An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Springer Nature - PMC COVID-19 Collection


HIV/AIDS: Current Updates on the Disease, Treatment and Prevention
Praveen kumar gupta.
Department of Biotechnology, R.V College of Engineering, Bangalore, 560059 India
Apoorva Saxena
CCR5-delta 32 homozygous stem cell transplantation for HIV-infected individuals is being treated as a milestone in the global AIDS epidemic. Since 2008, when the second Berlin patient was cured from HIV after undergoing transplantation from a donor with delta-32 mutation, scientists are aiming for a long-term cure for the wider population. In 2019, a London patient became the second person to be free of HIV and came off the antiretroviral drugs completely. CCR5 gene is now being treated as a viable target for HIV treatment. It can be used in the treatment of HIV either through administration of drugs that bind to CCR5 and stop the receptor from working or through gene therapy to alter the CCR5 gene using CRISPR/Cas9 and prevent protein production. This review article aims to identify the obstacles and the need to overcome them in order to bridge the gap between current research and future potential cures for HIV.
Introduction
Human immunodeficiency virus or HIV is the cause of HIV infection that leads to the autoimmune disorder acquired immune deficiency syndrome (AIDS) [ 1 ] (Fig. 1 ). The major cause of spreading of HIV is through unprotected sex, during pregnancy from mother to foetus, through contaminated hypodermic needles and infected blood transfusions [ 1 ]. In the year 2016, an estimated 37 million people were living with HIV and 1 million deaths were reported. HIV/AIDS is a pandemic condition—an epidemic of diseases that spreads across large areas like multiple continents or even worldwide [ 1 ]. The first time AIDS was recognized was in the year 1981 by the United States Center for Disease Control and Prevention (CDC). Since the reported case of an individual who had successfully undergone a stem cell transplant from a person who showed a homozygous CCR5-delta 32 mutation, after receiving extensive high dose chemotherapy, there has been a greater interest in finding a potential cure.

Human Immunodeficiency Virus [ 5 ]
HIV is a type of retrovirus that adversely infects the immune system of a human, mainly targeting the CD4 + T-helper cells, accessory cells and the macrophages [ 2 ]. When it gains entry into the target cell, the viral genomic RNA undergoes a process of the reverse transcription with the help of reverse transcriptase enzyme and forms double stranded DNA (ds-DNA). This ds-DNA then gets integrated into the target cellular DNA with the help of enzyme integrase and other host co-factors [ 3 ]. The virus now can either become dormant or conceal itself and the target cell detection by the host immune system or it can get transcribed into new viral RNA and proteins that are released from the cell and begin the cycle again. HIV can be characterized into 2 major classes—HIV-1 and HIV-2. HIV-1, which is more virulent, infective and the major cause of HIV in humans, was discovered first and was initially referred to as HTLV-III or LAV [ 4 ] (Fig. 2 ). HIV-2 is less infective and far fewer people exposed to it are infected.

Structure of HIV-1 [ 8 ]
The crucial factor in gaining entry into target cell is through binding of HIV to the CD4 receptor present on the T-helper cells and to one of the chemokine receptors- either CCR5 or CXCR4 [ 6 , 7 ]. Binding to the co-receptor depends on the virus’s tropism which is the ability to bind to a specific receptor. Naturally, there are two types of tropic strains—R5 that bind to CCR5 and X4 which bind to CXCR4. Dual tropic strains are capable of binding to both. Of these two co-receptors, CCR5 is the prime receptor for virus’s entry into the target cell. R5-tropic strains prevail during early stages of infection, whereas the X4-tropic strains emerge later with disease progression. The envelope-like glycoprotein structure of HIV-1 is paramount in ensuring the viral entry into a target host cell [ 7 ]. This glycoprotein has 2 protein subunits: the gp41 (transmembrane) subunit and gp120 (external) subunit, which mimics a chemokine [ 6 , 7 ]. It does not manifest the unique structure of the chemokine but somehow manages to bind to both the co-receptors [ 6 ]. It forms a heterotrimeric complex wherein the gp120 subunit binds to the CD4 protein and specific co-receptor present on the target cell [ 6 ]. When this complex is formed, it triggers the release of a peptide which facilitates cell–cell fusion, that causes the viral membrane to fuse with the target cell membrane [ 6 ]. Binding to CD4 alone is not sufficient as it can result in gp120 shedding. So, it has to bind to the specific co-receptor for the fusion to proceed. The V1–V2 region of gp120 is recognized by the co-receptor, that influences which co-receptor will bind to the protein and is determined by degree of N-linked glycosylation and peptide composition. The highly variable V3 loop is the one that determines co-receptor specificity. The binding of gp120 glycoprotein to the CCR5 co-receptor is determined by two essential factors—the tyrosine-sulphated amino terminus of CCR5 receptor and following which there must be reciprocal action between the transmembrane domains of CCR5 and gp120 protein, i.e., inter-communication and synergy.
Antiretroviral Therapy
The usage of a combination of three or more antiretroviral drugs for suppression of the HIV infection is called antiretroviral therapy. Using multiple drugs in combination to increase the effectivity on various viral targets is called highly active antiretroviral therapy (HAART). It helps in maintaining the immune system to function, preventing HIV from developing resistance and other infections that potentially lead to death. The five classes of drugs used in combination to treat HIV infection are: entry inhibitors, nucleoside/nucleotide reverse transcriptase inhibitors, non-nucleoside reverse transcriptase inhibitors, integrase inhibitors and protease inhibitors.
Zidovudine/ZVD (also called azidothymidine) is an extensively used antiretroviral medication [ 9 ]. It is a thymidine analogue and is dosed twice daily in combination with other antiretrovirals. Its function is to particularly inhibit the reverse transcriptase enzyme which is necessary for the production of ds-DNA.
Cellular enzymes are used in converting AZT into the 5′-triphosphate form. Research studies suggest that the termination of forming ds-DNA chains is a crucial factor that leads to an inhibitory effect.
Studies have also shown that at very high dosage of this drug, its triphosphate form may inhibit the DNA polymerase enzyme which is used for cell division by the uninfected cells and mitochondria for replication. It may lead to toxic but reversible effects on certain skeletal and the cardiac muscles, causing the condition of myositis [ 10 ]. However, zidovudine also shows greater affinity for the reverse transcriptase enzyme, which is around 100-fold. This selectivity has been proven by the cell's ability to quickly repair its DNA strands if broken by AZT during its formation, whereas the HIV virus will lack this ability (Fig. 3 ).

Structure of zidovudine [ 11 ]
Zidovudine is commonly used in combination with nucleotide reverse transcriptase inhibitor, non-nucleoside reverse transcriptase inhibitor, HIV integrase strand transfer inhibitor and protease inhibitor [ 9 ]. The combination of lamivudine and zidovudine is not recommended for non-pregnant HIV-infected adults and adolescents due to greater toxicity but is used as an alternative, though not a preferred one, in antiretroviral-naive pregnant women as an initial treatment [ 9 ]. However, for paediatric patients (neonates, infants and children of age 12 or less), zidovudine with lamivudine/emtricitabine is a preferred option. For adolescents greater than the age of 12, it is an alternative [ 9 ].
Zidovudine Administration and Pharmacokinetics
Administration and dosage.
It is usually administered orally or by continuous IV infusion, although not rapid infusion and IM injection [ 9 ] (Tables (Tables1, 1 , ,2). 2 ). The dosage for paediatric patients and adult patients depends on their body weight (Tables (Tables3, 3 , ,4 4 ).
Oral administration [ 9 ]
IV administration [ 9 ]
Dosage for paediatric patients [ 9 ]
Dosage for adult patients [ 9 ]
Administration
Zidovudine: 1 mg/kg every 4 h [ 9 ].
Pharmacokinetics
Pharmacokinetics gives a detailed view of the fate of drugs in the human system. It includes various components like absorption, distribution, excretion or elimination and metabolism (Tables (Tables5, 5 , ,6, 6 , ,7). 7 ). The stability of such retroviral drugs should also be taken into account for both oral and parenteral dosage forms (Table (Table8 8 ).
Absorption [ 9 ]
Distribution [ 9 ]
Elimination process [ 9 ]
Stability of antiretrovirals [ 9 ]
Contraindications [ 9 ]
- Zidovudine has a history of life-threatening hypersensitivity reactions like Stevens–Johnson syndrome and anaphylaxis to the drug or maybe due to some ingredient in the formulation.
- Lamivudine/zidovudine: hypersensitivity history.
- Abacavir/zidovudine/lamivudine: history of hypersensitivity to abacavir, zidovudine or lamivudine; hepatic impairments may be mild or severe.
CCR5 Gene Structure
C–C chemokine receptor type 5 (also called CCR5 or CD195) is a receptor for chemokines present on the white blood cells. The CCR5 gene in humans is located on the short arm (p) at position 21 on chromosome number 3 (Fig. 4 ). It is mainly expressed cells like T-cells, macrophages, microglia, dendritic cells and eosinophils and is found within a cluster of genes coding for some other receptors like XCR1, CCBP2, etc. [ 12 , 13 ]. The gene has two promoters, three exons and two introns. Pu or PR2, the upstream promoter, has a 1.9 kb region, 57 bp in length and precedes the exon 1 [ 12 ]. Exon 1, which is the start of the coding region, is followed by the first intron, 501 bp in length. The second exon 2 is intron-less. It is found as exon 2a, 235 bp in length, and exon 2b, 54 bp in length. Pd or PR1, the second promoter, accommodates the intron 1 and exon 2 regions [ 12 ]. A 1.9 kb length intron is located between exon 2 and exon 3. Exon 3 is also intron-less and consists of the full ORF of the CCR5 gene, 11 bp of the 5′ untranslated regions and the complete 3′ untranslated regions [ 12 ].

Location of CCR5 gene on chromosome 21 [ 14 ]
These two promoters are devoid of the consensus TATA and CCAAT sequences, although the Pd promoter has a non-consensus TATA sequence and have an unusually high content of pyrimidine in them [ 12 ]. The upstream Pu promoter was found to be weaker than the downstream Pd promoter which had exhibited up to fivefold greater activity. But these results were established as erroneous [ 13 ]. With the help of RT-PCR technique, it was later identified that the Pu promoter was used in stimulated T-cells and the Pd promoter was used in unstimulated primary T-cells [ 13 ]. The error resulted due to the use of transformed T-cells affecting the overall expression of CCR5 protein via the Pu promoter [ 13 ]. Results also showed that transcription of the CCR5 gene when controlled by the Pu promoter containing exon 1 resulted in CCR5A or B and when controlled by the Pd promoter resulted in truncated isoforms [ 13 ].
CCR5 Gene Expression Regulation
The expression of CCR5 gene is regulated at three levels: 1. genetic factors, 2. factors involved in activation, signalling and trafficking of the receptor which includes desensitization, internalization and recycling and 3. environmental triggers [ 13 ].
CCR5 receptor is part of the G-protein coupled receptor family, which binds to its ligand and releases αi and βγ G-protein subunits. This results in a mediated effector response. Such responses stimulate the release of phospholipase Cβ and adenylyl cyclase. This in turn facilitates the release of intracellular calcium and form inositol triphosphate [ 13 ]. This leads to activation of phosphorylation of the CCR5 receptor which occurs at the serine and C-terminal residues via protein kinase C and G-protein coupled receptor kinases [ 13 ]. The regulatory proteins, β-arrestin 1 and 2, bind to the activated serine and the conserved DRY motif in the intracellular loop [ 13 ]. The β-arrestin proteins have functions like desensitizing the receptor to further stimulation and participating in endocytosis. The CCR5 expression level is controlled by the rates of recycling and endocytosis [ 13 ]. In the endocytosis process, β-arrestin protein facilitates the binding process between clathrin-coated pits and the phosphorylated receptor. Infection and entry of HIV into cells do not require CCR5 signalling, but the chemokine-induced endocytosis decreases the available receptor for HIV entry. This is the process of chemokine-mediated anti-HIV activity [ 13 ].
Environmental factors affecting CCR5 expression are infectious pathogenic agents like Mycobacterium tuberculosis , which increases the CCR5 expression. Studies have shown that CCR5 expression is considerably increased in all leukocyte subset cells during tuberculosis and dual infection with HIV [ 13 ]. However, the level of CCR5 expression on CD4 + T-cells was not increased. Conversely, it was also shown that HIV affects the level of expression of CCR5, due to a correlation with HIV disease progression. Individuals with end stage HIV were shown to have the highest percentages of CCR5 expressing CD4 + T-cells [ 13 ].
The regulation of CCR5 is complex. The introns as well as sequences in the 5′ UTR and 3′ UTR affect CCR5 gene regulation [ 13 ]. Therefore, mutations in these regions should be considered critical in the regulation process.
CCR5-Delta 32 Mutation
The discovery of CCR5-delta 32 mutation in the CCR5 gene in 1996 which exhibited some protection against HIV was a ground breaking one. Studies showed that the CD4 + T-cells when expressing this mutation prevented HIV envelope fusion [ 12 ] (Fig. 5 ). The mutant allele has a length of 215 in comparison to the wild type which contains 352 amino acid residues [ 13 ]. This mutation basically results due to the deletion of 32 base pairs from the position of nucleotides starting from 794 till 825, a frameshift mutation, and seven new amino acids are incorporated between amino acid 174 and stop codon at amino acid 182 [ 13 ] (Fig. 6 ). This mutation affects the region of second extracellular loop where the resultant protein lacked the last three transmembrane domains and also some regions necessary for G-protein interaction and signal transduction.

Comparison of HIV infecting cell with CCR5 and without CCR5 [ 15 ]

Difference between wild type CCR5 and CCR5-delta 32 [ 16 ]
This mutation is majorly restricted to people of European descent. The gene frequencies are found to be around 10% and shows a decline from north to south latitude. A 2–5% gene frequency in Europe, the Middle East and parts of the Indian subcontinent was observed in more than 3000 individuals. The highest frequency, at 20.93%, was discovered in the Ashkenazi Jewish population. The mutant allele is absent in Black populations excluding the African American group who may have acquired the mutation through genetic admixture [ 13 ].
The origin of the delta-32 mutant allele has been dated back to the year 275–1875, which increased over a period of time as a result of selective pressure, mainly the Black plague. However, historical data have shown that Black plague may not in fact be the cause [ 13 ]. The distribution of the delta-32 mutant allele in a north to south gradient does not correlate to the casualties of the plague and instead follows a south to the north gradient. The Black plague has shown the greatest casualties in areas like the Mediterranean region and China, with lowest allele frequencies of the mutation [ 13 ].
Studies suggested that delta-32 arose without a selective event. Tandem repeats found in the coding region of the CCR5 gene could cause unequal homologous recombination, which results in the delta-32 allele. The origins of the delta-32 mutation, however, remain a mystery [ 13 ].
The hype about the delta-32 mutation comes from its ability to protect homozygous individuals from HIV. The protective effect of the delta-32 mutation is a result of eliminating the expression of CCR5 protein on the cell surface, which prevents HIV’s entry into the cell. In the year 1997, however, studies showed that some of them having the homozygous delta-32 mutation were HIV-infected [ 13 ]. Further studies revealed the HIV virus was of the X4 type, which led to very rapid CD4 + T cell decline. Hence, this mutation is limited in its function and does not protect against viral strains which utilize other receptors or show dual-tropism [ 13 ].
In contrast, however, the delta-32 protein product which is localized to the endoplasmic reticulum is an important factor. It is shown to exert a trans-dominant negative effect on the wild-type CCR5 protein, which inhibits its transport to the cell surface. Further analysis in vitro showed the reduction of surface expression of wild type CCR5 and CXCR4 through dimerization by this mutant protein product [ 13 ]. This confers an inhibition to R5, X4 and R5X4 HIV infections [ 13 ]. Homozygous delta-32 individuals with this mutant protein were shown to have suppressed CXCR4 surface protein expression and decreased susceptibility to X4 infection. Experimental proofs also suggested that delta-32 heterozygous individuals with HIV infection do not stably express the mutant protein, are devoid of the molecular mechanism of complete protection and only maybe partially protected [ 13 ].
Stem Cell Transplantation
Stem cells are undifferentiated cells that can differentiate into specialized cells and can also undergo mitosis to produce more stem cells. There are mainly two classes—embryonic stem cells (ECS) and adult stem cells. Stem cells are also taken from the umbilical cord blood just after birth. These act as a repair mechanism for the body, such as skin, blood or intestinal tissues. Adult stem cells are majorly used in medical therapies like bone marrow transplantation. Bone marrow is the spongy tissue present inside the bones which serves as a rich source of adult stem cells. Long-term control of HIV is possible with CCR5-delta 32 stem cell transplantation [ 13 ].
Allogeneic transplantation of stem cells with this mutation in patients with HIV infection and malignancy has been considered as an option since the late 1990s (Fig. 7 ). Human leukocyte antigen (HLA) is a critical factor to be considered during the process of transplantation. The HLA should be a proper match; otherwise, it would lead to rejection by the recipient’s immune system. The limited availability of HLA-matched unrelated donors has made it even more difficult. Only about 1% of Caucasians possess this CCR5 null allele [ 13 ].

