Analysis of risk factors of preeclampsia in pregnant women with chronic hypertension and its impact on pregnancy outcomes
- Xiaorui Nie 1 ,
- Zijie Xu 1 &
- Hong Ren 1
BMC Pregnancy and Childbirth volume 24 , Article number: 307 ( 2024 ) Cite this article
190 Accesses
Metrics details
To investigate the risk factors and maternal and fetal outcomes of preeclampsia after pregnancy in patients with primary chronic hypertension.
A total of 500 singleton pregnant women with a history of hypertension who were admitted for delivery at our Hospital from March 2015 to May 2022 were retrospectively collected by random sampling and divided into the non-occurrence group ( n = 200) and the occurrence group ( n = 300) according to whether they were complicated by preeclampsia. Afterward, the general data and the pregnancy-related data of patients were collected for comparison.
The univariate analysis showed significant differences between the non-occurrence group and the occurrence group in terms of the proportion of preeclampsia history (4.00% VS 24.67%, χ2 = 37.383, P < 0.001), duration of hypertension > 3 years (18.00% VS 31.67%, χ2 = 11.592, P < 0.001), systemic therapy (20.50% VS 10.00%, χ2 = 10.859, P < 0.001), gestational age at admission [37.72 (34.10, 38.71) VS 35.01 (31.91, 37.42) weeks, Z = -9.825, P < 0.001]. Meanwhile, the multivariate analysis showed that a history of preeclampsia (OR = 6.796, 95% CI: 3.575 ∼ 10.134, χ2 = 8.234, P < 0.001), duration of hypertension > 3 years (OR = 3.456, 95% CI: 2.157 ∼ 5.161, χ2 = 9.348, P < 0.001), and a lack of systemic antihypertensive treatment (OR = 8.983, 95% CI: 7.735 ∼ 9.933, χ2 = 9.123, P < 0.001) were risk factors for chronic hypertension complicated by preeclampsia during pregnancy.
A history of preeclampsia, a longer duration of hypertension, and a lack of systematic antihypertensive treatment are risk factors for chronic hypertension complicated by preeclampsia during pregnancy. The occurrence of preeclampsia in pregnant women with chronic hypertension increases the incidence of maternal HELLP syndrome and fetal distress.
Peer Review reports

Introduction
Chronic hypertension complicated by pregnancy refers to the occurrence of elevated blood pressure before pregnancy or before 20 weeks of gestation, with no significant aggravation during pregnancy, or diagnosed as hypertension after 20 weeks of gestation while blood pressure remains elevated for 12 weeks after delivery [ 1 ]. Studies have shown that about 6% of pregnant women in China suffer from chronic hypertension [ 2 ], and the number of patients is increasing worldwide. Meanwhile, the incidence of chronic hypertension complicated by pregnancy has increased by 67% in recent years according to foreign reports [ 3 ]. Chronic hypertension complicated by pregnancy not only affects the organ function of pregnant women but also increases the risk of adverse pregnancy outcomes. A study showed that pregnant women with a history of chronic hypertension have at least a nearly 5-fold to 6-fold increased risk of cardiovascular and cerebrovascular diseases and multi-organ dysfunction than those with normal blood pressure [ 4 ]. More studies also indicate that women with primary hypertension experience earlier and more severe maternal and fetal complications once complicated by preeclampsia after pregnancy [ 5 ]. The previous research conducted by Bramham K et al. [ 6 ] in the United States on 822 pregnant women with chronic hypertension already demonstrated that the potential risk of severe intrauterine hypoxia, fetal growth restriction, and even stillbirth was significantly increased in pregnant women with preeclampsia [ 7 ]. The incidence of preeclampsia in the general Chinese pregnant population is about 3 − 5%, while the incidence of preeclampsia in pregnant women with chronic hypertension can reach 17 − 25% [ 8 ]. In contrast, foreign studies have indicated an incidence of 13 − 40% for preeclampsia in women with chronic hypertension [ 9 ].
Preeclampsia is a complex and dynamic process, and its exact pathogenesis remains unclear. Currently, it is believed that the infiltration of trophoblast cells and the remodeling of uterine spiral arteries during placental formation are important links in the occurrence of preeclampsia [ 2 ]. Some scholars have proposed the “two-stage” theory for the occurrence of preeclampsia [ 10 ] and further developed the “six-stage” model [ 11 ]. In addition to causing adverse pregnancy outcomes, the occurrence of preeclampsia also has some impact on the long-term prognosis of pregnant patients, such as depression [ 12 , 13 , 14 , 15 ]. Therefore, it is of great significance to identify high-risk factors for chronic hypertension complicated by preeclampsia, screen out high-risk pregnant women promptly, and take early intervention measures for the pregnancy outcomes and long-term prognosis of both mother and child.
Most current research and clinical trials focus on statistical analysis of pregnancy-induced hypertension with or without preeclampsia and comparisons of different pregnancy outcomes. However, there is limited research on the special population of chronic hypertension with preeclampsia. Therefore, the risk factors for the occurrence of preeclampsia in pregnant women with chronic hypertension have not been clearly identified. This study is designed to analyze the population of pregnant women with chronic hypertension and explore the high-risk factors for the occurrence of preeclampsia, as well as its impact on maternal and fetal outcomes, so as to better guide the screening of high-risk groups before pregnancy and reduce the occurrence of adverse maternal and fetal outcomes.
Study subjects and methods
Study subjects.
A total of 500 singleton pregnant women with a history of hypertension who were admitted for delivery at Beijing Chaoyang District Maternal and Child Health Care Hospital from March 2015 to May 2022 were retrospectively collected by random sampling and divided into the non-occurrence group ( n = 200) and the occurrence group ( n = 300) based on whether they developed concurrent preeclampsia. Inclusion Criteria: (1) Patients with a singleton pregnancy; (2) Patients diagnosed with chronic hypertension complicated by pregnancy (without preeclampsia) or chronic hypertension complicated by pregnancy with preeclampsia. Exclusion Criteria: (1) Patients with secondary hypertension such as renal hypertension and pheochromocytoma diagnosed during pregnancy or postpartum; (2) Patients with normal maternal blood pressure during follow-up at 12 weeks after delivery; (3) Patients with malformed infants found in the second trimester requiring induction of labor; (4) Patients with multiple pregnancies.
Study methods
Diagnostic criteria for chronic hypertension: Diastolic blood pressure ≥ 90 mmHg and/or systolic blood pressure ≥ 140 mmHg before pregnancy or before 20 weeks of gestation, with the latter seeing persistent blood pressure ≥ 140/90 mmHg 3 months after delivery.
Criteria for cardiovascular risk stratification of chronic hypertension: (1) Mild (low risk): diastolic blood pressure = 90 ∼ 99 mmHg, systolic blood pressure = 140 ∼ 159 mmHg, without target organ damage; (2) Moderate (medium risk): diastolic blood pressure = 100 ∼ 109 mmHg, systolic blood pressure = 160 ∼ 179 mmHg; (3) Severe (high risk): diastolic blood pressure ≥ 110 mmHg, systolic blood pressure ≥ 180 mmHg, without target organ damage, or diastolic blood pressure = 90 ∼ 99 mmHg, systolic blood pressure = 140 ∼ 150 mmHg, with diabetes or target organ damage.
Diagnostic criteria for preeclampsia: (1) Presence of proteinuria after 20 weeks of gestation; (2) pregnant women with hypertension and proteinuria before 20 weeks of gestation suddenly developed elevated blood pressure or increased proteinuria; (3) Elevated creatinine and liver enzymes, or platelets < 100 × 109/L, or accompanied by right upper abdominal pain, headache, and other symptoms.
Treatment methods for hypertension [ 16 ]: All pregnant women were treated with low-dose aspirin (100 mg/d) before 20 weeks of gestation. For patients with mild hypertension, low-dose aspirin alone was used; for patients with blood pressure ≥ 150/100 mmHg for more than 2 times and target organ damage, antihypertensive drugs were added; for patients with a sharp increase in blood pressure or proteinuria, additional tests were conducted to determine if they had preeclampsia. Those with preeclampsia were hospitalized for observation, and if the condition stabilized, they could continue the pregnancy and be discharged with follow-up. However, they could continue hospitalization if severe preeclampsia develops. Low-dose aspirin was discontinued after 36 weeks of gestation in pregnant women without preeclampsia, with premature infants and low birth weight infants transferred to the neonatal ICU for treatment.
Data collection
General characteristics data of the patients were collected, including: age, pre-delivery BMI, previous pregnancy and delivery history, previous blood pressure control, family history of hypertension, and history of previous preeclampsia in pregnancy. Delivery-related data included: newborn birth weight, newborn Apgar score results, and the occurrence of related maternal and fetal complications.
The newborn Apgar score is used to determine the severity of neonatal asphyxia and asphyxia, which is based on five signs within one minute after birth, i.e., heart rate, respiration, muscle tone, laryngeal reflex, and skin color, each of which scored from 0 to 2, with a maximum score of 10. Scores of 8 ∼ 10: normal; 4 ∼ 7: mild asphyxia; 0 ∼ 3: severe asphyxia. The lower the score, the more severe acidosis and hypoxemia, and the higher the mortality rate, which required immediate rescue to improve asphyxia [ 17 ].
Common maternal complications include placental abruption, postpartum hemorrhage, and HELLP syndrome, while fetal complications mainly include intrauterine growth restriction (IUGR), fetal distress, abnormal amniotic fluid volume, abnormal diastolic blood flow signals, premature delivery, and stillbirth. (1) Diagnostic criteria for placental abruption: the placental abruption surface does not exceed 1/3 of the placental area, the signs are not obvious, the main symptoms are a large amount of vaginal bleeding, no abdominal pain or mild abdominal pain, and the fetal heart rate is normal [ 18 ]; (2) Diagnostic criteria for postpartum hemorrhage: the amount of blood loss reaches or exceeds 500 mL within 24 h after delivery of the fetus [ 18 ]. (3) Diagnostic criteria for fetal growth restriction (FGR): fetal head circumference, femur length, and abdominal circumference are measured by ultrasound, and fetal weight (EFW) is estimated by substituting the HadlockC formula, and FGR is diagnosed if EFW is less than the 10th percentile of the same gestational age [ 19 ]. (4) Diagnostic criteria for fetal distress: the fetus in the womb due to acute or chronic hypoxia endangering health and life syndrome, mainly manifested as abnormal fetal heart rate during delivery, amniotic fluid meconium contamination and abnormal fetal heart rate monitoring (late deceleration, frequent mutation deceleration), abnormal fetal movement (hypoxia in the initial stage of frequent fetal movements, then weakened and reduced, and then disappeared). Intrauterine distress is diagnosed if any of the above are achieved [ 18 ]. (5) Diagnostic criteria for oligohydramnios: those with less than 300 ml of amniotic fluid in the third trimester of pregnancy are called oligohydramnios. The prenatal diagnosis of oligohydramnios is mainly determined by the maximum depth (AFV) of the dark area of the amniotic fluid and the index of amniotic fluid (AFI) by color ultrasound, with AFV ≦ 2 cm being oligohydramnios and AFI ≦ 5 cm being the standard for oligohydramnios. Hypohydramnios can be clearly diagnosed if the total amount is less than 300 ml when the membrane is broken and the amount of amniotic fluid is collected by various methods after delivery. Polyhydramnios: The amount of amniotic fluid during pregnancy is more than 2000 ml, which is called polyhydramnios. The prenatal diagnosis of polyhydramnios is mainly determined by the maximum depth (AFV) of the dark area of the amniotic fluid and the amniotic fluid index (AFI) monitored by color ultrasound, AFV ≧ 8 cm is diagnosed as polyhydramnios, and AFI ≧ 25 cm is diagnosed as polyhydramnios. A total amount of more than 2000 mL of amniotic fluid collected postpartum confirms the diagnosis of polyhydramnios [ 18 ].(6) Premature delivery: It refers to delivery at 28 weeks of gestation and less than 37 weeks of gestation, resulting in premature infants with a birth weight between 1,000 and 2,499 g [ 20 ].
Statistical analysis
SPSS 26.00 software was used for statistical analysis. The K-S method was used for the normality test, measurement data complying with normality were expressed as (x ± s), and the independent sample t-test was used for inter-group comparison. Count data were expressed as frequency (n) or rate (%), with the χ2 test used for the comparison of general data and the rank-sum test for the comparison of grade data. Meanwhile, the skewed distribution was described using the median (interquartile range), and the rank-sum test was used for inter-group comparison. In addition, multivariate analysis was conducted using Logistic regression, and the ROC curve was used to analyze the predictive value of each factor for the occurrence of preeclampsia in patients with chronic hypertension during pregnancy. The significance level was set at α = 0.05.
Comparison of general data between patients with/without preeclampsia
The comparison of general data between the two groups showed that the mean age of the group without preeclampsia was 33.69 ± 5.80, with 104 primiparas, a median pre-delivery BMI of 30.00 (27.38, 32.23) kg/m2, and a history of preeclampsia ( n = 8); the mean age of the group with preeclampsia was 32.74 ± 5.25, with 146 primiparas, the median pre-delivery BMI of 31.51 (29.21, 34.91) kg/m2, and a history of preeclampsia ( n = 74). There were significant differences between the two groups in the history of preeclampsia (4.00% VS 24.67%, χ 2 = 37.383, P < 0.001), duration of hypertension > 3 years (18.00% VS 31.67%, χ 2 = 11.592, P < 0.001), systemic therapy (20.50% VS 10.00%, χ 2 = 10.859, P < 0.001), and gestational age at admission (37.72 (34.10, 38.71) VS 35.01 (31.91, 37.42) weeks, Z = -9.825, P < 0.001). However, no significant difference was found in factors such as age, proportion of primiparous, pre-delivery BMI, proportion of positive antiphospholipid antibody, gravidity, parity, and family history of hypertension between the two groups ( P > 0.05), as shown in Table 1 .
Multivariate logistic regression analysis of patients with chronic hypertension complicated by preeclampsia
A logistic regression analysis model was constructed with the presence or absence of preeclampsia as the dependent variable (occurrence = 1, absence = 0), and statistically significant factors in the aforementioned analysis as independent variables [history of preeclampsia (presence = 1, absence = 0), duration of hypertension > 3 years (presence = 1, absence = 0), performing systemic therapy (presence = 1, absence = 0), and gestational age at admission entered at the original value]. The findings revealed that a history of preeclampsia (OR = 6.796, 95% CI: 3.575 ∼ 10.134, χ 2 = 8.234, P < 0.001), duration of hypertension > 3 years (OR = 3.456, 95% CI: 2.157 ∼ 5.161, χ 2 = 9.348, P < 0.001), and a lack of systemic antihypertensive treatment (OR = 8.983, 95% CI: 7.735 ∼ 9.933, χ 2 = 9.123, P < 0.001) were risk factors for the occurrence of chronic hypertension complicated by preeclampsia. See Table 2 .
Predictive value of duration of hypertension, history of preeclampsia, and systemic therapy for chronic hypertension complicated by preeclampsia in pregnant women
The duration of hypertension, history of preeclampsia, and systemic therapy were of certain value in predicting the occurrence of preeclampsia in pregnant women with chronic hypertension ( P < 0.05). Specifically, the area under the curve (AUC) of the duration of hypertension, history of preeclampsia, and systemic therapy in predicting preeclampsia in pregnant women with chronic hypertension were 0.752 (95% CI: 0.683, 0.792), 0.746 (95% CI: 0.679, 0.821), and 0.756 (95% CI: 0.691, 0.823), respectively. In terms of combined prediction, the combined prediction effect was better than that of the single prediction, and the AUC of the three factors combined for predicting the occurrence of preeclampsia in pregnant women with chronic hypertension was 0.856 (95%CI: 0.790, 0.898), as shown in Table 3 .
Effect of preeclampsia on pregnancy outcomes in pregnant women with chronic hypertension
A comparison of pregnancy outcomes between pregnant women with and without preeclampsia in chronic hypertension showed that there were significant differences in the occurrence of HELLP syndrome (1 VS 22 cases, χ 2 = 12.769, P < 0.001), gestational age at delivery [38.10 (36.11, 38.91) VS 35.61 (32.42, 37.61) weeks, Z = -9.874, P < 0.001], newborn birth weight (3200.32 ± 956.81 VS 2513.41 ± 903.82 g, t = -7.452, P < 0.001), 1-min newborn Apgar score (9.41 ± 0.54 VS 8.46 ± 0.33 points, t = 9.417, P < 0.001), 5-min newborn Apgar score (9.67 ± 0.45 VS 9.12 ± 0.24 points, t = 8.593, P < 0.001), umbilical artery S/D value [2.21 (1.91, 2.50) VS 2.61 (2.22, 2.93), Z =-9.523, P < 0.001], abnormal amniotic fluid volume (2 VS 15 cases, χ 2 = 5.846, P = 0.016), and fetal distress (4 VS 42 cases, χ 2 = 20.686, P < 0.001) were significantly different. However, there was no significant difference in postpartum hemorrhage, placental abruption, stillbirth, and IUGR between the two groups ( P > 0.05). See Table 4 .
Chronic hypertension is a lifelong disease that affects the function of various organs in the body and is the leading disease that endangers people’s health, it has been reported in literature that the incidence of adverse pregnancy outcomes increases with the elevated blood pressure levels in pregnant women with different degrees of hypertension [ 21 ]. The relationship between hypertension and preeclampsia (PE) is traceable. In 2017, Boriboonhirunsarn et al. [ 22 ] performed a statistical analysis on 300 singleton pregnant women diagnosed with primary hypertension, which showed an incidence of 43.3% for concurrent PE in pregnant women with primary hypertension, and the incidence of adverse fetal outcomes increased. Numerous reports have shown that pregnant women complicated by PE see a significantly increased risk of maternal complications such as placental abruption and fetal growth restriction, leading to poor perinatal outcomes like premature delivery [ 23 ], cardiovascular disease [ 24 ]. Therefore, monitoring and management of pregnant women with chronic hypertension complicated by preeclampsia has become a common concern worldwide.
Some studies have found [ 25 ] that the aggregation of risk factors greatly increases the occurrence of adverse maternal and fetal outcomes in preeclampsia. Therefore, identifying high-risk factors for preeclampsia and strengthening prenatal monitoring of high-risk patients have become a hot topic in obstetric research. In our study, we identified several risk factors according to analyses of univariate cox regression and multiple cox regression, among them, the discovery on the risky nature of PE history aligned with previous established researches [ 26 , 27 ]. Though the negative effects of hypertension duration and patient age have been proved in PE development among hypertension patients [ 28 ], there is still a gap in related researches based on chronic hypertension population. We successfully illustrated the promoting effect of hypertension duration (> 3 years) to PE occurrence on chronic hypertension subjects, while the patient age showed no significant contribution, according to the investigation outcomes of this study. Moreover, for pregnant women with mild to moderate primary hypertension, strict and reasonable control of blood pressure levels can also reduce the incidence of preeclampsia [ 29 ], it seems to be equally applicable to pregnant subjects with chronic hypertension. The findings of this study demonstrated that untreated chronic hypertension and a longer course of hypertension increase the incidence of preeclampsia in patients with chronic hypertension.
In addition, it has been shown that family history of preeclampsia, history of preeclampsia, pregnancy interval ≥ 10 years, and primiparity are all risk factors for developing preeclampsia [ 29 ]. This study also found that a history of preeclampsia is a risk factor for developing preeclampsia after pregnancy in patients with primary chronic hypertension, which is consistent with previous research findings.
During a normal pregnancy, umbilical artery blood flow resistance gradually decreases with increasing gestational age, reflecting an increase in maternal-fetal blood exchange and normal fetal growth and development [ 30 ]. Studies have shown that the umbilical artery resistance index (S/D) should be ≤ 3 after 30 weeks of gestation [ 31 ]. This index is also a major parameter reflecting the fetal-placental circulation status and plays a role in predicting pregnancy outcomes. If this value shows no downward trend or even increases in the third trimester of pregnancy, it indicates increased blood flow resistance and increased placental perfusion pressure. This may manifest as reversed or absent umbilical artery blood flow signals, and in severe cases, it can lead to fetal hypoxia and distress.
In patients with chronic hypertension after pregnancy, due to long-term maintenance of high blood pressure levels, the small blood vessels throughout the body are in a state of spasm, affecting multiple organs and causing corresponding changes in their functions. Once complicated by preeclampsia, maternal and fetal complications (e.g., placental abruption, postpartum hemorrhage, HELLP syndrome) tend to occur earlier and more severely [ 32 ]. In order to balance the risks between the mother and the perinatal outcomes, they often lead to preterm termination of pregnancy, resulting in an increase in preterm delivery and cesarean section. The findings of this study also revealed that pregnant women with chronic hypertension complicated by preeclampsia experience a higher proportion of HELLP syndrome and shorter gestational age at delivery, which is consistent with the above findings.
Chronic hypertension complicated with preeclampsia is a common cause of iatrogenic preterm delivery, and the gestational age directly affects the maturity of the fetus, which is crucial for perinatal outcomes. Many studies have reported that preeclampsia increases the risk of fetal complications (e.g., fetal growth restriction, fetal distress, stillbirth, etc.). A statistical analysis of clinical mortality in China comparing pre-eclampsia with or without chronic hypertension suggested [ 33 ] that the probability of neonatal death due to chronic hypertension complicated with preeclampsia may be the highest among the studies of the classification of hypertensive disorders of pregnancy at various stages. Some scholars believe that chronic hypertension itself may not necessarily increase the incidence of IUGR. Only when preeclampsia causes insufficient early placental blood flow in the mother, it may become a key factor in the occurrence of fetal growth restriction [ 34 ]. The findings of of this study revealed that newborn birth weight and Apgar scores were relatively lower and the incidence of fetal distress events was higher in patients with chronic hypertension complicated by preeclampsia. However, there was no significant increase in the risk of complications such as severe fetal growth restriction and stillbirth.
Of course, this study comes with some limitations. Firstly, it is a single-center retrospective analysis, relying on medical records and laboratory query systems for data collection, and there was missing data for some pregnant women. Secondly, since its sample size is relatively small, further large-scale studies are needed to increase the persuasiveness. Specifically, further multi-center large-scale prospective studies are needed in the future.
In conclusion, a history of pre-eclampsia, long duration of hypertension, and a lack of systematic antihypertensive treatment are risk factors for chronic hypertension complicated with pre-eclampsia during pregnancy. The occurrence of preeclampsia in pregnant women with chronic hypertension increases the incidence of maternal HELLP syndrome and fetal distress.
Data availability
All data generated or analyzed during this study are included in this article.
ACOG Practice Bulletin No. 203 Summary: chronic hypertension in pregnancy. Obstet Gynecol. 2019;133:215–9. https://doi.org/10.1097/AOG.0000000000003021 .
Article Google Scholar
Ye C, Ruan Y, Zou L, Li G, Li C, Chen Y, et al. The 2011 survey on hypertensive disorders of pregnancy (HDP) in China: prevalence, risk factors, complications, pregnancy and perinatal outcomes. PLoS ONE. 2014;9:e100180. https://doi.org/10.1371/journal.pone.0100180 .
Article CAS PubMed PubMed Central Google Scholar
Martin JA, Hamilton BE, Ventura SJ, Osterman MJ, Kirmeyer S, Mathews TJ, et al. Births: final data for 2009. Natl Vital Stat Rep. 2011;60:1–70.
PubMed Google Scholar
Gilbert WM, Young AL, Danielsen B. Pregnancy outcomes in women with chronic hypertension: a population-based study. J Reprod Med. 2007;52:1046–51.
Zheng DM, Li SH, Wang J, Li C. Effect of hypertensive disorder complicating pregnancy on neonatal birth outcome and umbilical artery blood flow. Med J Chin People’s Liberation Army. 2013;38:757–9. doi: CNKI:SUN:JFJY.0.2013-09-013.
Google Scholar
Bramham K, Parnell B, Nelson-Piercy C, Seed PT, Poston L, Chappell LC. Chronic hypertension and pregnancy outcomes: systematic review and meta-analysis. BMJ. 2014;348:g2301. https://doi.org/10.1136/bmj.g2301 .
Article PubMed PubMed Central Google Scholar
Glover AV, Tita A, Biggio JR, Anderson SB, Harper LM. Incidence and risk factors for Postpartum severe hypertension in women with underlying chronic hypertension. Am J Perinatol. 2019;36:737–41. https://doi.org/10.1055/s-0038-1675153 .
Article PubMed Google Scholar
Kumar M, Singh A, Garg R, Goel M, Ravi V. Hypertension during pregnancy and risk of stillbirth: challenges in a developing country. J Matern Fetal Neonatal Med. 2021;34:3915–21. https://doi.org/10.1080/14767058.2019.1702943 .
American College of Obstetricians and Gynecologists, Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and gynecologists’ Task Force on hypertension in pregnancy. Obstet Gynecol. 2013;122:1122–31. https://doi.org/10.1097/01.AOG.0000437382.03963.88 .
Aouache R, Biquard L, Vaiman D, Miralles F. Oxidative stress in Preeclampsia and placental diseases. Int J Mol Sci. 2018;19:1496. https://doi.org/10.3390/ijms19051496 .
Redman C. The six stages of pre-eclampsia. Pregnancy Hypertens. 2014;4:246. https://doi.org/10.1016/j.preghy.2014.04.020 .
Youn H, Lee S, Han SW, Kim LY, Lee TS, Oh MJ, et al. Obstetric risk factors for depression during the postpartum period in South Korea: a nationwide study. J Psychosom Res. 2017;102:15–20. https://doi.org/10.1016/j.jpsychores.2017.09.003 .
McVittie C, Craig S, Temple M. A conversation analysis of communicative changes in a time-limited psychotherapy group for mothers with post-natal depression. Psychother Res. 2020;30:1048–60. https://doi.org/10.1080/10503307.2019.1694721 .
Pálinkás A, Sándor J, Papp M, Kőrösi L, Falusi Z, Pál L, et al. Associations between untreated depression and secondary health care utilization in patients with hypertension and/or diabetes. Soc Psychiatry Psychiatr Epidemiol. 2019;54:255–76. https://doi.org/10.1007/s00127-018-1545-7 .
Li Z, Li Y, Chen L, Chen P, Hu Y. Prevalence of Depression in patients with hypertension: a systematic review and Meta-analysis. Med (Baltim). 2015;94:e1317. https://doi.org/10.1097/MD.0000000000001317 .
Article CAS Google Scholar
Obstetrics and Gynecology Branch of the Chinese Medical Association. Guidelines for the Diagnosis and Treatment of Hypertensive Disorders in Pregnancy. (2020). Chinese Journal of Obstetrics and Gynecology. 2020;55, 227–238. https://doi.org/10.3760/cma.j.cn112141-20200114-00039 .
Simon LV, Hashmi MF, Bragg BN, APGAR Score. 2023 May 22. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–.
Xie X, Kong B, Duan T et al. (2018). Obstetrics and Gynecology (9th ed.) [M]. People’s Medical Publishing House. July 18, 2018.
Albu AR, Horhoianu IA, Dumitrascu MC. Growth assessment in diagnosis of fetal growth restriction. Rev J Med Life. 2014;7:150–4.
CAS Google Scholar
Bian XM, Fu CW. Definition classification and diagnosis of premature delivery. Progress Obstet Gynecol. 2011;20:164–5. doi: CNKI:SUN:XDFC. 0.2011-03-003.
Wang XX, Song XL. Effect of different degrees of hypertensive disorder complicating pregnancy combined with cervical infection on pregnancy outcome and postoperative infection. Maternal Child Health Care China. 2016;31:3247–9. https://doi.org/10.7620/zgfybj.j.issn.1001-4411.2016 .
Boriboonhirunsarn D, Pradyachaipimol A, Viriyapak B. Incidence of superimposed preeclampsia among pregnant Asian women with chronic hypertension. Hypertens Pregnancy. 2017;36:226–31. https://doi.org/10.1080/10641955.2017.1311340 .
Sibai BM, Caritis SN, Thom E, Klebanoff M, McNellis D, Rocco L, et al. Prevention of preeclampsia with low-dose aspirin in healthy, nulliparous pregnant women. The National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med. 1993;329:1213–8. https://doi.org/10.1056/NEJM199310213291701 .
Article CAS PubMed Google Scholar
Mongraw-Chaffin ML, Cirillo PM, Cohn BA. Preeclampsia and cardiovascular disease death: prospective evidence from the child health and development studies cohort. Hypertension. 2010;56:166–71. https://doi.org/10.1161/HYPERTENSIONAHA.110.150078 .
Williams B, Masi S, Wolf J, Schmieder RE. Facing the challenge of lowering blood pressure and cholesterol in the same patient: report of a Symposium at the European Society of Hypertension. Cardiol Ther. 2020;9:19–34. https://doi.org/10.1007/s40119-019-00159-1 .
Wang XL, Yang SY, Zeng XY, Chen FZ. Effect of blood pressure control level during pregnancy on pregnancy outcomes in pregnant women with mild to moderate chronic hypertension. Chin J Hypertens. 2021;29:268–71. https://doi.org/10.16439/j.issn.1673-7245.2021.03.012 .
Wang JL. Clinical analysis of pregnant women with chronic hypertension. J Med Forum. 2014;28:123–4. doi: CNKI:SUN:HYYX.0.2014-10-059.
Teng XH, Pan SL. Relationship between maternal age and high risk factors of pregnancy and pregnancy outcomes. J Practical Obstet Gynecol. 2017;33:692–6. doi: CNKI:SUN:SFCZ.0.2017-09-019.
Lecarpentier E, Tsatsaris V, Goffinet F, Cabrol D, Sibai B, Haddad B. Risk factors of superimposed preeclampsia in women with essential chronic hypertension treated before pregnancy. PLoS ONE. 2013;8:e62140. https://doi.org/10.1371/journal.pone.0062140 .
Xiao HY, Wang YM. Clinical Value of Nursing Intervention for Diabetic Nephropathy Based on Maslow Hierarchy Theory. Chin J Gen Pract. 2019;17:1065–8. doi: CNKI:SUN:SYQY.0.2019-06-049.
Ayati S, Vahidroodsari F, Talebian M. Maternal death due to Placenta Percreta with bladder involvement: a Case Report. Tehran Univ Med J. 2011. b26a817249d1442fa9de7b6335385e85.
Yu S, Ren Q, Wu W. Effects of losartan on expression of monocyte chemoattractant protein-1 (MCP-1) in hyperuricemic nephropathy rats. J Recept Signal Transduct Res. 2015;35:458–61. https://doi.org/10.3109/10799893.2015.1006332 .
Li XM, Chen DJ, Li XY, Wang X, Gong JJ, Tang WT, et al. Clinical comparison of simple preeclampsia and chronic hypertension complicated by Preeclampsia. J Trop Med. 2016;16:1494–7. https://doi.org/10.3969/j.issn.1672-3619.2016.12.004 .
Benigni A, Gregorini G, Frusca T, Chiabrando C, Ballerini S, Valcamonico A, et al. Effect of low-dose aspirin on fetal and maternal generation of thromboxane by platelets in women at risk for pregnancy-induced hypertension. N Engl J Med. 1989;321:357–62. https://doi.org/10.1056/NEJM198908103210604 .
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Department of obstetrics and gynecology Beijing Chaoyang District Maternal and Child Health Care Family Planning Service Center (Beijing Chaoyang District Maternal and Child Health Care Hospital), No. 25 Huaweili, Panjiayuan Street, Chaoyang District, Beijing, 100021, China
Xiaorui Nie, Zijie Xu & Hong Ren
You can also search for this author in PubMed Google Scholar
Contributions
Nie XR designed and performed the experiments, analyzed the data, and wrote the manuscript; Xu ZJ and Ren H performed the experiments; all authors performed experiments and wrote the manuscript; all authors have read and approved the manuscript.
Corresponding author
Correspondence to Hong Ren .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics approval and consent to participate
This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Beijing Chaoyang District Maternal and Child Health Care Hospital. Written informed consent was obtained from all participants.
Consent for publication
Additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Nie, X., Xu, Z. & Ren, H. Analysis of risk factors of preeclampsia in pregnant women with chronic hypertension and its impact on pregnancy outcomes. BMC Pregnancy Childbirth 24 , 307 (2024). https://doi.org/10.1186/s12884-024-06476-1
Download citation
Received : 12 December 2023
Accepted : 01 April 2024
Published : 24 April 2024
DOI : https://doi.org/10.1186/s12884-024-06476-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Preeclampsia
- Chronic hypertension
- Pregnancy outcome
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Effects of a Case Management Program for Women With Pregnancy-Induced Hypertension
Affiliations.
- 1 PhD, RN, Assistant Professor, Institute of Community Health Care, College of Nursing, National Yang Ming Chiao Tung University, Taipei, Taiwan.
- 2 PhD, RN, Professor, School of Nursing, National Defense Medical Center, Taipei, Taiwan.
- 3 BSN, RN, Case Manager, Department of Nursing, National Cheng Kung University Hospital, Tainan, Taiwan.
- 4 PhD, RN, Distinguished Professor, Institute of Community Health Care, College of Nursing, National Yang Ming Chiao Tung University, Taipei, Taiwan.
- 5 PhD, RN, Associate Professor, Department of Nursing, College of Medicine, National Cheng Kung University, and National Cheng Kung University Hospital, Tainan, Taiwan.
- PMID: 34432727
- DOI: 10.1097/jnr.0000000000000450
Background: Pregnancy-induced hypertension (PIH) is a leading cause of maternal and fetal morbidity and mortality. Although case management programs have been proposed to improve maternal and fetal outcomes in high-risk pregnancies, limited data are available regarding the effect of case management on women with PIH.
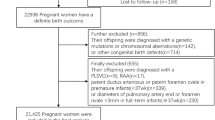
Purpose: The aim of this study was to evaluate the effect of an antepartum case management program on stress, anxiety, and pregnancy outcomes in women with PIH.
Methods: A quasi-experimental research design was employed. A convenience sample of women diagnosed with PIH, including preeclampsia, was recruited from outpatient clinics at a medical center in southern Taiwan. Sixty-two women were assigned randomly to either the experimental group (n = 31) or the control group (n = 31). The experimental group received case management for 8 weeks, and the control group received routine clinical care. Descriptive statistics, independent t or Mann-Whitney U tests, chi-square or Fisher's exact tests, paired t test, and generalized estimating equations were used to analyze the data.
Results: The average age of the participants was 35.1 years (SD = 4.5). No significant demographic or clinical differences were found between the control and experimental groups. The results of the generalized estimating equations showed significantly larger decreases in stress and anxiety in the experimental group than in the control group. No significant differences were identified between the two groups with respect to infant birth weeks, infant birth weight, average number of medical visits, or frequency of hospitalization.
Conclusions/implications for practice: The nurse-led case management program was shown to have short-term positive effects on the psychosocial outcomes of a population of Taiwanese patients with PIH. These results have important clinical implications for the healthcare administered to pregnant women, particularly in terms of improving the outcomes in those with PIH.
Copyright © 2021 The Authors. Published by Wolters Kluwer Health, Inc.
Publication types
- Randomized Controlled Trial
- Case Management
- Hypertension, Pregnancy-Induced* / therapy
- Pre-Eclampsia* / therapy
- Pregnancy Outcome
- Prenatal Care
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 09 January 2020
Association of circulating saturated fatty acids with the risk of pregnancy-induced hypertension: a nested case–control study
- Xinping Li 1 ,
- Yichao Huang 2 ,
- Wenxin Zhang 1 ,
- Chenhui Yang 1 ,
- Weijie Su 2 ,
- Xiaomei Chen 1 ,
- Aifen Zhou 3 ,
- Xia Huo 2 ,
- Wei Xia 1 ,
- Shunqing Xu 1 ,
- Da Chen 2 &
- Yuanyuan Li 1
Hypertension Research volume 43 , pages 412–421 ( 2020 ) Cite this article
190 Accesses
9 Citations
1 Altmetric
Metrics details
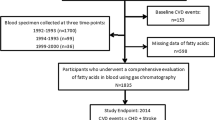
Circulating saturated fatty acids (SFAs) have been associated with cardiovascular disease. However, little is known about the relationship of SFAs with the risk of pregnancy-induced hypertension (PIH). We conducted a nested case–control study to examine the associations between circulating SFAs and the risk of PIH. A total of 92 PIH cases were matched to 184 controls by age (±2 years) and infant sex from a birth cohort study conducted in Wuhan, China. Levels of circulating fatty acids in plasma were measured using gas chromatography–mass spectrometry. Conditional logistic regressions were conducted to calculate odds ratios (ORs) and 95% confidence intervals (95% CIs). Even-chain SFAs, including myristic acid (14:0) and palmitic acid (16:0), were positively associated with the risk of PIH [ORs (95% CIs): 2.92 (1.27, 6.74) for 14:0 and 2.85 (1.18, 6.89) for 16:0, % by wt]. In contrast, higher levels of very-long-chain SFAs, including arachidic acid (20:0), behenic acid (22:0), and lignoceric acid (24:0), were associated with a lower risk of PIH [ORs (95% CIs): 0.40 (0.17, 0.92) for 20:0, 0.30 (0.12, 0.71) for 22:0 and 0.26 (0.11, 0.64) for 24:0, μg/mL]. For odd-chain SFAs, including pentadecanoic acid (15:0) and heptadecanoic acid (17:0), no significant difference was observed. Our results provided convincing evidence that different subclasses of SFAs showed diverse effects on the risk of PIH. This suggests that dietary very-long-chain SFAs may be a novel means by which to prevent hypertension. Future studies are required to confirm these associations and elucidate the underlying mechanisms.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
251,40 € per year
only 20,95 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others

