitation program, as at this moment a relapse in HR-QoL is frequently observed, when patients cannot rely on their therapists anymore [ 16 ]. By teaching patients to actively cope with stressful situations, through adapting and realizing their goals, we expect that patients will use more effective coping styles, which consequently may prevent the relapse in HR-QoL, and possibly increase HR-QoL in the long term. With regard to the secondary aims of this study, we expect the incidence of depression to decrease, social participation to improve, and health care consumption to decrease, resulting in a favorable cost-effectiveness ratio for the intervention.
Study design and procedure
The effectiveness of PST for stroke patients will be evaluated in a multicenter pragmatic randomized controlled trial (RCT) with one year follow-up, with the intervention performed in the daily practice of a sub-acute outpatient stroke rehabilitation program. As such, the potential effects of the intervention have a good external validity, which allows us to calculate the cost-effectiveness of the therapy compared with standard care.
The study will be performed in Rijndam Rehabilitation Center in collaboration with Erasmus MC, both in the Netherlands, and in Ghent University Hospital in Belgium. Patients are invited by their rehabilitation physician to participate in the study. Before the start of the study, patients need to sign the informed consent form. Data will be collected at four time points by one of three research psychologists. T0 is the baseline measurement, performed within three weeks before the start of the intervention phase. T1 will be performed within ten days after the intervention phase, T2 six months and T3 twelve months after the intervention phase (Figure 1 ). The measurements will be performed in the rehabilitation center or at the patients’ home in a face-to-face interview. The study has been approved by the Medical Ethics Committee of Erasmus MC University Medical Center and the Ethics Committee of Ghent University Hospital.
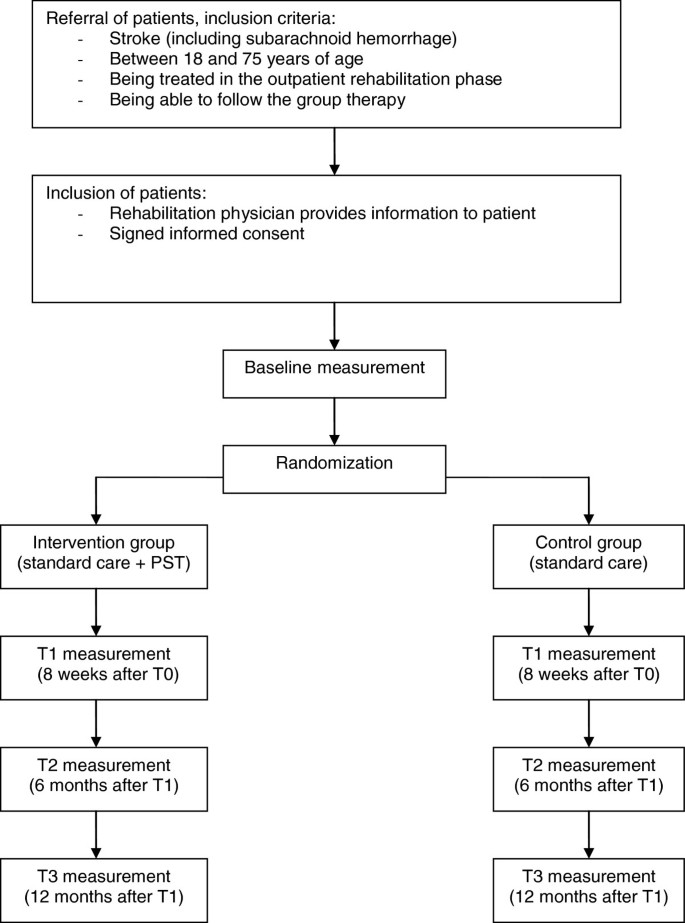
Design of the randomized controlled trial.
Study population
We strive to include 200 stroke patients. Inclusion criteria are: stroke (including subarachnoid hemorrhage), age between 18 and 75 years, being treated in the outpatient rehabilitation phase, and being able to participate in group therapy. Exclusion criteria are: progressive neurological disorders, life expectancy less than one year, insufficient understanding of the Dutch language, excessive drinking or drug abuse, subdural hematomas, moderate and severe aphasia. The same criteria would apply to the implementation of PST in practice, which stresses the pragmatic character of the trial. The inclusion of patients started March 2011 and will end August 2013. The one-year follow-up of all patients will be finished by September 2014.