Allogeneic hematopoietic stem cell transplant [ 17 ]
Gene Therapy
Zinc finger nuclease technology is a popular tool which can be used for targeting specific DNA sequences in the genome. It falls in the class of restriction enzymes and is artificially made by fusing a zinc finger DNA-binding domain and DNA-cleavage domain. This technique is also engineered to eliminate the CCR5 expression over CD4 + T-cells, and the modified cells have shown to have a half-life of 48 weeks [ 13 ]. But it has its own issues. It is difficult to ensure that the desired repair mechanism is one which is used to repair the double stranded break (DBS) [ 13 ]. It is also challenging to scale it upwards and is an expensive technique.
A breakthrough technique, the CRISPR/Cas9 gene-editing system, is also used to eliminate the CCR5 receptor on the blood stem cells which can give rise to differentiated blood cells that are devoid of this receptor [ 18 ] (Fig. 8 ). These gene-edited stem cells can be established into an HIV-infected patient through bone marrow transplantation and give rise to an HIV-resistant immune system [ 18 ]. This technique, however, can also go sideways which leads to unwanted results that can cause ethical issues to rise. As seen in the highly controversial case of the Chinese scientist, He Jiankui, who with the help of this technology deleted the CCR5 gene in the twins, Lulu and Nana, introduced some unintended mutations in their genetic codes. There is still a lot of research needed to make this technology bioethically a safe tool.

CRISPR/Cas9 gene editing [ 19 ]
Researchers have also engineered a molecule called the chimeric antigen receptor (CAR) and introduced a gene for that molecule into blood-forming stem cells [ 18 ]. This molecule has two receptors that will recognize the antigen (HIV) and direct the immune cells to locate and kill the HIV-infected cells [ 18 ]. When transplanted into mice, which would have the CAR-carrying blood stem cells, it would result in reduced levels of HIV by inducing the immune cells to fight effectively against the virus [ 18 ]. An 80% to 95% drop in viral load was observed in the mice [ 18 ]. It was concluded that gene therapy could be a feasible option for treatment in HIV-positive humans.
Immunological Approaches
Studies have shown that vaccine can contribute effectively in viral clearance such as the Rhesus CMV vaccine vector [ 18 ]. A vaccine vector is a kind of vaccine which consists of chemically weakened viruses that are transported in the body to generate an immune response. The genes used in these vaccines are antigen coding surface proteins from that particular pathogen.
SAV001-H is the first and only preventive HIV vaccine which uses killed HIV-1 virus [ 18 ]. It is unique from other vaccines, as it uses genetically engineered whole virus genome, eliminating its pathogenicity and inactivating its virulence through irradiation and chemical treatments, finally approaching to the first “whole-killed virus”-based HIV vaccine [ 18 ]. The results of Phase 1 clinical trial, which were completed in the year 2013, were found to have serious and adverse effects in the 33 participants [ 18 ]. There was also a surprising boost in the antibody production against p24 and gp120. The HIV viral core is mostly made up of the structural protein, p24, which is called the capsid. A crucial factor in the diagnosis of primary HIV-infected individuals is the p24 antigen assay. High levels of p24 are found in the blood serum during the period between infection and seroconversion. The antibody production is found to increase as much as 64-fold [ 18 ]. The antibody production against gp120, which is a glycoprotein, necessary for attachment to a cell receptor and allow HIV entry, is found to increase up to eight-fold [ 18 ].
Another promising vaccine called the Kang's vaccine also uses the “whole-killed HIV-1,” which is similar to vaccines developed for rabies, polio and influenza [ 18 ]. However, HIV-1 is genetically engineered in such vaccines and raises questions about safety and possibility of large quantity production.
Researchers have also tested an immunogen called eOD-GT8 60mer, a protein nanoparticle, which is designed to mimic a crucial part of the HIV envelope protein which will bind to and activate the B cells to produce plasma cells that secrete antibodies needed to fight HIV [ 18 ]. This nanoparticle was developed in the Schief laboratory and tested in mouse models engineered by the Nemazee laboratory [ 18 ]. The researchers showed that immunization with eOD-GT8 60mer produced antibody progenitors with some of the characters crucial to recognize and block the HIV infection, proposing that it could be a promising first step in a series of immunizations against HIV [ 18 ]. The vaccine appears to work well in mouse models. The researchers are now investigating other immunogens that could work in coexistence with eOD-GT8 60mer [ 18 ].
Case Studies
The berlin patient [ 20 ].
The strongest proof available in favour of a HIV cure stems from the case of Timothy Brown who is popularly known as the Berlin patient (Fig. 9 ). He is considered the first person ever to be cured of HIV. The victory was predicated on doctors taking advantage of nature’s own experiment—the genetic mutation of CCR5 gene that produces a protein co-receptor present on the surface of CD4 + T-cells that HIV uses to gain entry. He was attending university in Berlin when was diagnosed HIV positive. His initial treatment include ART, and he was taking low doses of zidovudine and protease inhibitors. He continued to live a normal life for the next 10 years. But one day, he was again feeling extremely exhausted and the doctor had diagnosed it to be anaemia. He had received red blood cell transfusion for nearly a week and was then sent to an oncologist, Dr Huetter, when the previous doctor was unable to resolve the situation. The oncologist performed a painful bone marrow biopsy and after further diagnosis he was informed that he had acute myeloid leukaemia (AML).

Timothy Ray Brown a.k.a. “The Berlin patient” [ 21 ]
He then started receiving treatment at one of the Berlin University hospitals and had to receive four rounds of chemotherapy treatment. During the third round of chemotherapy, he had gotten a fatally dangerous infection and was immediately put into an induced coma. His blood sample was collected and sent to a stem cell donor bank with the German Red Cross to find matches in case he needed transplantation. Luckily, he had 267 matches which sparked an idea to locate donors with a homozygous CCR5 delta-32 mutation on CD4 + T-cells who are almost immune to HIV infection. A donor was found at the 61st attempt and had agreed to donate when necessary (Fig. 10 ).

Adam Castillejo a.k.a “The London patient” [ 23 ]
However, Timothy Brown had been reluctant and had said no to transplantation as the success rate was only 50–50. But at the end of 2006, leukaemia had rebounded and he desperately needed transplantation to survive. He received the stem cell transplant on February 6, 2007 and stopped taking his antiretroviral medication. Nearly 3 months after he underwent transplantation, HIV was no longer found in his body and he had thrived until the end of the year.
Unfortunately, life had other plans for him. After coming back from a trip to the USA, he was diagnosed with pneumonia and the leukaemia was back. The doctors decided to treat him with a second transplantation from the same donor in February 2008. The recovery was a tough one. He was almost paralyzed and went nearly blind. He had, however, eventually learnt to walk again and fully recovered 6 years later. He was continuously tested for HIV with extensive and precise tests. It was finally good news for him! Since 2010, when he decided to go public, he had interviewed for various magazines: POZ Magazine , New York Magazine and Science Magazine among others and decided to devote his life in supporting research for cures against HIV. In July 2012, he started the Timothy Ray Brown Foundation under World AIDS Institute and has worked with many scientists, organizations, research laboratories and universities to work on cures such as vaccination against HIV.
The London Patient [ 22 ]
The London patient may be the second person with HIV to no longer have the virus. In March 2019, in a report published in journal Nature , a group of investigators had announced the cure of a second HIV-positive patient. His success story depicts that CCR5 is a viable target for HIV research and treatment.
The London patient, who had chosen to remain anonymous, came out in public on March 9 th 2020. Adam Castillejo grew up in Caracas, Venezuela, and later shifted to London with his mother, as his parents were divorced. He was first diagnosed with HIV in 2003 and had started taking drugs to control the HIV infection in 2012. He had taken antiretroviral therapy for years before being diagnosed with an advanced form of blood cancer called Hodgkin’s lymphoma. Again, as in the case of the Berlin patient, the cancer was resistant to standard chemotherapy, so his doctors had advised more intensive chemotherapy along with bone marrow stem cell transplant. In 2016, he had agreed to transplantation and received it from a healthy donor who carried the CCR5 mutation. So, when his immune system regrew, it lacked the protein and was impervious to HIV. His virologist, Dr Ravindra Gupta, from the University of Cambridge, thinks it is a cure because a year had passed and they had carried out a few more tests for the viral load. In Adam Castillejo’s own words, “I don’t want people to think, “Oh, you’ve been chosen.” No, it just happened. I was in the right place, probably at the time right time, when it happened.” Adam Castillejo wants to be the “ambassador of hope” for people with this illness.
Although the scientists describe this case as a long-term remission, experts are calling it a potential cure. Such transplants are, however, dangerous and can be fatal. They are also an impractical approach to cure the millions already infected. These are highly risky procedures and can lead to serious complications. There still has to be a lot of research done to extend this type of treatment to a wider population infected with HIV.
A comparative study of the two patients reveals that their cases were in fact quite similar (Table (Table9 9 ).
Summary of the two cases—the Berlin patient and the London patient [ 24 ]
Lifestyle Practices to Prevent HIV Infection
Prevention is better than cure. And with HIV infections, one should practice prevention with utmost care and sincerity. An HIV diagnosis could turn one’s life upside down. So, it’s better to lead a healthy lifestyle by making the correct choices.
Measures for Protection Against HIV Infection
HIV is majorly spread through unprotected vaginal or anal sex. Choose less risky behaviour and be cautious. Not taking medicines to prevent or treat HIV is equally responsible for HIV infection. The number of sexual partners should be limited. One should get tested for sexually transmitted diseases and also know the sexual partner’s status. One can talk about pre-exposure prophylaxis to their respective healthcare provider. It is a preventive option for people who are not infected yet but are exposed to high risks of being HIV positive. HIV is also spread through intravenous injections and blood transfusions. Use of sterile equipment in such cases is a necessity.
Pre-exposure Prophylaxis
This is a preventive method of taking pills by people who are not HIV positive yet but who are at a high risk of getting infected and spreading it to others. A pill, named Truvada, contains two medicinal components, emtricitabine and tenofovir, that are used in combination with other drugs to treat HIV [ 25 ]. These medicines work on keeping the virus from creating a permanent infection.
Post-exposure Prophylaxis
Post-exposure prophylaxis (PEP) is a short course of HIV medicines taken soon after a possible exposure to HIV [ 25 ]. Every hour counts. For the treatment to be effective, the course should begin within 72 h after exposure to HIV; otherwise, it will not have any effect [ 25 ]. This treatment should be used only in cases of emergency. A person prescribed with PEP will need to take the medicines for 28 days at a stretch and then visit their respective healthcare provider for further tests [ 25 ]. Even if taken correctly, it may not be 100% effective. The sooner the medication is started, the better.
Healthy Practices to Follow When Living with HIV
A healthy, well-balanced and nutritious diet can help a person lead a better life by preventing health related issues like malnutrition and stopping the progression from HIV to AIDS. A well-balance diet is rich in whole grains, fresh fruits and vegetables, protein, low fat dairy products and multivitamins like zinc and B12. It also constitutes what should be cut down—fried foods, processed foods and sugary drinks. Smoking should be stopped when diagnosed with HIV. According to CDC, in the USA, the rate of adults with HIV, smoking is two to three times higher in adults infected with HIV than the nearly 18% of uninfected adults who smoke. Researchers at the Syracuse University analysed the data from 212 adults infected with HIV and found that the ones who smoked reported having more symptoms like dizziness and coughing.
Putting a stop to illegal drug use is equally necessary. People should seek treatment for addiction to illegal drugs like heroin, cocaine and methamphetamines. Sharing of needles for drugs can leave one exposed to other infections like hepatitis which might lead to a faster progression from HIV to AIDS. A recent study from the University of Pennsylvania School of Medicine showed a dramatic increase in the ability of HIV to attack healthy cells when methamphetamine is present in the bloodstream. This indicates that illegal drugs are also aiding in the HIV infection.
Being physically fit through a good work-out three to six times a week can help improve a person’s mood, perspective and overall quality of life. A good amount of moderate exercise can help fight HIV symptoms of nerve pain, loss of appetite and reduce the risks of other chronic diseases like heart disease, diabetes and osteoporosis. Taking the prescribed medication on time is known as adherence. This is vital to help reduce the risk of HIV becoming drug resistant and helps the immune system function for a longer time.
Nowadays, with the help of Internet of Things or IoT, patient’s health can be monitored 24/7. The quality of care provided can be increased many-folds with the help of monitoring devices enabled with current technology [ 26 ]. Concept of E-Health and M-Health is currently trending. E-Health makes use of electronic and communication processes with improved cyber security [ 26 ]. Some of the E-Health devices include GPS tracking, pedometer and electronic health records [ 26 ]. M-Health systems provide doctors with the complete medical history of the patient, so the treatment becomes easier and does not delay in case of emergencies. It makes use of mobile phones and other communication systems to help the patients with information about preventive health care services and collects data in real time as well [ 26 ]. The other important applications include chronic disease management, monitoring of diseases and tracking of epidemic outbreaks [ 26 ].
Genomic Diversity and Clinical Implications
Despite billions of dollars being invested, there is currently no HIV vaccine available that can either prevent the disease or treat those who suffer from it. An AIDS patient harbours 100 million genetically distinct variants of HIV [ 27 ]. This high diversity of HIV-1 is due to high replication rates, errors in reverse transcriptase and recombination events that mainly occur during the viral replication process. Reverse transcriptase enzyme has approximately a rate of 10 –4 nucleotide substitutions per replication cycle. Deletions, insertions and duplications are major contributing factors to the genetic variation of the virus [ 27 ]. Genetic recombination also plays an important role in creating genetic diversity. Template switches between two copies of RNA strands occur regularly during reverse transcription [ 27 ]. This generates a lot of mutations with the help of inter- and intra-molecular jumps. These mutations can either be drug resistant or inhibit the viral replication capacity.
HIV-1 can be classified into four main groups: M, N, O and the recently identified P. The M group is further identified into 4 subtypes (A to J). Studies have shown that there is a worldwide spread of non-B subtype viruses, and with the introduction of antiretroviral drugs, more research has to be conducted regarding the responsiveness of the drug resistance in non-B subtypes [ 27 ]. Different types of HIV-1 resistance are observed in different subtypes at varied levels. For example, subtypes B and G have shown to develop resistance against nelfinavir [ 27 ]. Research is also being done in the role of polymorphisms for development of drug resistance, to assess the genotypes before and after the therapy to be able to establish any association between the two [ 27 ].
Variation of Disease Progression Rate
There are 3 phases of the progression of HIV-1 infection- primary infection, chronic asymptomatic phase of infection and finally, AIDS. In the asymptomatic phase, neither signs nor symptoms of the disease are present, and this phase lasts an average of about 10 years. They can be divided as typical progressors, rapid progressors, slow progressors and long-term progressors. Rapid ones (10–20%) develop AIDS within 5 years of infection [ 28 ]. Slow progressors (5–15%) remain free of AIDS 15 years after infection [ 28 ]. Long-term progressors that constitute 1% show no signs and symptoms [ 28 ]. Factors like host genetic make-up, immune responses, co-infection and viral genetics and adaptation are attribute to this huge variation in disease progression [ 28 ]. But there is no solid evidence as such.
Some individuals known as elite controllers are able to manage the viral replication for longer durations, others are shown to rapidly lose CD4 + T-cells after seroconversion in the absence of cART (combination antiretroviral therapy). Scientists have conducted research studies that has led to the conclusion that rapid progression before administration of cART stops the recovery of CD4 + T-cells once the suppressive response to HIV-1 through cART is achieved. These findings have implications in public health policy making, clinical outcomes and science research. Ideally, cART should be initiated as soon the patient is diagnosed with HIV-1 irrespective of the CD4 + T-cell count. However, in clinical settings where cART is not widely available, these results would support strategies that may help in promoting frequent testing to reduce the proportion of patients initiating cART at low CD4 + T-cell counts. For those testing early, frequent CD4 + T-cell count should be monitored close to the time of HIV diagnoses to establish the rapid progressors phenotype in order to avoid unnecessary CD4 + T-cell count decay among rapid progressors. Finally, interpretation of the immunopathological basis of rapid progression can help improve individual clinical outcomes and limit its impact in the global HIV-1 pandemic.
Development of Drug Resistance as a Major Barrier to Treat HIV
HIV-1 has a high mutation rate. An estimated 10 10 virions per day can be produced in untreated patients that may result in variants called quasispecies. The complexity is also increased due to high recombination rate whenever more than one variant infects the same cell. All these are contributing factors that help in invading the host’s immune system and fostering drug resistance. Salvage therapy is also useful in cases when more than one regimen failed or a single regimen failed for a patient. It can be used to suppress the virus levels below the detection level and should have high genetic barrier to resistance to prevent rebound [ 29 ]. Clinicians need to focus on patient’s adherence as well as access to antiretrovirals (ARVs), drug interactions, tolerability, genotypic and phenotypic resistance testing, cross-resistance, genetic barrier and potency of ARVs [ 29 ].
Overcoming Obstacles and Future Prospects
At present, the reason for not being able to achieve a complete cure with the help of ART, in spite of achievement of undetectable viral load, is due to the presence of dormant virus or HIV latency. In a method call shock and kill, immune stimulants shock the latent virus from hidden reservoirs and then attempt to kill reactivated HIV [ 18 ]. An enzyme has been identified which is called histone deacetylase (HDAC) which is responsible for the sustained latency. Some studies show promise but are yet to be confirmed by clinical trials. Flushing these latent CD4 HIV-infected cells from their reservoirs with these HDAC-inhibitors into the blood circulation makes them susceptible to ART. Vorinostat and panobinostat are two such promising drugs [ 18 ].
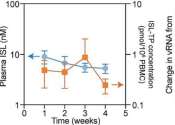
Histone deacetylase inhibitors seem to have a broad spectrum of epigenetic activities. Vorinostat (also called Zolinza) is a U.S. Food and Drug Administration approved medicine, which has been used for the treatment of cutaneous T-cell lymphoma (CTCL) [ 18 ]. They help in flushing the virus from the reservoirs into the circulation. The dose is 400 mg. Other drugs on the pipeline are Protein kinase C agonist bryostatin-1 and GS-9620—TLR7 agonist [ 18 ].
Romidepsin (also called Istodax) is another HDAC inhibitor drug, which induces HIV-1 transcription to form plasma HIV-1 RNA that can be easily detected with standard assays [ 18 ]. This gives a possibility of reversing the HIV-1 latency in vivo without hindering T cell mediated immune response [ 18 ]. These findings will help the researchers with future clinical trials aiming to eliminate the HIV-1 reservoirs.
Research for curing HIV is at an infant stage but a promising one. Scientists are working on two broad types of HIV cures—a functional cure and a sterilising one.
The approach of the functional cure is to reduce the virus levels in the body to an undetectable stage, where the patient no longer needs to be on HIV medication or has no risk of progression to AIDS nor transferring the virus to others. Unlike the functional cure, however, a sterilising cure aims to get rid of HIV from the body completely by eliminating cells from latent reservoirs. It has proved to be an extremely challenging task for scientists, who believe it may be unachievable in the majority of them living with HIV. However, some findings by researchers at the University of Pittsburgh could lead to a foundation for an HIV vaccine. Clinical trials are in the works.
Abivax, a French company, is developing a drug that binds to some specific sequence of the viral RNA and inhibits its replication. During clinical trials, it has shown that this may have the potential to become a functional cure. The key is that it can target the reservoir of HIV viruses that hide inactive within our cells. It can target the reservoirs where HIV viruses act as inactive, within the infected cells. The result of phase IIa trial was quite promising. Fifteen patients were given the drug in combination with ART, and it was observed after 28 days of treatment that eight patients showed a 25% to almost 50% reduction of their HIV reservoirs compared to those only taking ART. The company is planning a phase IIb clinical trial to confirm the effects of the drug in the long term.
Research and development in HIV and its cure have come a long way since the disease was discovered in the 1980s. ART was a major milestone that has changed the lives of millions for good, but the next ambitious goal is to find an HIV cure before the year 2020. There are several approaches to an HIV cure ranging from shock and kill therapy, immunotherapy, vaccine development to gene editing using zinc finger nucleases and the CRISPR/Cas9 system, but finding the best possible solution is a challenge. One of the biggest challenges around any HIV treatment is the ability of the virus to rapidly mutate and develop resistance. Many of the new approaches do not provide any valuable insights as to whether the virus has the potential to become resistant. As of now, none of these functional cures have reached late-stage clinical trials, and the aim of finding an HIV cure until 2020 seems far-fetched. However, 2020 will likely be marked as an important milestone as the first late-stage trials will be executed. If successful, it could bring the approval of the first functional HIV cure in ten years.
There are two gene therapies undergoing human trials—one is to destroy the CCR5 receptor of the immune cells of people infected with HIV and the other therapy includes the CRISPR technology which is still under early trials. This mutation does not necessarily protect the person against all types of HIV. It was found that in one of the patients who had received the bone marrow treatment, it was found to have the CXCR4-tropic form. It uses a different type of receptor to enter and infect the cells. It was, however, not known whether this virus was acquired after the treatment or if some patients do contract a small amount of CXCR4-tropic virus that starts to multiply when other types are not present.
HIV research continues on many fronts that could provide the same results and only some of which rely on the CCR5 delta 32 mutation, which should be explored extensively. There are many strategies which are in the early stages of development. Scientific process can be slow but if done correctly, advances can be made to find a scalable, cost-effective cure for everyone.
Acknowledgments
The authors listed in this paper wish to express their appreciation to the RSST trust Bangalore for their continuous support and encouragement.
Authors Contribution
All authors have contributed equally with their valuable comments which made the manuscript to this form.
There was no funding provided for the above research and preparation of the manuscript.
Compliance with Ethical Standards
The authors declare that they have no conflict of interest.
All the authors listed hereby confirmed that in the above research, there were no human participants and/or animals involved in any kind of determination, evaluation or research studies.
There is also final confirmation given by all the listed authors for the submission of manuscript in its actual state. The authors listed above also confirm that the above-mentioned manuscript is in its original state and the manuscript is neither submitted anywhere nor in the submission process in any other journals. In addition, all the authors have solely contributed their original work in the preparation of this manuscript. If the copying or similarity have been found, then in all situations the listed authors are solely responsible.
Significance Statement
This article aims to increase awareness among the society about the current scenario of HIV/AIDS. The scientists are working on 2 types of cures—functional and sterilizing. The path to finding a cure is a promising one as late-phase trials begin in 2020.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Praveen Kumar Gupta, Email: ni.ude.ecvr@atpugkneevarp .
Apoorva Saxena, Email: [email protected] .