The association between dietary fatty acid intake and the risk of developing preeclampsia: a matched case–control study
Association between Plasma N-6 Polyunsaturated Fatty Acids Levels and the Risk of Cardiovascular Disease in a Community-based Cohort Study
Association between lipid profile in early pregnancy and the risk of congenital heart disease in offspring: a prospective cohort study
Khan KS, Wojdyla D, Say L, Gulmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: a systematic review. Lancet. 2006;367:1066–74.
PubMed Google Scholar
Ghulmiyyah L, Sibai B. Maternal mortality from preeclampsia/eclampsia. Semin Perinatol. 2012;36:56–9.
Article Google Scholar
Jwa SC, Arata N, Sakamoto N, Watanabe N, Aoki H, Kurauchi-Mito A, et al. Prediction of pregnancy-induced hypertension by a shift of blood pressure class according to the JSH 2009 guidelines. Hypertens Res. 2011;34:1203–8.
Kristensen JH, Basit S, Wohlfahrt J, Damholt MB, Boyd HA. Pre-eclampsia and risk of later kidney disease: nationwide cohort study. BMJ. 2019;365:l1516.
PubMed PubMed Central Google Scholar
Behrens I, Basit S, Melbye M, Lykke JA, Wohlfahrt J, Bundgaard H, et al. Risk of post-pregnancy hypertension in women with a history of hypertensive disorders of pregnancy: nationwide cohort study. BMJ. 2017;358:j3078.
Bellamy L, Casas JP, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007;335:974.
Mol BWJ, Roberts CT, Thangaratinam S, Magee LA, de Groot CJM, Hofmeyr GJ. Pre-eclampsia. Lancet 2016;387:999–1011.
Hu J, Li Y, Zhang B, Zheng T, Li J, Peng Y, et al. Impact of the 2017 ACC/AHA guideline for high blood pressure on evaluating gestational hypertension-associated risks for newborns and mothers. Circ Res 2019;125:184–94.
CAS PubMed Google Scholar
Alsnes IV, Vatten LJ, Fraser A, Bjorngaard JH, Rich-Edwards J, Romundstad PR, et al. Hypertension in pregnancy and offspring cardiovascular risk in young adulthood: prospective and sibling studies in the HUNT study (Nord-Trondelag Health Study) in Norway. Hypertension. 2017;69:591–8.
Lane-Cordova AD, Gunderson EP, Carnethon MR, Catov JM, Reiner AP, Lewis CE, et al. Pre-pregnancy endothelial dysfunction and birth outcomes: The Coronary Artery Risk Development in Young Adults (CARDIA) study. Hypertens Res. 2018;41:282–9.
Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006;114:82–96.
Eyre H, Kahn R, Robertson RM. Preventing cancer, cardiovascular disease, and diabetes: a common agenda for theAmerican Cancer Society, the American Diabetes Association, and the American Heart Association. CA Cancer J Clin. 2004;54:190–207.
Micha R, Mozaffarian D. Saturated fat and cardiometabolic risk factors, coronary heart disease, stroke, and diabetes: a fresh look at the evidence. Lipids. 2010;45:893–905.
CAS PubMed PubMed Central Google Scholar
de Souza RJ, Mente A, Maroleanu A, Cozma AI, Ha V, Kishibe T, et al. Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies. BMJ. 2015;351:h3978.
Howard BV, Van Horn L, Hsia J, Manson JE, Stefanick ML, Wassertheil-Smoller S, et al. Low-fat dietary pattern and risk of cardiovascular disease: the Women's Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006;295:655–66.
Ascherio A, Rimm EB, Giovannucci EL, Colditz GA, Rosner B, Willett WC, et al. A prospective study of nutritional factors and hypertension among US men. Circulation. 1992;86:1475–84.
Fretts AM, Mozaffarian D, Siscovick DS, Djousse L, Heckbert SR, King IB, et al. Plasma phospholipid saturated fatty acids and incident atrial fibrillation: the Cardiovascular Health Study. J Am Heart Assoc. 2014;3:e000889.
Zheng JS, Sharp SJ, Imamura F, Koulman A, Schulze MB, Ye Z, et al. Association between plasma phospholipid saturated fatty acids and metabolic markers of lipid, hepatic, inflammation and glycaemic pathways in eight European countries: a cross-sectional analysis in the EPIC-InterAct study. BMC Med. 2017;15:203.
Forouhi NG, Koulman A, Sharp SJ, Imamura F, Kroger J, Schulze MB, et al. Differences in the prospective association between individual plasma phospholipid saturated fatty acids and incident type 2 diabetes: the EPIC-InterAct case–cohort study. Lancet Diabetes Endocrinol. 2014;2:810–8.
Patel PS, Sharp SJ, Jansen E, Luben RN, Khaw KT, Wareham NJ, et al. Fatty acids measured in plasma and erythrocyte-membrane phospholipids and derived by food-frequency questionnaire and the risk of new-onset type 2 diabetes: a pilot study in the European Prospective Investigation into Cancer and Nutrition (EPIC)-Norfolk cohort. Am J Clin Nutr. 2010;92:1214–22.
Zheng ZJ, Folsom AR, Ma J, Arnett DK, McGovern PG, Eckfeldt JH. Plasma fatty acid composition and 6-year incidence of hypertension in middle-aged adults: the Atherosclerosis Risk in Communities (ARIC) study. Am J Epidemiol. 1999;150:492–500.
Afonso MS, Lavrador MS, Koike MK, Cintra DE, Ferreira FD, Nunes VS, et al. Dietary interesterified fat enriched with palmitic acid induces atherosclerosis by impairing macrophage cholesterol efflux and eliciting inflammation. J Nutr Biochem. 2016;32:91–100.
Matejcic M, Lesueur F, Biessy C, Renault AL, Mebirouk N, Yammine S, et al. Circulating plasma phospholipid fatty acids and risk of pancreatic cancer in a large European cohort. Int J Cancer. 2018;143:2437–48.
Santaren ID, Watkins SM, Liese AD, Wagenknecht LE, Rewers MJ, Haffner SM, et al. Serum pentadecanoic acid (15:0), a short-term marker of dairy food intake, is inversely associated with incident type 2 diabetes and its underlying disorders. Am J Clin Nutr. 2014;100:1532–40.
Chiu YH, Bertrand KA, Zhang S, Laden F, Epstein MM, Rosner BA, et al. A prospective analysis of circulating saturated and monounsaturated fatty acids and risk of non-Hodgkin lymphoma. Int J Cancer. 2018;143:1914–22.
Malik VS, Chiuve SE, Campos H, Rimm EB, Mozaffarian D, Hu FB, et al. Circulating very-long-chain saturated fatty acids and incident coronary heart disease in US men and women. Circulation. 2015;132:260–8.
Lemaitre RN, Fretts AM, Sitlani CM, Biggs ML, Mukamal K, King IB, et al. Plasma phospholipid very-long-chain saturated fatty acids and incident diabetes in older adults: the Cardiovascular Health Study. Am J Clin Nutr. 2015;101:1047–54.
Yamagishi K, Iso H, Yatsuya H, Tanabe N, Date C, Kikuchi S, et al. Dietary intake of saturated fatty acids and mortality from cardiovascular disease in Japanese: the Japan Collaborative Cohort Study for Evaluation of Cancer Risk (JACC) Study. Am J Clin Nutr. 2010;92:759–65.
Filipovic MG, Aeschbacher S, Reiner MF, Stivala S, Gobbato S, Bonetti N, et al. Whole blood omega-3 fatty acid concentrations are inversely associated with blood pressure in young, healthy adults. J Hypertens. 2018;36:1548–54.
Bonaa KH, Bjerve KS, Straume B, Gram IT, Thelle D. Effect of eicosapentaenoic and docosahexaenoic acids on blood pressure in hypertension. A population-based intervention trial from the Tromso study. N. Engl J Med. 1990;322:795–801.
Dokholyan RS, Albert CM, Appel LJ, Cook NR, Whelton P, Hennekens CH. A trial of omega-3 fatty acids for prevention of hypertension. Am J Cardiol. 2004;93:1041–3.
Lim WY, Chong M, Calder PC, Kwek K, Chong YS, Gluckman PD, et al. Relations of plasma polyunsaturated Fatty acids with blood pressures during the 26th and 28th week of gestation in women of Chinese, Malay, and Indian ethnicity. Medicine. 2015;94:e571.
Begg DP, Sinclair AJ, Stahl LA, Premaratna SD, Hafandi A, Jois M, et al. Hypertension induced by omega-3 polyunsaturated fatty acid deficiency is alleviated by alpha-linolenic acid regardless of dietary source. Hypertens Res. 2010;33:808–13.
Qiao GH, Sun XZ. Increased plasma fatty acid binding protein 4 concentration at the first prenatal visit and its relevance to preeclampsia. Hypertens Res. 2018;41:763–9.
Brown MA, Lindheimer MD, de Swiet M, Van Assche A, Moutquin JM. The classification and diagnosis of the hypertensive disorders of pregnancy: statement from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Hypertens Pregnancy. 2001;20:Ix–xiv.
Folch J, Lees M, Sloane Stanley GH. A simple method for the isolation and purification of total lipides from animal tissues. J Biol Chem. 1957;226:497–509.
Mikolajczyk RT, Zhang J, Betran AP, Souza JP, Mori R, Gulmezoglu AM, et al. A global reference for fetal-weight and birthweight percentiles. Lancet. 2011;377:1855–61.
Association AD. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2011;34(Suppl 1):S62–9.
Google Scholar
Davenport MH, Ruchat SM, Poitras VJ, Jaramillo Garcia A, Gray CE, Barrowman N, et al. Prenatal exercise for the prevention of gestational diabetes mellitus and hypertensive disorders of pregnancy: a systematic review and meta-analysis. Br J Sports Med. 2018;52:1367–75.
Leng B, Jin Y, Li G, Chen L, Jin N. Socioeconomic status and hypertension: a meta-analysis. J Hypertens. 2015;33:221–9.
Simon JA, Fong J, Bernert JT Jr., Browner WS. Relation of smoking and alcohol consumption to serum fatty acids. Am J Epidemiol. 1996;144:325–34.
Lane-Cordova AD, Tedla YG, Carnethon MR, Montag SE, Dude AM, Rasmussen-Torvik LJ. Pre-pregnancy blood pressure and body mass index trajectories and incident hypertensive disorders of pregnancy. Pregnancy Hypertens. 2018;13:138–40.
Iwama N, Metoki H, Nishigori H, Mizuno S, Takahashi F, Tanaka K, et al. Association between alcohol consumption during pregnancy and hypertensive disorders of pregnancy in Japan: the Japan Environment and Children's Study. Hypertens Res. 2019;42:85–94.
Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B. 1995;57:289–300.
Zhou A, Xiong C, Hu R, Zhang Y, Bassig BA, Triche E, et al. Pre-pregnancy BMI, gestational weight gain, and the risk of hypertensive disorders of pregnancy: a cohort study in Wuhan, China. PLoS ONE. 2015;10:e0136291.
Lepsch J, Farias DR, Eshriqui I, Rebelo F, Dos Santos Vaz J, Adegboye AA, et al. Serum fatty acids are positively associated with changes in systemic blood pressure throughout pregnancy. Pregnancy Hypertens. 2018;13:7–13.
Kim SR, Jeon SY, Lee SM. The association of cardiovascular risk factors with saturated fatty acids and fatty acid desaturase indices in erythrocyte in middle-aged Korean adults. Lipids Health Dis. 2015;14:133.
Granger JP, Alexander BT, Bennett WA, Khalil RA. Pathophysiology of pregnancy-induced hypertension. Am J Hypertens. 2001;14:178s–85s.
Ali SM, Khalil RA. Genetic, immune and vasoactive factors in the vascular dysfunction associated with hypertension in pregnancy. Exp Opin Ther Targets. 2015;19:1495–515.
CAS Google Scholar
Grosch S, Schiffmann S, Geisslinger G. Chain length-specific properties of ceramides. Prog Lipid Res. 2012;51:50–62.
Kihara A. Very long-chain fatty acids: elongation, physiology and related disorders. J Biochem. 2012;152:387–95.
Harvey KA, Walker CL, Pavlina TM, Xu Z, Zaloga GP, Siddiqui RA. Long-chain saturated fatty acids induce pro-inflammatory responses and impact endothelial cell growth. Clin Nutr. 2010;29:492–500.
Jump DB, Tripathy S, Depner CM. Fatty acid-regulated transcription factors in the liver. Annu Rev Nutr. 2013;33:249–69.
Wahli W, Michalik L. PPARs at the crossroads of lipid signaling and inflammation. Trends Endocrinol Metab. 2012;23:351–63.
Siler SQ, Neese RA, Hellerstein MK. De novo lipogenesis, lipid kinetics, and whole-body lipid balances in humans after acute alcohol consumption. Am J Clin Nutr. 1999;70:928–36.
Crowder CM. Cell biology. Ceramides-friend or foe in hypoxia? Science. 2009;324:343–4.
Ngene NC, Moodley J. Role of angiogenic factors in the pathogenesis and management of pre-eclampsia. Int J Gynaecol Obstet. 2018;141:5–13.
Hartmann D, Lucks J, Fuchs S, Schiffmann S, Schreiber Y, Ferreiros N, et al. Long chain ceramides and very long chain ceramides have opposite effects on human breast and colon cancer cell growth. Int J Biochem Cell Biol. 2012;44:620–8.
Download references
Acknowledgements
We thank all the participants, staff, and students involved in the birth cohort study.
This study was supported by grants from the National Key Research and Development Plan (2016YFC0206700, 2016YFC0206203), the National Natural Science Foundation of China (91743103, 21437002, 91643207), the Fundamental Research Funds for the Central Universities, Huazhong University of Science and Technology (2018KFYXMPT00), and the Program for HUST Academic Frontier Youth Team (2018QYTD12).
Author information
Authors and affiliations.
Key Laboratory of Environment and Health, Ministry of Education & Ministry of Environmental Protection, and State Key Laboratory of Environmental Health, School of Public Health, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei, PR China
Xinping Li, Wenxin Zhang, Chenhui Yang, Yi Wu, Xiaomei Chen, Wei Xia, Shunqing Xu & Yuanyuan Li
School of Environment, Guangdong Key Laboratory of Environmental Pollution and Health, Jinan University, Guangzhou, Guangdong, PR China
Yichao Huang, Weijie Su, Xia Huo & Da Chen
Wuhan Medical & Healthcare Center for Women and Children, Wuhan, Hubei, PR China
You can also search for this author in PubMed Google Scholar
Corresponding authors
Correspondence to Da Chen or Yuanyuan Li .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary table 1, supplementary table 2, supplementary table 3, rights and permissions.
Reprints and permissions
About this article
Cite this article.
Li, X., Huang, Y., Zhang, W. et al. Association of circulating saturated fatty acids with the risk of pregnancy-induced hypertension: a nested case–control study. Hypertens Res 43 , 412–421 (2020). https://doi.org/10.1038/s41440-019-0383-7
Download citation
Received : 25 September 2019
Revised : 12 November 2019
Accepted : 03 December 2019
Published : 09 January 2020
Issue Date : May 2020
DOI : https://doi.org/10.1038/s41440-019-0383-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Blood pressure
- Gestational hypertension
- Pre-eclampsia
- Saturated fatty acids
This article is cited by
Comprehensive fatty acid fractionation profilling in preeclampsia: a case control study with multivariable analysis.
- Herlambang Herlambang
- Anggelia Puspasari
- Mas Rizky Anggun Adipurna Syamsunarno
BMC Pregnancy and Childbirth (2022)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