Randomization
Patients are randomized to the intervention- or control condition using a stratified block randomization procedure with a block size of four. To ensure comparability between the two groups, patients are stratified per rehabilitation center. A member of the research group, who is not involved in the collection of the data, prospectively allocates the patients to the intervention- or control condition in a one-to-one ratio using an online random-number generator. To allow blinded randomization, the allocation information will be put in separate sealed envelopes which are consecutively numbered. At the end of the baseline measurement, the investigator opens the numbered envelop and informs the patient about the condition he or she is assigned to. The research psychologists who perform the baseline and follow-up measurements are blinded for treatment condition. The therapists who provide the intervention are not involved in the collection of the data. The investigator who will analyze the data is not involved in the collection of the follow-up measurements.
Intervention: problem solving therapy
Patients who are assigned to the intervention condition will receive PST in addition to the standard rehabilitation program, which will start during the last eight weeks of outpatient treatment. PST is a widely used and practical intervention method, based on a general model of coping with stress [ 17 , 18 ]. The model states that having a chronic disease causes stressful daily problems, which increase the chance of experiencing psychological stress and depressive feelings. Therefore, the aim of PST is to improve the skills to cope with the stressful daily problems in life after stroke.
The intervention will be provided in an open group design, with a continuous flow of patients, which means that patients can enter the group every week and leave the group after eight sessions (Figure 2 ). The reason for this design is that it studies group therapy in its most feasible form, where patients start and end their programs at different time-points. If we had chosen to study the effect in closed groups, many patients in the similar stage of their programs are necessary. This would only be possible if patients are admitted to large scale rehabilitation centers, which is not the rehabilitation practice in The Netherlands, or patients would have to wait for a long time before entering the group. The open group design has some disadvantages. Patients may feel unsafe when they enter an already existing group. Furthermore, a continuous flow of patients is required to keep a balanced number of patients in the group. Therefore, interventions aimed at rare diseases cannot be studied with an open group design. However, for our population of stroke patients we do expect the design to be suitable and beneficial, because these patients are frequently seen in rehabilitation treatment. An open group design has several benefits as well. Advantages for the patients are that they do not have to wait until they can start with the intervention, they can share their experiences with other ‘experienced’ stroke patients, and there is room for interaction with many fellow patients. Other advantages are that the intervention is relatively easy to organize and implement in the daily practice of the rehabilitation center. This open group design has not been investigated in PST research yet.
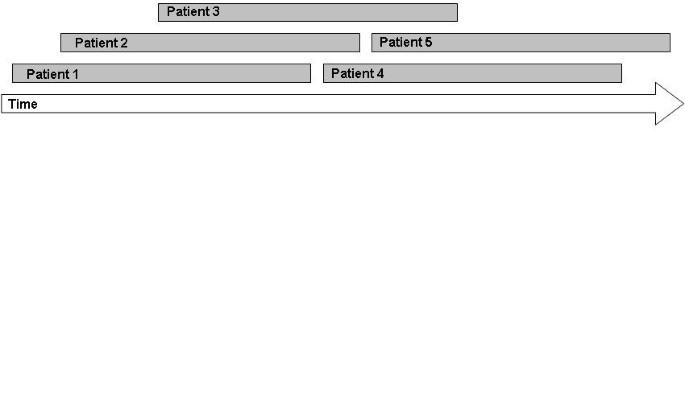
Patient flow in an open group therapy.
The intervention in this study consists of eight group sessions of 1,5 hours a week, with homework exercises after each session. The group consists of a minimum of three and a maximum of six participants. PST is provided by one to three trained neuropsychologists per rehabilitation center. Solving problems will be structured, by dividing the problem solving process in four steps:
Define problem and goal;
Generating multiple solutions;
Considering the possible consequences of the solutions systematically and select the best solution;
Implement the solution and evaluate.
Each session starts with the sharing of experiences from the past week. Then, the model of problem solving will be repeated and explained. If there are some participants who are in the group for a couple of weeks already, they will be asked to explain the model to other new participants. Subsequently, one step of the model will be highlighted every week. With emphasis on this specific step, the model will be applied to one or more examples from the participants. Finally, the participants will be asked to practice the specific step at home by making a homework assignment. During the sessions, inadequate and irrational thoughts will be challenged by common cognitive interventions. A unique aspect of the intervention is the focus on the definition of the problem in the first step of the model. A clear definition of the problem will lead to a better understanding and more solutions to it.