Personalize Your Experience
Log in or create an account for a personalized experience based on your selected interests.
Already have an account? Log In
Free standard shipping is valid on orders of $45 or more (after promotions and discounts are applied, regular shipping rates do not qualify as part of the $45 or more) shipped to US addresses only. Not valid on previous purchases or when combined with any other promotional offers.
Register for an enhanced, personalized experience.
Receive free access to exclusive content, a personalized homepage based on your interests, and a weekly newsletter with topics of your choice.
Home / Innovation & Research / The innovative research behind HIV/AIDS treatment
The innovative research behind HIV/AIDS treatment
Please login to bookmark.

It’s been 40 years since the release of the first scientific report describing acquired immune deficiency syndrome (AIDS). Thanks to innovative research, scientists learned how the HIV virus that causes AIDS replicates and how the immune system responds to the virus. Today, many people with HIV take just one pill a day to suppress the virus, and treatment is continuing to evolve.
In this video, Dr. Stacey Rizza , Mayo Clinic infectious disease physician and HIV researcher, explains how dedicated innovative science contributed to where we are today and what scientists are working on for the future.
What did the early research find?
Because of truly dedicated innovative science, within a few years, the scientific community figured out that AIDS was due to HIV. It then took a few years to figure out how to test for that virus. Several years later, the scientific community was able to quantitate how much virus was in a person’s blood. During all this time, truly innovative research into how the virus replicates and how the immune system responds to the virus allowed bio pharmacy companies to develop what we call anti-retroviral drugs or medications to slow down the viral replication. How has medication to treat HIV evolved?
The first drug approved for HIV was in 1987, which was AZT (now known as zidovudine). At that time, it was the fastest drug ever approved by the FDA (Food and Drug Administration) and started the fast-track mechanism through the FDA.
Then several other drugs within that same class were approved in the early 1990s. In late 1995, very early 1996, the first HIV protease inhibitors were approved. At that point, it was possible to combine three different medications from two different classes and completely suppress the HIV replication.
In the last 20 years, we’ve gone from people taking multiple medicines with lots of side effects to many of my patients with HIV now take a single pill a day. That’s a combination of medicines coformulated into one pill a day that’s extremely well-tolerated and completely suppresses their virus. We know it does not eliminate the virus. If they were to stop taking that medicine, the virus would come back. But we now have a handful of people in the world who have been what we called functionally cured of HIV, meaning they’ve gone through some research protocols that eliminated the reservoir of HIV in their body.
The new drugs are so effective in people who have fully suppressed virus that many only need to use two medications to maintain HIV treatment and control. New research is investigating ways to deliver the medications differently, such as a shot that lasts several months, or maybe someday even implantable medication delivery mechanisms so that people don’t have to take the pill every day. It is very exciting that HIV therapy is moving that direction.
Why isn’t there a cure for HIV?
The reason why it is so difficult to cure HIV is that once HIV infects a person’s body, it integrates into the host genome of several cell types. Those cells then hide in any of the lymphoid tissue, such as the lymph nodes, the liver and the spleen. And they lay there as what we call “latent” or “hiding”, as long as the person is on HIV therapy. Anytime a virus does leave a cell, it gets taken care of by HIV therapy. But if the infected individual stops the HIV therapy, that latent virus will come back. To cure HIV, you have to eliminate those hiding viruses in the cells or that latent viral reservoir, which is the term. There are many ways you can approach eliminating the reservoir.
Where is the research now?
One of the more popular ways that have been investigated is something called — and there are many different terms for it — “prime, shock, and kill” or “kick, and kill”, which is essentially giving medications that first wake the virus up from latency and then find ways to make the cells that have the virus susceptible to dying. When the virus is awake, and the cell is susceptible to dying, it kills itself but does not kill any other cells in the body.
Essentially, it specifically targets the HIV-infected cells and eliminates them without hurting anything else. This new science is exciting. It’s getting closer and closer to understanding how to do this effectively. And if you can do that with oral medications rather than fancy therapies like gene therapy or bone marrow transplant, it’s scalable to large parts of the world, and you can touch millions of people that way. That’s where the area of research is on how to make those hiding cells wake up, how to make them sensitive to die, and how to target just the HIV-infected cell.
Will we see a vaccine for HIV?
HIV has been a very hard vaccine to develop. In the world of viruses, vaccines fall into one of three buckets. They fall into the bucket where they respond to antibodies induced by the vaccine, and the vaccines are outstanding. Such viruses include polio, mumps, and lucky for us, SARS-CoV-2. Then we have the second category, like the influenza vaccine, which is about 60% effective. It certainly saves lives and makes a difference, but it’s not perfect. And then we have the third bucket, which quite frankly is the vast majority of viruses that infect humans. And HIV is in that category, where simply forming an antibody to the virus is not adequate to prevent infection. You have to do very sophisticated engineering to induce T cell effects, as well as innate effects and antibody effects. Even then, sometimes it’s very hard to decide what is the part of the virus to target. After decades, and billions of dollars of research, we’re still not there for HIV. There have been many approaches of how to do this science. Many different scientific delivery mechanisms, many different areas of the viruses targeted, many different parts of the immune system targeted, and so far, none of them have been effective at preventing HIV infection.
What needs to happen next?
We still need to slow down the number of people getting infected through good public health measures and good education to stop the HIV epidemic. We still need to get more people who are infected on therapy.
We know we can do it with public health measures. But we also need to find out more about how we eliminate that reservoir and get people cured of the virus in a simple and effective way so that we can cure more people. And the last major hurdle we have is to develop an effective vaccine. We still don’t have a vaccine that can prevent infection, a preventive vaccine, or a therapeutic vaccine where you give it to people who already have the virus that can help them control the infection. A huge amount of research has happened, but we’re still not there yet.
This article originally appeared on Mayo Clinic News Network.

Relevant reading
You're the Leader. Now What?
You’re the Leader. Now What? provides proven strategies that will help you lead through those times when colleagues disagree, emotions run high, and your leadership skills are put to the test. Through engaging stories and proven processes, you will master specific techniques used by Mayo Clinic leaders to address conflicts and setbacks, employ organizational learning, and enact lasting change in your organization.

Discover more Innovation & Research content from articles, podcasts, to videos.
You May Also Enjoy

Privacy Policy
We've made some updates to our Privacy Policy. Please take a moment to review.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
Last update: Apr 23, 2024
Perinatal transmission of HIV can lead to cognitive deficits
- Date 6 hours 12 hours 1 day 3 days all
- Rank Last day 1 week 1 month all
- LiveRank Last day 1 week 1 month all
- Popular Last day 1 week 1 month all
HIV & AIDS news
Perinatal transmission of HIV to newborns is associated with serious cognitive deficits as children grow older, according to a detailed analysis of 35 studies conducted by Georgetown University Medical Center neuroscientists. ...
Apr 23, 2024
COVID-19 found to increase the risk of severe cardiovascular problems in people with HIV
A study led by the Centre for Epidemiological Studies on STIs and AIDS of Catalonia (CEEISCAT)—a group from the Germans Trias i Pujol Research Institute (IGTP), the Fundació Lluita contra les Infeccions (FLI), and Odense ...
Apr 19, 2024
New study uncovers why boys born to mothers with HIV are at greater risk of health problems and death in infancy
Researchers have found that children of women with HIV infection have an increased risk of immune abnormalities following exposure to maternal HIV viremia, immune dysfunction, and co-infections during pregnancy. The research ...
Apr 17, 2024

Project determines HIV epidemic cannot be ended without stopping former prisoners and other patients being lost to care
New data from an implementation program to be presented at this year's the ESCMID Global Congress (formerly ECCMID) in Barcelona, Spain (27–30 April) stress that the global HIV epidemic cannot be ended without keeping former ...
Apr 16, 2024

Study confirms how RNA chemical modifications benefit HIV-1
A chemical modification in the HIV-1 RNA genome whose function has been a matter of scientific debate is now confirmed to be key to the virus's ability to survive and thrive after infecting host cells, a new study has found.
Apr 11, 2024
FDA approves Dovato for teens living with HIV
The U.S. Food and Drug Administration has approved Dovato (dolutegravir/lamivudine) for adolescents living with HIV.
Scientists identify pro-aging 'sugar signature' in the blood of people living with HIV
The Wistar Institute's associate professor Mohamed Abdel-Mohsen, Ph.D., along with his team and collaborators, has identified sugar abnormalities in the blood that may promote biological aging and inflammation in people living ...
Apr 10, 2024

Small protein plays big role in chronic HIV infection
NeuroHIV refers to the effects of HIV infection on the brain or central nervous system, and to some extent, the spinal cord and peripheral nervous system. A collection of diseases, including neuropathy and dementia, neuroHIV ...
Apr 4, 2024

Early coronary disease, impaired heart function found in asymptomatic people with HIV
A new study has found that increased coronary vessel wall thickness is significantly associated with impaired diastolic function in asymptomatic, middle-aged individuals living with HIV. The study is published in Radiology: ...
'It's the greatest living experiment': Pitt Men's Study marks 40 years of AIDS research
In a Pittsburgh hospital in the early 1980s, Charles Rinaldo saw a young, previously healthy gay man critically ill with a virus usually only seen in weakened immune systems.
Apr 1, 2024

The pioneer of America's embattled global HIV program recalls the hope after years of despair
Through his office window at what was then one of Africa's few modern clinics dealing with HIV and AIDS, the man who now oversees the United States' threatened global AIDS effort used to hear the sound of taxis pulling up ...