A CASE STUDY ON LIFE-THREATENING PREGNANCY-INDUCED HYPERTENSION IN PRETERM PREGNANCY AND MANAGEMENT CHALLENGES

Related Papers
Introduction: Hypertensive disorders of pregnancy are the most common causes of adverse maternal & perinatal outcomes. Such investigations in resource limited settings would help to have great design strategies in preventing maternal and perinatal morbidity and mortality. All women who presented with hypertensive disorders of pregnancy and delivered in the hospital and whose records were complete, were included in the study and divided into 5 groups namely, Gestational hypertension (GH), Mild pre-eclampsia (PE), Severe pre-eclampsia, Eclampsia and Chronic hypertension with superimposed pre-eclampsia (CHPE) based on their clinical presentation at admission. After excluding all incomplete data entries, the sample size was finalized at 200. Results: In this study, records of 2,989 women who delivered in our tertiary hospital were reviewed and of these, 256 women had hypertensive disorders of pregnancy. Fifty six of these women had either left the hospital against medical advice or their records were incomplete so their outcome could not be followed and hence were excluded from the study. Conclusion: Pre-eclampsia and Eclampsia still remains a major problem in developing countries. Pregnancy induced hypertension is one of the most extensively researched subjects in obstetrics. Still the etiology remains an enigma to us. Though the incidence of pre-eclampsia and eclampsia is on the decline, still it remains the major contributor to poor maternal and foetal outcome. The fact that pre-eclampsia, eclampsia is largely a preventable disease is established by the negligible incidence of pre-eclampsia and eclampsia with proper antenatal care and prompt treatment of pre-eclampsia. In preclampsia and eclampsia, pathology should be understood and that i-involves multiorgan dysfunction should be taken into account. The early use of antihypertensive drugs, optimum timing of delivery and strict fluid balance, anticonvulsants in cases of eclampsia will help to achieve successful outcome. Early transfer to specialist centre is important and the referral the referral centers should be well equipped to treat such critically ill patients.
IOSR Journals
Back Ground: Aim: The Aim of the study was to find out the incidence of PIH & Preeclampsia and to evaluate the risk factors, predictors of severity and obstetrical and perinatal outcome in severe preeclampsia and Eclampsia.. Place and duration Methodology: Out of total 8800 deliveries 880 were diagnosed to have pregnancy induced hypertension. Out of these 580 (66%) had gestational hypertension. 80(0.9%) cases had preeclampsia without severe features, 220(2.5%) cases had preeclampsia with severe features. The present study was conducted in 200 cases of preeclampsia with severe features. The cases were evaluated and managed as per the existing protocol in the department and Obstetrical and perinatal outcome were recorded and analyzed. Results: The incidence of pregnancy induced hypertension was 10% and preeclampsia 3.5% in our study. 50% had anemia and 30% had obesity as risk factors. Materanl mortality was seen in 12cases of severe preeclamsia, accounting to 50% of total maternal deaths in our centre. Other maternal complications were seen in 60% of cases.Most common was Eclamsia in 30% of cases followed by Abruption in 20% & DIC in 18% and 20% of cases required transfusion of blood & Blood components for thrombocytopenia and coagulation failure. 10% cases required ventilator support for dyspneoa. Perinatal mortality was seen in 16% of cases. Perinatal morality is due to premaurity, low birth weight and abruption. NICU admissions were required in 20% of cases because of severe birth Asphyxia. Conclusion: Regular antenatal checkup and regular blood pressure measurement will help in early detection of hypertensive cases. Treating anemia and educating women on significance of alarming symptoms will improve maternal and perinatal outcome. Hospitalisation, regular BP monitoring, investigations and timely delivery will improve significantly the maternal and perinatal outcome. A good maternal intensive care unit and neonatal intensive care unit will help to improve obstetrical and perinatal outcome in hypertensive disorders of pregnancy.
Hypertension in Pregnancy
Altaf shaikh
Corine Koopmans
https://www.ijhsr.org/IJHSR_Vol.11_Issue.1_Jan2021/IJHSR_Abstract.041.html
International Journal of Health Sciences and Research (IJHSR)
Background: Hypertension is one of the common medical complications of pregnancy & contributes significantly to maternal & perinatal morbidity & mortality. The World Health Organization estimates that at least one woman dies every seven minutes from complications of hypertensive disorders of pregnancy. Hence a study was undertaken to assess the impact of Pregnancy Induced Hypertension on fetal outcomes among mothers with PIH who delivered at tertiary care hospital, Dadra & Nagar Haveli. Method: It was a cross sectional study conducted at Shri Vinoba Bhave Civil Hospital, Silvassa, Dadra & Nagar Haveli from September to November 2020.The sample size of the study was 32. The data regarding demographic variables, obstetric history, clinical details & examinations, investigations & fetal outcomes was collected using Structured Interview Schedule. Result: In the present study, Gestational Hypertension was found to be 65.62%, Pre eclampsia was 28.12% and Eclampsia was found to be 6.25%. It was more prevalent among multipara mothers. The clinical representation of PIH showed that 71.87% mothers had pain in lower abdomen, 37.3% had pedal edema followed by 15.62% headache & 9.37% blurring of vision. Antihypertensive drugs (93.75%) were given to almost all the mothers whereas 9.37% were treated with anticonvulsant medicines. The most common fetal complications found were preterm births (43.75%) & LBW (37.5%). 28.12% babies required NICU admission due to various reasons whereas 6.25% neonatal deaths were reported. Conclusion: Pregnancy-related hypertensive disorders are common and adversely impact perinatal outcomes. Efforts should be made at both the community and hospital levels to increase awareness regarding hypertensive disorder of pregnancy and reduce its associated morbidity and mortality.
Clinical & Biomedical Research
Francisco Maximiliano Pancich Gallarreta
Scholar Science Journals
Background: Preeclampsia and eclampsia have been recognized as clinical entities since the times of Hippocrates. Pregnancy induced hypertension (PIH) is one of the commonest disorders associated with the increased risk of maternal and fetal complications. It is reported in the world literature that the incidence of eclampsia is on the decline, but still a menace in developing countries. Objectives: To study the maternal and foetal outcome in pregnancy induced hypertension. Material and Methods: A prospective randomized study was carried out A total of 100 pregnant women with PIH were enrolled in the study. A pre-tested interview tool was used to collect necessary information such as detailed history, clinical examination findings and investigations performed. Results were analysed using SPSS 13.0 Results: In the present study, the overall incidence of PIH was 8.96%, which includes preeclampsia in 7.26% and eclampsia in 1.70%. Preterm labour was the commonest maternal obstetrical complication observed in 18% of mild PIH and 48% of severe PIH cases. Prematurity was the commonest foetal complication seen in 17.99%, 47.62% and 52.63% of mild PIH, severe PIH and Eclampsia cases respectively. Conclusion: Pregnancy induced hypertension is a common medical disorder seen associated with pregnancy in the rural population, especially among young primigravidas, who remain unregistered during pregnancy. Maternal and fetal morbidity and mortality can be reduced by early recognition and institutional management.
American Journal of Pediatrics
Mustafa Captain
Archives of Gynecology and Obstetrics
Eray Çalışkan
Objective: The aim of the study was to determine the risk factors, prevalance, epidemiological parameters and maternal-perinatal outcome in pregnant women with hypertensive disorder. Materials and methods: A retrospective analysis was undertaken on 255 consecutive cases of hypertensive disorder in pregnancy who were managed at Kocaeli University, School of Medicine, Department of Obstetrics and Gynecology from June 1997 to November 2004. Demographic data involving age, parity, gestational week, clinical and laboratory findings were recorded from the medical files. Additionally delivery route, indications of cesarean section, fetal and maternal complications were determined. Statistical analysis was performed by SPSS programme using Kruskal Wallis nonparametric test, ANOVA (Analysis of variance) and chi-square tests. Results: Of 5,155 deliveries in our clinic during the defined period, 438 cases (8.49%) were managed as hypertensive disorder of pregnancy. Medical records of 255 cases could be avaliable. Of 255 cases, 138 patients (54.11%) were found to have severe preeclampsia while 88 cases (34.50%) were diagnosed as mild preeclampsia. Twenty-nine patients (11.37%) were suffering from chronic hypertension. Of 138 severely preeclamptic cases, 28 cases (11%) had eclamptic convulsion and another 28 patients (11%) were demonstrated to have HELLP syndrome. Intrauterine growth restriction, oligohydramnios, placental ablation were the obstetric complications in 75 (29.4%), 49 (19.2%), 19 (7.5%) cases, respectively. Additionally multiple pregnancy and gestational diabetes mellitus were noted in 5.9% (n:15) and 3.9% (n:10) of the patients. Delivery route was vaginal in 105 patients (41.2%) while 150 patients (58.8%) underwent cesarean section with the most frequent indication to be fetal distress in 69 cases (46%). Cesarean section rate seemed to be the lowest (48.3%) in chronic hypertensive women while the highest (63.8%) in severe preeclamptic patients. Maternal mortality occured in 3 cases (1.2%) and all of those cases were complicated with HELLP syndrome. Intracranial bleeding was the cause of maternal death in one case while the other two cases were lost due to acute renal failure and disseminated intravascular coagulation, respectively. Intrauterine fetal demise was recorded in 24 cases on admission. Ten fetuses died during the intrapartum period. Mean gestational age and birth weight were 28±3.5 and 1000±416 g, respectively in this group. In these ten women, five cases were diagnosed as HELLP syndrome, two were severely preeclamptic and three were eclamptic. Perinatal mortality rate was found to be 144/1,000 births Conclusion: Hypertensive disorder of pregnancy is associated with increased risk of maternal-perinatal adverse outcome. The complications of severe preeclampsia and eclampsia could be prevented by more widespread use of prenatal care, education of primary medical care personnel, prompt diagnosis of high-risk patients and timely referral to tertiary medical centers.
South African Family Practice
Nnabuike Chibuoke Ngene
RELATED PAPERS
Call/Wa 0857 9154 2283|cara belajar inggris pemula
kursusbahasainggris 0102
Revista Médica del Uruguay
Gonzalo Silveira
Journal of Vacuum Science & Technology B: Microelectronics and Nanometer Structures
Eric Harmon
Marize Malta
The Astrophysical Journal
Nature Communications
Heledd Griffiths
SPE Reservoir Simulation Symposium
Michael Edwards
SEG Technical Program Expanded Abstracts 2008
Gilles Lambaré
DESIDADES - Revista Científica da Infância, Adolescência e Juventude
H. Masud Taj
reza elvira junita
Energy Conversion and Management
Bilal Akash
Jurnal Media Informatika
Sundari Putri Lestari
Masa Zdralevic
2017 ASEE Annual Conference & Exposition Proceedings
John Marco Santiago
Ana Estévez-braun
DergiPark (Istanbul University)
Paul Gleirscher
Tópicos, Revista de Filosofía
paula arizpe
George P. Petropoulos
Proceedings of the Nutrition Society
Danielle Logan
RePEc: Research Papers in Economics
Pierre-guillaume Méon
njjfr hggtgrf
De Gruyter eBooks
Friedrich Neubarth
Indian Journal of Animal Research
ilker camkerten
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024

Create Free Account or
- Acute Coronary Syndromes
- Anticoagulation Management
- Arrhythmias and Clinical EP
- Cardiac Surgery
- Cardio-Oncology
- Cardiovascular Care Team
- Congenital Heart Disease and Pediatric Cardiology
- COVID-19 Hub
- Diabetes and Cardiometabolic Disease
- Dyslipidemia
- Geriatric Cardiology
- Heart Failure and Cardiomyopathies
- Invasive Cardiovascular Angiography and Intervention
- Noninvasive Imaging
- Pericardial Disease
- Pulmonary Hypertension and Venous Thromboembolism
- Sports and Exercise Cardiology
- Stable Ischemic Heart Disease
- Valvular Heart Disease
- Vascular Medicine
- Clinical Updates & Discoveries
- Advocacy & Policy
- Perspectives & Analysis
- Meeting Coverage
- ACC Member Publications
- ACC Podcasts
- View All Cardiology Updates
- Earn Credit
- View the Education Catalog
- ACC Anywhere: The Cardiology Video Library
- CardioSource Plus for Institutions and Practices
- ECG Drill and Practice
- Heart Songs
- Nuclear Cardiology
- Online Courses
- Collaborative Maintenance Pathway (CMP)
- Understanding MOC
- Image and Slide Gallery
- Annual Scientific Session and Related Events
- Chapter Meetings
- Live Meetings
- Live Meetings - International
- Webinars - Live
- Webinars - OnDemand
- Certificates and Certifications
- ACC Accreditation Services
- ACC Quality Improvement for Institutions Program
- CardioSmart
- National Cardiovascular Data Registry (NCDR)
- Advocacy at the ACC
- Cardiology as a Career Path
- Cardiology Careers
- Cardiovascular Buyers Guide
- Clinical Solutions
- Clinician Well-Being Portal
- Diversity and Inclusion
- Infographics
- Innovation Program
- Mobile and Web Apps
Pregnancy-Induced Hypertension and Risk for Heart Failure
Quick Takes
- In a large, nationwide, retrospective cohort study, the rate of HF in women with pregnancy-induced hypertension was higher compared to normotensive women (HR, 1.8; 95% CI, 1.6-2.0).
- The risk for both ischemic (ICM) and nonischemic cardiomyopathy (NICM) was increased with pregnancy-induced hypertension, and these risks were highest in the first 6 years following pregnancy and persisted thereafter.
- Median time to diagnosis of NICM was 16 years and for ICM was 20 years from 6 months post-partum.
Study Questions:
What is the association between pregnancy-induced hypertension (preg-HTN) among primiparous women and risk of heart failure (HF) stratified as ischemic (ICM) versus nonischemic cardiomyopathy (NICM)?
This is a nationwide population-based observational study from Sweden. All births from 1988–2019 were included except triplet or more births. Mothers with pre-existing HF, hypertension, ischemic heart disease, and atrial fibrillation prior to conception were excluded, as were those with peripartum cardiomyopathy within 6 months post-partum. Follow-up started 6 months post-partum. Primary outcomes of interest were HF stratified as ICM or NICM.
A total of 1,433,268 births in primiparous women were included: 80,293 pregnancies were complicated by preg-HTN. The authors matched 79,334 women with preg-HTN to 396,531 normotensive women. Diagnosis of HF before pregnancy was more common in women with preg-HTN (odds ratio, 1.73). Patients with preg-HTN were more likely to be obese, have diabetes pre-pregnancy, and were more likely to give birth to twins. All pregnancy complications were more common with preg-HTN. Over a median follow-up of 13.2 years, the rate of HF in women with preg-HTN was higher compared to normotensive women (hazard ratio [HR], 1.8; 95% confidence interval [CI], 1.6-2.0). The hazard for developing NICM and ICM was higher after preg-HTN compared with normotensive women (HR, 1.7 and 2.3, respectively). Risk for HF was higher with characteristics for more severe preg-HTN such as preterm delivery before 34 weeks and pregnancies with small for gestational age. Median time to diagnosis of NICM was 16 years and for ICM was 20 years from 6 months post-partum. The incidence of HF was highest in the first 6 years following preg-HTN.
Conclusions:
In a large observational study of primiparous women with preg-HTN, the risk for subsequent ischemic and nonischemic HF was increased, with the highest risk being in the 6 years following pregnancy.
Perspective:
Pregnancy-induced hypertensive disorders complicate 5-10% of all pregnancies. In this study, the authors note a higher risk for subsequent ICM and NICM among primiparous women with preg-HTN compared with normotensive women. This risk was highest in the first 6 years post-partum, and while the risk subsequently declined, it remained elevated at longitudinal follow-up. More severe phenotypes of preg-HTN were associated with a higher risk for subsequent HF. Results of this study suggest that women with preg-HTN constitute a high-risk group and perhaps should be followed more closely for development of HF. Strengths of this study include the large numbers from a nationwide cohort. However, given its retrospective nature only, association can be established but not causation.
Clinical Topics: Congenital Heart Disease and Pediatric Cardiology, Diabetes and Cardiometabolic Disease, Heart Failure and Cardiomyopathies, Prevention, Vascular Medicine, CHD and Pediatrics and Arrhythmias, CHD and Pediatrics and Prevention, CHD and Pediatrics and Quality Improvement, Acute Heart Failure, Hypertension
Keywords: Cardiomyopathies, Diabetes Mellitus, Heart Failure, Hypertension, Pregnancy-Induced, Infant, Small for Gestational Age, Myocardial Ischemia, Obesity, Pregnancy, Premature Birth, Primary Prevention, Risk Factors, Twins, Women
You must be logged in to save to your library.
Jacc journals on acc.org.
- JACC: Advances
- JACC: Basic to Translational Science
- JACC: CardioOncology
- JACC: Cardiovascular Imaging
- JACC: Cardiovascular Interventions
- JACC: Case Reports
- JACC: Clinical Electrophysiology
- JACC: Heart Failure
- Current Members
- Campaign for the Future
- Become a Member
- Renew Your Membership
- Member Benefits and Resources
- Member Sections
- ACC Member Directory
- ACC Innovation Program
- Our Strategic Direction
- Our History
- Our Bylaws and Code of Ethics
- Leadership and Governance
- Annual Report
- Industry Relations
- Support the ACC
- Jobs at the ACC
- Press Releases
- Social Media
- Book Our Conference Center
Clinical Topics
- Chronic Angina
- Congenital Heart Disease and Pediatric Cardiology
- Diabetes and Cardiometabolic Disease
- Hypertriglyceridemia
- Invasive Cardiovascular Angiography and Intervention
- Pulmonary Hypertension and Venous Thromboembolism
Latest in Cardiology
Education and meetings.
- Online Learning Catalog
- Products and Resources
- Annual Scientific Session
Tools and Practice Support
- Quality Improvement for Institutions
- Accreditation Services
- Practice Solutions
Heart House
- 2400 N St. NW
- Washington , DC 20037
- Email: [email protected]
- Phone: 1-202-375-6000
- Toll Free: 1-800-253-4636
- Fax: 1-202-375-6842
- Media Center
- ACC.org Quick Start Guide
- Advertising & Sponsorship Policy
- Clinical Content Disclaimer
- Editorial Board
- Privacy Policy
- Registered User Agreement
- Terms of Service
- Cookie Policy
© 2024 American College of Cardiology Foundation. All rights reserved.
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Determinants of pregnancy-induced hypertension on maternal and foetal outcomes in Hossana town administration, Hadiya zone, Southern Ethiopia: Unmatched case-control study
Roles Writing – original draft
* E-mail: [email protected]
Affiliation Department of Nursing College of Medicine and Health Science, Wachemo University, Hossana, Ethiopia
Roles Writing – review & editing
Roles Data curation
Affiliation Department of Public Health College of Medicine and Health Science, Wachemo University, Hossana, Ethiopia
Affiliation Department of Health Management and Economics, School of Public Health, Tehran University of Medical Science, Tehran, Iran
- Getachew Ossabo Babore,
- Tsegaye Gebre Aregago,
- Tadesse Lelago Ermolo,
- Mangistu Handiso Nunemo,
- Teshome Tesfaye Habebo