Control condition: standard care
Patients who are assigned to the control condition will receive the standard rehabilitation program, in order to be able to study the additional effect of the intervention to the standard rehabilitation program. This standard rehabilitation program consists of individualized amounts of treatment by a physical therapist, occupational therapist, speech therapist, psychologist, social worker, and rehabilitation physician, depending on the severity of stroke. On average, stroke patients in outpatient rehabilitation receive twelve hours of treatment a week during a nine week rehabilitation program.
Primary outcome measures are changes in task-oriented coping and psychosocial HR-QoL in patients in the intervention group in comparison with the control group. Coping style is measured using the Coping Inventory for Stressful Situations (CISS) and the short version of the Social Problem Solving Inventory-Revised (SPSI-R:SF). The CISS questionnaire consists of 48 questions and contains three subscales; Task-oriented coping, Emotion-oriented coping, and Avoidant coping. The subscale Avoidant coping consists of two subscales; Distraction and Social Diversion [ 18 , 19 ]. Because the PST aims at tasks, ‘Task-oriented coping’ is chosen as a primary endpoint; the other two subscales are used as secondary endpoints. The SPSI-R:SF questionnaire consists of ten questions about problem solving skills regarding daily situations. There are five subscales: Positive Problem Orientation, Rational Problem Solving, Negative Problem Orientation, Impulsivity/Carelessness Style, and Avoidance Style, and all are used as secondary endpoints in this trial [ 20 ].
HR-QoL is measured using the EuroQol (EQ-5D-5L) and the Stroke Specific Quality of Life Scale (SS-QoL-12). The EQ-5D is a generic questionnaire, and consists of five questions regarding mobility, self-care, daily activities, pain/complaints, mood, and a VAS scale. The five dimensions can be combined to one utility scale, representing the societal perspective of the general public [ 21 ]. The SS-QoL-12 is specifically developed for the population of stroke patients [ 22 ]. We will use the abbreviated version containing twelve items, which has been shown valid [ 23 ]. The questionnaire provides a total score and two sub scores: physical and psychosocial, of which the psychosocial sub-score is defined as the primary endpoint. The other HR-QoL scores are used as secondary endpoints.
Other secondary outcome measures are differences in depression, social participation, and health care consumption between patients in the intervention and control group. Additionally, the influence of cognitive functioning, personality characteristics, aphasia, type of stroke, side of stroke, level of functioning, and demographic characteristics on the outcomes will be assessed. Finally, the cost-effectiveness of the intervention will be calculated compared with standard care.
Depression is measured using the Center for Epidemiologic Studies Depression Scale (CES-D). This questionnaire consists of twenty items concerning depression, higher scores indicate more depressive symptoms [ 24 ].
Social participation is measured using the Impact on Participation and Autonomy (IPA). The questionnaire consists of five dimensions; Autonomy indoors, Family role, Autonomy outdoors, Social life and relationships, Work and education [ 25 ].
Health care consumption is measured using the Trimbos Questionnaire for Costs association with Psychiatric Illness (TiC-P). The questionnaire was developed for economic evaluation in mental health care, and measures health care consumption and productivity losses [ 26 ].
Sample size calculation
To determine the sample size for measuring differences between the intervention- and control group in coping style and HR-QoL, we searched for comparable effect sizes in the literature. With regard to coping style, there was no data available for this calculation. With regard to HR-QoL, Studenski (2005) measured an increase in HR-QoL after a physical therapy for stroke patients, with a long term effect size f ranging from 0.06 to 0.18 [ 27 ]. Because of the lack of more comparable data, we used this data and carefully estimated the effect size f to be 0.08. Considering the design of two groups and four repeated measurements, an expected correlation of 0.70, an alpha of 0.05, and a power of 0.80, we calculated a total required sample size of 132 patients based on the F-test. Because potential drop out is estimated at 0.30, we will strive to include 200 patients.
Statistical analyses
Demographic variables will be analyzed with an independent sample T-test for continuous variables, the Mann–Whitney U test for ordinal variables, and the chi-square test for categorical variables. Linear Mixed Models will be used to compare the repeated measurements between treatment groups, taking into account the correlation within and between subjects. We will create models for all the primary and secondary outcome variables, with time, group condition (intervention or control), and the interaction between these variables as predictors. Furthermore, we will control for variables that are accidentally not equally distributed between the two group conditions.