Exploring the relationship between HIV pre-exposure prophylaxis and the incidence of chlamydia, gonorrhea and syphilis
In their research article published in Eurosurveillance, von Schreeb et al. challenge existing assumptions regarding the relationship between the use of HIV pre-exposure prophylaxis (PrEP) and the incidence of bacterial sexually ...
Mar 28, 2024


Half of those with HIV in developed countries are at least age 50, at higher risk of frailty and multiple comorbidities
A new research review to be presented at a pre-congress day for this year's European Congress of Clinical Microbiology & Infectious Diseases (ECCMID 2024) will focus on the growing prevalence of HIV in older adults, with—using ...
Mar 27, 2024

Implantable device delivers HIV antiviral with more potency than oral drugs
A team from Houston Methodist Research Institute recently showed that a nanofluidic implant delivered an HIV drug that achieved more potency than other forms of drug administration (oral) and other HIV drugs.
Mar 26, 2024
New study shows virus-like particle can effectively 'shock and kill' latent HIV reservoir
By 2030, the World Health Organization (WHO), the Global Fund and UNAIDS are hoping to end the human immunodeficiency virus (HIV) and AIDS epidemic. An international team of researchers led by Eric Arts, professor at the ...

Abuse found to increase risk for cardiovascular disease among women with HIV
A study by Allison Appleton, Mark Kuniholm and Elizabeth Vásquez in the School of Public Health's Department of Epidemiology and Biostatistics is the first to establish a connection between physical and sexual abuse and ...
Mar 21, 2024

Drug candidate may 'unmask' latent HIV-infected cells, mark them for destruction
University of Pittsburgh School of Medicine scientists have identified drug candidates that show promise to reverse the ability of HIV to escape detection by the immune system.
Mar 19, 2024
HIV in cell culture can be completely eliminated using CRISPR-Cas gene editing technology, increasing hopes of cure
New research presented early ahead of this year's European Congress of Clinical Microbiology and Infectious Diseases (ECCMID 2024, Barcelona, 27-30 April) from a team of researchers in the Netherlands shows how the latest ...

Long-acting injectable ART superior to standard care for poorly adherent people with HIV
For people with HIV (PWH) and a history of suboptimal adherence to antiretroviral therapy, long-acting injectable treatment with cabotegravir and rilpivirine (LAI) is superior to oral standard of care (SOC), according to ...
Mar 13, 2024

Improving care of hospitalized patients with HIV in Tanzania
Researchers at Weill Cornell Medicine have shown that three months of social worker follow-up support to people hospitalized with HIV in Tanzania had health benefits at low cost. The protocol shortened the time it took participants ...
Mar 11, 2024

7 hours ago

8 hours ago

10 hours ago

4 hours ago

6 hours ago

11 hours ago

12 hours ago

13 hours ago

E-mail newsletter
- What Are HIV and AIDS?
- How Is HIV Transmitted?
- Who Is at Risk for HIV?
- Symptoms of HIV
- U.S. Statistics
- Impact on Racial and Ethnic Minorities
- Global Statistics
- HIV and AIDS Timeline
- In Memoriam
- Supporting Someone Living with HIV
- Standing Up to Stigma
- Getting Involved
- HIV Treatment as Prevention
- Pre-exposure Prophylaxis (PrEP)
- Post-exposure Prophylaxis (PEP)
- Preventing Sexual Transmission of HIV
- Alcohol and HIV Risk
- Substance Use and HIV Risk
- Preventing Perinatal Transmission of HIV
- HIV Vaccines
- Long-acting HIV Prevention Tools
- Microbicides
- Who Should Get Tested?
- HIV Testing Locations
- HIV Testing Overview
- Understanding Your HIV Test Results
- Living with HIV
- Talking About Your HIV Status
- Locate an HIV Care Provider
- Types of Providers
- Take Charge of Your Care
- What to Expect at Your First HIV Care Visit
- Making Care Work for You
- Seeing Your Health Care Provider
- HIV Lab Tests and Results
- Returning to Care
- HIV Treatment Overview
- Viral Suppression and Undetectable Viral Load
- Taking Your HIV Medicine as Prescribed
- Tips on Taking Your HIV Medication Every Day
- Paying for HIV Care and Treatment
- Other Health Issues of Special Concern for People Living with HIV
- Alcohol and Drug Use
- Coronavirus (COVID-19) and People with HIV
- Hepatitis B & C
- Vaccines and People with HIV
- Flu and People with HIV
- Mental Health
- Mpox and People with HIV
- Opportunistic Infections
- Sexually Transmitted Infections
- Syphilis and People with HIV
- HIV and Women's Health Issues
- Aging with HIV
- Emergencies and Disasters and HIV
- Employment and Health
- Exercise and Physical Activity
- Food Safety and Nutrition
- Housing and Health
- Traveling Outside the U.S.
- Civil Rights
- Workplace Rights
- Limits on Confidentiality
- National HIV/AIDS Strategy (2022-2025)
- Implementing the National HIV/AIDS Strategy
- Prior National HIV/AIDS Strategies (2010-2021)
- Key Strategies
- Priority Jurisdictions
- HHS Agencies Involved
- Learn More About EHE
- Ready, Set, PrEP
- Ready, Set, PrEP Pharmacies
- Ready, Set, PrEP Resources
- AHEAD: America’s HIV Epidemic Analysis Dashboard
- HIV Prevention Activities
- HIV Testing Activities
- HIV Care and Treatment Activities
- HIV Research Activities
- Activities Combating HIV Stigma and Discrimination
- The Affordable Care Act and HIV/AIDS
- HIV Care Continuum
- Syringe Services Programs
- Finding Federal Funding for HIV Programs
- Fund Activities
- The Fund in Action
- About PACHA
- Members & Staff
- Subcommittees
- Prior PACHA Meetings and Recommendations
- I Am a Work of Art Campaign
- Awareness Campaigns
- Global HIV/AIDS Overview
- U.S. Government Global HIV/AIDS Activities
- U.S. Government Global-Domestic Bidirectional HIV Work
- Global HIV/AIDS Organizations
- National Black HIV/AIDS Awareness Day February 7
- HIV Is Not A Crime Awareness Day February 28
- National Women and Girls HIV/AIDS Awareness Day March 10
- National Native HIV/AIDS Awareness Day March 20
- National Youth HIV & AIDS Awareness Day April 10
- HIV Vaccine Awareness Day May 18
- National Asian & Pacific Islander HIV/AIDS Awareness Day May 19
- HIV Long-Term Survivors Awareness Day June 5
- National HIV Testing Day June 27
- Zero HIV Stigma July 21
- Southern HIV/AIDS Awareness Day August 20
- National Faith HIV/AIDS Awareness Day August 27
- National African Immigrants and Refugee HIV/AIDS and Hepatitis Awareness Day September 9
- National HIV/AIDS and Aging Awareness Day September 18
- National Gay Men's HIV/AIDS Awareness Day September 27
- National Latinx AIDS Awareness Day October 15
- World AIDS Day December 1
- Event Planning Guide
- U.S. Conference on HIV/AIDS (USCHA)
- National Ryan White Conference on HIV Care & Treatment
- AIDS 2020 (23rd International AIDS Conference Virtual)
Want to stay abreast of changes in prevention, care, treatment or research or other public health arenas that affect our collective response to the HIV epidemic? Or are you new to this field?
HIV.gov curates learning opportunities for you, and the people you serve and collaborate with.
Stay up to date with the webinars, Twitter chats, conferences and more in this section.
Sexually Transmitted Infections—A Closer Look at NIAID Research
- Share on Facebook
- Share on Twitter
- Share on LinkedIn
- Share on Email

Sexually transmitted infections (STIs) are caused by bacteria, viruses, or parasites. STIs have a devastating impact on adults and infants and annually affect millions of people in the United States. Certain STIs can increase a person’s risk of developing cancer and increase the likelihood of acquiring or transmitting HIV. In addition, STIs can cause long-term health complications, especially in the reproductive and central nervous systems. In rare cases, they can lead to serious illness or death.
NIAID supports research across the spectrum from basic to clinical science to develop effective diagnostic, preventive and therapeutic approaches to STIs in alignment with the National STI Strategic Plan . In recognition of National STI Awareness Week , NIAID shares a snapshot of new projects and recent scientific advances in STI research.
Improving treatment for syphilis and trichomoniasis
New reports of syphilis and congenital syphilis are increasing at an alarming rate in the United States. Syphilis is caused by the bacterium Treponema pallidum . Benzathine penicillin G (BPG) is one of only a few antibiotics known to effectively treat syphilis. There is currently a shortage of BPG, and some people are allergic to penicillin antibiotics. In February 2024, NIAID convened a workshop with a wide range of experts on alternative therapies to BPG for the treatment of adult syphilis, neurosyphilis, and syphilis in pregnant persons and infants. The workshop addressed preclinical evaluation of candidate drugs, the potential need for studies on how candidate drugs are processed in the body during pregnancy, and how to approach clinical trials of treatment for congenital syphilis. This work is part of NIAID’s comprehensive portfolio of syphilis diagnosis, prevention, and treatment research.
Trichomoniasis is the most common parasitic STI, caused by Trichomonas vaginalis . Trichomoniasis can increase the risk of getting or spreading other STIs, including HIV. The parasite can also cause inflammation of the cervix and the urethra. T. vaginalis is treated with an antibiotic drug class called nitroimidazoles. The currently recommended nitroimidazole, called metronidazole, cures 84-98% of T. vaginalis cases but does have high rates of breakthrough infection. A new project led by Tulane University will examine a single dose of secnidazole, a medicine in the same drug class, as a more effective and cost-effective treatment option for women and men.
Developing a vaccine for herpes simplex virus 2
Herpes simplex virus 2 (HSV-2) is a common subtype of herpes simplex virus that is transmitted through sexual contact. The Centers for Disease Control and Prevention estimates that 18.6 million people aged 15 years and older United States live with HSV-2. In severe cases, HSV-2 may lead to life-threatening or long-term complications. There is no licensed preventive HSV-2 vaccine, and there is no cure. A new project led by the University of Pennsylvania seeks to define correlates of protection for HSV-2, meaning they intend to identify immune processes involved in preventing HSV-2 disease. They will do this by analyzing laboratory samples from animal studies of a promising preventive vaccine candidate that they developed with prior funding. That vaccine candidate is also now in an industry-sponsored early-stage clinical trial . The same project will expand on the HSV-2 targets in the preventive vaccine to develop a therapeutic vaccine concept to reduce recurrent outbreaks. This research responds to the scientific priorities in the NIH Strategic Plan for Herpes Simplex Virus Research .
Increasing fundamental knowledge of bacterial vaginosis
Bacterial vaginosis (BV) results from an imbalance in the vaginal microbiome. BV can be caused by sexual activity, douches and menstrual products. BV can increase women’s biological susceptibility to HIV and other STIs and can cause premature birth or low birthweight if untreated in pregnant people. In a recent publication, NIAID-supported researchers, led by researchers at the University of Washington and University of California San Diego, shared findings on how damage to the vaginal skin barrier occurs during bacterial vaginosis. Those skin barrier cells, called epithelial cells, are covered in carbohydrate molecules called glycans. The research team found that people with BV had damaged glycans on their vaginal epithelial cells. They suggested that future work should examine the relationship between treatment and restoration of normal glycans. If an association is detected, it could help healthcare providers monitor for successful treatment outcomes to reduce the likelihood that BV will return after a course of treatment. The findings were published in Science Translational Medicine .
These activities are among the research investments in NIAID’s STI portfolio. For more information on STIs, please visit:
- NIAID Diseases & Conditions: Sexually Transmitted Infections
- U.S. Department of Health and Human Services STI National Strategic Plan
Related HIV.gov Blogs
- NIAID National Institute of Allergy & Infectious Diseases
- STDs Sexually Transmitted Diseases
- STI Plan Federal STI Action Plan
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
How to Thrive as You Age
Got tinnitus a device that tickles the tongue helps this musician find relief.

Allison Aubrey

After using the Lenire device for an hour each day for 12 weeks, Victoria Banks says her tinnitus is "barely noticeable." David Petrelli/Victoria Banks hide caption
After using the Lenire device for an hour each day for 12 weeks, Victoria Banks says her tinnitus is "barely noticeable."
Imagine if every moment is filled with a high-pitched buzz or ring that you can't turn off.
More than 25 million adults in the U.S., have a condition called tinnitus, according to the American Tinnitus Association. It can be stressful, even panic-inducing and difficult to manage. Dozens of factors can contribute to the onset of tinnitus, including hearing loss, exposure to loud noise or a viral illness.
There's no cure, but there are a range of strategies to reduce the symptoms and make it less bothersome, including hearing aids, mindfulness therapy , and one newer option – a device approved by the FDA to treat tinnitus using electrical stimulation of the tongue.
The device has helped Victoria Banks, a singer and songwriter in Nashville, Tenn., who developed tinnitus about three years ago.
"The noise in my head felt like a bunch of cicadas," Banks says. "It was terrifying." The buzz made it difficult for her to sing and listen to music. "It can be absolutely debilitating," she says.

Shots - Health News
Tinnitus bothers millions of americans. here's how to turn down the noise.
Banks tried taking dietary supplements , but those didn't help. She also stepped up exercise, but that didn't bring relief either. Then she read about a device called Lenire, which was approved by the FDA in March 2023. It includes a plastic mouthpiece with stainless steel electrodes that electrically stimulate the tongue. It is the first device of its kind to be approved for tinnitus.
"This had worked for other people, and I thought I'm willing to try anything at this point," Banks recalls.
She sought out audiologist Brian Fligor, who treats severe cases of tinnitus in the Boston area. Fligor was impressed by the results of a clinical trial that found 84% of participants who tried Lenire experienced a significant reduction in symptoms. He became one of the first providers in the U.S. to use the device with his patients. Fligor also served on an advisory panel assembled by the company who developed it.
"A good candidate for this device is somebody who's had tinnitus for at least three months," Fligor says, emphasizing that people should be evaluated first to make sure there's not an underlying medical issue.
Tinnitus often accompanies hearing loss, but Victoria Banks' hearing was fine and she had no other medical issue, so she was a good candidate.
Banks used the device for an hour each day for 12 weeks. During the hour-long sessions, the electrical stimulation "tickles" the tongue, she says. In addition, the device includes a set of headphones that play a series of tones and ocean-wave sounds.
The device works, in part, by shifting the brain's attention away from the buzz. We're wired to focus on important information coming into our brains, Fligor says. Think of it as a spotlight at a show pointed at the most important thing on the stage. "When you have tinnitus and you're frustrated or angry or scared by it, that spotlight gets really strong and focused on the tinnitus," Fligor says.
"It's the combination of what you're feeling through the nerves in your tongue and what you're hearing through your ears happening in synchrony that causes the spotlight in your brain to not be so stuck on the tinnitus," Fligor explains.