- Published: May 12, 2021
- https://doi.org/10.1371/journal.pone.0250548
- Peer Review
- Reader Comments
Globally, 292,982 women die due to the complications of pregnancy and childbirth per year, out of those deaths 85% occurs in Sub Saharan Africa. In Ethiopia, pre-eclampsia accounts for 11% of direct maternal deaths.
To determine maternal and foetal outcomes of pregnancy-induced hypertension among women who gave birth at health facilities in Hossana town administration.
Institutional based unmatched case-control study was conducted among women, who gave birth at health facilities from May 20 to October 30, 2018. By using Epi-Info version 7; 207 sample size was estimated, for each case two controls were selected. Two health facilities were selected using a simple random sampling method. Sample sizes for each facility were allocated proportionally. All cleaned & coded data were entered into Epi-info version 3.5.1 and analysis was carried out using SPSS version 20. Multivariate analysis was performed to determine predictors of pregnancy-induced hypertension at a p-value of <0.05.
Women between 18 to 41 years old had participated in the study with the mean age of 26.00(SD ±4.42), and 25.87(SD ±5.02) for cases and controls respectively. Out of participants 21(30.4%) among cases and 21(15.2%) among controls had developed at least one complication following delivery. 12 (17.4%) and 8 (5.7%) foetal deaths were found in cases and controls groups respectively whereas 15.6% from cases and 3.6% from controls groups women gave birth to the foetus with intra-uterine growth retardation. Women gravidity AOR = 0.32 [95% CI (0.12 0.86)], Previous history of pregnancy-induced hypertension AOR = 22.50 [95% CI (14.95 16.52)] and educational status AOR = 0.32[95% CI (0.12, 0.85)] were identified as predictor of pregnancy-induced hypertension.
Women with a previous history of pregnancy-induced hypertension had increased risk of developing pregnancy-induced hypertension, whilst ≥ 3 previous pregnancies and informal educational status decrease odds of developing pregnancy-induced hypertension.
Citation: Babore GO, Aregago TG, Ermolo TL, Nunemo MH, Habebo TT (2021) Determinants of pregnancy-induced hypertension on maternal and foetal outcomes in Hossana town administration, Hadiya zone, Southern Ethiopia: Unmatched case-control study. PLoS ONE 16(5): e0250548. https://doi.org/10.1371/journal.pone.0250548
Editor: Frank T. Spradley, University of Mississippi Medical Center, UNITED STATES
Received: May 1, 2020; Accepted: April 9, 2021; Published: May 12, 2021
Copyright: © 2021 Babore et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All the necessary data and materials are incorporated in the article and Supporting Information . Any further requests will be addressed by the corresponding author upon reasonable request.
Funding: The authors received no specific funding for this work from any source. all of us doing for academic qualification and put finger print for scientific society.
Competing interests: The authors declare that no competing interests.
Introduction
Pregnancy and childbirth are natural processes, which comes up with multiple consequences. A hypertensive disorder is one of the pregnancy consequences which is a major alarming cause for maternal, perinatal morbidity and mortalities [ 1 ]. The term hypertension in pregnancy is commonly used to describe a wide spectrum of the patient who may have only mild elevations in blood pressure to severe organ dysfunction. Thus, it is accompanied by minor to major complications. Worldwide hypertensive disorder in pregnancy/HDP affects 5–22% and it is responsible for 5–10% of complications in all pregnancies [ 2 – 4 ] .
Among four classes of HDP, preeclampsia remains a leading cause, which needs rigorous public intervention for better outcome of foetus and mother, and Preeclampsia affects up to 5–8% out of all pregnancies [ 5 ]. Also, preeclampsia is a unique form of hypertension during pregnancy which usually occurs after 20 weeks of gestation. If the early investigation and appropriate management are not undertaken for the women diagnosed with pre-eclampsia. It progress to a severe form called eclampsia, which end-up with maternal as well as foetal adverse outcomes like abruption placenta, acute renal failure/ARF, intravascular coagulation, intra-uterine growth retardation/IUGR, and stillbirth [ 6 ]. Therefore, the origin for eclampsia is pre-eclampsia (Eclampsia is the definition of Preeclampsia plus ≥ +2 proteinuria plus the occurrence of convulsion or coma) [ 7 ].
Studies suggested that either pre-existing pregnancy-induced hypertension/PIH or pregnancy changes could be responsible for the occurrence of pre-eclampsia. In a multicentre study approximately, 30% of hypertensive disorders of pregnancy were occurred due to chronic hypertension while 70% of the cases were diagnosed as gestational hypertension or pre-eclampsia [ 8 ]. Regardless of new-onset or pre-existing occurrences, the harmful effects of preeclampsia and eclampsia upraised from mother to child, family to the country and its severity is from trivial to life-threatening. Still, it has remained a significant public health threat in both developed and developing countries [ 9 ].
PIH denotes women’s systolic blood pressure/SBP ≥ 140mmHg, and diastolic blood pressure/DBP ≥ 90mmHg on two or more consecutive measures without proteinuria after 20 weeks of gestation; pre-eclampsia is characterized as when pregnant women presented with SBP ≥ 140mmHg and DBP ≥ 90mmHg on two or more consecutive measures within 4 hours interval with the presence of proteinuria that occurs after 20 weeks of gestation whereas eclampsia denotes the occurrence of convulsion plus proteinuria +2 or more and sign and symptom of severe pre-eclampsia for the women who fulfil the definition of PIH [ 10 – 12 ].
Pre-eclampsia and eclampsia are the second direct cause for maternal death which accounts for 10 to 15% of maternal deaths worldwide [ 13 ]. The incidence of pre-eclampsia has significant variation in different parts of the continents. For instance, 4% in Africa, 3.8% in Europe, and 4.2% in the western Pacific region [ 14 ]. Moreover, the prevalence of pre-eclampsia throughout the country has vast variation, in Jima University specialized hospital, it was 51.8%, three southwest Ethiopia hospitals 6.3% [ 15 ], and in seven Tigray hospitals 50% [ 16 ].
Globally, 292,982 women died due to the complications of pregnancy and childbirth. Out of those deaths, 85% have occurred in Sub Saharan Africa/ SSA, yet the majority of those deaths occurred in low resource settings, and most of them could have been preventable [ 17 , 18 ]. Furthermore, the highest share of maternal death has been reported in Africa as compared to other regions. Maternal death due to pregnancy-related causes is 1 in 4,000 in Europe and 1 in 16 in African countries [ 18 , 19 ]. Likewise, The probability of a 15 year-old girl eventually dying from a maternal cause in Africa was as high as 1 in 37- as compared to 1 in 3400 in the European region [ 20 ].
According to the latest joint trend review study in maternal mortality conducted by United Nation Population Division/UNPD, World health organization/WHO and World Bank, the proportion of mothers dying per 100,000 live births has declined from 380 to 210 in 1990 to 2013 [ 21 ]. Besides, there was a slight reduction in maternal mortalities in the last three consecutive Ethiopian demographic health surveys/EDHs; MMR was 667, 665 and 412 per 100,000 life birth and all those deaths might have happened as a result of direct or indirect causes [ 22 ]. On the other hand, a trend review study from 1980 to 2012 in Ethiopia, on maternal death reported that as a result of hypertensive disorder of pregnancy/HDP, maternal death has increased from 4%-29%. In-addition to the death trend, the review pointed out the major direct obstetric complications (sepsis, haemorrhage, unsafe abortion, obstructed labour) including pre-eclampsia, accounts for 85% of maternal death. Whereas pre-eclampsia solely accounts for 11% of maternal death [ 23 , 24 ]. Whilst pre-eclampsia and Eclampsia contribute to 53% of maternal and 62.7% of perinatal complications during pregnancy and birth [ 25 ].
HDP especially preeclampsia, in primigravida women is 2 times more risky than multigravida [ 26 , 27 ]. Impacts of pre-eclampsia and eclampsia are disproportional in both developed and developing countries which are seven times higher in developing countries than in developed worldwide [ 28 ].
Impacts of Pre-eclampsia and eclampsia on maternal and foetal outcomes are enormous, which results in life-threatening events to death. For instance, it increases the risk of placenta abruption, postpartum haemorrhage/PPH and intra-uterine growth retardation. According to the WHO multicentre survey, the risk of perinatal death among women with preeclampsia and eclampsia increased 3 and 5 folds respectively, as compared to women with no preeclampsia or eclampsia [ 26 , 29 , 30 ]. Still, preeclampsia is one of the major causes of perinatal death in developing countries, accounts for 20–50% of deaths [ 31 ]. In Ethiopia, eclampsia accounts for 35.7% of maternal death [ 32 , 33 ].
Studies were done abroad and our country revealed that pregnancy-induced hypertension has been associated with poor maternal and prenatal outcomes and loos of life [ 34 ]. Case control hospital-based study done in India reported that 10, 8, 3 and 2 complications of Haemolysis, Elevated Liver enzymes, and Low Platelet count/HELLP syndrome, PPH, Infection and ARF respectively [ 35 ]. On another case control study conducted by Guduri GB revealed that there were 18%, 2% PPH and 36%, 7% preterm complication, among cases and controls respectively [ 36 ].
Studies done in different regional hospitals, Ethiopia reported various proportions of maternal complications and deaths following delivery occurred as a result of pre-eclampsia/eclampsia. The Eastern part of, Ethiopia finding revealed that 53% maternal and 62.7% perinatal complication with a fatality rate of 11% [ 25 ], in Woliata Sodo University teaching Hospital 48.89% perinatal complication and 8.89% perinatal deaths [ 37 ]. In Zewuditu Memorial Hospital, among women had developed PIH, 131 (52.4%) of them developed complication whilst 31.1% of them experienced with HELLP syndrome [ 38 ].
Different studies noted that previous history of pregnancy-induced hypertension, age, and educational status were independent risk factors for the development of preeclampsia. In addition to these, occupation, gravidity, family history of hypertension, gestational diabetic Mellitus and residence had a significant statistical association with preeclampsia [ 39 – 42 ].
Yet, there have been different studies conducted to explore PIH in Ethiopia, but there was no study conducted on predictors of pregnancy-induced hypertension in the study area. Thus, to come up with effective public as well as clinical intervention approach and strong policy development direction, conducting root cause identification research is essential. Therefore, the main objective of this study is to determine maternal and foetal outcomes of pregnancy-induced hypertension among women who gave birth at Public health facility in Hossana town administration, Hadiya zone, Southern Ethiopia: unmatched case control [ Fig 1 ].
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
Legend: PIH: Pregnancy-induced hypertension, HDP: hypertensive disorder of pregnancy, Hx: history, ANC: antenatal care, GA: gestational age.
https://doi.org/10.1371/journal.pone.0250548.g001
Methods and material
The study was conducted in Hossan town administration, Hadiya Zone, South Nation Nationality and People Regional state/SNNPR, Ethiopia. Hadiya zone has ten woredas and two town administrations. According to the Hadiya Zone Finance and Economic Development office statistics, the total population of the zone was 2,486,242 of which 1,218,258 were men whereas 1,267,983 of them were female.
Hossana town is located in the northern part of SNNPR state. It is 232 KM far from the country’s capital city to the south and 120 KM from the regional capital town. The town administration is classified into 3 subs administrative with a total of 8 kebeles. According to the Hossana town administrative office, the current (2018/2019) projection estimated total population was 104,053 whereas 50,986 males and 53, 067 of them were females. Among the total town population, women within the reproductive age group encompass 24,244 from them the estimated number of women who are eligible to be pregnant in the current physical year were 8,388 [ 43 ].
The town has one teaching hospital which has been serving more than 3, 548,800 million people from the entire Hadiya Zone and partial part of kembeta and Silte Zone. As well, the town has three health centres, one private surgical hospital, and more than 15 private clinics.
Study design and period
Institutional based unmatched case control study was conducted in OB/GYN department of the selected public health facilities, from May 20/2018 to October 30/2018.
All pregnant women who were on follow up after 20 weeks gestational age and visit health facilities for delivery service and screened as of having pregnancy-induced hypertension registered in the OB/GYN departments of the respective facilities.
Pregnant women who have no PIH in the same period and the same health facilities and who came for delivery service after 20 weeks of gestational age.
Source population
The source population of the study were all women, who have been on follow-up care unit and visit facilities for delivery service in Public Health facilities those resided in Hossana town administration.
Study population
All women who were selected using systematic sampling method applying population proportionate to sample size (PPS) from randomly selected public health facilities among women who had been on follow-up care unit and visit the health facility for delivery service whose gestational age above 20 weeks.
Eligibility criteria
Inclusion criteria..
All pregnant women who were on flow up and visited selected public health facility for delivery service whose gestational age above 20 weeks were included. For women representing cases, they diagnosed having Pregnancy-induced hypertension as of her SBP ≥140mmHg and DBP ≥90 mmHg on two separate reading which measure within at least four hours apart, plus a dipstick reading +1 and above. For women represent Controls, women within the same health facilities who were attending delivery care was not diagnosed as having Pregnancy-induced hypertension.
Exclusion criteria.
Women who didn’t indweller in respective town administrative sub towns and no longer stay at Hossan town administration for more than six months.
Women with a known diagnosis for Epilepsy and women who were not voluntary to give consent also excluded from the study.
Simple size and sampling technique
Sample size..
The sample size for this study was computed based on the comparison of proportion for case control study by using Epi-info version 7 for windows. According to a study conducted by Eskeziaw Agedew [ 39 ], by considering the factors gravidity and maternal age had an association with PIH. Being multigravida and age during current pregnancy between 25–30 years which have a significant association with pregnancy-induced hypertension with case to control ratio 1:2 and Odds ratio (OR) = 4 and using the following assumptions: power 80%, confidence level 95% ( Table 1 ). The final sample size was taken from the women who were multigravida by adding 10% non-response rate. Thus, an estimated sample was employed for case 69 and 138 for controls yielding a total sample of 207.
https://doi.org/10.1371/journal.pone.0250548.t001
Sampling technique
To select a study unit two Public Health facilities were selected randomly among four facilities. Considering the two months report data from the health management information system/HMIS office sample size allocated proportionally by using proportionate to population size for cases and controls. All newly registered pregnant women who were more than 20 gestational weeks suffered from pregnancy-induced hypertension were selected representing the cases. For each case, women who registered for ANC follow up and had given delivery whose gestational age ≥20 weeks, but hadn’t experienced with PIH at the same time in the same facilities were taken as control. To select controls, a list of total women the MCH department registration book for those who have ANC follow up after 20 weeks of gestation age was considered as a sampling frame. The estimated sample size for this study (n) was divided by a total number of women (N) registered in randomly selected HFs during the last two months which yield proportionate (P). Then through multiplying proportionate value with two months sample, a proportional sample was allocated for each selected health facilities. Finally, by employing a systematic sampling method based on the k th value sampling unit was traced in respective facilities. The sampling procedure was presented ( Fig 2 ).
HC: health centre, NEMMTH: Nigest Eleni Mohomod Memorial Teaching Hospital, n: proportional allocated sample size.
https://doi.org/10.1371/journal.pone.0250548.g002
Data collection method, tools and procedures
Structured and pretested questionnaires which was prepared in English and translated to Amharic and then translated back into English again to assure consistency of tool, which developed from reviewing different literature was used in this study.
Data were collected by 4 BSc midwives, 2 BSc Nurses supervised and monitored during the data collection phase by using structured questionnaires whereas the principal investigator undertakes the overall coordination. Data were collected from women who gave birth in the OB/GYN department, for each case, two controls were interviewed on the same day and health facilities. Participant’s medical charts were also reviewed to obtain biomedical laboratory data at the same time.
Data quality control measures and management
Before the actual data collection date, data collectors & supervisors were trained concerning the overall issue of data collection format like, in time data collection following delivery, completeness, participant confidentiality and consistency.
One week before the actual data collection date, research tool was tested on 13 women who gave birth at Doyogena primary hospital, validity checked then a lot amendment was undertaken.
Every day, the principal investigator and supervisors were checked data for completeness and incomplete questionnaires were discarded. Cross-checked and coded data were entered into Epi-info software version 3.5.1. For further analysis and data cleaning, it was exported to SPSS (statistical package for social science) version 20.
Data analysis
To identify the proportion of the pregnancy induce hypertension impact on maternal and foetal outcome in-relation to outcome variable cross-tabulation frequencies were done. Cross tabulation was also employed to test the relation of variables against with outcome variable. Bivariate logistic regression was conducted to select candidate variables for multivariate analysis at P-value < 0.05. Finally, to determine predictors of outcome variables multivariate analysis was employed.
Data was described and presented using cross-tabulation value to for descriptive findings and interpreted by looking at a variable that has an association with outcome variables on multivariate analysis with a 95% confidence interval for AOR.
Study variables
Dependent variable..
Foeto-maternal outcomes of Pregnancy Induced Hypertension
Independent variable.
Socio demographic variables . Maternal age, residence, educational status, occupation and monthly income.
Obstetrics variables . Gravidity, number of parity, gestational age at delivery, number ANC follow up, number of babies (twin).
Medical variables . Previous history of pregnancy induced HTN, History of D/M, anaemia and renal disease.
Hypertensive disorder sign and symptoms of pregnancies on admission . Level of blood pressure during admission/presentation, vomiting, proteinuria, typical symptoms (oedema, blurred vision, headache and epigastric pain).
Ethical consideration
Ethical approval was obtained from IRB of WCU, Official letter for zonal/woreda health department was written from University research and community service V/P office and a cooperation letter was written from respective woreda office managers to the randomly selected health facilities.