The cost-effectiveness of the intervention will be calculated by counting all the medical and non-medical costs, like productivity losses. The incremental cost-effectiveness ratio will be calculated by dividing the difference in total costs by the difference in quality-adjusted life years (QALYs). These QALYs will be calculated based on the EQ-5D questionnaire. The economic evaluation will be conducted according to the Dutch guidelines [ 28 ] and includes multivariate probabilistic sensitivity analyses. In the base case scenario the time horizon will be one year. If the effect is still present at one year follow up, a Markov model will be made to model a longer time horizon.
This study investigates the effect of PST on coping style and HR-QoL in stroke patients. In addition, the effect on depression, social participation, and health care consumption will be investigated, as well as the cost-effectiveness of the intervention. We will study the effectiveness of PST as close to the implementation in practice as possible, using a pragmatic trial design and an open group therapy. Any pragmatic trial has limitations; MacPherson (2004) argued that a pragmatic trial design cannot be used to determine the specific components of a treatment that caused an effect [ 29 ]. It may be possible that patients in the intervention group show improvement caused by the extra attention they receive and not so much by the assumed effective elements of the therapy; this attention effect may be considered a placebo effect. If we would like to distinguish between this ‘placebo effect’ and the effect of the specific treatment elements, the control group should have received a ‘sham therapy’. Such sham therapy would hinder the estimation of the effect of PST in practice, as in practice such additional effort would not take place. Therefore, one of the advantages of the pragmatic study design is that the external validity is better than using a sham-controlled design; the results will be generalizable to the normal rehabilitation setting [ 30 ]. The study population represents the normal stroke population in the outpatient phase of rehabilitation treatment, and the psychologists will provide the intervention to the patients just as they would do in practice. The results of a pragmatic trial are directly applicable to the usual care setting [ 31 ]. Moreover, if the intervention will prove effective, it will be easy to implement the intervention in the standard rehabilitation program, since it is already in use and the psychologists will already be trained. Other rehabilitation centers can use the therapy manual we developed.
We expect that patients who received PST will use more effective coping styles and experience a higher HR-QoL. Furthermore, we expect that patients after PST will show a decrease in depression score, an increase in social participation, and a decrease in health care consumption, which would lead to a reduction in the health care costs. We expect the intervention to be cost-effective, since the costs of the intervention are relatively low; one psychologist can train three to six patients at the same time. Darlington (2009) estimated the cost-effectiveness of an intervention aimed at coping strategies in stroke patients: the maximum costs for a single patient were 2500 euros, which will be lower if the therapy is provided in a group [ 32 ]. If PST will be proved effective for stroke patients in outpatient rehabilitation, the intervention will be an inexpensive, deliverable and sustainable group intervention that could be added to usual stroke rehabilitation programs.
Abbreviations
Center for Epidemiologic Studies Depression Scale
Coping Inventory for Stressful Situations
- Health-related quality of life
Impact on Participation and Autonomy
- Problem Solving Therapy
Quality-adjusted life years
Randomized controlled trial
Social Problem Solving Inventory-Revised
Stroke Specific Quality of Life Scale
Traumatic brain-injured
Trimbos Questionnaire for Costs association with Psychiatric Illness
World Health Organization Quality of Life.
Evers SM, Engel GL, Ament AJ: Cost of stroke in The Netherlands from a societal perspective. Stroke. 1997, 28 (7): 1375-1381. 10.1161/01.STR.28.7.1375.
Article CAS PubMed Google Scholar
Vaartjes I, van Dis I, Visseren F, Bots M: Hart- en vaatziekten in Nederland 2009, cijfers over leefstijl- en risicofactoren, ziekte en sterfte. 2009, Den Haag: Nederlandse Hartstichting
Google Scholar
Group W, Harper A, Power M: Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998, 28 (3): 551-558.
Article Google Scholar
Sturm JW, Donnan GA, Dewey HM, Macdonell RAL, Gilligan AK, Srikanth V, Thrift AG: Quality of life after stroke - The North East Melbourne Stroke Incidence Study (NEMESIS). Stroke. 2004, 35 (10): 2340-2345. 10.1161/01.STR.0000141977.18520.3b.