A clinical trial found 84% of people who used the device experienced a significant reduction in symptoms. Brian Fligor hide caption
A clinical trial found 84% of people who used the device experienced a significant reduction in symptoms.
"It unsticks your spotlight" and helps desensitize people to the perceived noise that their tinnitus creates, he says.
Banks says the ringing in her ears did not completely disappear, but now it's barely noticeable on most days.
"It's kind of like if I lived near a waterfall and the waterfall was constantly going," she says. Over time, the waterfall sound fades out of consciousness.
"My brain is now focusing on other things," and the buzz is no longer so distracting. She's back to listening to music, writing music, and performing music." I'm doing all of those things," she says.
When the buzz comes back into focus, Banks says a refresher session with the device helps.
A clinical trial found that 84% of people who tried Lenire , saw significant improvements in their condition. To measure changes, the participants took a questionnaire that asked them to rate how much tinnitus was impacting their sleep, sense of control, feelings of well-being and quality of life. After 12 weeks of using the device, participants improved by an average of 14 points.
"Where this device fits into the big picture, is that it's not a cure-all, but it's quickly become my go-to," for people who do not respond to other ways of managing tinnitus, Fligor says.
One down-side is the cost. Banks paid about $4,000 for the Lenire device, and insurance doesn't cover it. She put the expense on her credit card and paid it off gradually.
Fligor hopes that as the evidence of its effectiveness accumulates, insurers will begin to cover it. Despite the cost, more than 80% of participants in the clinical trial said they would recommend the device to a friend with tinnitus.
But, it's unclear how long the benefits last. Clinical trials have only evaluated Lenire over a 1-year period. "How durable are the effects? We don't really know yet," says audiologist Marc Fagelson, the scientific advisory committee chair of the American Tinnitus Association. He says research is promising but there's still more to learn.
Fagelson says the first step he takes with his patients is an evaluation for hearing loss. Research shows that hearing aids can be an effective treatment for tinnitus among people who have both tinnitus and hearing loss, which is much more common among older adults. An estimated one-third of adults 65 years of age and older who have hearing loss, also have tinnitus.
"We do see a lot of patients, even with very mild loss, who benefit from hearing aids," Fagelson says, but in his experience it's about 50-50 in terms of improving tinnitus. Often, he says people with tinnitus need to explore options beyond hearing aids.
Bruce Freeman , a scientist at the University of Pittsburgh Medical Center, says he's benefitted from both hearing aids and Lenire. He was fitted for the device in Ireland where it was developed, before it was available in the U.S.
Freeman agrees that the ringing never truly disappears, but the device has helped him manage the condition. He describes the sounds that play through the device headphones as very calming and "almost hypnotic" and combined with the tongue vibration, it's helped desensitize him to the ring.
Freeman – who is a research scientist – says he's impressed with the results of research, including a study published in Nature, Scientific Reports that points to significant improvements among clinical trial participants with tinnitus.
Freeman experienced a return of his symptoms when he stopped using the device. "Without it the tinnitus got worse," he says. Then, when he resumed use, it improved.
Freeman believes his long-term exposure to noisy instruments in his research laboratory may have played a role in his condition, and also a neck injury from a bicycle accident that fractured his vertebra. "All of those things converged," he says.
Freeman has developed several habits that help keep the high-pitched ring out of his consciousness and maintain good health. "One thing that does wonders is swimming," he says, pointing to the swooshing sound of water in his ears. "That's a form of mindfulness," he explains.
When it comes to the ring of tinnitus, "it comes and goes," Freeman says. For now, it has subsided into the background, he told me with a sense of relief. "The last two years have been great," he says – a combination of the device, hearing aids and the mindfulness that comes from a swim.
This story was edited by Jane Greenhalgh
- ringing in ears
- hearing loss
- International edition
- Australia edition
- Europe edition

Cost of developing new drugs may be far lower than industry claims, trial reveals
Exclusive: MSF calls for transparency after its bill for a trial of TB treatment came to a fraction of the billions claimed by pharmaceutical companies
Doctors have for the first time released details of their spending on a major clinical trial, demonstrating that the true cost of developing a medicine may be far less than the billions of dollars claimed by the pharmaceutical industry.
Médecins Sans Frontières (MSF) is challenging drug companies to be transparent about the cost of trials, which has always been shrouded in secrecy. Its own bill for landmark trials of a four-drug combination treatment for drug-resistant tuberculosis came to €34m (£29m).
Current estimates for research and development of new medicines range from €40m to €3.9bn. The extortionate cost of trials is used to justify high prices of new medicines, but companies do not publish either the topline or a breakdown of their spending. MSF says this opacity should end. It has produced a toolkit for drug trialists, which categorises each item of expenditure and allows the costs to be collated throughout the process, which can last for years.
MSF’s trial, called TB Practecal, has transformed prospects for people with drug-resistant forms of TB, which have high mortality rates and in some countries have been untreatable because of the high price of the few drugs that still work.
Dr Bern-Thomas Nyang’wa, MSF’s medical director and the chief investigator of the trial, said: “We hope that our disclosure of clinical trial costs for identifying an improved regimen for drug-resistant tuberculosis will serve as a clarion call for other public and nonprofit actors to join us and publicly share their clinical trial costs to ensure broader transparency in medical R&D costs.”
He added: “We encourage clinical trial sponsors and implementors to try our Transparency Core toolkit, and to build on it as a guide to facilitate the publication of cost data. While transparency in R&D expenditure remains largely elusive, transparency in clinical trial costs is a transformative step towards exposing what medical innovation actually costs and building a future where access to medicines and medical tools is not hindered by high prices.”

The two antimicrobial drugs that have been the staple treatment for TB for decades, isoniazid and rifampicin, no longer work as well as they did. The outlook for patients with drug-resistant TB has been bleak in middle and low-income countries. Even if alternative drugs were available, they had to be taken regularly for an entire year.
Bedaquiline, a new drug with a different mechanism against drug-resistant TB, was developed by Johnson & Johnson and, in 2012, became the first TB drug to be approved by the Food and Drug Administration in the US in 40 years. But the cost was prohibitive for many of the worst-affected countries . It took a long battle by campaigners to get the price reduced . The cost of R&D was a key factor. Eventually, it was revealed by academics that the drug was developed thanks to public funding, which was five times more than private investment.
MSF trialled the use of a combination of four oral drugs, including bedaquiline, against drug-resistant TB. Its success led to the World Health Organization (WHO) recommending six months’ treatment with the combination for rifampicin-resistant TB. It is now in use in 40 countries.
Roz Scourse, a policy adviser with MSF’s Access Campaign, said: “The global movement that pushed for a significant price reduction of the lifesaving TB drug bedaquiline demonstrated that transparency of R&D costs can lead to increased access to medical tools and help save more lives.
“The unsubstantiated yet dominant narrative that high prices are needed to recoup high R&D costs can no longer remain an evidence-free zone – this information is a critical piece of the policy puzzle that can inform the price of medical products, and who gets access.”
MSF’s paper, presented Thursday at a WHO conference on medicines pricing, showed it was possible to collect good data on spending in trials, Scourse said. She urged public disclosure, so that governments and communities can have the evidence they need to discuss pricing and work towards access for all those who need the medicines.
Although MSF’s trials took place in middle-income countries, the costs were not low, said Scourse, because they had to invest substantial sums to upgrade infrastructure – such as TB clinics – to be able to conduct high-quality research.

The pharmaceutical industry trade body, the International Federation of Pharmaceutical Manufacturers and Traders (IFPMA), said most estimates for the cost of an approved drug ranged from $2.2bn-$3.2bn (£1.7bn-£2.5bn), and pointed to a Deloitte analysis from 2022 which put the average at $2.3bn .
“The pharmaceutical industry invests around $200bn every year on research and development,” said James Anderson, IFPMA’s executive director of global health. “Over the last 10 years alone, companies have developed over 470 medicines to treat diseases such as cancer, cardiovascular diseases and diabetes, as well as vaccines to protect against significant infections from malaria, RSV and Covid-19, among others.
“Medicines should be affordable to healthcare systems, available to patients everywhere, and prices must reflect the value that a medicine delivers to societies in different countries. This can only be achieved by recognising the value of medicines, while engaging in dialogue on how to make innovations more affordable and accessible to all.”
- Global development
- Fair Access
- Global health
- Pharmaceuticals industry
- Tuberculosis
Most viewed
- Share full article
Advertisement
Supported by
Why Are Younger Adults Developing This Common Heart Condition?
New research suggests that A-fib may be more prevalent, and more dangerous, in people under 65 than previously thought.

By Dani Blum
Atrial fibrillation, a common cardiac condition that raises the risk of stroke, is increasingly affecting the health of people under the age of 65.
For years, experts thought that A-fib, a type of irregular heartbeat, primarily occurred in people age 65 and older, and that younger people with the condition most likely wouldn’t develop other cardiac issues, said Dr. Aditya Bhonsale, a cardiac electrophysiologist at the University of Pittsburgh Medical Center. But in new research published Monday, Dr. Bhonsale and his colleagues examined data on more than 67,000 patients with A-fib who were treated at the center, nearly one-quarter of whom were under the age of 65. Those patients had an increased risk of death, compared to people without the condition. They also often had risk factors for A-fib like high blood pressure, obesity and sleep apnea, which could make cardiovascular health issues worse.
What is A-fib?
In A-fib, the upper and lower chambers of the heart are not coordinated as they should be, which makes the heart beat chaotically — sometimes too slow, sometimes too fast, often just irregularly. People with the condition can experience a fluttering heartbeat and palpitations.
Dr. Geoffrey Barnes, a cardiologist and vascular medicine specialist at University of Michigan Health, said that he frequently saw patients who say “I felt like my heart was racing away” or “I felt like it was skipping beats.” People with A-fib can also experience shortness of breath and chest discomfort. Some people have occasional episodes; others will continuously experience an irregular heartbeat. People often have no symptoms and don’t even realize they have the condition, Dr. Barnes said.
Increasingly, doctors said, patients are seeking care because their smart watches have detected an irregular heartbeat. That might help explain why more younger people are being diagnosed, said Dr. Hugh Calkins, a professor of cardiology at Johns Hopkins Medicine. “The more you screen, the more you’re going to find,” he said.
Doctors typically diagnose atrial fibrillation with an electrocardiogram while factoring in your medical and family history. They will sometimes give patients a portable monitor to wear for up to a month to look for an irregular heartbeat.
A-fib can cause clots to form in the heart that can travel to the brain and lead to strokes, even in younger patients, Dr. Bhonsale said. The condition may also raise the risk of cognitive decline and dementia , as well as heart failure. In the study, researchers found that people with A-fib under the age of 65 were at a significantly higher risk of hospitalization for heart failure, stroke and heart attack, compared to people without A-fib.
What’s driving the increase in younger adults?
Atrial fibrillation may also be increasing among younger adults because many of the risk factors for the condition — including pre-existing heart disease and diabetes — are on the rise in that age group, too, Dr. Bhonsale said.
Nearly one in five people in the study who had A-fib also had obstructive sleep apnea , which is a significant risk factor for the condition. People with sleep apnea stop and restart breathing in the night; they struggle to get sufficient rest. The condition, which often goes undiagnosed , is tied to a range of cardiovascular issues .
There is also a correlation between how much alcohol people consume and the likelihood they will develop A-fib, said Dr. Bradley Knight, the medical director of electrophysiology at the Northwestern Medicine Bluhm Cardiovascular Institute. Smoking cigarettes and vaping are also linked with a greater risk of A-fib, Dr. Barnes said.
While exercise in general is associated with a lower risk of cardiac conditions, extreme endurance exercise, like marathons and triathlons, are linked with a higher risk of A-fib, Dr. Calkins said.
How is A-fib treated?
Doctors work with patients to address factors that make A-fib more likely to occur, such as by making sure someone with sleep apnea is using a CPAP machine or by helping patients quit smoking. Sometimes, particularly for younger patients, physicians will recommend a procedure called catheter ablation , which doctors use to get rid of tissue in the heart that may be causing an irregular heartbeat.
Doctors may also prescribe blood thinners, to reduce stroke risk, as well as other medications to manage symptoms. These include drugs that can help regulate heart rate and rhythm , Dr. Knight said. While medications can help reduce the frequency and duration of A-fib episodes, “they rarely eliminate the A-fib,” he added. He tells patients that the disease is like high blood pressure: It must be continuously managed.
“If you are diagnosed with A-fib at any age, but in particular at a younger age, you have been given a great opportunity to now say, OK, what things can I do to help better manage my health and reduce the chance of having a problem later in life?” Dr. Barnes said. “I almost think of it like a wake-up call.”
Dani Blum is a health reporter for The Times. More about Dani Blum
Tips for Better Sleep
Tired of tossing and turning there are some strategies you could try to maximize your hours in bed..
Four out of five people say that they suffer from sleep problems at least once a week and wake up feeling exhausted. Use our guide for a better night’s sleep .
Poor sleep can make anxiety, depression and other mental health issues worse. Here’s what to do about it .
Sleep deprivation doesn’t just feel terrible — it can also hamper your ability to form and recall memories .
The “sleepy girl mocktail” has gone viral on TikTok, where wellness influencers are touting it as a must-have to help you sleep. But is it effective ?
Do sleeping pills work? We asked experts about the different types of medications for treating insomnia .
Sharing a bed with a restless partner doesn’t have to be torture. Try these tips .
Turn Your Bedroom Into a Sleep Sanctuary With Wirecutter’s Recommendations
Good rest starts with a great mattress. These tips can help you pick the right one for you out of the countless options available .
Next, you’ll need a good pillow. These customizable models offer the comfort you need — whether you sleep on your stomach, side or back.
Looking for a more luxe experience? The right sheets can make a big difference. Here is a selection to choose from .
White noise machines have the power to mask yapping dogs, clanky radiators and late-night parties. Consider buying one .
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 21 June 2023
Prevention, treatment and cure of HIV infection
- Raphael J. Landovitz ORCID: orcid.org/0000-0002-1442-714X 1 ,
- Hyman Scott ORCID: orcid.org/0000-0001-8775-7214 2 , 3 &
- Steven G. Deeks ORCID: orcid.org/0000-0001-6371-747X 3
Nature Reviews Microbiology volume 21 , pages 657–670 ( 2023 ) Cite this article
8930 Accesses
16 Citations
199 Altmetric
Metrics details
- Antiviral agents
- HIV infections
The development of antiretroviral therapy for the prevention and treatment of HIV infection has been marked by a series of remarkable successes. However, the efforts to develop a vaccine have largely failed, and efforts to discover a cure are only now beginning to gain traction. In this Review, we describe recent progress on all fronts — pre-exposure prophylaxis, vaccines, treatment and cure — and we discuss the unmet needs, both current and in the coming years. We describe the emerging arsenal of drugs, biologics and strategies that will hopefully address these needs. Although HIV research has largely been siloed in the past, this is changing, as the emerging research agenda is marked by multiple cross-discipline synergies and collaborations. As the limitations of antiretroviral drugs as a means to truly end the epidemic are becoming more apparent, there is a great need for continued efforts to develop an effective preventative vaccine and a scalable cure, both of which remain formidable challenges.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others

Why and where an HIV cure is needed and how it might be achieved

Research priorities for an HIV cure: International AIDS Society Global Scientific Strategy 2021