Operational definitions of terms
Hypertensive disorders of pregnancy..
Includes chronic hypertensive and pregnancy induced hypertension, regardless of previous history of hypertensive disorder.
Pregnancy-induced hypertension.
Hypertension developed after 20 weeks of gestation where SBP ≥ 140mmHg and DBP ≥ 90mmHg, within two consecutive reading which measured 4–6 hours apart without proteinuria among mothers who were attended delivery unit at health facilities among previously normotensive women.
Preeclampsia.
The new onset of hypertension with SBP ≥ 140 and DBP ≥ 90 mmHg, within two reading which measured 4–6 hours interval with the presence of proteinuria with or without oedema which occurred after 20 weeks of gestation.
Mother with DBP greater than or equal to 110mmHg after 20 weeks of gestation and in-addition to the features of pre-eclampsia having one or more episode of convulsion or coma plus proteinuria + 2 or more.
Pregnancy outcome.
Any women who had at least one prenatal as well as maternal unfavourable outcome after delivery
Maternal complication.
Any mothers had at least one complication among who had attended delivery at Hospital.
Gestational age.
The duration of gestation is measured from the first day of last menstrual period more than 20 weeks for this study.
Foetal outcomes.
Any diagnosed complication or death confirmed after delivery.
Socio-demographic characteristics
Among a total of 207 participants, 69 cases and 139 controls women have participated in the study. Women from the age of 18–41 participated in the study while their mean age was 26.00 (SD ± 4.42), 25.87 (SD ± 5.02) for cases and controls respectively. Two women were participated in the study where their age was below legally eligible for marriage. The majority 97 (47.3%) participants’ were house-hold wives, 9(4.3% of them were students and 69 (42.9%) had no formal education.
Reproductive history and pre-existing medical illness during current pregnancy
Among women who had ANC visits three and above, 34 (52.3%) from cases and 72 (55.0%) from control were not developed PIH. Women with a high frequency of ANC follow-Up had a low proportion of becoming hypertensive on current pregnancy while among women who had no ANC follow-up, 4 from cases and 10 from controls groups had developed pregnancy-induced hypertension.
More than one-third of the study participants were primigravida among them 34 (31.5%) were not know their LNMP. However, 180 (86.9%) didn’t attend the minimum expected ANC follow up, only 16 (7.7%) had four and above ANC follow up. Seven women among cases and 44 women from control groups gave birth by caesarean section, but the largest proportion 62 (89.8%) of women from cases gave birth via spontaneous vaginal delivery/SVD as compared with controls 94 (68.1%).
Among all interviewed women, 29 (14.0%) were experienced with pre-existing medical illness includes: diabetic Mellitus, anaemia and non-pregnancy induced hypertension 4.3%, 5.3% and 3.9% respectively. A high proportion of women from cases 14 (20.3%) had medical problems as compared to controls 15 (10.9%). Out of the total cases that participated in this study; twenty-four women had a previous history of PIH. On the occasion of health facility arrival, 120 (57.9%) women were admitted with pushing labour pain, but the remaining were came up with one or more features rather than labour pain ( Table 2 ).
https://doi.org/10.1371/journal.pone.0250548.t002
Even though the DBP range from 90 to 144 mmHg among cases the mean DBP, 104.13 (SD ± 9.20) was above the cut-off point of the normotensive women. Perinatal delivered from women with cases experienced with an average of 0.7 complications. On the occasion of reception for delivery service and follow-up care in addition to having high blood pressure, every woman from cases was admitted with at least of two suggestive clinical features for PIH whereas controlled had less than 1 clinical feature ( Table 3 ).
https://doi.org/10.1371/journal.pone.0250548.t003
Maternal and fetal outcomes
A total of 69 women with cases participated in the study and showed a potential effect on maternal and perinatal health. Among the interviewed cases, 11 (15.9%) of them were developed eclampsia. On the occasion of the arrival to health facility among women who had developed eclampsia, only 3 (27.2%) of them were comatose on the occasion of the arrival of health facility. For all Women who developed PIH urine test was performed and a test result had shown a minimum +1 proteinuria for the dipstick test.
Among the total of interviewed cases, 21(30.4%) women have developed at least one complication following delivery. The majority of complications were 13 PPH and 7 disseminated intravascular coagulopathy/DIC. Moreover, PIH has a potential effect on maternal as well as perinatal outcomes; perinatal borne from women with PIH more likely to develop complication than normotensive women. Out of 55, alive births among cases 32 (58.2%) had at least one complication, but out of total alive births, 32.9% (n = 68) perinatal hadn’t any complication. From 20 perinatal deaths, 12 (17.4%) was reported from women who had developed PIH. Among 13 foetal IUGR, 8 of them were from cases as far as women diagnosed for PIH 3.7 times more risky to causes foetal IUGR than normotensive women ( Table 4 ).
https://doi.org/10.1371/journal.pone.0250548.t004
Pregnancy-induced hypertension and associated factors
Binary logistic regression with a confidence level of 95%, (α = 0.05) was conducted and variables which have statistically significant at p-value < 0.05 were selected as candidate variable for the last model that determine predictors of pregnancy-induced hypertension among women gave birth at health facilities.
Finally, variables entered into the last model and multivariate analysis was performed. The Previous history of pregnancy-induced hypertension increased odds of developing pregnancy-induced hypertension by 22 folds, [95% CI (6.313, 80.204)], three and above previous pregnancies decreases odds of pregnancy-induced hypertension AOR = 0.32 [95% CI (0.12, 0.86)] and women who had no formal education, 68.4% [95% CI (0.12, 0.85)] less likely to develop PIH than women had primary and above educational status. Thus, the model was identified; gravidity, educational status, and previous history of pregnancy-induced hypertension were determinant factors for pregnancy-induced hypertension. Furthermore, Pregnancy-induced hypertension had an impact on inducing maternal complication, perinatal death and Intra-Uterine growth retardation/IUGR ( Table 5 ).
https://doi.org/10.1371/journal.pone.0250548.t005
This study revealed that 21(30.4%) among cases and 21(15.2%) women in control groups had developed at least one complication following delivery. The finding is supported by the study conducted in India 54% among case and 9% from controls developed maternal complications [ 36 ]. Also, a study done by Kapil Dev revealed that among cases 24% of women developed at least one maternal complication, but there was no maternal complication in controls [ 37 ]. A lower proportion of maternal complication in this study could be due to living style and women in the study area had less history of medical complications.
The commonest maternal complications in this study were postpartum haemorrhage/PPH 13 (18.8%), which is higher than the study done in India [ 35 ]. The lower proportion reported from elsewhere might be a better management approach and health care setups in those facilities were more intensive and organized as compared to our study area.
This study showed that perinatal complications were more prevalent among controls (63.4%) as compared to cases (58.2%). The finding is supported by the study done by Aleem Arshad, only 1 and 13 low birth weight reported from cases and control, respectively [ 44 ]. In this study, neonatal death was the second leading outcome of PIH, 17.4% from cases and 5.7% controls deaths were reported. Concerning perinatal complications, this study reported that 15.6% IUGR from cases and 3.6% from control which was lower than a study conducted in India; 29% and 71% IUGR were reported from women who had developed PIH and normotensive, respectively [ 36 ]. The possible reason for the low proportion could be socio-demographic factors and women in our study area affected by low superimposed medical problems.
Out of the cases, group preeclampsia accounted for 58(84.1%) whereas eclampsia comprises 11(15.9%). A study was done in Harare, Zimbabwe reported the proportion of pre-eclampsia and eclampsia were 1.7% & 0.3% respectively [ 9 ], but the proportion was lower than a study conducted by Selemawit, 121 women developed Pre-eclampsia and 17 of them Eclampsia [ 45 ]. The difference might be due to early identification and alerting women during ANC visits which decrease the possible occurrences of preeclampsia and eclampsia. Other study carried in three south-west hospitals, Ethiopia and tertiary care hospital of Visakhapatnam, India reported in the prevalence of pre-eclampsia and eclampsia were 7.9%, 3% and 16%, 36% respectively among cases [ 36 , 46 ].
In this study gravidity has an association with PIH, women with gravidity 3 and above were 68% [95% CI (0.12, 0.86)], less likely to develop Pregnancy-induced hypertension as compared to their counterparts. This study is in-line with a study done in Darashe Special woreda [ 39 ] and Kombolicha, Ethiopia [ 41 ]. Whereas, the finding is in contrast with the study done in Addis Ababa, Ethiopia and Colombia; primigravida women were 2.7 times more likely to develop PIH than multigravida [ 24 ], and 36.9% of primigravida women among cases had developed PIH [ 47 ], the possible reason might be due to difference in assigning the reference group.
History of previous pregnancy-induced hypertension was significantly associated with PIH. In our study previous history of pregnancy-induced hypertension had 22 times increased odds of pregnancy-induced hypertension as compared to previous normotensive women. Out of the total interviewed women who had previous history of pregnancy-induced hypertension, 34.8% in cases and 2.9% in controls groups developed PIH in the current pregnancy. This finding is in-line with the studies done in Addis Ababa, Ethiopia and Karnataka, India. Women with a previous history of pregnancy-induced hypertension were 4 times more likely to develop PIH during current conception, which reported 28.95% women among cases and 10.9% among control had developed PIH in Karnataka, India. Women with a previous history of PIH were 58 times odds of developing PIH, out of the total interviewed cases 60% and controls 2.50% of women developed PIH during current pregnancy [ 36 ]. However, the finding of this study contradicts with the study done in Jaipur, India [ 40 ].
In this study, multivariable analysis revealed that previous history of medical illness had no statistical association with PIH, but studies conducted in Tigray, Kombolicha in Ethiopia, and Southern India reported that women with diabetic Mellitus were 5.4, 11 and 5 times more likely to develop PIH respectively [ 16 , 41 , 48 ]. The possible reason for this discrepancy could be that the number of women with a pre-existing medical problem in this study was fewer than those studies conducted elsewhere.
In addition to the maternal complication, this study singled-out that perinatal complications such as low birth weight, IUGR, and pre-term were higher in the cases than controls. Also, the study demonstrated that there was no association between PIH and birth weight which is in contrast with the study done in Zimbabwe where women with PIH were 3 times more likely to have a baby with low birth weight [ 9 ]. However, this study is in-line with a study done by Eskzyiaw [ 39 ]. Major perinatal complications reported in this study were LBW (31.1%), IUGR (6.9%) and preterm (6.8%).
Conclusion and recommendation
Pregnancy-induced hypertension yet has been seen as a burning issue, which provokes adverse health impact on mothers and their babies. In this study, both maternal and perinatal outcomes were significantly different in both groups (cases & control). Women with PIH were at higher risk for a maternal and perinatal adverse outcome as compared to normotensive women. Women with a previous history of PIH had increased risk of developing PIH whilst women who had ≥ 3 previous pregnancies and with informal education were less likely to develop pregnancy-induced hypertension.
Recommendation
For women diagnosed with a previous history of pregnancy-induced hypertension, health care providers should have taken especial attention and focused care to tackle the adverse effect of PIH on their current conception. Furthermore, concerning governing bodies and partners engaged in maternal service should have facilitated basic setups like on-job training on early screening skills and managements, tax-free transportation. When gravidity increased women may not caution as like the first conception so that clinical expertise gave attention to alerting women regarding early warning sign and improve health service delivery strategies. Principal governing bodies and concern partners should have facilitated maternal waiting room/village for better health, good perinatal and maternal outcome.
Supporting information
https://doi.org/10.1371/journal.pone.0250548.s001
https://doi.org/10.1371/journal.pone.0250548.s002
Acknowledgments
First, of all, I would like to Praise and give thanks to God for his grace and blessings over this work. Secondly, I would like to thanks Wachamo University research and community service and vice President Office and College of Health science and medicine for overall coordination since preparation to finalizing the research project. Finally, my greatest gratitude extends to my NEMMRH MCH departments professionals and Hossana town administration health office for giving the baseline data for this study.
- 1. Malawi M., Baseline Survey of Management at Lilongwe Central Hospital , Malawi . Boston, MA, MSH, 2004.
- View Article
- PubMed/NCBI
- Google Scholar
- 13. Duley L. The global impact of pre-eclampsia and eclampsia . in Seminars in perinatology . 2009. Elsevier. https://doi.org/10.1053/j.semperi.2009.02.010 pmid:19464502
- 14. Nwanodi O.B. Preeclampsia-eclampsia adverse outcomes reduction : the preeclampsia-eclampsia checklist . in Healthcare . 2016. Multidisciplinary Digital Publishing Institute. https://doi.org/10.3390/healthcare4020026 pmid:27417614
- 21. Alkema L., et al., Trends in maternal mortality : 1990 to 2013-estimates by WHO , UNICEF , UNFPA , the World Bank , and the United Nations population division . 2014, The World Bank.
- 22. ICF E.E.M.D., Health Survey , 2019 . Key Indicators . Rockville, Maryland, USA: EPHI and ICF, 2019.
- 28. Organization W.H., The World health report : 2005 : make every mother and child count . 2005: World Health Organization.
- 38. Dufera S., Maternal and Perinatal Outcomes of Pregenancies Complecated by Preeclampsia/Eclampsia at Zewditu Memorial Hospital . 2015, Addis Ababa University.
- 43. Hossan town finace and economic office., annual plan of the town, Hossana, Ethipia 2018 (unpublished)
- 45. Selamawit D. and Sisay T., Maternal and Perinatal outcomes of pregenancies complecated by preeclampsia/eclampsia at zewditu memorial hospital . Addis Ababa Aniversity school of graduate studies faculty of Medicine, 2015.
- Open access
- Published: 02 December 2021
Pregnant women’s experiences with the management of hypertensive disorders of pregnancy: a qualitative study
- Amyna Helou 1 ,
- Kay Stewart 1 ,
- Kath Ryan 2 &
- Johnson George 1
BMC Health Services Research volume 21 , Article number: 1292 ( 2021 ) Cite this article
3724 Accesses
3 Citations
1 Altmetric
Metrics details
Hypertensive disorders are a leading cause of mortality and morbidity during pregnancy. Despite multiple national and international clinical guidelines and a plethora of research in the field of optimising management, there has been limited research describing the perspectives and experiences of pregnant women with the management of hypertensive disorders of pregnancy (HDP). Understanding these perceptions and experiences is imperative to the optimisation of HDP management.
A qualitative study involving face-to-face, in-depth interviews were undertaken with 27 pregnant women diagnosed with and being treated for HDP to explore their perspectives of and experiences with clinical management. Written consent was obtained individually from each participant, and the interviews ranged from 16 to 54 min. Inductive codes were generated systematically for the entire data set. Line-by-line analysis was then performed and nodes were created within NVivo, a qualitative data management software. Data collection was continued until thematic saturation was reached. Thematic analysis was employed to interpret the data.
Three major descriptive themes were discerned regarding the women’s perspectives on and experiences with the management of HDP: attitudes towards monitoring of HDP, attitudes and perceptions towards development and management of complications, and perceptions of pregnant women with chronic hypertension. Trust in the hospital system, positive attitudes towards close blood pressure monitoring as well as self-monitoring of blood pressure, and a realistic approach to emergency antenatal hospital admissions contributed to a positive attitude towards monitoring of HDP. Women with prior experiences of HDP complications, including pre-eclampsia, were more confident in their clinical management and knew what to expect. Those without prior experience were often in shock when they developed pre-eclampsia. Some women with chronic hypertension displayed limited understanding of the potential risks that they may experience during pregnancy and thus lacked comprehension of the seriousness of the condition.
Conclusions
The clinical management experiences of pregnant women with HDP were varied. Many women did not feel that they were well informed of management decisions and had a desire to be more informed and involved in decision-making. Clear, concise information about various facets of HDP management including blood pressure monitoring, prescription of the appropriate antihypertensive agent, and planning for potential early delivery are required .
Peer Review reports
Introduction
Hypertensive disorders of pregnancy (HDP) affect around 10% of pregnancies in Australia and around the world [ 1 ]. Combined, they are the second largest cause of maternal death, after haemorrhage, in the developed world [ 1 ].
In Australia, the public health system provides maternity care from pre-conception to postpartum. The main health professionals who care for the pregnant women are obstetricians, midwives, general practitioners (GP) and obstetric physicians [ 1 ]. The GP has an important role in pre-conception counselling, especially with women who have chronic diseases such as hypertension or asthma. It is also the responsibility of the GP to confirm the pregnancy and refer the woman to the relevant maternal hospital service.
Initially, the choice of model of care is given to the woman. The Midwifery Group Practice model [ 1 ] allows for one-to-one maternal care, often with the same midwife throughout the term of pregnancy, which is a suitable option for women without complications. Pregnant women with complications such as chronic hypertension or a previous pregnancy complicated by hypertensive disorders of pregnancy (HDP), however, need to be cared for by an obstetrician, who can monitor the progress of the pregnancy, blood pressure (BP), signs of pre-eclampsia, and fetal growth. The obstetric physician is usually involved in prescribing and monitoring antihypertensive medication and BP control. Pregnant women who have had pre-eclampsia previously or who have chronic hypertension are at risk of developing pre-eclampsia. Timely administration of low-dose (81-100 mg) aspirin before 16 weeks gestation has been found to reduce risk of pre-eclampsia [ 2 ].
Monitoring of BP occurs at each antenatal visit. If her BP is elevated, the woman may be referred to a day assessment unit for 4-h assessment of BP, which involves taking BP readings every half an hour for 4 h to observe the pattern of the BP and decide whether a diagnosis of HDP and/or prescription of an antihypertensive medication is warranted. In addition, test for urinary protein, full blood examination, renal function tests and fetal monitoring are performed [ 3 ]. This 4-h assessment is seen as a favourable alternative to overnight inpatient stays, both in terms of patient satisfaction and public health economics [ 3 ].
The timing of delivery in women with HDP is dependent on many maternal and fetal factors, including inability to stabilise BP, deteriorating liver and/or renal function, placental abruption, and severe fetal growth restriction [ 4 ]. Fetal morbidity and mortality are linked to the gestational age at delivery [ 4 ], so there is always a desire to prolong the pregnancy as close as possible to term (37 weeks) in the absence of an emergency. HYPITAT was a multicentre, open-label randomised controlled trial investigating induction of labour versus expectant monitoring for gestational hypertension or mild pre-eclampsia after 36 weeks’ gestation [ 5 ]. The study reported a reduction in the incidence of severe hypertension as result of induction of labour at 36 weeks gestation. No significant clinical differences were found in outcomes such as thromboembolism, eclampsia or placental abruption [ 5 ]. This study was followed by HYPITAT-II, which found that delivery should be deferred until 37 weeks as opposed to 36 weeks, unless maternal deterioration supervenes [ 6 ].
Despite multiple clinical guidelines [ 4 , 7 , 8 ] and a plethora of research in the field of optimising HDP management, there have been limited published studies describing the experiences of pregnant women with the management of HDP, as distinct from medication treatment.
A survey of women with pre-eclampsia or their partners, friends or relatives found that many had no knowledge of pre-eclampsia prior to diagnosis and once diagnosed, did not appreciate how serious or life threatening it was [ 9 ]. Women wanted access to information about pre-eclampsia and their experience contributed substantial anxiety towards future pregnancies. Partners/friends/relatives also had no prior understanding of pre-eclampsia and expressed fear for the woman and/or her baby [ 9 ]. A qualitative study of pregnant Moroccan women in the Netherlands or Morocco found that knowledge of symptoms related to hypertensive disorders of pregnancy was limited or absent [ 10 ]. The limited knowledge of hypertension-related symptoms and complications was based on their own experiences or on those of some family members or stories from their social network or internet, with little or no information on symptoms from their midwives or obstetricians [ 10 ]. The experiences, perceptions and behaviours of pregnant women with regard to the management of HDP during pregnancy remain largely unexplored. Understanding these perceptions and experiences is imperative to the optimisation of HDP management.
To explore pregnant women’s perspectives of and experiences with clinical management of HDP.
Study design
A qualitative study using in-depth interviews was conducted, with pregnant women in their second or third trimester, recruited from antenatal clinics in two large tertiary hospitals in Melbourne, Australia.
Participants were sourced via a larger mixed-methods study, which included 100 pregnant women with HDP. Eligible participants were identified by one researcher (AH), who reviewed the medical records of pregnant women attending antenatal clinics, and then approached them individually. Participants were provided with written information for the larger study and on receipt of written informed consent, a questionnaire was given for self-completion. At the end of the questionnaire, participants were asked to indicate their interest in undertaking an interview. Of the 98 women who responded to the questionnaire, 65 expressed interest in being interviewed. Combined convenience and purposive sampling was conducted among these 65 women to seek a breadth of views. All of the women who were invited accepted to participate in an interview. Informed written consent was obtained prior to each interview, which included permission to audio record the conversation and to use quotations when anonymously reporting and publishing the results.
Study sample
Face-to-face, qualitative in-depth interviews were conducted with 27 pregnant women who were diagnosed with HDP and had a prescription for an antihypertensive medication, in either the second or third trimester of pregnancy, recruited from the antenatal outpatient clinics of two large tertiary maternity hospitals in Melbourne, Australia. Together, these hospitals provide antenatal care to approximately 13,000 women annually. They were identified using hospital records and approached during subsequent clinic visits. Participation was voluntary and involved informed consent.
The study sample size was determined based on theme saturation during analysis and was not predetermined. Recruitment ceased when no new information was forthcoming from the last three interviews, with regard to replication of data relating to attitudes towards HDP monitoring, perceptions of the development and management of complications (including early delivery) and perceptions of the women who had chronic hypertension.
Data collection
Interviews were conducted face to face by a single researcher (AH) a female Pharmacist (who was a PhD candidate at the time) after receiving training in in-depth interviewing prior to the commencement of the study using an interview guide developed based on the literature [ 11 , 12 ] and was agreed upon by the authors (Table 1 ). Open-ended questions, such as “Tell me about …? ”, followed by appropriate prompts, such as “How did that make you feel?” or “Can you explain that in more detail?” were used to guide the interview and encourage the interviewee to speak freely and in-depth about their experiences and thoughts. As the interviewer had met the participants during the larger study, some rapport had been established prior to the interview. The interviewer did not disclose their healthcare background to participants to avoid requests for health advice during the interviews. Interviews on average lasted 35 min (range 16 to 54 min) and were conducted in a private room near the antenatal clinics. No repeat interviews were performed.
Socio-demographic and self-reported health information was collected from participants through the questionnaire. Health information was verified, with consent, through medical records.
All interviews were audio-recorded, transcribed verbatim and de-identified. Interviews continued until data saturation was reached, deemed to be the point after which no new information for analysis was forthcoming [ 13 ]. The transcripts were not returned to the participants for comments or correction.
Data analysis
Data analysis occurred concurrently with the interviews. Initial coding was completed by AH using the qualitative data management software QSR NVivo 10 (QSR International) [ 14 ]. Inductive codes were generated systematically for the entire data set. Line-by-line analysis was then performed and nodes were created within NVivo. To ensure reliability, a random selection of 20% of the transcripts were coded independently by another member of the research team (KS). KS and KR read all the transcripts and any differences were discussed among all three to reach consensus. The researchers were all pharmacists; KS and KR had extensive experience in conducting qualitative research. Transcripts were reread by AH and KS to ensure that coding was accurate and all relevant data were included.
Thematic analysis was employed [ 15 ]. This was done across all HDP subtypes and severities to obtain a wide range of views. AH read and reread the codes, collapsed them into potential themes, compared the developing themes with the intact transcripts and cross referenced to HDP subtypes. When a pattern was seen within a certain subtype, coding was grouped specifically for that subgroup. Codes were arranged into potential themes. Themes were reviewed, refined and prepared into a final set with KS; sub-themes were identified within this process.
Participants
Of the 98 women who responded to the questionnaire, 65 expressed interest in being interviewed. A combination of convenience and purposive sampling was conducted among these women to seek a wide breadth of views. All participants had a diagnosis of HDP and were prescribed antihypertensive medication. Interviews occurred during pregnancy except for one, which happened 1 day postpartum. All participants were aged 18 years or over and were fluent in English. Twenty-seven women were interviewed to reach data saturation. Their demographics, clinical and obstetric characteristics are shown in Table 2 . Family members were present for some interviews but none of them participated in the interview or made comments. Field notes were taken by the interviewer during the interviews. No participants dropped out of the study or refused participation.
Eight participants were primigravidae, the remainder were multigravidae, including six who had previous miscarriages. One participant had an assisted pregnancy (in vitro fertilisation). Twelve were prescribed aspirin for the prevention of pre-eclampsia. Participants ranged in age from 26 to 42 years. The annotations at the end of each quote give a description of the participant’s age, parity, gestational trimester and subtype of HDP at the time of the interview. The participants did not provide feedback on the findings.
Interview themes
Three major descriptive themes were discerned regarding the women’s experiences with the management of HDP:
attitudes towards monitoring of hypertensive disorders of pregnancy;
attitudes and perceptions towards development and management of complications; and
perceptions of pregnant women with chronic hypertension.
Theme 1: Attitudes towards monitoring of hypertensive disorders of pregnancy.
Most women had general trust in the hospital system. Some felt extra confidence knowing that they were being managed at a maternity hospital:
“Hospital is for saving lives of people...as soon as I see the hospital I know that I am in safe hands.” (#14, 40 years, 2nd pregnancy, second trimester, severe pre-eclampsia).
“I felt very comfortable here...it seems like they are well prepared for these things...I was in the section of the hospital where all women were in the same [hypertension] situation.” (#9, 30 years, 1st pregnancy, second trimester, chronic hypertension).
One woman expressed some distrust in general hospitals, which she perceived as not managing her BP well:
“My own GP at that time increased it [methyldopa] to six a day … the hospital … increased to 10 a day … but I couldn’t lift my head up … so I ended up coming to the women’s hospital to Emergency, because I felt like no one’s helping me.” (# 71, 37 years, 3rd pregnancy, third trimester, severe pre-eclampsia superimposed on chronic hypertension).
Self-monitoring of BP was often recommended to women treated with antihypertensives. For some, it gave reassurance, but for others it was a source of confusion, with different messages coming from various members of the treating team:
“I take up to eight [methyldopa tablets] a day...I take two and then I’ll see what my readings are...at home, myself...I also do it if I have any other symptoms.....” (# 71, 37 years old, 3rd pregnancy, third trimester, severe pre-eclampsia superimposed on chronic hypertension).
“One of the physicians I saw told me to do it three times a day … three times in a row and then she said take the average of the second two readings each time...Then I told the obstetrician my readings and she said the machine that I had at home is under-measuring...but...the physician, he was quite interested...he wanted to see my readings because he likes to compare his machine to home machines.” (#53, 40 years, 6th pregnancy, third trimester, secondary chronic hypertension).
Some women had milder HDP in previous pregnancies, which gave them a sense that the monitoring and management was overstated. Others with more severe cases and their prior experience brought back memories initiating action to make plans:
“With [child 1] it was really bad during pregnancy. With [child 2] it was bad just in the last couple of weeks and straight afterwards...[child 3] was bad, but not really bad enough. They just called it hypertension, pregnancy induced hypertension and they just left it at that. They didn’t make a big song and dance about it...They made a big song and dance last time [child 4] and then this time [they said] ‘You’re going for your monitoring’...come back a week later...’You’re going for your monitoring’, couple of hours later – ‘You’re being admitted’...Then a couple of hours later...’You’re starting on medicine’.” (#6, 28 years, 4th pregnancy, 1 day postpartum, gestational hypertension).
“Last Wednesday when they [found] blood pressure’s up … it just brought back memories from last time because same thing. I just went in for an appointment and I never came home...Ten days later I came home with a baby. So I think those aspects freak me out a bit because it’s like ‘Oh, it’s happening again’ … every appointment...even this appointment, we’ve got contingency plans, just in case.” (#74, 36 years, 2nd pregnancy, third trimester, chronic hypertension).
Some women wondered about why they were not told their BP readings unless they asked:
“I find it funny that when they take your blood pressure they don’t tell it to you. I always have to ask, always, no matter who it is, midwife, physician, obstetrician. They take it and they walk away. It’s my body but they don’t tell me.” (#53, 40 years, 6th pregnancy, third trimester, secondary chronic hypertension).
Close monitoring was perceived as frustrating, but also as part of the life adjustments that come with having a baby. Some women considered spending four hours in the day assessment centre for monitoring their BP better than being an inpatient and staying overnight, whilst others saw it as an annoyance:
“I am happy to come back every day as long as I don’t have to spend overnight here. I am happy to be here for 12 hours a day, but I just can’t be away from my children at night time.” (#29, 26 years, 3rd pregnancy, second trimester, secondary chronic hypertension).
“They just monitor me at that perinatal care...you just sit here four hours a day...it’s shocking...worse than taking the tablet.” (#90, 35 years, 7th pregnancy, third trimester, chronic hypertension).
“The only thing that was slightly frustrating was [that] four hours is a long time to sit around, but again, you’re having a baby so you’ve got to make a few adjustments to your life.” (#99, 34 years, 1st pregnancy, third trimester, pre-eclampsia).
Some of the women required a short inpatient stay to stabilise their BP and avert an emergency premature delivery. For many, it was an emotional experience filled with apprehension and uncertainty about the future:
“It was very emotional, very scary, and at the same time still trying to stay strong. So that when my husband and my kids came in, I was like ‘I’ve just got a little bit high blood pressure, everything’s alright’...I didn’t know that a possible side effect of having the blood pressure is that they may have to deliver the baby [early].” (#32, 42 years, 3rd pregnancy, third trimester, severe early onset pre-eclampsia).
“B.P. at first was around 160...she came back 15 minutes – 170, another 15 minutes 180, within 10 minutes 190...I got nervous … After 160 they gave me ...labetalol...but [the BP] did not go down...There were other tablets they gave to me but [the BP still] didn’t go down...All the doctors came up...surrounded with those with scrub suits, I panic...blood pressure...went to 210..they were panicked...one just looked at me and said “AAAH”. I cried...of course you feel anxious, you feel sad...worried... what’s going on with me? I cried and cried. It was just like a movie, they push my bed out from the room and sent me quickly down to the birthing suite [in case delivery was imminent].” (#14, 40 years, 2nd pregnancy, second trimester, severe pre-eclampsia).
Theme 2: Attitudes and perceptions towards development and management of complications.
For many women, the diagnosis of pre-eclampsia came as a shock. Those with prior experience knew what to expect and were hesitant to cease antihypertensive treatment even if their BP was low. One woman without prior experience self-educated about pre-eclampsia, became concerned about the symptoms and developed anxiety about developing it:
“It was a shock and it was a bit scary...I thought ‘I’ve heard of pre-eclampsia but I don’t really know what it is’...but all the staff, they explained everything quite well... [I could see] how they were being very concerned about it, so that was making me realise this isn’t just a small thing, this is obviously a serious situation.” (#32, 42 years, 3rd pregnancy, third trimester, severe early onset pre-eclampsia).
“I didn’t want to stop the medication altogether, only because I just didn’t want to go through the path of having the high blood pressure affect the baby [intra-uterine growth restriction].” (#8, 36 years, 2nd pregnancy, third trimester, chronic hypertension).
“I was reading that if you do develop pre-eclampsia... it is a risk for the baby and the mother as well. Upon reading all that information...I became a bit paranoid, swollen foot, swollen hands, they’re part of the symptoms, headaches, generally not feeling well...I became quite paranoid looking at my symptoms and [thinking] have I got this, have I not got this? But the doctors actually did say that I have got borderline pre-eclampsia, so they were waiting to see if I was going to develop it. However, they haven’t been able to reassure me that I’m not going to develop it and...that was quite scary for me.” (# 24, 35 years, 1st pregnancy, third trimester, chronic hypertension diagnosed during pregnancy).