Article PubMed Google Scholar
Mittmann N, Trakas K, Risebrough N, Liu BA: Utility scores for chronic conditions in a community-dwelling population. Pharmaco Economics. 1999, 15 (4): 369-376. 10.2165/00019053-199915040-00004.
Article CAS Google Scholar
Paul SL, Sturm JW, Dewey HM, Donnan GA, Macdonell RAL, Thrift AG: Long-term outcome in the north east Melbourne stroke incidence study - Predictors of quality of life at 5 years after stroke. Stroke. 2005, 36 (10): 2082-2086. 10.1161/01.STR.0000183621.32045.31.
Almborg AH, Ulander K, Thulin A, Berg S: Discharged after stroke - important factors for health-related quality of life. J Clin Nursing. 2010, 19 (15–16): 2196-2206.
Patel MD, Tilling K, Lawrence E, Rudd AG, Wolfe CDA, McKevitt C: Relationships between long-term stroke disability, handicap and health-related quality of life. Age Ageing. 2006, 35 (3): 273-279. 10.1093/ageing/afj074.
Wolters G, Stapert S, Brands I, Van Heugten C: Coping styles in relation to cognitive rehabilitation and quality of life after brain injury. Neuropsychol Rehabil. 2010, 20 (4): 587-600. 10.1080/09602011003683836.
Herrmann M, Curio N, Petz T, Synowitz H, Wagner S, Bartels C, Wallesch CW: Coping with illness after brain diseases - a comparison between patients with malignant brain tumors, stroke, Parkinson's disease and traumatic brain injury. Disabil Rehabil. 2000, 22 (12): 539-546. 10.1080/096382800416788.
Darlington ASE, Dippel DWJ, Ribbers GM, van Balen R, Passchier J, Busschbach JJV: Coping strategies as determinants of quality of life in stroke patients: A longitudinal study. Cerebrovasc Dis. 2007, 23 (5–6): 401-407.
Backhaus SL, Ibarra SL, Klyce D, Trexler LE, Malec JF: Brain Injury Coping Skills Group: A Preventative Intervention for Patients With Brain Injury and Their Caregivers. Archives Physical Med Rehabil. 2010, 91 (6): 840-848. 10.1016/j.apmr.2010.03.015.
Merlijn V, Hunfeld JAM, van der Wouden JC, Hazebroek-Kampschreur A, van Suijlekom-Smit LWA, Koes BW, Passchier J: A cognitive-behavioural program for adolescents with chronic pain - a pilot study. Patient Educ Counseling. 2005, 59 (2): 126-134. 10.1016/j.pec.2004.10.010.
Hopko DR, Armento MEA, Robertson SMC, Ryba MM, Carvalho JP, Colman LK, Mullane C, Gawrysiak M, Bell JL, McNulty JK, et al: Brief Behavioral Activation and Problem-Solving Therapy for Depressed Breast Cancer Patients: Randomized Trial. J Consult Clin Psychol. 2011, 79 (6): 834-849.
Robinson RG, Jorge RE, Moser DJ, Acion L, Solodkin A, Small SL, Fonzetti P, Hegel M, Arndt S: Escitalopram and problem-solving therapy for prevention of poststroke depression - A randomized controlled trial. Jama-Journal The Am Med Assoc. 2008, 299 (20): 2391-2400. 10.1001/jama.299.20.2391.
Ch'ng AM, French D, McLean N: Coping with the Challenges of Recovery from Stroke Long Term Perspectives of Stroke Support Group Members. J Health Psychology. 2008, 13 (8): 1136-1146. 10.1177/1359105308095967.
Nezu AM, Perri MG, Nezu CM, Berking M: Problem-solving therapy for depression: theory, research, and clinical guidelines. 1989, New York: Wiley
Nezu AM, Nezu CM: Problem Solving Therapy. J Psychother Integr. 2001, 11 (2): 187-205. 10.1023/A:1016653407338.
Endler NS, Parker JDA: Coping inventory for stressful situations (CISS) manual. 1990, Toronto: Multi-Health Systems
Hawkins D, Sofronoff K, Sheffield J: Psychometric Properties of the Social Problem Solving Inventory-Revised Short-Form: Is the Short Form a Valid and Reliable Measure for Young Adults?. Cognitive Therapy Res. 2009, 33 (5): 462-470. 10.1007/s10608-008-9209-7.