CD8+ T cells in HIV control, cure and prevention
Landovitz, R. J. et al. Cabotegravir for HIV prevention in cisgender men and transgender women. N. Engl. J. Med. 385 , 595–608 (2021).
CAS PubMed PubMed Central Google Scholar
Grant, R. M. et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N. Engl. J. Med. 363 , 2587–2599 (2010).
Joint United Nations Programme on HIV/AIDS. Global HIV and AIDS statistics — 2022 fact sheet. UNAIDS https://www.unaids.org/en/resources/fact-sheet (2022).
Cohen, S. E. et al. Acquisition of tenofovir-susceptible, emtricitabine-resistant HIV despite high adherence to daily pre-exposure prophylaxis: a case report. Lancet HIV https://doi.org/10.1016/S2352-3018(18)30288-1 (2018).
Article PubMed PubMed Central Google Scholar
Cohen, S. M., Hu, X., Sweeney, P., Johnson, A. S. & Hall, H. I. HIV viral suppression among persons with varying levels of engagement in HIV medical care, 19 US jurisdictions. J. Acquir. Immune Defic. Syndr. 67 , 519–527 (2014).
PubMed Google Scholar
Havlir, D. V. et al. HIV testing and treatment with the use of a community health approach in rural Africa. N. Engl. J. Med. 381 , 219–229 (2019).
PubMed PubMed Central Google Scholar
Hayes, R. J. et al. Effect of universal testing and treatment on HIV incidence — HPTN 071 (PopART). N. Engl. J. Med. 381 , 207–218 (2019).
Makhema, J. et al. Universal testing, expanded treatment, and incidence of HIV infection in Botswana. N. Engl. J. Med. 381 , 230–242 (2019).
Cohen, M. S. et al. Prevention of HIV-1 infection with early antiretroviral therapy. N. Engl. J. Med. 365 , 493–505 (2011).
Larmarange, J. et al. The impact of population dynamics on the population HIV care cascade: results from the ANRS 12249 Treatment as Prevention trial in rural KwaZulu-Natal (South Africa). J. Int. AIDS Soc. 21 , e25128 (2018).
Thigpen, M. C. et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N. Engl. J. Med. 367 , 423–434 (2012).
CAS PubMed Google Scholar
Liu, A. Y. et al. Preexposure prophylaxis for HIV infection integrated with municipal- and community-based sexual health services. JAMA Intern. Med. 176 , 75–84 (2016).
Choopanya, K. et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet 381 , 2083–2090 (2013).
Mayer, K. H. et al. Emtricitabine and tenofovir alafenamide vs emtricitabine and tenofovir disoproxil fumarate for HIV pre-exposure prophylaxis (DISCOVER): primary results from a randomised, double-blind, multicentre, active-controlled, phase 3, non-inferiority trial. Lancet 396 , 239–254 (2020).
Molina, J. M. et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 Infection. N. Engl. J. Med. 373 , 2237–2246 (2015).
World Health Organization. Guidelines on Long-Acting Injectable Cabotegravir for HIV Prevention (WHO, 2022).
Gandhi, R. T. et al. Antiretroviral drugs for treatment and prevention of HIV infection in adults: 2022 recommendations of the International Antiviral Society-USA panel. J. Am. Med. Assoc. 329 , 63–84 (2022).
Google Scholar
Van Damme, L. et al. Preexposure prophylaxis for HIV infection among African women. N. Engl. J. Med. 367 , 411–422 (2012).
Marrazzo, J. M. et al. Tenofovir-based preexposure prophylaxis for HIV infection among African women. N. Engl. J. Med. 372 , 509–518 (2015).
Abdool Karim, Q. et al. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science 329 , 1168–1174 (2010).
Baeten, J. M. et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N. Engl. J. Med. 367 , 399–410 (2012).
Baeten, J. M. et al. Use of a vaginal ring containing dapivirine for HIV-1 prevention in women. N. Engl. J. Med. 375 , 2121–2132 (2016).
World Health Organization. WHO recommends the dapivirine vaginal ring as a new choice for HIV prevention for women at substantial risk of HIV infection. WHO https://www.who.int/news/item/26-01-2021-who-recommends-the-dapivirine-vaginal-ring-as-a-new-choice-for-hiv-prevention-for-women-at-substantial-risk-of-hiv-infection (2021).
Baeten, J. M., Hendrix, C. W. & Hillier, S. L. Topical microbicides in HIV prevention: state of the promise. Annu. Rev. Med. 71 , 361–377 (2020).
Delany-Moretlwe, S. et al. Cabotegravir for the prevention of HIV-1 in women: results from HPTN 084, a phase 3, randomised clinical trial. Lancet 399 , 1779–1789 (2022).
Marzinke, M. A. et al. Characterization of human immunodeficiency virus (HIV) infection in cisgender men and transgender women who have sex with men receiving injectable cabotegravir for HIV prevention: HPTN 083. J. Infect. Dis. 224 , 1581–1592 (2021).
Gulick, R. M. et al. Treatment with indinavir, zidovudine, and lamivudine in adults with human immunodeficiency virus infection and prior antiretroviral therapy. N. Engl. J. Med. 337 , 734–739 (1997).
Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents with HIV. Clinicalinfo.HIV.gov https://clinicalinfo.hiv.gov/en/guidelines/hiv-clinical-guidelines-adult-and-adolescent-arv/whats-new (2023).
Trickey, A. et al. Associations of modern initial antiretroviral drug regimens with all-cause mortality in adults with HIV in Europe and North America: a cohort study. Lancet HIV 9 , e404–e413 (2022).
Venter, W. D. F. et al. Dolutegravir plus two different prodrugs of tenofovir to treat HIV. N. Engl. J. Med. 381 , 803–815 (2019).
Editorial. PEPFAR looks to the future. Lancet HIV 9 , e367 (2022).
Orkin, C. et al. Long-acting cabotegravir plus rilpivirine for treatment in adults with HIV-1 infection: 96-week results of the randomised, open-label, phase 3 FLAIR study. Lancet HIV 8 , e185–e196 (2021).
Christopoulos, K. A. et al. First demonstration project of long-acting injectable antiretroviral therapy for persons with and without detectable HIV viremia in an urban HIV clinic. Clin. Infect. Dis. 76 , e645–e651 (2022).
PubMed Central Google Scholar
Segal-Maurer, S. et al. Capsid Inhibition with lenacapavir in multidrug-resistant HIV-1 infection. N. Engl. J. Med. 386 , 1793–1803 (2022).
Benhabbour, S. R. et al. Ultra-long-acting tunable biodegradable and removable controlled release implants for drug delivery. Nat. Commun. 10 , 4324 (2019).
Kovarova, M. et al. Ultra-long-acting removable drug delivery system for HIV treatment and prevention. Nat. Commun. 9 , 4156 (2018).
Haynes, B. F., Burton, D. R. & Mascola, J. R. Multiple roles for HIV broadly neutralizing antibodies. Sci. Transl Med. 11 , eaaz2686 (2019).
Caskey, M., Klein, F. & Nussenzweig, M. C. Broadly neutralizing anti-HIV-1 monoclonal antibodies in the clinic. Nat. Med. 25 , 547–553 (2019).
Gaudinski, M. R. et al. Safety and pharmacokinetics of broadly neutralising human monoclonal antibody VRC07-523LS in healthy adults: a phase 1 dose-escalation clinical trial. Lancet HIV 6 , e667–e679 (2019).
Gaudinski, M. R. et al. Safety and pharmacokinetics of the Fc-modified HIV-1 human monoclonal antibody VRC01LS: a phase 1 open-label clinical trial in healthy adults. PLoS Med. 15 , e1002493 (2018).
Corey, L. et al. Two randomized trials of neutralizing antibodies to prevent HIV-1 acquisition. N. Engl. J. Med. 384 , 1003–1014 (2021).
Sneller, M. C. et al. Combination anti-HIV antibodies provide sustained virological suppression. Nature 606 , 375–381 (2022).
Gaebler, C. et al. Prolonged viral suppression with anti-HIV-1 antibody therapy. Nature 606 , 368–374 (2022).
Pegu, A. et al. Potent anti-viral activity of a trispecific HIV neutralizing antibody in SHIV-infected monkeys. Cell Rep. 38 , 110199 (2022).
Collins, F. et al. The NIH-led research response to COVID-19. Science 379 , 441–444 (2023).
Buchbinder, S. P. et al. Efficacy assessment of a cell-mediated immunity HIV-1 vaccine (the Step Study): a double-blind, randomised, placebo-controlled, test-of-concept trial. Lancet 372 , 1881–1893 (2008).
Rerks-Ngarm, S. et al. Vaccination with ALVAC and AIDSVAX to prevent HIV-1 infection in Thailand. N. Engl. J. Med. 361 , 2209–2220 (2009).
Haynes, B. F. et al. Immune-correlates analysis of an HIV-1 vaccine efficacy trial. N. Engl. J. Med. 366 , 1275–1286 (2012).
Gray, G. E. et al. Immune correlates of the Thai RV144 HIV vaccine regimen in South Africa. Sci. Transl Med. 11 , eaax1880 (2019).
Moodie, Z. et al. Analysis of the HVTN 702 Phase 2b-3 HIV-1 vaccine trial in South Africa assessing RV144 antibody and T-cell correlates of HIV-1 acquisition risk. J. Infect. Dis. 226 , 246–257 (2022).
Gray, G. E. et al. Vaccine efficacy of ALVAC-HIV and bivalent subtype C gp120-MF59 in adults. N. Engl. J. Med. 384 , 1089–1100 (2021).
Barouch, D. H. et al. Evaluation of a mosaic HIV-1 vaccine in a multicentre, randomised, double-blind, placebo-controlled, phase 1/2a clinical trial (APPROACH) and in rhesus monkeys (NHP 13-19). Lancet 392 , 232–243 (2018).
Hansen, S. G. et al. Immune clearance of highly pathogenic SIV infection. Nature 502 , 100–104 (2013).
Jiang, C. et al. Distinct viral reservoirs in individuals with spontaneous control of HIV-1. Nature 585 , 261–267 (2020).
Turk, G. et al. A possible sterilizing cure of HIV-1 infection without stem cell transplantation. Ann. Intern. Med. 175 , 95–100 (2022).
Jardine, J. G. et al. HIV-1 broadly neutralizing antibody precursor B cells revealed by germline-targeting immunogen. Science 351 , 1458–1463 (2016).
Haynes, B. F. et al. Strategies for HIV-1 vaccines that induce broadly neutralizing antibodies. Nat. Rev. Immunol. 23 , 142–158 (2023).
Leggat, D. J. et al. Vaccination induces HIV broadly neutralizing antibody precursors in humans. Science 378 , eadd6502 (2022).
Sanders, R. W. et al. A next-generation cleaved, soluble HIV-1 Env trimer, BG505 SOSIP.664 gp140, expresses multiple epitopes for broadly neutralizing but not non-neutralizing antibodies. PLoS Pathog. 9 , e1003618 (2013).
Borst, A. J. et al. Germline VRC01 antibody recognition of a modified clade C HIV-1 envelope trimer and a glycosylated HIV-1 gp120 core. eLife 7 , e37688 (2018).
Arunachalam, P. S. et al. T cell-inducing vaccine durably prevents mucosal SHIV infection even with lower neutralizing antibody titers. Nat. Med. 26 , 932–940 (2020).
McMahan, K. et al. Correlates of protection against SARS-CoV-2 in rhesus macaques. Nature 590 , 630–634 (2021).
Ndung’u, T., McCune, J. M. & Deeks, S. G. Why and where an HIV cure is needed and how it might be achieved. Nature 576 , 397–405 (2019).
Deeks, S. G. et al. Research priorities for an HIV cure: International AIDS Society global scientific strategy 2021. Nat. Med. 27 , 2085–2098 (2021).
Dybul, M. et al. The case for an HIV cure and how to get there. Lancet HIV 8 , e51–e58 (2021).
Ho, Y. C. et al. Replication-competent noninduced proviruses in the latent reservoir increase barrier to HIV-1 cure. Cell 155 , 540–551 (2013).
Siliciano, J. D. et al. Long-term follow-up studies confirm the stability of the latent reservoir for HIV-1 in resting CD4 + T cells. Nat. Med. 9 , 727–728 (2003).
Wagner, T. A. et al. HIV latency. Proliferation of cells with HIV integrated into cancer genes contributes to persistent infection. Science 345 , 570–573 (2014).
Maldarelli, F. et al. HIV latency. Specific HIV integration sites are linked to clonal expansion and persistence of infected cells. Science 345 , 179–183 (2014).
Einkauf, K. B. et al. Parallel analysis of transcription, integration, and sequence of single HIV-1 proviruses. Cell 185 , 266–282.e15 (2022).
Cohn, L. B. et al. HIV-1 integration landscape during latent and active infection. Cell 160 , 420–432 (2015).
Nixon, C. C. et al. Systemic HIV and SIV latency reversal via non-canonical NF-κB signalling in vivo. Nature 578 , 160–165 (2020).
Badley, A. D., Sainski, A., Wightman, F. & Lewin, S. R. Altering cell death pathways as an approach to cure HIV infection. Cell Death Dis. 4 , e718 (2013).
Yates, K. B. et al. Epigenetic scars of CD8 + T cell exhaustion persist after cure of chronic infection in humans. Nat. Immunol. 22 , 1020–1029 (2021).
Rutishauser, R. L. et al. TCF-1 regulates HIV-specific CD8 + T cell expansion capacity. JCI Insight 6 , e136648 (2021).
Mancuso, P. et al. CRISPR based editing of SIV proviral DNA in ART treated non-human primates. Nat. Commun. 11 , 6065 (2020).
Kessing, C. F. et al. In vivo suppression of HIV rebound by didehydro-cortistatin A, a “block-and-lock” strategy for HIV-1 treatment. Cell Rep. 21 , 600–611 (2017).
Borducchi, E. N. et al. Ad26/MVA therapeutic vaccination with TLR7 stimulation in SIV-infected rhesus monkeys. Nature 540 , 284–287 (2016).
Bailon, L. et al. Safety, immunogenicity and effect on viral rebound of HTI vaccines in early treated HIV-1 infection: a randomized, placebo-controlled phase 1 trial. Nat. Med. 28 , 2611–2621 (2022).
Nishimura, Y. et al. Early antibody therapy can induce long-lasting immunity to SHIV. Nature 543 , 559–563 (2017).
Mendoza, P. et al. Combination therapy with anti-HIV-1 antibodies maintains viral suppression. Nature 561 , 479–484 (2018).
Borducchi, E. N. et al. Antibody and TLR7 agonist delay viral rebound in SHIV-infected monkeys. Nature 563 , 360–364 (2018).
Niessl, J. et al. Combination anti-HIV-1 antibody therapy is associated with increased virus-specific T cell immunity. Nat. Med. 26 , 222–227 (2020).
Gunst, J. D. et al. Early intervention with 3BNC117 and romidepsin at antiretroviral treatment initiation in people with HIV-1: a phase 1b/2a, randomized trial. Nat. Med. 28 , 2424–2435 (2022).
Tebas, P. et al. CCR5-edited CD4 + T cells augment HIV-specific immunity to enable post-rebound control of HIV replication. J. Clin. Invest. 131 , e144486 (2021).
Gardner, M. R. et al. AAV-expressed eCD4-Ig provides durable protection from multiple SHIV challenges. Nature 519 , 87–91 (2015).
Martinez-Navio, J. M. et al. Adeno-associated virus delivery of anti-HIV monoclonal antibodies can drive long-term virologic suppression. Immunity 50 , 567–575.e5 (2019).
Casazza, J. P. et al. Safety and tolerability of AAV8 delivery of a broadly neutralizing antibody in adults living with HIV: a phase 1, dose-escalation trial. Nat. Med. 28 , 1022–1030 (2022).
Hutter, G. et al. Long-term control of HIV by CCR5 delta32/delta32 stem-cell transplantation. N. Engl. J. Med. 360 , 692–698 (2009).
Gupta, R. K. et al. HIV-1 remission following CCR5Δ32/Δ32 haematopoietic stem-cell transplantation. Nature 568 , 244–248 (2019).
Okoye, A. A. et al. Early antiretroviral therapy limits SIV reservoir establishment to delay or prevent post-treatment viral rebound. Nat. Med. 24 , 1430–1440 (2018).
Henrich, T. J. et al. HIV-1 persistence following extremely early initiation of antiretroviral therapy (ART) during acute HIV-1 infection: an observational study. PLoS Med. 14 , e1002417 (2017).
Mitchell, J. L. et al. Plasmacytoid dendritic cells sense HIV replication before detectable viremia following treatment interruption. J. Clin. Invest. 130 , 2845–2858 (2020).
Gondim, M. V. P. et al. Heightened resistance to host type 1 interferons characterizes HIV-1 at transmission and after antiretroviral therapy interruption. Sci. Transl Med. 13 , eabd8179 (2021).
Prator, C. A. et al. Circulating CD30 + CD4 + T cells increase before human immunodeficiency virus rebound after analytical antiretroviral treatment interruption. J. Infect. Dis. 221 , 1146–1155 (2020).
Landovitz, R. J. et al. Tail-phase safety, tolerability, and pharmacokinetics of long-acting injectable cabotegravir in HIV-uninfected adults: a secondary analysis of the HPTN 077 trial. Lancet HIV 7 , e472–e481 (2020).
Eshleman, S. H. et al. HIV RNA screening reduces integrase strand transfer inhibitor resistance risk in persons receiving long-acting cabotegravir for HIV prevention. J. Infect. Dis. 226 , 2170–2180 (2022).
Beacroft, L. & Hallett, T. B. The potential impact of a “curative intervention” for HIV: a modelling study. Glob. Health Res. Policy 4 , 2 (2019).
Lehman, D. A. et al. Risk of drug resistance among persons acquiring HIV within a randomized clinical trial of single- or dual-agent preexposure prophylaxis. J. Infect. Dis. 211 , 1211–1218 (2015).
Dube, K. et al. Participant experiences using novel home-based blood collection device for viral load testing in the HIV cure trials with analytical treatment interruptions. HIV Res. Clin. Pract. 23 , 76–90 (2022).
Deeks, S. G. et al. Strong cell-mediated immune responses are associated with the maintenance of low-level viremia in antiretroviral-treated individuals with drug-resistant human immunodeficiency virus type 1. J. Infect. Dis. 189 , 312–321 (2004).
Bertagnolli, L. N. et al. Autologous IgG antibodies block outgrowth of a substantial but variable fraction of viruses in the latent reservoir for HIV-1. Proc. Natl Acad. Sci. USA 117 , 32066–32077 (2020).
Blazkova, J. et al. Distinct mechanisms of long-term virologic control in two HIV-infected individuals after treatment interruption of anti-retroviral therapy. Nat. Med. 27 , 1893–1898 (2021).
Jones, R. B. & Walker, B. D. HIV-specific CD8 + T cells and HIV eradication. J. Clin. Invest. 126 , 455–463 (2016).
Collins, D. R., Gaiha, G. D. & Walker, B. D. CD8 + T cells in HIV control, cure and prevention. Nat. Rev. Immunol. 20 , 471–482 (2020).
Fukazawa, Y. et al. B cell follicle sanctuary permits persistent productive simian immunodeficiency virus infection in elite controllers. Nat. Med. 21 , 132–139 (2015).
Imamichi, H. et al. Defective HIV-1 proviruses produce viral proteins. Proc. Natl Acad. Sci. USA 117 , 3704–3710 (2020).
Pollack, R. A. et al. Defective HIV-1 proviruses are expressed and can be recognized by cytotoxic T lymphocytes, which shape the proviral landscape. Cell Host Microbe 21 , 494–506.e4 (2017).
Gaiha, G. D. et al. Structural topology defines protective CD8 + T cell epitopes in the HIV proteome. Science 364 , 480–484 (2019).
Mothe, B. et al. Therapeutic vaccination refocuses T-cell responses towards conserved regions of HIV-1 in early treated individuals (BCN 01 study). eClinicalMedicine 11 , 65–80 (2019).
Korber, B. & Fischer, W. T cell-based strategies for HIV-1 vaccines. Hum. Vaccin. Immunother. 16 , 713–722 (2020).
Stevenson, E. M. et al. HIV-specific T cell responses reflect substantive in vivo interactions with antigen despite long-term therapy. JCI Insight 6 , e142640 (2021).
Stevenson, E. M. et al. SARS CoV-2 mRNA vaccination exposes latent HIV to Nef-specific CD8 + T-cells. Nat. Commun. 13 , 4888 (2022).
Duette, G. et al. The HIV-1 proviral landscape reveals that Nef contributes to HIV-1 persistence in effector memory CD4 + T cells. J. Clin. Invest. 132 , e154422 (2022).
Collins, D. R. et al. Functional impairment of HIV-specific CD8 + T cells precedes aborted spontaneous control of viremia. Immunity 54 , 2372–2384.e7 (2021).
Lewin, S. R. et al. Multi-stakeholder consensus on a target product profile for an HIV cure. Lancet HIV 8 , e42–e50 (2021).
Colasanti, J. et al. Continuous retention and viral suppression provide further insights into the HIV care continuum compared to the cross-sectional HIV care cascade. Clin. Infect. Dis. 62 , 648–654 (2016).
Joint United Nations Programme on HIV/AIDS. African leaders unite in pledge to end AIDS in children. UNAIDS https://www.unaids.org/en/keywords/children (2023).
Patel, P. et al. Pregnancy outcomes and pharmacokinetics in pregnant women living with HIV exposed to long-acting cabotegravir and rilpivirine in clinical trials. HIV Med. 24 , 568–579 (2022).
Penazzato, M. et al. Advancing the prevention and treatment of HIV in children: priorities for research and development. Lancet HIV 9 , e658–e666 (2022).
Persaud, D. et al. Absence of detectable HIV-1 viremia after treatment cessation in an infant. N. Engl. J. Med. 369 , 1828–1835 (2013).
Violari, A. et al. A child with perinatal HIV infection and long-term sustained virological control following antiretroviral treatment cessation. Nat. Commun. 10 , 412 (2019).
Frange, P. et al. HIV-1 virological remission lasting more than 12 years after interruption of early antiretroviral therapy in a perinatally infected teenager enrolled in the French ANRS EPF-CO10 paediatric cohort: a case report. Lancet HIV 3 , e49–54 (2016).
Hartana, C. A. et al. Immune correlates of HIV-1 reservoir cell decline in early-treated infants. Cell Rep. 40 , 111126 (2022).
Uprety, P. et al. Human immunodeficiency virus type 1 DNA decay dynamics with early, long-term virologic control of perinatal infection. Clin. Infect. Dis. 64 , 1471–1478 (2017).
Capparelli, E. V. et al. Safety and pharmacokinetics of intravenous 10-1074 and VRC01LS in young children. J. Acquir. Immune Defic. Syndr. 91 , 182–188 (2022).
Bonacci, R. A., Smith, D. K. & Ojikutu, B. O. Toward greater pre-exposure prophylaxis equity: increasing provision and uptake for black and Hispanic/Latino individuals in the US. Am. J. Prev. Med. 61 , S60–S72 (2021).
Harris, N. S. et al. Vital signs: status of human immunodeficiency virus testing, viral suppression, and HIV preexposure prophylaxis — United States, 2013–2018. MMWR Morb. Mortal. Wkly. Rep. 68 , 1117–1123 (2019).
Xavier Hall, C. D., Feinstein, B. A., Rusie, L., Phillips Ii, G. & Beach, L. B. Race and sexual identity differences in PrEP continuum outcomes among Latino men in a large Chicago area healthcare network. AIDS Behav. 26 , 1943–1955 (2022).
Monroe, A. K. et al. Integrase inhibitor prescribing disparities in the DC and Johns Hopkins HIV cohorts. Open Forum Infect. Dis. 8 , ofab338 (2021).
Joint United Nations Programme on HIV/AIDS. In danger: UNAIDS global AIDS update 2022 (UNAIDS, 2022).
Yukl, S. A. et al. Challenges in detecting HIV persistence during potentially curative interventions: a study of the Berlin Patient. PLoS Pathog. 9 , e1003347 (2013).
Jensen, B.-E. O. et al. In-depth virological and immunological characterization of HIV-1 cure after CCR5Δ32/Δ32 allogeneic hematopoietic stem cell transplantation. Nat. Med. 29 , 583–587 (2023).
Hsu, J. et al. HIV-1 remission and possible cure in a woman after haplo-cord blood transplant. Cell 186 , 1115–1126.e8 (2023).
Mendoza, D. et al. Comprehensive analysis of unique cases with extraordinary control over HIV replication. Blood 119 , 4645–4655 (2012).
Saez-Cirion, A. et al. Post-treatment HIV-1 controllers with a long-term virological remission after the interruption of early initiated antiretroviral therapy ANRS VISCONTI Study. PLoS Pathog. 9 , e1003211 (2013).
Download references
Author information
Authors and affiliations.
Center for Clinical AIDS Research and Education, David Geffen School of Medicine, University of California, Los Angeles, CA, USA
Raphael J. Landovitz
Bridge HIV, San Francisco Department of Public Health, San Francisco, CA, USA
Hyman Scott
Division of HIV, Infectious Diseases & Global Medicine, Department of Medicine, University of California, San Francisco, CA, USA
Hyman Scott & Steven G. Deeks
You can also search for this author in PubMed Google Scholar
Contributions
S.G.D. researched data for the article. All authors contributed substantially to discussion of the content. All authors wrote the article. All authors reviewed and/or edited the manuscript before submission.
Corresponding author
Correspondence to Steven G. Deeks .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Peer review
Peer review information.
Nature Reviews Microbiology thanks Linda-Gail Bekker and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Landovitz, R.J., Scott, H. & Deeks, S.G. Prevention, treatment and cure of HIV infection. Nat Rev Microbiol 21 , 657–670 (2023). https://doi.org/10.1038/s41579-023-00914-1
Download citation
Accepted : 12 May 2023
Published : 21 June 2023
Issue Date : October 2023
DOI : https://doi.org/10.1038/s41579-023-00914-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
The possible mechanisms of cu and zn in the treatment and prevention of hiv and covid-19 viral infection.
- Shatha A Albalawi
- Raneem A Albalawi
- Mohamed S. Abdel-Maksoud
Biological Trace Element Research (2024)
Making genome editing a success story in Africa
- Hussein M. Abkallo
- Patrick Arbuthnot
- Charles Wondji
Nature Biotechnology (2024)
PrEPping the skin
- Andrea Du Toit
Nature Reviews Microbiology (2023)
AZD5582 plus SIV-specific antibodies reduce lymph node viral reservoirs in antiretroviral therapy-suppressed macaques
- Amir Dashti
- Sophia Sukkestad
- Ann Chahroudi
Nature Medicine (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Common HIV treatments may aid Alzheimer's disease patients
Alzheimer's disease (AD) currently afflicts nearly seven million people in the U.S. With this number expected to grow to nearly 13 million by 2050, the lack of meaningful therapies represents a major unmet medical need. Scientists at Sanford Burnham Prebys have now identified promising real-world links between common HIV drugs and a reduced incidence of AD. The study, led by Jerold Chun, M.D., Ph.D., was published in Pharmaceuticals .
Chun's new research builds on his lab's landmark publication in Nature in 2018 that described how somatic gene recombination in neurons can produce thousands of new gene variants within Alzheimer's disease brains. Importantly, it also revealed for the first time how the Alzheimer's-linked gene, APP, is recombined by using the same type of enzyme found in HIV.
The enzyme, called reverse transcriptase (RT), copies RNA molecules and changes them into complementary DNA duplicates that can then be inserted back into DNA, producing permanent sequence changes within the cell's DNA blueprint.
HIV and many other viruses rely on RT to hijack a host's cells to establish a chronic infection, so drugs that block the RT enzyme's activity have become a common part of treatment cocktails for keeping HIV at bay.
The brain appears to have its own RTs that are different from those in viruses, and the research team wondered if inhibiting brain RTs with HIV drugs actually helps AD patients.
To assess the link between real-world RT inhibitor exposure and AD in humans, the team analyzed anonymized medical records with prescription claims from more than 225,000 control and HIV-positive patients, and found that RT inhibitor exposure was associated with a statistically significant reduced incidence and prevalence of AD.
"Thus, we looked at HIV-positive individuals taking RT inhibitors and other combined antiretroviral therapies as they aged, and asked the question: How many of them got Alzheimer's disease?" says Chun. "And the answer is that there were many fewer than might have been expected compared to the general population."
Of the more than 225,000 individuals with claims data in the study, just shy of 80,000 were HIV-positive individuals over the age of 60. More than 46,000 had taken RT inhibitors during a nearly three-year observation period from 2016 to 2019. The data was obtained through a collaboration with health information technology and clinical research firm IQVIA, led by Tiffany Chow, M.D.
In living persons with HIV, there were 2.46 Alzheimer's disease diagnoses per 1,000 persons among HIV-positive individuals taking these inhibitors, versus 6.15 for the general population. This control group was represented by more than 150,000 HIV-negative patients over the age of 60 with medical insurance claims related to treatment for the common cold.
"You cannot feasibly run a prospective clinical trial with this number of patients," Chun adds. "This approach is a way to look at how a drug can act on a large patient population."
Chun underscores that the drugs patients took in this retrospective study were designed to counter RT activity in HIV and likely only had a limited effect on many different possible forms of the enzyme active in the brain.
"What we're looking at now is very crude," says Chun. "The clear next step for our lab is to identify which versions of RTs are at work in the AD brain so that more targeted treatments can be discovered, while prospective clinical trials of currently available RT inhibitors on persons with early AD should be pursued."
Jerold Chun, M.D. Ph.D., is a professor in the Center for Genetic Disorders and Aging Research at Sanford Burnham Prebys.
Additional authors on the study include Tiffany W. Chow, Mark Raupp, Matthew W. Reynolds, Siying Li and Gwendolyn E. Kaeser.
The work was supported by the National Institute on Aging -- NIH (R01AG071465, R01AG065541 and R56AG073965), the Shaffer Family Foundation and the Bruce Ford & Anne Smith Bundy Foundation.
- HIV and AIDS
- Infectious Diseases
- Alzheimer's Research
- Diseases and Conditions
- Alzheimer's
- Disorders and Syndromes
- Antiretroviral drug
- Alzheimer's disease
- Vaccination
- Dementia with Lewy bodies
- Urinary incontinence
- Huntington's disease
Story Source:
Materials provided by Sanford-Burnham Prebys . Note: Content may be edited for style and length.
Journal Reference :
- Tiffany W. Chow, Mark Raupp, Matthew W. Reynolds, Siying Li, Gwendolyn E. Kaeser, Jerold Chun. Nucleoside Reverse Transcriptase Inhibitor Exposure Is Associated with Lower Alzheimer’s Disease Risk: A Retrospective Cohort Proof-of-Concept Study . Pharmaceuticals , 2024; 17 (4): 408 DOI: 10.3390/ph17040408
Cite This Page :
Explore More
- Food in Sight? The Liver Is Ready!
- Acid Reflux Drugs and Risk of Migraine
- Do Cells Have a Hidden Communication System?
- Mice Given Mouse-Rat Brains Can Smell Again
- How Do Birds Flock? New Aerodynamics
- Cancer: Epigenetic Origin Without DNA Mutation
- Climate Change Driving Biodiversity Loss
- Why Can't Robots Outrun Animals?
- Evolution of Gliding in Marsupials
- Novel One-Dimensional Superconductor
Trending Topics
Strange & offbeat.
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
Nih research matters.
April 23, 2024
Research in Context: Treating depression
Finding better approaches.
While effective treatments for major depression are available, there is still room for improvement. This special Research in Context feature explores the development of more effective ways to treat depression, including personalized treatment approaches and both old and new drugs.