Some women understood that low-dose aspirin was being used for prevention of pre-eclampsia, whereas others did not always perceive it as being effective for this purpose. Many women thought that aspirin helped with controlling the BP rather than for prevention of pre-eclampsia:
“I started on aspirin throughout the pregnancy … just to...prevent mild pre-eclampsia happening again.” (#64, 30 years, 3rd pregnancy, third trimester, chronic hypertension).
“Obstetrician put me on one aspirin a day which is supposed to help control blood pressure. So perhaps that’s also why my blood pressure is being well controlled.” (#21, 35 years, 1st pregnancy, second trimester, chronic hypertension).
Most women had a general understanding that the only way to stop the direct effects of pre-eclampsia was to deliver the baby for the safety of both mother and child. The level of comfort with such a decision varied depending on the gestational stage of diagnosis of pre-eclampsia:
“I was really disappointed and very worried about the effect it [pre-eclampsia] would have on the baby [at 21 weeks] and whether or not I would be able to carry the baby to a safe week. I just thought...if something had happened and I was forced, like accidentally went into labour too early or something like that, the baby’s chances of survival would be very low and I was really upset.” (#21, 35 years, 1st pregnancy, second trimester, chronic hypertension).
“All I know is that you just need to get the baby out...I mean plenty of women and plenty of babies survive it...but you need to detect it pretty quickly before it turns into the full...is it eclampsia?” (#41, 34 years, 1st pregnancy, third trimester, chronic hypertension).
Although many women understood that they would not continue to full-term, their perceptions and fears about the potential for a premature delivery were related to their week of gestation, concern about the welfare of the baby, and fear of separation after the birth:
“I know from my reading that 24 weeks, it’s still not ideal obviously, but if you had the baby at 24 weeks that the chance of survival was higher. I think it was 43% chance of survival from this...prior to that it was like 16% chance of survival...My sister-in–law, who is a midwife, had said...they consider 26 weeks more viable. So after that it was like, right (a) to get to 24, (b) get to 26.”. (#21, 35 years, 1st pregnancy, second trimester, chronic hypertension).
“I am just worried about my baby [having] to be delivered earlier because you see the consequences...you see things happen in the future...they are still very weak...no sucking reflex yet, the lungs are not fully developed, so many things not developed...she may live but maybe there are some disabilities...I am just hoping that I will reach even up to 30 weeks or 32 weeks. That would make me feel better.” (#14, 40 years, 2nd pregnancy, second trimester, severe pre-eclampsia).
“I was 28 weeks [when I developed severe pre-eclampsia]...they gave me steroid injections to increase the lung capacity of the baby...One of the doctors came from the NICU with a leaflet about possibly having a premature baby...that was very upsetting...and to think of having the baby...then me going home with the baby staying here is just a very scary thought.”(#32, 42 years, 3rd pregnancy, third trimester, severe early onset pre-eclampsia).
Intervention with the delivery process was a likely reality for many women who had a prospect of early delivery. Some women were apprehensive about the prospect of induction of labour or caesarean section but understood that it was for their benefit and that of their child. Others were hesitant to allow for intervention unless the risks were made clear:
“So a little bit scary, but in a way I want it to, because I’m starting to feel the uncomfortable risk that’s associated with pregnancy in this condition. Knowing that she’s at full term now at 37 weeks and she’s fine and healthy, I don’t want to develop pre-eclampsia if I can help it.” (# 24, 35 years, 1st pregnancy, third trimester, chronic hypertension diagnosed during pregnancy).
“I’m trying to push it off because I don’t want to do it. I like to have the baby when the baby’s ready, not when they tell me to. But if they tell me to because it’s really dangerous for me then I’ll listen to them obviously ….” (#53, 40 years, 6th pregnancy, third trimester, secondary chronic hypertension).
Concerns about lack of information sharing by health professionals led some women to feel that they were left out of the planning for potential intervention in the delivery, whilst others voiced concern about having low-dose aspirin in the context of a possible emergency caesarean section:
“I even asked her last time actually because she said...I’m happy with the baby’s growth, but the blood pressure’s going up so … she said ‘I’m formulating a plan in my mind’ but she doesn’t like to disclose it. I don’t know why. It’s about me; I don’t know why she just doesn’t tell me.” (#53, 40 years, 6th pregnancy, third trimester, secondary chronic hypertension).
“I also thought...what if I have an emergency caesarean tomorrow and I haven’t gotten off the aspirin? Is it going to cause me issues?” (#29, 26 years, 3rd pregnancy, second trimester, secondary chronic hypertension).
Theme 3: Perceptions of pregnant women with chronic hypertension.
Many women with chronic hypertension were already on antihypertensive medication not deemed safe during pregnancy when they found out they were pregnant. For some, it was changed to a safer alternative as soon as possible, whilst for others, the decision to change the medication was delayed and the patient’s assessment of potential risks was downplayed:
“I was on medication [telmisartan]...then when I had the kidney scan and I found out [that I was pregnant], my G.P. said ‘You’ve got to stop taking that medication because it’s not safe...so then she gave me another one to take.” (#2, 30 years, 1st pregnancy, third trimester, secondary chronic hypertension).
“The first time I found out I was pregnant I went to a GP...I told the GP that I’m taking atenolol, and then she told me that...atenolol is not recommended for pregnancy... so I asked....What medication do you think that I should take?’...she said she doesn’t dare to prescribe me any medicine because she knows she is going to refer me to a hospital.” (#59, 34 years, 1st pregnancy, second trimester, chronic hypertension).
Other women had their antihypertensive changed during the pre-pregnancy planning stage:
“[To be safe during pregnancy] I would just have to change my medications. The medication I was on I couldn’t be on while being pregnant. So when we decided to try for our first child, I went on the Aldomet and oxprenolol and that’s what I pretty much stayed on because we always wanted a second child.” (#1, 39 years, 2nd pregnancy, third trimester, secondary chronic hypertension).
Some women with chronic hypertension had concerns about lack of information sharing by health professionals and felt that they were not well informed of the potential risks that their hypertension may have on the pregnancy. Some mentioned that they may have ‘taken it more seriously’ if they had known about the risk of premature delivery associated with uncontrolled hypertension, whilst others had some limited awareness of pre-eclampsia:
“When they told me I had protein in my urine, I was a bit scared because I don’t know if it’s related to my BP.” (#4, 33 years, 1st pregnancy, third trimester, chronic hypertension).
One woman was very anxious about her diagnosis of severe, early-onset pre-eclampsia so she did some ‘self-research’. Unfortunately, she misinterpreted the information and caused herself extra unwarranted fear:
“I read on [US website found on Google] and found that 80% die after/during birth that have pre-eclampsia. That was really scary.” (#71, 37 years, 2nd pregnancy, third trimester, severe pre-eclampsia superimposed on chronic hypertension).
The information on the US Preeclampsia Foundation website actually states that “Nearly 80% of women who die from pre-eclampsia die post-partum” [ 16 ].
For some women with chronic hypertension, lack of knowledge of the seriousness of the condition resulted in lack of comprehension of the importance of BP monitoring and treatment:
“I think it was about 140 over 110 or something like that … which is pretty normal for me but they think it’s high … I feel alright. It’s all good.” (#90, 35 years, 7th pregnancy, third trimester, chronic hypertension).
“I really tried for weeks not to go on [the antihypertensive], but then when she said that maybe you could have a stroke, I got a bit scared, a lot scared … I got really worried because then they said … you could have problems, the baby could die. And I got really upset when she said the baby could not get enough oxygen. I just felt, oh just have whatever it is.” (#22, 37 years, 3rd pregnancy, third trimester, chronic hypertension).
Most women who had chronic hypertension were under a model of care involving both an obstetrician and a physician. One was triaged to midwife-only care, despite having a diagnosis of chronic hypertension and being prescribed an antihypertensive medication. This then caused a delay in the change of the antihypertensive to a safer alternative:
“Actually, I asked the midwife whether it [atenolol] is safe or not [at 18 weeks gestation]...and then she said that...it should be okay, but to be safe discuss with the physician. And so, because she said it should be okay, I presumed that ‘Oh that is okay’ ... but then the physician said ‘No, it’s better not to...so from now onwards you have to take this medicine [oxprenolol]’.” (#59, 34 years, 1st pregnancy, second trimester, chronic hypertension).
Many women had their first antenatal appointment at the hospital between 16 and 20 weeks gestation. Some women, especially those with chronic hypertension, had concerns about the timing of this appointment:
“It takes a long time now for women to get their first appointment through the hospital. It wasn’t like that, I think, about 10 years ago, must’ve changed by now … Now you have to wait ‘til you’re about 18, 20 weeks before you get your first actual appointment...and if you’ve got other health issues, things can go wrong, which it did with me.” (#71, 37 years, 2nd pregnancy, third trimester, severe pre-eclampsia superimposed on chronic hypertension).
Some women did not know that they had high BP before pregnancy. This may have been because they did not get regular check-ups with the GP or that their BP was not routinely checked at regular GP visits:
“I think if I had never gotten pregnant, I definitely would not have had [high BP], would not have to be on medication … because I wouldn’t be under the strain that I am. And also I wouldn’t be in with the doctor. I don’t think I would’ve gone to the doctor and said put me on medication … because I didn’t, want anything to change. But my lifestyle is changing now so I don’t have a choice.” (#18, 35 years, 2nd pregnancy, second trimester, chronic hypertension).
“It [BP] was quite normal before the pregnancy, so obviously it’s pregnancy-related according to the doctors [despite having been diagnosed at 7 weeks].” (#24, 35 years, 1st pregnancy, third trimester, chronic hypertension diagnosed during pregnancy).
Many women had developed chronic hypertension after a previous pregnancy that involved either gestational hypertension or pre-eclampsia. Some of them had routine follow-up for their hypertension postpartum and understood that it was now chronic hypertension, whilst others did not:
“Once I’d had the baby they changed my medication to the perindopril...I was then checking my BP at home...the readings were fine...when they did get too high, I’d go back to my local GP who would then once again adjust the dosage accordingly...I have been told by my local GP that generally once you’re on a blood pressure medication, you’re on it for life, whether it’s a minimal dosage or, depending on what the readings are, what they need to give...I’m happy to stay on that.” (#8, 36 years, 2nd pregnancy, third trimester, chronic hypertension).
“I got increased blood pressure at the end [of the previous pregnancy] and they put me in perinatal care, but then afterwards it was okay....I honestly just didn’t go to the doctor, and I haven’t gone to the doctor since I fell pregnant with this one.” (#90, 35 years, 7th pregnancy, third trimester, chronic hypertension).
One woman described having been prescribed an antihypertensive during her previous pregnancy and never told to stop it, so she continued with no formal review of her hypertension until the current pregnancy:
“They never told me to stop taking the tablet [labetalol] after I had him [first child] so I just kept continuing with it ... I saw the physician [during this current pregnancy] and he just said just keep taking it...he actually questioned ‘Did they ask you to stop it?...I said no one spoke to me about anything...I was here for a week after I had him [first child]...no one ever discussed it.” (#58, 38 years, 2nd pregnancy, third trimester, chronic hypertension).
Trust in the hospital system, positive attitudes towards close BP monitoring as well as self-monitoring of BP (SMBP) and a realistic approach to emergency antenatal hospital admissions contributed to a positive attitude towards monitoring of HDP. Most of the women in our study had a general trust in the healthcare system. Distrust surfaced when health services outside the women’s hospital were not seen as able to control hypertension early in the pregnancy, triggering patient-initiated referral to the women’s hospital. Trust of healthcare systems in western countries is generally declining [ 17 ]. It is, however, important to note that pregnant women with HDP are considered to be in a high-risk pregnancy and are thus more vulnerable than the general population. Therein lies dependence on the hospital system, especially in urgent situations such as needing to lower BP or planning for an early delivery, similar to the dependence reported in patients with coronary heart disease [ 18 ].
Anecdotally, it is common for healthcare professionals to mention that the BP reading is ‘good’ or ‘too high’ without telling the patient the systolic/diastolic numbers. An important factor relating to patient evaluation of care is their involvement in decision-making [ 19 ]. Most of the women in our study were not involved in decision-making, leaving some to wonder why this was so. This suggests that pregnant women with HDP would like to be better informed of their situation and be part of the decision-making process when deemed appropriate. This is consistent with the women’s views from the pilot of the CHIPS study who enjoyed being heavily involved in their BP management [ 20 ]. One way to have women more involved in their BP management is to encourage SMBP. SMBP in the general population has been shown to reduce BP [ 21 ] and improve adherence to antihypertensive medication [ 22 ]. In our study, SMBP was often recommended to women who were prescribed antihypertensive medications. This was taken up well by most, similar to the CHIPS pilot study [ 20 ]. SMBP during pregnancy has also been shown to be reassuring and not anxiety provoking [ 23 ] which was seen in our study. A recent survey of 5555 pregnant women from antenatal clinics in 16 hospitals in England, found that nearly half of the 389 hypertensive women reported SMBP, and that the majority of them (79%) shared their BP readings with their treating doctor [ 24 ]. Such partnership has been shown to improve patient adherence in the general population [ 25 ]. There is however an assumption that because these women are in a high-risk pregnancy, the healthcare professionals (HCP) tend to take over and do not acknowledge that the women are quite competent and that with the correct information can be involved in SMBP in collaboration with the HCPs. It is thus important to have a good doctor-patient relationship to reduce confusion, instil confidence in SMBP and complete the circle of care.
Those with prior experience with HDP and monitoring had varied views, often depending on the severity of disease in the previous pregnancy (ies). Good communication about how HDP can vary from one pregnancy to another, being either worse or better, may assist in reducing the cynicism of some and reassure others. Similarly, those who had prior experience with pre-eclampsia were a lot more confident in their management and knew what to expect. Those who did not have prior experience were often in shock and were at times anxious about the diagnosis, a finding similar to another study relating to the understanding of pre-eclampsia [ 26 ]. Moreover, the use of low-dose aspirin to prevent pre-eclampsia was only partially understood by women in our study. This indication should be communicated clearly to women who are at high risk of developing pre-eclampsia. The plan for the cessation of aspirin before delivery should also be communicated clearly to reduce any anxiety that may be present, especially in terms of a potential emergency delivery.
At times, antenatal inpatient admission was required to stabilise BP and closely monitor both the mother and baby. This was a particularly apprehensive time, especially for women who had not experienced HDP during a previous pregnancy. It is important to have good, clear communication with women about the need for close monitoring, affirmation concerning their status as worthy of hospital care, provision of consistent information, inclusion in decision-making and good social support [ 27 ]. A possible alternative to inpatient admission can be pregnancy day assessment monitoring. Despite limited research into this model of care, pregnant women have been found to prefer a four-hour stay rather be admitted to hospital for one or more nights, if the situation is deemed safe to do so [ 3 ]. This is consistent with our findings. Once again, clear consistent information regarding the need for this type of monitoring should be given to women who require it. Recent advancements in the integration of telemedicine into antenatal care [ 28 ] have encouraged early research into the feasibility of incorporating this for women with HDP to reduce the burden of multiple antenatal hospital visits [ 29 ]. The unpredictable course of worsening BP and the development of pre-eclampsia pose specific challenges to this monitoring and would require a holistic approach. A recent single centre study in the UK [ 29 ] developed and trialled an innovative SMBP intervention including a downloadable mobile app in for women with HDP to monitor for signs of pre-eclampsia or worsening hypertension. Although this study showed positive acceptance and compliance from the women, further research is required to meet the standard of care required for them [ 29 ].
In general, most women desire to labour spontaneously and have a natural birth [ 30 ]. When the reality that the only way to stop the direct effects of pre-eclampsia is to deliver the baby at any given gestational week is revealed to some women, it is received with disappointment. Good communication by the treating doctor about the intention to preserve the pregnancy for as close as possible to term is required. Likewise, sound communication about the need for a premature delivery should be communicated clearly. Moreover, it has been shown that pregnant women who require induction of labour or caesarean section often feel left out of the decision-making process [ 30 ]. An Australian study of women’s experiences of decision-making and attitudes in relation to induction of labour, reported a clear need for women to be provided with more information and agency when making decisions about their timing of birth, particularly when there are multiple reasonable treatment options [ 30 ]. Furthermore, emergency caesarean sections have been found to negatively contribute to several psychosocial outcomes for women, in particular post-traumatic stress [ 31 ]. There is, thus, a need for careful consideration and counselling for women after an emergency caesarean delivery. This can involve the members of the antenatal treating team but also counsellors or psychologists. Moreover, counselling of pregnant women who are at risk of emergency caesarean, either because of their HDP or otherwise, about this possibility may help to pre-empt potential trauma.
Research into the management experiences of pregnant women with chronic hypertension, as distinct from medication treatment, is scant. Our study has highlighted the need for extra attention to be given to improve management pre-conception, during the pregnancy and postpartum. A qualitative study exploring knowledge and attitudes related to pregnancy and preconception health in women with chronic medical conditions, including chronic hypertension, found that the women had limited knowledge of the specific potential complications of pregnancy [ 32 ]. Some women in our study also displayed limited understanding of the potential risks that they may endure during pregnancy and thus had a lack of comprehension of the seriousness of the condition. Counselling women pre-conception regarding potential risks during pregnancy allows them to be more aware of what to expect [ 33 ]. Moreover, an open conversation about the information that the pregnant woman may have either from prior experience or ‘self-research’ would help to improve understanding as well as avoiding confusion and unnecessary anxiety. The provision of written material so that the women can refer to it when necessary would also be appropriate. Another facet of management of chronic hypertension pre-conception is the initial diagnosis of hypertension. Some women in our study were not aware of their BP readings before pregnancy and were diagnosed with hypertension quite early in pregnancy and thus classed as having chronic hypertension. Regular checking of BP in women of reproductive age at routine GP visits may help to identify chronic hypertension earlier. This can help in the planning of a pregnancy, or ensure that the BP is under control in the case of an unexpected pregnancy. Similarly, for those who have chronic hypertension and are prescribed antihypertensives, switching the medication to one that is safer during pregnancy, either pre-conception or as early as possible, can help to reduce fetal exposure and reduce the mother’s anxiety. Both GPs and community pharmacists have a role in counselling women of reproductive age who are prescribed an antihypertensive. A simple question as to whether the women is planning a pregnancy can help initiate the necessary conversation and trigger the switch to a safer alternative in a timely manner. Various resources are available to help make the decision to change the antihypertensive, including drug information lines at maternity hospitals. Moreover, a large number of women who had entered our study with chronic hypertension had developed the condition after a previous pregnancy that was affected by gestational hypertension or pre-eclampsia. Furthermore, our study found that many women developed chronic hypertension soon after a pregnancy complicated by HDP. This is supported by a recent systematic review and meta-analysis which reported that the risk of developing hypertension after HDP is highest in the early postpartum period [ 34 ]. The authors also suggested that diagnosis and targeted interventions to improve maternal cardiovascular health may need to be commenced in the immediate postpartum period [ 33 ]. We agree with this and call for a more integrated follow up with women in the postpartum period and beyond. This may involve the GP and the community pharmacist for easy accessibility for the women.
Although most women with chronic hypertension in our study were under a model of care involving an obstetrician and a physician, one was under midwifery care despite having chronic hypertension and being prescribed an antihypertensive. Although it is recognised by Australian guidelines for the management of HDP that midwives play a role in a multidisciplinary team in relation to management of HDP [ 4 , 35 ], they are not qualified to independently prescribe medication and manage cases of pregnant women with chronic hypertension requiring treatment. Similarly, a recent scoping review found that practising midwives worldwide lack knowledge on several aspects of pre-eclampsia diagnosis and care and have called for an increase in in-service training to increase midwives’ knowledge in this area [ 36 ]. It is therefore important that all pregnant women who have chronic hypertension be under the doctor model of care to monitor both mother and baby throughout the pregnancy.
Recommendations for practice
Good communication between the HCP and the patient is important to optimise management. Clear, direct and concise information about various facets of the management of HDP should be provided for all women who experience HDP.
Women who experience any form of HDP during pregnancy should be invited to be part of the decision-making pertaining to the monitoring of BP and progression to pre-eclampsia as well as the timing and mode of delivery when appropriate.
There should be a priority for women with chronic hypertension to be seen at the hospital under an obstetrician led model of care before 18 weeks, not only for the regular monitoring of BP and fetal progress but also for the timely prescription of low-dose aspirin before 16 weeks gestation for the prevention of pre-eclampsia. Furthermore, other health professionals, including psychologists and pharmacists, can be involved in the prenatal care of these women to address potential fear and anxiety as well as the optimal use of medication.
Women who have chronic hypertension and are of reproductive age should be informed of the potential risks of pregnancy and be switched to a pregnancy safe antihypertensive in the preconception stage.
Women who experience gestational hypertension or pre-eclampsia during pregnancy should have their BP monitored postpartum by the GP or the community pharmacist to identify any risk of developing severe cardiovascular events.
Recommendations for future research
Currently, much of the monitoring of HDP requires a hospital visit. Further research into the feasibility of telehealth for the monitoring of HDP, especially in mild cases will help to include patients in the decision-making. Moreover, future research into the role of the GP and the community pharmacist in the pre-pregnancy planning stage for those with chronic hypertension and postpartum for those with gestational hypertension or pre-eclampsia is warranted.
Strengths and limitations
This qualitative study is the first to use in-depth interviews to explore pregnant women’s experiences, perceptions and behaviours with regard to the management of HDP during pregnancy. Our study included women with all forms of HDP except HELLP and eclampsia, as the interviews were done when the women were in a comfortable, non-emergency situation. Participants varied in gestation stage, subtype of HDP, severity of HDP, ethnicity and socioeconomic status allowing for a wide range of views. The interviews were conducted during pregnancy thus reducing recall bias. This is in contrast to other qualitative studies which explored aspects of HDP in retrospect [ 27 , 35 , 37 ]. Recruitment was from two major public maternity referral hospitals in Melbourne with a widespread combined catchment including metropolitan, regional and rural areas. Participants did not include those in the first trimester of pregnancy, as most were scheduled to attend the antenatal clinics after 12 weeks gestation. Views of women with chronic hypertension during the first trimester of pregnancy may vary from those in the second and third trimesters and they were not captured . Women with poor English skills were excluded from the study, therefore, caution should be taken in the extrapolation of our findings to women from non-English speaking backgrounds.
The clinical management experiences of pregnant women with HDP were varied. Many women did not feel that they were well informed of treatment and management decisions and had a desire to be more informed and more involved in decision-making. Clear, concise information about various facets of HDP management including BP monitoring, administration of low dose aspirin in women with a high risk of developing pre-eclampsia, prescription of the appropriate antihypertensive, and planning for potential early delivery are required. In addition, cardiovascular pre-pregnancy planning and postpartum follow-up should be routinely offered to women.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to privacy surrounding participant information as stipulated in the written consent form, but are available from the corresponding author on reasonable request.
Royal Australian and New Zealand College of Obstetrians and Gynaecologists. Maternity Care in Australia. 1st ed; 2017.
Google Scholar
Roberge S, Nicolaides K, Demers S, Hyett J, Chaillet N, Bujold E. The role of aspirin dose on the prevention of preeclampsia and fetal growth restriction: systematic review and meta-analysis. Am J Obstet Gynecol. 2017;216(2):110–20 e6.
Article CAS Google Scholar
Dunlop L, Umstad M, McGrath G, Reidy K, Brennecke S. Cost-effectiveness and patient satisfaction with pregnancy day care for hypertensive disorders of pregnancy. Aust NZ J Obstet Gyn. 2003;43(3):207–12.
Article Google Scholar
Lowe SA, Bowyer L, Lust K, McMahon LP, Morton MR, North RA, et al. The SOMANZ guidelines for the Management of Hypertensive Disorders of pregnancy 2014. Aust NZ J Obstet Gyn. 2015;55(1):11–6.
Koopmans CM, Bijlenga D, Groen H, Vijgen SMC, Aarnoudse JG, Bekedam DJ, et al. Induction of labour versus expectant monitoring for gestational hypertension or mild pre-eclampsia after 36 weeks’ gestation (HYPITAT): a multicentre, open-label randomised controlled trial. Lancet. 2009;374(9694):979–88.
Broekhuijsen K, van Baaren GJ, van Pampus MG. Immediate delivery versus expectant monitoring for hypertensive disorders of pregnancy between 34 and 37 weeks of gestation (HYPITAT-II): a multicentre, open-label randomised controlled trial (vol 385, pg 2492, 2015). Lancet. 2016;387(10021):848.
Brown MA, Magee LA, Kenny LC, Karumanchi SA, McCarthy FP, Saito S, et al. Hypertensive disorders of pregnancy ISSHP classification, diagnosis, and management recommendations for international practice. Hypertension. 2018;72(1):24–43.
Magee LA, Pels A, Helewa M, Rey E, von Dadelszen P, Pr CHD. Diagnosis, evaluation, and management of the hypertensive disorders of pregnancy. Pregnancy Hypertens. 2014;4(2):105–45.
East C, Conway K, Pollock W, Frawley N, Brennecke S. Women’s experiences of preeclampsia: Australian action on preeclampsia survey of women and their confidants. J Pregnancy. 2011. Article number 375653.
Ouasmani F, Engeltjes B, Haddou Rahou B, Belayachi O, Verhoeven C. Knowledge of hypertensive disorders in pregnancy of Moroccan women in Morocco and in the Netherlands: a qualitative interview study. BMC Pregnancy Childbirth. 2018;18(1):344.
Sawicki E, Stewart K, Wong S, Leung L, Paul E, George J. Medication use for chronic health conditions by pregnant women attending an Australian maternity hospital. Aust NZ J Obstet Gynaecol. 2011;51(4):333–8.
Lim AS, Stewart K, Abramson MJ, Ryan K, George J. Asthma during pregnancy: the experiences, concerns and views of pregnant women with asthma. J Asthma. 2012;49(5):474–9.
Fusch PI, Ness LR. Are we there yet? Data saturation in qualitative research. Qual Rep. 2015;20(9):1408–16.
Microsoft Windows NVivo 10. [Available from: http://help-nv10.qsrinternational.com/desktop/concepts/about_nodes.htm .] Accessed 21 Feb 2020.
Braun VC, V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Preeclampsia Foundation 2021 [Available from: https://www.preeclampsia.org/health-information ]. Accessed 11/02/2021.
Ward PR, Rokkas P, Cenko C, Pulvirenti M, Dean N, Carney S, et al. A qualitative study of patient (dis) trust in public and private hospitals: the importance of choice and pragmatic acceptance for trust considerations in South Australia. BMC Health Serv Res. 2015;15:297.
Meyer SB, Ward PR. Differentiating between trust and dependence of patients with coronary heart disease: furthering the sociology of trust. Health Risk Soc. 2013;15(3):279–93.
Hodnett ED. Pain and women’s satisfaction with the experience of childbirth: a systematic review. Am J Obstet Gynecol. 2002;186(5):S160–S72.
Magee LA, von Dadelszen P, Chan S, Gafni A, Gruslin A, Helewa M, et al. Women’s views of their experiences in the CHIPS (control of hypertension in pregnancy study) pilot trial. Hypertension Pregnancy. 2007;26(4):371–87.
Tucker KL, Sheppard JP, Stevens R, Bosworth HB, Bove A, Bray EP, et al. Self-monitoring of blood pressure in hypertension: a systematic review and individual patient data meta-analysis. PLoS Med. 2017;14(9):e1002389. https://doi.org/10.1371/journal.pmed.1002389 .
Ogedegbe G, Schoenthaler A. A systematic review of the effects of home blood pressure monitoring on medication adherence. J Clin Hypertens (Greenwich). 2006;8(3):174–80.
Hinton L, Tucker KL, Greenfield SM, Hodgkinson JA, Mackillop L, McCourt C, et al. Blood pressure self-monitoring in pregnancy (BuMP) feasibility study; a qualitative analysis of women’s experiences of self-monitoring. BMC Pregnancy Childbirth. 2017;17(1):427. https://doi.org/10.1186/s12884-017-1592-1 .
Tucker KL, Hodgkinson J, Wilson HM, Crawford C, Stevens R, Lay-Flurrie S, et al. Current prevalence of self-monitoring of blood pressure during pregnancy: the BUMP survey. J Hypertens. 2021;39(5):994–1001.
Sabate E, editor. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization; 2003.
You WB, Wolf M, Bailey SC, Pandit AU, Waite KR, Sobel RM, et al. Factors associated with patient understanding of preeclampsia. Hypertens Pregnancy. 2012;31(3):341–9.
Barlow JHHJ. Thornton S Women’s experiences of hospitalisation with hypertension during pregnancy: feeling a fraud. J Reprod Infant Psychol. 2008;26(3):157–67.
Zairina E, Abramson MJ, McDonald CF, Li J, Dharmasiri T, Stewart K, et al. Telehealth to improve asthma control in pregnancy: a randomized controlled trial. Respirology. 2016;21(5):867–74.
Sheehan EKA, Kay L. Using a smartphone app to identify signs of pre-eclampsia and/or worsening blood pressure. Br J Midwifery. 2019;27(2):92–9.
Coates D, Goodfellow A, Sinclair L. Induction of labour: experiences of care and decision-making of women and clinicians. Women Birth. 2020;33(1):e1–e14.
Benton M, Salter A, Tape N, Wilkinson C, Turnbull D. Women’s psychosocial outcomes following an emergency caesarean section: a systematic literature review. BMC Pregnancy Childbirth. 2019;19(1):535.
Chuang CH, Velott DL, Weisman CS. Exploring knowledge and attitudes related to pregnancy and preconception health in women with chronic medical conditions. Matern Child Hlth J. 2010;14(5):713–9.
Seely EW, Ecker J. Chronic hypertension in pregnancy. Circulation. 2014;129(11):1254–61.
Giorgione V, Ridder A, Kalafat E, Khalil A, Thilaganathan B. Incidence of postpartum hypertension within 2 years of a pregnancy complicated by pre-eclampsia: a systematic review and meta-analysis. BJOG. 2021;128(3):495–503.
Roberts LM, Davis GK, Homer CS. Pregnancy with gestational hypertension or preeclampsia: a qualitative exploration of women’s experiences. Midwifery. 2017;46:17–23.
Garti I, Gray M, Tan JY, Bromley A. Midwives’ knowledge of pre-eclampsia management: a scoping review. Women Birth. 2021;34(1):87–104.
Shanmugalingam R, Mengesha Z, Notaras S, Liamputtong P, Fulcher I, Lee G, et al. Factors that influence adherence to aspirin therapy in the prevention of preeclampsia amongst high-risk pregnant women: a mixed method analysis. PLoS One. 2020;15(2):e0229622. https://doi.org/10.1371/journal.pone.0229622 .
Download references
Acknowledgements
We would like to thank the staff at both the Mercy Hospital for Women and the Royal Women’s Hospital for their help with this study. We would also like to thank all the women who participated.
This study did not receive any funding.
Author information
Authors and affiliations.
Centre for Medicine Use and Safety, Faculty of Pharmacy and Pharmaceutical Sciences, Monash University, 381 Royal Parade, Parkville, Melbourne, Victoria, Australia
Amyna Helou, Kay Stewart & Johnson George
Reading School of Pharmacy, University of Reading, Whiteknights, Reading, RG6 6AP, UK
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the conception and design of the study. Patient recruitment and in-depth interviews were undertaken by AH. Data analyses and interpretation were performed by AH, KS and KR. The manuscript was written by AH and critically reviewed by all authors. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Johnson George .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from Mercy Health Human Research Ethics Committee Heidelberg-Melbourne (R12/62) 08/01/2013, The Royal Women’s Hospital Research and Human Research Ethics Committee Parkville-Melbourne (R13/18) 12/07/2013 and Monash University Human Research Ethics Committee Clayton-Melbourne (CF13/117) 18/01/2013. Informed written consent was obtained prior to each interview, which included permission to audio record the conversation and use quotations when anonymously reporting and publishing the results. All methods were carried out in accordance with relevant guidelines and regulations of the ethics committees.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Helou, A., Stewart, K., Ryan, K. et al. Pregnant women’s experiences with the management of hypertensive disorders of pregnancy: a qualitative study. BMC Health Serv Res 21 , 1292 (2021). https://doi.org/10.1186/s12913-021-07320-4
Download citation
Received : 12 July 2021
Accepted : 08 November 2021
Published : 02 December 2021
DOI : https://doi.org/10.1186/s12913-021-07320-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Hypertension
- Chronic hypertension
- Pre-eclampsia
- Experiences
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Practice Test
- Fundamentals of Nursing
- Anatomy and Physiology
- Medical and Surgical Nursing
- Perioperative Nursing
- Psychiatric Mental Health Nursing
- Maternal & Child Nursing
- Community Health Nursing
- Pathophysiology
- Nursing Research
- Study Guide and Strategies
- Nursing Videos
- Work for Us!
- Privacy Policy