Lamers LM, McDonnell J, Stalmeier PF, Krabbe PF, Busschbach JJ: The Dutch tariff: results and arguments for an effective design for national EQ-5D valuation studies. Health Econ. 2006, 15 (10): 1121-1132. 10.1002/hec.1124.
Williams LS, Weinberger M, Harris LE, Clark DO, Biller J: Development of a stroke-specific quality of life scale. Stroke. 1999, 30 (7): 1362-1369. 10.1161/01.STR.30.7.1362.
Post MWM, Boosman H, van Zandvoort MM, Passier P, Rinkel GJE, Visser-Meily JMA: Development and validation of a short version of the Stroke Specific Quality of Life Scale. J Neurol Neurosurg Psychiatry. 2011, 82 (3): 283-286. 10.1136/jnnp.2009.196394.
Radloff LS: The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977, 1: 385-401. 10.1177/014662167700100306.
Cardol M, de Haan RJ, de Jong BA, van den Bos GAM, de Groot IJM: Psychometric properties of the impact on participation and autonomy questionnaire. Arch Physical Med Rehabil. 2001, 82 (2): 210-216. 10.1053/apmr.2001.18218.
Hakkaart-Van Roijen L: Trimbos/iMTA questionnaire for Costs associated with Psychiatric Illness (TiC-P). Manual. September 2010, Rotterdam: Erasmus University Rotterdam
Studenski S, Duncan PW, Perera S, Reker D, Lai SM, Richards L: Daily functioning and quality of life in a randomized controlled trial of therapeutic exercise for subacute stroke survivors. Stroke. 2005, 36 (8): 1764-1770. 10.1161/01.STR.0000174192.87887.70.
Oosterbrink JB, Bouwmans CAM, Koopmanschap MA, Rutten FFH: Handleiding voor kostenonderzoek, methoden en standaard kostprijzen voor economische evaluaties in de gezondheidszorg. 2004, Diemen: College voor zorgverzekeringen
Macpherson H: Pragmatic clinical trials. Complement Ther Med. 2004, 12 (2–3): 136-140.
Tunis SR, Stryer DB, Clancy CM: Practical clinical trials - Increasing the value of clinical research for decision making in clinical and health policy. Jama-Journal Am Med Assoc. 2003, 290 (12): 1624-1632. 10.1001/jama.290.12.1624.
Zwarenstein M, Treweek S, Gagnier JJ, Altman DG, Tunis S, Haynes B, Oxman AD, Moher D: Improving the reporting of pragmatic trials: an extension of the CONSORT statement. BMJ. 2008, 337: a2390-10.1136/bmj.a2390.
Article PubMed PubMed Central Google Scholar
Darlington ASE, Dippel DWJ, Ribbers GM, van Balen R, Passchier J, Busschbach JJV: A Prospective Study On Coping Strategies And Quality Of Life In Patients After Stroke, Assessing Prognostic Relationships And Estimates Of Cost-Effectiveness. J Rehabil Med. 2009, 41 (4): 237-241. 10.2340/16501977-0313.
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1471-2377/13/67/prepub
Download references
Acknowledgements
This study is funded by the National Initiative Brain and Cognition (NIHC 056-11-010), Stichting Coolsingel, and Erasmus MC Cost-Effectiveness Research.
Author information
Authors and affiliations.
Department of Rehabilitation Medicine, Erasmus MC, University Medical Center Rotterdam, PO Box 2040, 3000, CA, Rotterdam, The Netherlands
Marieke M Visser, Majanka H Heijenbrok-Kal & Gerard M Ribbers
Rijndam Rehabilitation Center, PO Box 23181, 3001, KD, Rotterdam, The Netherlands
Department of Psychiatry, Erasmus MC, University Medical Center Rotterdam, Section Medical Psychology and Psychotherapy, PO Box 2040, 3000, CA, Rotterdam, The Netherlands
Adriaan van ’t Spijker & Jan JV Busschbach
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Marieke M Visser .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
All authors contributed to the development of the study protocol. AvtS adapted the PST-manual for the population of stroke patients. MMV implemented the therapy in the rehabilitation program. All authors read and corrected the draft version of this manuscript, and approved the final version.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Visser, M.M., Heijenbrok-Kal, M.H., van ’t Spijker, A. et al. The effectiveness of problem solving therapy for stroke patients: study protocol for a pragmatic randomized controlled trial. BMC Neurol 13 , 67 (2013). https://doi.org/10.1186/1471-2377-13-67
Download citation
Received : 23 April 2013
Accepted : 20 June 2013
Published : 27 June 2013
DOI : https://doi.org/10.1186/1471-2377-13-67
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Rehabilitation
- Coping style
BMC Neurology
ISSN: 1471-2377
- General enquiries: [email protected]
Effect of a telephone and web-based problem-solving intervention for stroke caregivers on stroke patient activities of daily living: A randomized controlled trial
Affiliations.