Everyone has a bad day sometimes. People experience various types of stress in the course of everyday life. These stressors can cause sadness, anxiety, hopelessness, frustration, or guilt. You may not enjoy the activities you usually do. These feelings tend to be only temporary. Once circumstances change, and the source of stress goes away, your mood usually improves. But sometimes, these feelings don’t go away. When these feelings stick around for at least two weeks and interfere with your daily activities, it’s called major depression, or clinical depression.
In 2021, 8.3% of U.S. adults experienced major depression. That’s about 21 million people. Among adolescents, the prevalence was much greater—more than 20%. Major depression can bring decreased energy, difficulty thinking straight, sleep problems, loss of appetite, and even physical pain. People with major depression may become unable to meet their responsibilities at work or home. Depression can also lead people to use alcohol or drugs or engage in high-risk activities. In the most extreme cases, depression can drive people to self-harm or even suicide.
The good news is that effective treatments are available. But current treatments have limitations. That’s why NIH-funded researchers have been working to develop more effective ways to treat depression. These include finding ways to predict whether certain treatments will help a given patient. They're also trying to develop more effective drugs or, in some cases, find new uses for existing drugs.
Finding the right treatments
The most common treatments for depression include psychotherapy, medications, or a combination. Mild depression may be treated with psychotherapy. Moderate to severe depression often requires the addition of medication.
Several types of psychotherapy have been shown to help relieve depression symptoms. For example, cognitive behavioral therapy helps people to recognize harmful ways of thinking and teaches them how to change these. Some researchers are working to develop new therapies to enhance people’s positive emotions. But good psychotherapy can be hard to access due to the cost, scheduling difficulties, or lack of available providers. The recent growth of telehealth services for mental health has improved access in some cases.
There are many antidepressant drugs on the market. Different drugs will work best on different patients. But it can be challenging to predict which drugs will work for a given patient. And it can take anywhere from 6 to 12 weeks to know whether a drug is working. Finding an effective drug can involve a long period of trial and error, with no guarantee of results.
If depression doesn’t improve with psychotherapy or medications, brain stimulation therapies could be used. Electroconvulsive therapy, or ECT, uses electrodes to send electric current into the brain. A newer technique, transcranial magnetic stimulation (TMS), stimulates the brain using magnetic fields. These treatments must be administered by specially trained health professionals.
“A lot of patients, they kind of muddle along, treatment after treatment, with little idea whether something’s going to work,” says psychiatric researcher Dr. Amit Etkin.
One reason it’s difficult to know which antidepressant medications will work is that there are likely different biological mechanisms that can cause depression. Two people with similar symptoms may both be diagnosed with depression, but the causes of their symptoms could be different. As NIH depression researcher Dr. Carlos Zarate explains, “we believe that there’s not one depression, but hundreds of depressions.”
Depression may be due to many factors. Genetics can put certain people at risk for depression. Stressful situations, physical health conditions, and medications may contribute. And depression can also be part of a more complicated mental disorder, such as bipolar disorder. All of these can affect which treatment would be best to use.
Etkin has been developing methods to distinguish patients with different types of depression based on measurable biological features, or biomarkers. The idea is that different types of patients would respond differently to various treatments. Etkin calls this approach “precision psychiatry.”
One such type of biomarker is electrical activity in the brain. A technique called electroencephalography, or EEG, measures electrical activity using electrodes placed on the scalp. When Etkin was at Stanford University, he led a research team that developed a machine-learning algorithm to predict treatment response based on EEG signals. The team applied the algorithm to data from a clinical trial of the antidepressant sertraline (Zoloft) involving more than 300 people.