Pregnacy Induced Hypertension (PIH) Case Study
Pregnancy-induced hypertension (PIH) is one of the most common complications of pregnancy. This occurs during the 20 th week of gestation or late in the second trimester of pregnancy. This is a health condition wherein there is a rise in the blood pressure and disappears after the termination of pregnancy or delivery. PIH was formerly called toxaemia or the presence of toxins in the blood. This is because its occurrence was not well understood in the clinical field. Its common manifestations are hypertension, proteinuria (presence of protein in the urine), and edema. There are 2 main types of pregnancy-induced hypertension namely: pre-eclampsia and eclampsia.
- Pre-eclampsia— this is the non-convulsive form of PIH. This affects 7% of all pregnant women. Its incidence is higher in lower socio-economic groups. It may be classified either mild or severe.
- Eclampsia— this is the convulsive form of PIH. It occurs with 5% of all pre-eclampsia cases. The mortality rate among mothers is nearly 20% and fetal mortality is also high due to premature delivery.
NORMAL ANATOMY AND PHYSIOLOGY
There are a lot of bodily changes that happen during a normal pregnancy. There are external changes that are noticeable, and there are internal changes that can only be appreciated through thorough clinical examinations. Most of the changes are the body’s response to the changes in levels of hormones and the growing demands of the fetus.
The two dominant female hormones, estrogen and progesterone , change in a normal level. Along with this, a significant rise/appearance of 4 more major hormones take place; these are 1. human chorionic gonadotropin (HCG), 2. human placental lactogen, 3. prolactin, and 4. oxytocin. All these 6 hormones interact with each other simultaneously to maintain a normal pregnancy as it progresses.
The following are the major effects of these hormones in the body:
The exact cause of pregnancy-induced hypertension is unknown; however, it is highly linked to angiotensin gene T235 and the existence of other risk factors. Malnutrition and inadequate prenatal care are the greatest risk factors. The history and presence of diabetes mellitus (DM), multifetal gestation (twin pregnancies), polyhydramnios (excessive amniotic fluid), and renal diseases are also among the major contributory factors in the development of PIH. In the past, the mystery revolving around PIH postulated a lot of theories on its true origin, most of them were believed to be of toxic nature. Among these are placental infarcts, autointoxication, uremia, pyelonephritis, and maternal sensitization to total proteins.
The i ncidence of PIH among pregnant women is very high (8%), costing hundreds and thousands of lives of both mothers and fetus around the world. This commonly affects first-time pregnancies due to the presence of functioning tropoblasts (develops after the 20 th week of gestation and stays evident until after 48 hours after delivery. Age is also an important indicator in the development of PIH. Too early, as in teenage pregnancies and old primigravidas (first-time pregnancy) as in over 35 years of age put a woman higher chances of having pregnancy-induced hypertension .
PATHOPHYSIOLOGY
SIGNS AND SYMPTOMS
The signs and symptoms of the type of PIH present in a pregnant woman are based on the presentation of evident clinical manifestations. These are shown in the table below:
COMPLICATIONS
Based on the severity of the PIH present to a person or the extent of damage left/occurred, a list of possible complications can be drawn.
- Abruption placenta
- Disseminated intravascular coagulation (DIC)
- Prematurity
- Intrauterine growth retardation (IUGR)
- HELLP syndrome
- Maternal and/or fetal death
The changes of the mother and/or fetus to survive after an episode of convulsion or until delivery depends on the threshold on the effects of PIH and its complications. This can be:
- Good— if the symptoms are mild or those that are with mild pre-eclampsia and is responding well to the treatment regimen
- Poor— if there are multiple and long episodes of convulsions that are associated or lead to the development of persistent coma, hyperthermia, cyanosis, tachycardia, and liver damage.
- Congestive heart failure (CHF)
- Pulmonary edema
- Cerebral hemorrhage
- Renal failure
DIAGNOSTIC EVALUATIONS
Diagnostic evaluations are performed after episodes of convulsions or after the client has been rushed to a health care facility. These are routinely done to assess the damages and will serve as the basis for the plan of treatment.
- 24-hour urine-protein— health problem through protein determination from the involvement of the renal system.
- Serum BUN and creatinine— to evaluate renal functioning.
- Ophthalmic examination— to assess spasm, papilledema, retinal edema/detachment, and/or hemorrhages.
- Ultrasonography with stress and non- stress test— to evaluate fetal well-being after.
- Stress test —fetalheart tone (FHT) and fetal activity are electronically monitored after oxytocin induction which causes uterine contraction.
- Non-stress test —fetal heart tone (FHT) and fetal activity are electronically monitored during fetal activity (no oxytocin induction).
NURSING DIAGNOSES
- Fluid volume excess related to altered blood osmolarity and sodium/water retention.
- Altered nutrition, less than body requirements related to loss through damaged renal membrane.
- Altered tissue perfusion related to increased peripheral resistance and vasospasm in renal and cardiovascular system.
- Altered urinary elimination related to hypovolemia.
- Sensory/perceptual alterations: visual related to cerebral edema and decreased oxygenation of the brain.
- Diversional activity deficit related to decreased time for rest and sleep from stimulating environment.
- Risk for injury related to seizure episodes.
- Anxiety-related to fear of the unknown.
The overall goal of management in pregnancy-induced hypertension is directed towards the control of hypertension and the correction of developed health problems that might leadto other serious complications. Among the specially-designed treatment course for PIH are the following:
- Use of antihypertensive drugs (hydralazine-drug of choice)
- Diet-high protein, high calories
- Magnesium sulphate (MgSO4) treatment
- Diazepam and amobarbital sodium (if convulsions don’t respond to MgSO4)
- Beta-adrenergic blockers (used for acute hypertension)
- Delivery (if all treatment regimen don’t work)
NURSING MANAGEMENT
A. Assessment
- Monitor blood pressure in sitting or side-lying position.
- Monitor fetal heart tone (FHT) and fetal heart rate (FHR).
- Check for deep tendon reflexes (DTR) and clonus.
- Monitor intake and output (I&O) and proteinuria.
- Monitor daily weight and edema.
- Assess for signs of labor (possibility of abruption placenta).
- Assess for emotional status.
B. Interventions
1. Fluid balance
- Maintain patent and regulated IVF
- Strict I&O monitoring
- Monitor hematocrit level
- Vital signs monitoring every hour
- Assess breath sounds for signs of pulmonary edema
2. Tissue perfusion
- Position on left-lateral position
- Monitor fetal activity (stress and fetal activity)
3. Preventing injury
- Monitor cerebral signs and symptoms (headache, visual disturbances, and dizziness)
- Lie on left-lateral position if cerebral symptoms are present
- Secure padded side rails
- Keep oxygen suction set, tongue blade, and emergency medications (diazepam and magnesium sulphate) at all times
- Never leave an unstable patient
4. Anxiety
Discuss the health condition and planned treatment
- PIH is not lifetime
- PIH is only for the first pregnancy
- All medications and its maternal and fetal effects
Allow to ask questions and answer it truthfully
Provide emotional support to the client and family
C. Educative
- Reinforce the importance of rest and sleep
- Encourage family cooperation with the treatment course
- Discuss the laboratory procedures and alternative managements
- Include medical team, client, and significant others in the discussion
- Be realistic in discussing the possibilities of premature delivery
- No sign of pulmonary edema
- Adequate urine output
- No episode of seizure
- Stable and normal heart rate
RELATED ARTICLES MORE FROM AUTHOR
Anaphylactic shock case study -the impending doom, ectopic pregnancy case study, chronic suppurative otitis media case study, gestational diabetes mellitus case study, leave a reply cancel reply.
Save my name, email, and website in this browser for the next time I comment.