- 1 Research Service, North Florida/South Georgia Veterans Health System, Gainesville, FL, USA.
- 2 Department of Anthropology, College of Liberal Arts and Sciences, University of Florida, Gainesville, FL, USA.
- 3 Department of Health Outcomes and Biomedical Informatics, College of Medicine, University of Florida, Gainesville, FL, USA.
- 4 Geriatric Research Education and Clinical Center, North Florida/South Georgia Veterans Health System, Gainesville, FL, USA.
- 5 Department of Aging & Geriatrics, College of Medicine, University of Florida, Gainesville, FL, USA.
- PMID: 36847253
- DOI: 10.1177/02692155231157301
Objective: To test for effects of a problem-solving intervention for stroke caregivers on stroke survivor activities of daily living.
Design: Two-arm parallel randomized clinical trial with repeated measures at 11 weeks and 19 weeks.
Setting: Medical centers for US military Veterans.
Subjects: Caregivers of stroke survivors.
Intervention: A registered nurse guided caregivers in using problem-solving strategies emphasizing creative thinking, optimism, planning, and expert information to address challenges associated with caregiving. Caregivers in the intervention completed one telephone orientation session followed by eight online, asynchronous messaging center sessions. The messaging center sessions involved (a) education on the Resources and Education for Stroke Caregivers' Understanding and Empowerment website (https://www.stroke.cindrr.research.va.gov/en/), (b) supportive communication between the nurse and caregiver, (c) nurse and caregiver interactions to improve problem-solving, and (d) maintain adherence to discharge planning instructions.
Main outcome: The Barthel Index was used to measure activities of daily living.
Results: 174 participants (standard care n = 88, intervention n = 86) were enrolled at baseline. There were no significant differences between groups at baseline. Change scores in activities of daily living between baseline and 11 weeks were significantly higher in the intervention group than the standard care group (group difference = 6.43, 95% confidence interval: 1.28, 11.58). Group differences in change scores between baseline and 19 weeks were not statistically significant (group difference = 3.89, 95% confidence interval: -3.58, 11.36).
Conclusions: This web-based caregiver intervention improved stroke survivor activities of daily living by 11 weeks, but intervention effects were undetectable after 19 weeks.
Keywords: Stroke; activities of daily living; caregiver; caregiver intervention; rehabilitation.
Publication types
- Randomized Controlled Trial
- Activities of Daily Living
- Caregivers / education
- Quality of Life
- Stroke Rehabilitation*
- Stroke* / complications
- Stroke* / diagnosis
Grants and funding
- I01 HX000834/HX/HSRD VA/United States

IMAGES
VIDEO
COMMENTS
More than half of all stroke survivors experience a post-stroke cognitive impairment. This may affect many functions, including memory, problem solving skills, and the ability to think clearly, among others. However, survivors can often improve their mental aptitude by practicing cognitive exercises for stroke patients.
35 Fun Activities for Stroke Patients. Board and Card Games. 1. Scrabble. Scrabble involves a variety of skills that stroke survivors can work on. Adding up the scores uses simple math, coming up with words requires cognitive flexibility, and the mechanics of the game involve simple grasp-and-release tasks. 2.
same. More than two-thirds of stroke survivors receive rehabilitation services after leaving the hospital. Effective rehabilitation is an essential part of stroke care. Stroke rehabilitation requires a sustainable and coordinated effort from a team with the patient and the patient's goals at the center. In addition to the patient, the team ...
Your rehabilitation plan will depend on the part of the body or type of ability affected by your stroke. Physical activities might include: Motor-skill exercises. Exercises can help improve muscle strength and coordination throughout the body. These can include muscles used for balance, walking and even swallowing.