EEG data for the participants were collected at the outset. Participants were then randomly assigned to take either sertraline or an inactive placebo for eight weeks. The team found a specific set of signals that predicted the participants’ responses to sertraline. The same neural “signature” also predicted which patients with depression responded to medication in a separate group.
Etkin’s team also examined this neural signature in a set of patients who were treated with TMS and psychotherapy. People who were predicted to respond less to sertraline had a greater response to the TMS/psychotherapy combination.
Etkin continues to develop methods for personalized depression treatment through his company, Alto Neuroscience. He notes that EEG has the advantage of being low-cost and accessible; data can even be collected in a patient’s home. That’s important for being able to get personalized treatments to the large number of people they could help. He’s also working on developing antidepressant drugs targeted to specific EEG profiles. Candidate drugs are in clinical trials now.
“It’s not like a pie-in-the-sky future thing, 20-30 years from now,” Etkin explains. “This is something that could be in people's hands within the next five years.”
New tricks for old drugs
While some researchers focus on matching patients with their optimal treatments, others aim to find treatments that can work for many different patients. It turns out that some drugs we’ve known about for decades might be very effective antidepressants, but we didn’t recognize their antidepressant properties until recently.
One such drug is ketamine. Ketamine has been used as an anesthetic for more than 50 years. Around the turn of this century, researchers started to discover its potential as an antidepressant. Zarate and others have found that, unlike traditional antidepressants that can take weeks to take effect, ketamine can improve depression in as little as one day. And a single dose can have an effect for a week or more. In 2019, the FDA approved a form of ketamine for treating depression that is resistant to other treatments.
But ketamine has drawbacks of its own. It’s a dissociative drug, meaning that it can make people feel disconnected from their body and environment. It also has the potential for addiction and misuse. For these reasons, it’s a controlled substance and can only be administered in a doctor’s office or clinic.
Another class of drugs being studied as possible antidepressants are psychedelics. These include lysergic acid diethylamide (LSD) and psilocybin, the active ingredient in magic mushrooms. These drugs can temporarily alter a person’s mood, thoughts, and perceptions of reality. Some have historically been used for religious rituals, but they are also used recreationally.
In clinical studies, psychedelics are typically administered in combination with psychotherapy. This includes several preparatory sessions with a therapist in the weeks before getting the drug, and several sessions in the weeks following to help people process their experiences. The drugs are administered in a controlled setting.
Dr. Stephen Ross, co-director of the New York University Langone Health Center for Psychedelic Medicine, describes a typical session: “It takes place in a living room-like setting. The person is prepared, and they state their intention. They take the drug, they lie supine, they put on eye shades and preselected music, and two therapists monitor them.” Sessions last for as long as the acute effects of the drug last, which is typically several hours. This is a healthcare-intensive intervention given the time and personnel needed.
In 2016, Ross led a clinical trial examining whether psilocybin-assisted therapy could reduce depression and anxiety in people with cancer. According to Ross, as many as 40% of people with cancer have clinically significant anxiety and depression. The study showed that a single psilocybin session led to substantial reductions in anxiety and depression compared with a placebo. These reductions were evident as soon as one day after psilocybin administration. Six months later, 60-80% of participants still had reduced depression and anxiety.
Psychedelic drugs frequently trigger mystical experiences in the people who take them. “People can feel a sense…that their consciousness is part of a greater consciousness or that all energy is one,” Ross explains. “People can have an experience that for them feels more ‘real’ than regular reality. They can feel transported to a different dimension of reality.”
About three out of four participants in Ross’s study said it was among the most meaningful experiences of their lives. And the degree of mystical experience correlated with the drug’s therapeutic effect. A long-term follow-up study found that the effects of the treatment continued more than four years later.
If these results seem too good to be true, Ross is quick to point out that it was a small study, with only 29 participants, although similar studies from other groups have yielded similar results. Psychedelics haven’t yet been shown to be effective in a large, controlled clinical trial. Ross is now conducting a trial with 200 people to see if the results of his earlier study pan out in this larger group. For now, though, psychedelics remain experimental drugs—approved for testing, but not for routine medical use.
Unlike ketamine, psychedelics aren’t considered addictive. But they, too, carry risks, which certain conditions may increase. Psychedelics can cause cardiovascular complications. They can cause psychosis in people who are predisposed to it. In uncontrolled settings, they have the risk of causing anxiety, confusion, and paranoia—a so-called “bad trip”—that can lead the person taking the drug to harm themself or others. This is why psychedelic-assisted therapy takes place in such tightly controlled settings. That increases the cost and complexity of the therapy, which may prevent many people from having access to it.
Better, safer drugs
Despite the promise of ketamine or psychedelics, their drawbacks have led some researchers to look for drugs that work like them but with fewer side effects.
Depression is thought to be caused by the loss of connections between nerve cells, or neurons, in certain regions of the brain. Ketamine and psychedelics both promote the brain’s ability to repair these connections, a quality called plasticity. If we could understand how these drugs encourage plasticity, we might be able to design drugs that can do so without the side effects.

Dr. David Olson at the University of California, Davis studies how psychedelics work at the cellular and molecular levels. The drugs appear to promote plasticity by binding to a receptor in cells called the 5-hydroxytryptamine 2A receptor (5-HT2AR). But many other compounds also bind 5-HT2AR without promoting plasticity. In a recent NIH-funded study, Olson showed that 5-HT2AR can be found both inside and on the surface of the cell. Only compounds that bound to the receptor inside the cells promoted plasticity. This suggests that a drug has to be able to get into the cell to promote plasticity.
Moreover, not all drugs that bind 5-HT2AR have psychedelic effects. Olson’s team has developed a molecular sensor, called psychLight, that can identify which compounds that bind 5-HT2AR have psychedelic effects. Using psychLight, they identified compounds that are not psychedelic but still have rapid and long-lasting antidepressant effects in animal models. He’s founded a company, Delix Therapeutics, to further develop drugs that promote plasticity.
Meanwhile, Zarate and his colleagues have been investigating a compound related to ketamine called hydroxynorketamine (HNK). Ketamine is converted to HNK in the body, and this process appears to be required for ketamine’s antidepressant effects. Administering HNK directly produced antidepressant-like effects in mice. At the same time, it did not cause the dissociative side effects and addiction caused by ketamine. Zarate’s team has already completed phase I trials of HNK in people showing that it’s safe. Phase II trials to find out whether it’s effective are scheduled to begin soon.
“What [ketamine and psychedelics] are doing for the field is they’re helping us realize that it is possible to move toward a repair model versus a symptom mitigation model,” Olson says. Unlike existing antidepressants, which just relieve the symptoms of depression, these drugs appear to fix the underlying causes. That’s likely why they work faster and produce longer-lasting effects. This research is bringing us closer to having safer antidepressants that only need to be taken once in a while, instead of every day.
—by Brian Doctrow, Ph.D.
Related Links
- How Psychedelic Drugs May Help with Depression
- Biosensor Advances Drug Discovery
- Neural Signature Predicts Antidepressant Response
- How Ketamine Relieves Symptoms of Depression
- Protein Structure Reveals How LSD Affects the Brain
- Predicting The Usefulness of Antidepressants
- Depression Screening and Treatment in Adults
- Serotonin Transporter Structure Revealed
- Placebo Effect in Depression Treatment
- When Sadness Lingers: Understanding and Treating Depression
- Psychedelic and Dissociative Drugs
References: An electroencephalographic signature predicts antidepressant response in major depression. Wu W, Zhang Y, Jiang J, Lucas MV, Fonzo GA, Rolle CE, Cooper C, Chin-Fatt C, Krepel N, Cornelssen CA, Wright R, Toll RT, Trivedi HM, Monuszko K, Caudle TL, Sarhadi K, Jha MK, Trombello JM, Deckersbach T, Adams P, McGrath PJ, Weissman MM, Fava M, Pizzagalli DA, Arns M, Trivedi MH, Etkin A. Nat Biotechnol. 2020 Feb 10. doi: 10.1038/s41587-019-0397-3. Epub 2020 Feb 10. PMID: 32042166. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. Ross S, Bossis A, Guss J, Agin-Liebes G, Malone T, Cohen B, Mennenga SE, Belser A, Kalliontzi K, Babb J, Su Z, Corby P, Schmidt BL. J Psychopharmacol . 2016 Dec;30(12):1165-1180. doi: 10.1177/0269881116675512. PMID: 27909164. Long-term follow-up of psilocybin-assisted psychotherapy for psychiatric and existential distress in patients with life-threatening cancer. Agin-Liebes GI, Malone T, Yalch MM, Mennenga SE, Ponté KL, Guss J, Bossis AP, Grigsby J, Fischer S, Ross S. J Psychopharmacol . 2020 Feb;34(2):155-166. doi: 10.1177/0269881119897615. Epub 2020 Jan 9. PMID: 31916890. Psychedelics promote neuroplasticity through the activation of intracellular 5-HT2A receptors. Vargas MV, Dunlap LE, Dong C, Carter SJ, Tombari RJ, Jami SA, Cameron LP, Patel SD, Hennessey JJ, Saeger HN, McCorvy JD, Gray JA, Tian L, Olson DE. Science . 2023 Feb 17;379(6633):700-706. doi: 10.1126/science.adf0435. Epub 2023 Feb 16. PMID: 36795823. Psychedelic-inspired drug discovery using an engineered biosensor. Dong C, Ly C, Dunlap LE, Vargas MV, Sun J, Hwang IW, Azinfar A, Oh WC, Wetsel WC, Olson DE, Tian L. Cell . 2021 Apr 8: S0092-8674(21)00374-3. doi: 10.1016/j.cell.2021.03.043. Epub 2021 Apr 28. PMID: 33915107. NMDAR inhibition-independent antidepressant actions of ketamine metabolites. Zanos P, Moaddel R, Morris PJ, Georgiou P, Fischell J, Elmer GI, Alkondon M, Yuan P, Pribut HJ, Singh NS, Dossou KS, Fang Y, Huang XP, Mayo CL, Wainer IW, Albuquerque EX, Thompson SM, Thomas CJ, Zarate CA Jr, Gould TD. Nature . 2016 May 26;533(7604):481-6. doi: 10.1038/nature17998. Epub 2016 May 4. PMID: 27144355.
Connect with Us
- More Social Media from NIH

IMAGES
VIDEO
COMMENTS
Emory Health Sciences. (2023, July 26). New findings offer potential breakthrough in HIV cure research. ScienceDaily. Retrieved April 22, 2024 from www.sciencedaily.com / releases / 2023 / 07 ...
Researchers a step closer to a cure for HIV. A new study shows virus-like particle can effectively 'shock and kill' latent HIV reservoir in those living with chronic HIV. By 2030, the World Health ...
National Ryan White Conference on HIV Care & Treatment; AIDS 2020 (23rd International AIDS Conference Virtual) ... 73 countries gathered in Denver and virtually from March 3-6 this year for CROI, an annual scientific meeting on the latest research that can help accelerate global progress in the response to HIV and other infectious diseases ...
Future focus. Investing in innovative strategies that meet the needs of individuals won't just be key to ending the HIV/AIDS pandemic by 2030. It will also help to ensure that global health ...
ViiV is trying to develop a version of cabotegravir to be given every four months and, ultimately, one every six months. The company aims to bring the four-month version to market for preventing H ...
A brief description of three types of agents under study for HIV treatment and future directions for HIV treatment research from NIAID. ... Diseases & Conditions HIV/AIDS Treatment. ... NIAID continues to support research to develop new drugs with unique mechanisms of action for daily antiretroviral therapy. Such drugs likely would be effective ...
Reducing Pill Burden with Single Tablet Regimens. In the early days of the HIV epidemic, high pill burden made successful adherence to treatment challenging. 5 Selective non-adherence to a regimen ...
Interview with Dr. Anthony Fauci on progress made during the past four decades of the HIV/AIDS pandemic and ongoing efforts to end this threat. 18m 44s Download. The dramatic saga of the acquired ...
An effective and scalable cure strategy is a top priority for the HIV research field; this Review discusses recent advances, knowledge gaps, and priority research areas for the next 5 years.
Post-exposure Prophylaxis. Post-exposure prophylaxis (PEP) is a short course of HIV medicines taken soon after a possible exposure to HIV [ 25 ]. Every hour counts. For the treatment to be effective, the course should begin within 72 h after exposure to HIV; otherwise, it will not have any effect [ 25 ].
Advances in HIV/AIDS Research. HIV virions budding and releasing from an infected cell. NIAID, NIH. For an update on what medical science is doing to fight the global HIV/AIDS pandemic, read a Parade article by NIH Director Francis S. Collins and NIAID Director Anthony S. Fauci, AIDS in 2010: How We're Living with HIV.
JASON BEAUBIEN, BYLINE: HIV/AIDS has gotten pushed out of the headlines recently. And while the annual number of new HIV infections has declined in recent years, the disease is still a significant ...
R.T. Gandhi and OthersN Engl J Med 2023;389:2468-2476. A 70-year-old woman with advanced HIV infection was evaluated because of cough, shortness of breath, and malaise. Eleven months earlier, she ...
HIV and AIDS information and facts. Read latest medical articles and view educational videos on AIDS and HIV symptoms and treatments. Stay informed about new developments on the AIDS/HIV front.
Thanks to innovative research, scientists learned how the HIV virus that causes AIDS replicates and how the immune system responds to the virus. Today, many people with HIV take just one pill a day to suppress the virus, and treatment is continuing to evolve. In this video, Dr. Stacey Rizza, Mayo Clinic infectious disease physician and HIV ...
This latest research and guidance are being presented at a time when progress towards ending the global AIDS epidemic has lagged, after the COVID-19 pandemic; but the response is rapidly catching up, with some countries now charting a path to end AIDS, including Australia, Botswana, Eswatini, Rwanda, United Republic of Tanzania, and Zimbabwe ...
In January 2021, the FDA approved the first long-acting injectable treatment for adults with HIV. Cabenuva is a combo of two drugs ( cabotegravir and rilpivirine) that you take as a shot once a ...
The latest news on HIV, Aids, HIV research, Aids Research, Aids Studies and HIV medicine. ... long-acting injectable treatment with cabotegravir and rilpivirine (LAI) is superior to oral standard ...
Between 510,000 and 860,000 people died from HIV in 2021, according to the UNAIDS update. Cabotegravir is the latest WHO-recommended drug that protects against HIV infection. In January 2021, the ...
The HIV research community is led by scientists with deep personal commitments to improving the lives of people with and affected by HIV. Our collective decades of work have generated HIV testing, prevention and treatment options beyond what we could have imagined in the 1980s. Those advances enable NIAID to explore new frontiers: expanding HIV prevention and treatment modalities, increasing ...
AIDS Research and Treatment publishes original research articles and review articles focused on all aspects of HIV and AIDS, from the molecular basis of the disease to translational and clinical research, prevention and education. ... Latest Articles More articles. Research Article. 30 Jan 2024.
Herpes simplex virus 2 (HSV-2) is a common subtype of herpes simplex virus that is transmitted through sexual contact. The Centers for Disease Control and Prevention estimates that 18.6 million people aged 15 years and older United States live with HSV-2. In severe cases, HSV-2 may lead to life-threatening or long-term complications.
MSN
Research shows that hearing aids can be an effective treatment for tinnitus among people who have both tinnitus and hearing loss, which is much more common among older adults. An estimated one ...
Its own bill for landmark trials of a four-drug combination treatment for drug-resistant tuberculosis came to €34m (£29m). Current estimates for research and development of new medicines range ...
But in new research published Monday, Dr. Bhonsale and his colleagues examined data on more than 67,000 patients with A-fib who were treated at the center, nearly one-quarter of whom were under ...
Nature Medicine (2023) The development of antiretroviral therapy for the prevention and treatment of HIV infection has been marked by a series of remarkable successes. However, the efforts to ...
Sanford-Burnham Prebys. "Common HIV treatments may aid Alzheimer's disease patients." ScienceDaily. ScienceDaily, 16 April 2024. <www.sciencedaily.com / releases / 2024 / 04 / 240416125313.htm ...
Its specialists provide compassionate, comprehensive care for more than 100,000 adults and children every year and access to more than 200 active clinical trials at any given time. Its innovative research program engages more than 240 scientists at UC Davis who work collaboratively to advance discovery of new tools to diagnose and treat cancer.
This special Research in Context feature explores the development of more effective ways to treat depression, including personalized treatment approaches and both old and new drugs. Choat / Adobe Stock. Everyone has a bad day sometimes. People experience various types of stress in the course of everyday life. These stressors can cause sadness ...