5.4.6 Activities of Daily Living .....17 5.4.7 Neuropsychological Testing .....17 5.5 Management for Vascular Cognitive ... Some form of cognitive impairment is observed in 40-70% of stroke patients (Godefroy et al. 2011). At three months, 1, 2 and 3 years post stroke, the prevalence rates of ... •Initiation, processing speed, problem solving ...
Many other thinking processes happen without us being aware of them, known as automatic processes. Together, many of these automatic processes are known as executive function. Executive function is about planning and problem-solving. It includes all the things that allow us to organise, make decisions and know when we need to do something.
Life After Stroke: Our Path Forward. There is life — and hope — after stroke. With time, new routines will become second nature. Rehabilitation can build your strength, capability and confidence. It can help you continue your daily activities despite the effects of your stroke. Life After Stroke Guide for Patients and Caregivers (PDF)
The following are some games that are helpful in stroke recovery cognitive exercises. Lumosity: This brain training app offers a variety of games designed to improve memory, attention, and problem-solving skills. Games like "Train of Thought" and "Memory Matrix" are particularly effective for cognitive exercise.
This read is likely to motivate the patients and also facilitate developing problem-solving skills in a realistic and relevant setting, the home. Problem solving is emerging as a component of developing healthy coping strategies for people post stroke. 40. Why else might home rehabilitation work?
About the Guidebook and Developer. This guidebook is an update of UAB Home Stimulation Program, a booklet originally developed in 2002 by Tom Novack, PhD, ABPP and Jacqueline Blankenship, MCD, CCC‐SLP. This update is made by Tom Novack, PhD, ABPP, Sean Hollis, PhD, Erin Brownlee, OTR/L, Meredith Allan PT, DPT, NCS, Lyndsey M. Holcombe, MS ...
Games help to improve a variety of skills that may have been affected by the stroke, including: Motor function: ability to move their body voluntarily. Cognitive function: memory, learning, attention, decision making and language abilities. Social interaction: conversations verbal or nonverbal. Games can help to reduce stress and anxiety and ...
The top 10 Constant Therapy exercises assigned by clinicians to patients recovering from stroke. 1. Follow instructions you hear: Works on auditory memory and auditory comprehension through following directions. Individuals Assigned: 10,207. Percent of Users Identified As Recovering from Stroke 56%.
Recovery activities for stroke patients. In addition to direct therapy at medical and rehabilitation centers, patients should beware of becoming isolated and try to engage in a handful of home-based and social activities throughout the week. ... The idea is to work your reasoning, comprehension and problem solving skills. Meditation and ...
10. Chinese Checkers. Chinese checkers can be a little bit harder for traumatic brain injury patients, because you're playing against more than one opponent. The goal of the game is to move all your pegs to the opposite side before the other players. You can only move one peg at a time, so plan carefully!
Following stroke, many people experience difficulties in arousal, attention, concentration, memory, perception, problem solving, decision making, insight and other areas of cognition that impede their ability to function in everyday activities. Cognitive abilities and disabilities must be considered in addressing all areas of functioning including communication, mobility, self-care, social ...
The PST intervention consisted of 8 group sessions of 1.5 hours a week, with additional homework exercises. Each group consisted of 3 to 6 participants and was provided by a trained neuropsychologist. ... The effectiveness of problem solving therapy for stroke patients: study protocol for a pragmatic randomized controlled trial. BMC Neurol ...
The primary aim of this study is to investigate if Problem Solving Therapy is an effective group intervention for improving coping style and health-related quality of life in stroke patients. The secondary aim is to determine the effect of Problem Solving Therapy on depression, social participation, health care consumption, and to determine the ...
As of 2023, stroke continues to be one of leading causes of significant long-term disability in the United States. 1 Cognitive deficits are a common component of post-stroke sequala, limiting or impacting participation in functional activities of daily living. In addition to having substantial impacts on the individual diagnosed with stroke, family members, caregivers, and society also absorb ...
Coping style is one of the determinants of health-related quality of life after stroke. Stroke patients make less use of active problem-oriented coping styles than other brain damaged patients. Coping styles can be influenced by means of intervention. The primary aim of this study is to investigate if Problem Solving Therapy is an effective group intervention for improving coping style and ...
Objective: To test for effects of a problem-solving intervention for stroke caregivers on stroke survivor activities of daily living. Design: Two-arm parallel randomized clinical trial with repeated measures at 11 weeks and 19 weeks. Setting: Medical centers for US military Veterans. Subjects: Caregivers of stroke survivors.