Case Study: Treating Chronic Hypertension in Pregnancy

Real-World Evidence Shows 82% Reduction in Infant RSV Hospitalizations With Nirsevimab

Pharmacy Focus - Pharmacist-Led Initiatives on C diff Rates

Investment Trends in Women's Health Are Driving Growth in Health Care Innovation

Public Health Matters: Seacrest Studios’ Impact on Children’s Hospitals and Healing Through Broadcasting

Research Suggests Acute Cardiac Events Are Common in Older Adults Hospitalized With RSV

FDA Grants Full Approval to Tisotumab Vedotin-tftv for Recurrent, Metastatic Cervical Cancer
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

- Case report
- Open access
- Published: 03 May 2024
Remission induced by renal protective therapy in nephrotic syndrome with thin basement membrane in an older patient: a case report
- Arisa Mizukawa Yoshida ORCID: orcid.org/0009-0004-5865-109X 1 ,
- Naohi Isse ORCID: orcid.org/0000-0001-5283-1592 1 ,
- Ryoma Shioji 1 &
- Kazuharu Sunami 1
Journal of Medical Case Reports volume 18 , Article number: 237 ( 2024 ) Cite this article
Metrics details
Adult nephrotic syndrome is a well-known kidney disease that causes heavy proteinuria, hypoalbuminemia, hypercholesterolemia, edema, and hypertension. The treatment varies according to its underlying cause but often faces medication resistance or adverse drug effects.
Case presentation
A Japanese woman in her 80s presented with nephrotic syndrome after a 3 year latent period of urinary protein and occult blood. She did not have any secondary causes of nephrotic syndrome. Renal biopsy revealed thin glomerular basement membrane, partial foot process fusion on electron microscopy with minor glomerular change on light microscopy, and slight coarse immunoglobulin M deposition in the mesangium on immunofluorescence microscopy, which was inconsistent with any other glomerular diseases. Without steroid treatment, she dramatically remitted from proteinuria after the administration of the renal protective agents enalapril, ezetimibe, rosuvastatin, and dapagliflozin. Recurrence after 8 months of follow-up subsided with the administration of additional doses of the agents.
Conclusions
This case illustrated the novel outcomes of combining medical treatment without steroid use for nephrotic syndrome with thin glomerular basement membrane disease. At the time of writing this report, the patient’s renal function was stable and she was free of edema, although moderate proteinuria and occult hematuria persisted. The final diagnosis was uncertain because of the lack of genetic investigation; however, the response to the aforementioned medical treatment suggests the effectiveness of the supportive therapy.
Peer Review reports
Adult nephrotic syndrome is one of the best-known presentations of kidney diseases. Inflammation of the glomeruli causes heavy proteinuria (> 3.5 g/24 hours), hypoalbuminemia (< 2.5 g/dL), hypercholesterolemia, edema, and hypertension as the main symptoms [ 1 , 2 ]. The predominant glomerular diseases causing adult-onset nephrotic syndrome include membranous nephropathy (MN), minimal change glomerular disease (MCD), focal segmental glomerulosclerosis (FSGS), mesangioproliferative glomerulonephritis (MesPGN), and membranoproliferative glomerulonephritis (MPGN) [ 1 , 2 ].
Treatment for nephrotic syndrome includes addressing underlying cause and controlling complications such as high blood pressure, high cholesterol, and edema. Medications including angiotensin-converting enzyme inhibitors and diuretics are the mainstays of symptom control.
Sequential investigations, including blood and urine laboratory examinations, initially guide to the underlying cause of the nephrotic syndrome. Definitive diagnosis usually requires renal biopsy under ultrasound, which also provides information on kidney disease severity and cues to predict the renal prognosis.
A challenge in the treatment of nephrotic syndrome is refractoriness to various medications for underlying causes, such as steroids or immunosuppressive agents. Some cases progress into life-threatening edema with end-stage renal disease.
Thin basement membrane (TBM) is a histologically diagnosed glomerular disorder with diffuse uniform thinning of the glomerular basement membrane (GBM) as observed on electron microscopy (EM) [ 3 ]. Specifically, TBM is an autosomal dominant inherited disorder of collagen IV (COL4) with variations in either COL4A3 or COL4A4 . TBM, often presenting with isolated hematuria with good renal prognosis, is distinct from Alport syndrome. Alport syndrome, genetically heterogeneous diseases with mutations either in COL4A3 , COL4A4 , or COLA45 , are associated with sensorineural hearing loss and ocular abnormalities, microscopic hematuria development, and progression to kidney insufficiency with proteinuria and hypertension [ 3 ]. However, various types of glomerulonephritis such as FSGS and immunoglobulin (Ig) A nephropathy are associated with thin GBM [ 3 ]. Therefore, it is sometimes difficult to differentiate between TBM, autosomal-dominant Alport syndrome, and glomerulonephritis such as FSGS and IgA nephropathy.
We present a case involving remission in an older woman diagnosed with nephrotic syndrome with thin GBM due to an unclassified cause. Her hypoalbuminemia responded dramatically well to the lipid-lowering agents rosuvastatin and ezetimibe, combined with enalapril and dapagliflozin in the short term.
A Japanese woman in her 80s visited our hospital because of weight gain, generalized edema, and loss of appetite, which progressively worsened over 2 months. She was under treatment for hypertension, hyperlipidemia, and insomnia in our hospital for 12 years. The initial workup revealed severe hypoalbuminemia and proteinuria. We admitted her for further examinations and treatment of the nephrotic syndrome.
Her slight proteinuria and occult hematuria appeared at her visit 3 years ago and was considered a urinary tract infection without further examinations. She had normal urine test results for a decade before the current episode. Her proteinuria was not quantified but the dipstick test indicated 2+ (approximately 100 mg/dL) (Fig. 1 ). She received aortic operations twice in the tertiary hospital: an abdominal aortic aneurysm repair operation 5 years ago and thoracic endovascular aortic repair (TEVAR) for a thoracic aortic aneurysm 4 months ago. The urinary sediment when she was admitted for TEVAR showed one to four normal-shaped red blood cells per high-power field and only one to nine hyaline casts per low-power field. Otherwise, she had a medical history of uterine fibroid, acute hepatitis, and Achilles tendon rupture at a younger age. She did not have hearing loss or eye disease. Her medications were amlodipine, rebamipide, bisoprolol, vonoprazan, tranexamic acid, ferrous sodium citrate, and brotizolam. She had taken rosuvastatin for more than 10 years before the TEVAR operation. The cardiovascular surgeon stopped prescribing rosuvastatin to her 1 month ago, that is, 3 months after discharge following the TEVAR operation, because he regarded her hypoalbuminemia as an index of malnutrition derived from loss of appetite requiring deprescription. She had never used over-the-counter drugs.
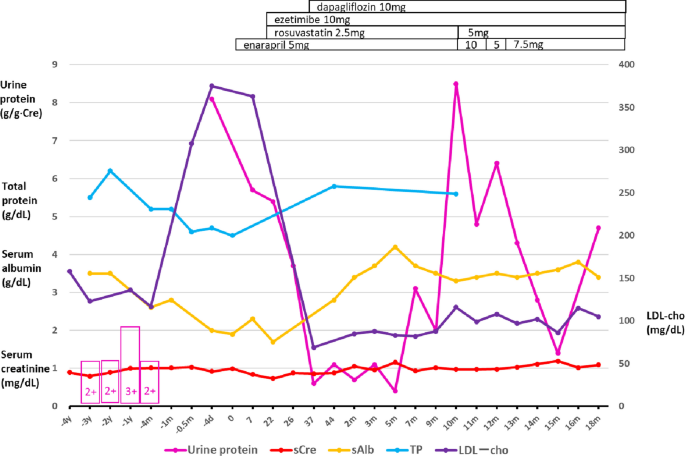
Trajectories of urine protein analysis and serum biochemistry [creatinine, albumin, total protein, and low-density lipoprotein (LDL) cholesterol]. The horizontal axis indicates the time or days before and after admission. The pink boxes with numbers indicate the results of the dipstick urinary protein test. y year, m month, d day
Her mother had died of breast and stomach cancer. There was no family history of renal diseases, hematuria, or vascular diseases. She never smoked or drank alcohol. She had no known allergies to either food or drugs.
Vital signs on admission were blood pressure 133/78 mmHg, heart rate 60 beats/minute with regular rhythm, and respiratory rate 16 breaths/minute. Height and weight were 148 cm and 56.1 kg, respectively. Bilateral extremities demonstrated pitting edema. Physical examination revealed no other problems in her chest or abdomen.
Investigations
Serum creatinine maintained around the upper limit of the normal range of 1.0 mg/dL for 3 years (Fig. 1 ). Serum total cholesterol (T-cho) and low-density lipoprotein cholesterol (LDL-cho) levels increased to 463 mg/dL and 367 mg/dL, respectively, compared with the last measured values (212 and 117 mg/dL, respectively) before the TEVAR operation. Her proteinuria was quantified as 8.1 g/g Cre after hospitalization. She was diagnosed with nephrotic syndrome (Table 1 ). The proteinuria selectivity index (PSI) reflects the glomerular permeability for small to large molecules and is useful for predicting the steroid response in glomerular diseases. It is calculated as the ratio of the clearance of IgG (large molecule) to that of transferrin (small molecule). A PSI of < 0.1 usually indicates MCD responsive to steroid therapy [ 4 ]. The patient’s PSI was 0.2, suggesting charge barrier disruption (and not size barrier disruption) as the relatively more likely cause of proteinuria. Blood tests ruled out secondary causes of nephrotic syndrome (Table 1 ). The postadmission titers of both myeloperoxidase antineutrophil cytoplasmic antibody and proteinase 3-antineutrophil cytoplasmic antibody were negative. Chest and abdominal computed tomography showed normal findings, including standard-size bilateral kidneys, except for the synthetic aortic graft and stent graft placement.
A renal biopsy specimen, obtained 9 days after admission, was used for histological investigations, including light microscopy (LM), immunofluorescence (IF) microscopy, and EM. A total of 19 glomeruli were observed in the renal biopsy specimen, 8 of which showed global sclerosis. LM images showed minor glomerular abnormalities without mesangium proliferation, spike appearance, or double contours (Fig. 2 A, B ). Crescents, adhesion formation, and segmental sclerosis, were absent in the glomeruli, and there were slight tubular atrophy, interstitial fibrosis (grade IF2), and arteriosclerosis. The IF images showed small IgM deposits on the mesangium in a granular pattern without IgA, IgG, and C3 depositions (Fig. 2 C–F). EM images revealed a diffuse and thin (approximately 180–260 nm) GBM with a partial flat fusion of the foot process with electron dense deposits in the diffuse glomeruli (Fig. 2 G). We investigated EM images of multiple glomeruli to confirm the diagnosis. The GBM thickness was measured in all capillary loops according to a general agreement. The GBM thickness was determined as the distance between the outer limits of the endothelial cell and the base of podocyte foot process cell membranes. These histological examinations ruled out nephrotic glomerular diseases such as MCD, MN, FSGS, MesPGN, and MPGN. Her glomerular sclerosis was compatible with her age and history of hypertension [ 5 ].
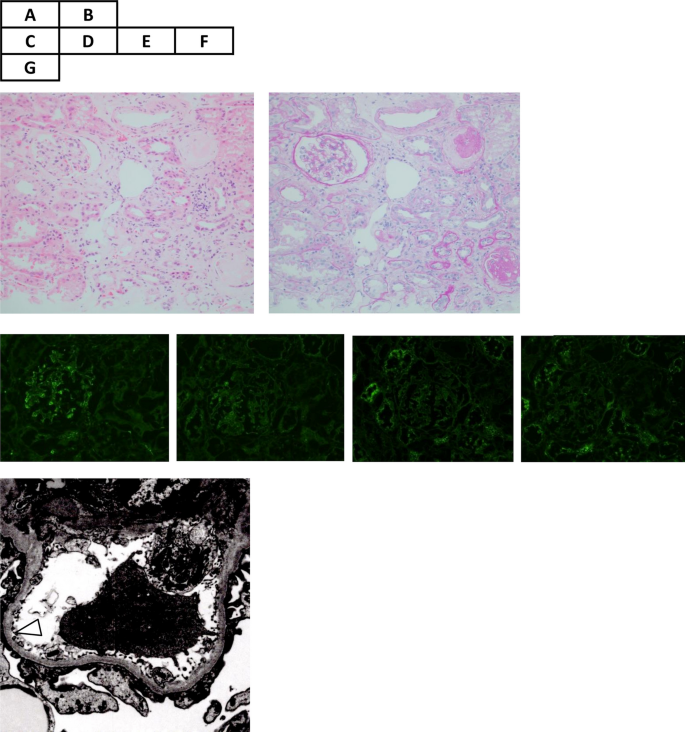
Microscopic examinations of renal biopsy specimens. Hematoxylin–eosin ( A ) and periodic acid-Schiff ( B ) staining shows minor glomerular abnormalities without mesangium proliferation, spike appearance, or double contours. There is slight tubular atrophy, interstitial fibrosis, and arteriosclerosis. Immunofluorescence shows small immunoglobulin M (IgM) deposits on the mesangium in a granular pattern ( C ), without IgA, IgG, and C3 depositions ( D – F , respectively). Electron microscopy images reveal a thin (approximately 225–250 nm) glomerular basement membrane (white triangle) with partial flat fusion of the foot process with electron dense deposits ( G ). The other glomerulus showed a much thinner (approximately 180–260 nm) basement membrane (not shown in the figure)
Differential diagnosis
First, we differentiated the case from secondary nephrotic syndromes. She never experienced episodes of fever, arthralgia, bone pains, neurological abnormalities, abdominal pains, or allergic symptoms, or those suggesting secondary causes of nephrotic syndromes, such as infections and cancer, in the initial phases of edema [ 1 ]. Blood investigation excluded secondary causes of the nephrotic syndrome, such as diabetes mellitus, systemic lupus erythematosus, and myeloma [ 1 ]. Chest and abdominal computed tomography images did not find any tumors suggesting lymphoma. She never used medicine that caused proteinuria, such as gold, antimicrobial agents, nonsteroidal anti-inflammatory drugs, penicillamine, captopril, tamoxifen, or lithium [ 1 ]. She had no infectious disease history of human immunodeficiency virus (HIV), hepatitis B and C, mycoplasma, syphilis, malaria, schistosomiasis, filariasis, or toxoplasmosis [ 1 ]. Histological investigations of renal biopsy specimens excluded amyloidosis. Her disease history and investigation, including renal biopsy, ruled out secondary causes of nephrotic syndrome.
Second, we differentiated the case from IgM nephropathy [ 6 ]. LM showed minor glomeruli changes similar to those in the second frequent pattern of IgM nephropathy. We ruled out secondary systemic diseases that cause mesangial IgM deposition, such as systemic lupus erythematosus, rheumatoid arthritis, diabetes mellitus, paraproteinemia, and Alport syndrome, by clinical and laboratory tests [ 6 ]. Additionally, we did not observe the colocalization of complementary components along with IgM, as seen in most IgM nephropathy cases. The EM findings seemed similar to those of IgM nephropathy with the fusion of foot processes. However, thin GBM has yet to be reported in IgM nephropathy [ 6 , 7 ]. Thus, we ruled out IgM nephropathy.
Third, we differentiated the case from previously reported secondary thin GBM diseases. Retrospective analyses of renal biopsies with thin GBM reported the association of thin GBM with FSGS and IgA nephropathy [ 3 , 7 , 8 ]. Approximately 40% of glomeruli showed global sclerosis but did not demonstrate segmental consolidation of capillary loops with obliteration of the capillary lumen in LM [ 9 ]. Moreover, podocyte foot process effacement, the characteristic feature of FSGS, was not present. An experienced pathologist familiar with EM examinations of the kidneys > 50 years also denied the possibility of MCD and FSGS in this case. Both glomerular diseases were histologically excluded in our case. Thin GBM were also described in Fabry’s disease and Alport syndrome [ 7 ]. There was no family history of hematuria, eye disease, or hearing disorders suggesting Alport syndrome. The “Guidelines for Testing and Management of Alport Syndrome” recommends genetic test for COL4A3 , COL4A4 , and COL4A5 to investigate TBM for differentiating between a pathogenic heterozygous COL4A3 or COL4A4 variant to avoid the underestimation of the risk of progressive renal impairment [ 10 ]. However, a wide spectrum of phenotypes and genetic polymorphism in those heterozygotes make a proper diagnosis difficult [ 10 ]. There is no guideline to recommend additional steroid therapy for COL4 heterozygotes even if we had detected some mutations in COL4 in this case [ 10 ]. Additionally, lack of commercially available genetic tests hindered us from performing the test. Furthermore, there were no mulberry bodies in the urine or inclusion bodies in the renal histological findings suggesting Fabry’s disease [ 11 ]. A recent case report described a patient with slight proteinuria (0.01 g/day) who had a novel heterozygous gene variant of intersectin 2 with thin GBM [ 12 ]. The case was similar to our case in global sclerotic glomeruli, with no specific IF findings and no remarkable podocyte foot process effacement. However, this case differed from our case, as one sibling had familial end-stage kidney disease without nephrotic syndrome.
Fourth, we ruled out anti-GBM disease based on negative results of antiglomerular basement membrane antibody and absence of crescentic glomerulonephritis and pathognomonic finding of IgG deposition along glomerular capillaries [ 13 ].
First, we started to treat generalized edema by limiting dietary sodium intake (< 5 g/day) and restricting fluid intake (< 1 L/day) with diuretics. Second, we added 5 mg of enalapril, an angiotensin-converting enzyme inhibitor, to reduce proteinuria 5 days after admission [ 14 , 15 ] (Fig. 1 ). Third, we represcribed 2.5 mg rosuvastatin to lower the LDL-cho level 10 days after admission. We also added ezetimibe to lower the LDL-c by inhibiting intestinal cholesterol absorption. She had never used ezetimibe before admission for her hyperlipidemia.
Interestingly, proteinuria rapidly decreased from 8.1 to 3.7 g/g Cre 18 days after starting the three medicines. Systemic blood pressure was stable at 130 mmHg. Subsequently, we added dapagliflozin for its antiproteinuric and renal protective effects 30 days after admission. Proteinuria declined to 0.7–1.1 g/g Cre at incomplete remission. Just before discharge, there was no reason to consider trying steroid therapy for a patient who only had 0.6 g/g Cre proteinuria without edema. Moreover, the histopathological results did not suggest steroid-responsive glomerulonephritis, such as minimal change disease. In such a case that was in remission, it was reasonable to withhold a steroid therapy trial for an elderly patient with an undetermined diagnosis, considering its systemic adverse effects. She was discharged 46 days after admission. While waiting for the EM report, we confirmed her final histopathological diagnosis after discharge: nephrotic syndrome with thin GBM due to an unclassified cause.
Outcome and follow-up
Her kidney function maintained around 1.1 mg/dL of serum creatinine without edema recurrence. Her daily proteinuria amount fluctuated between 0.4 and 3.1 g/g Cre after discharge (Fig. 1 ). At the time of remission of nephrotic syndrome, the urine occult blood disappeared for 2 months but reappeared as 2+ subsequently. Heavy proteinuria recurred 8 months after discharge. Increased doses of enalapril (10 mg) and rosuvastatin (5 mg) dramatically reduced the proteinuria from 8.4 to 4.8 g/g Cre in 2 weeks, while maintaining the serum albumin level at 3.3–3.4 g/dL. The ezetimibe and dapagliflozin doses were maintained as well, leading to incomplete remission of proteinuria subsequently.
Discussion and conclusions
The main findings of our case were as follows:
A 3 year latent period of proteinuria and urinary occult blood before the occurrence of nephrotic edema;
Histopathological features of thin GBM and partial foot process fusion in the diffuse glomeruli, inconsistent with any other glomerular diseases;
Dramatic remission of proteinuria in 17 days after addition of enalapril and ezetimibe and restarting of rosuvastatin;
A possible additional effect of dapagliflozin on the reduction of proteinuria;
Maintenance of incomplete remission from nephrotic syndrome without steroid or immunosuppressant use.
Her edema and weight increase worsened after stopping rosuvastatin. We were unsure whether the initial worsening of proteinuria was due to stopping rosuvastatin or the natural course of her glomerular disease. Her nephrotic syndrome started to remit after restarting rosuvastatin. Nephrotic syndrome results in marked elevation of serum T-cho and LDL-cho due to increased production and impaired catabolism/clearance of LDL and apoB-100 [ 16 ]. In nephrotic patients, dyslipidemia is usually treated to prevent long-term cardiovascular events [ 1 ]. LDL-cho toxicity on the kidney and the effect of statin on preventing renal damage has been addressed in reviews [ 16 ]. The mechanisms of nephrotoxicity are (1) the uptake of abnormal lipoproteins by glomerular mesangial cells, which promotes glomerulosclerosis and (2) reabsorption of filtered albumin and other lipid-containing proteins, leading to the accumulation of lipids and cytotoxicity in proximal tubular epithelial cells [ 16 ]. The ability of statins to improve renal parameters in individuals with chronic kidney disease (CKD) is still under debate [ 17 ]. Non-dialysis-dependent CKD patients, early stage CKD patients, kidney transplant patients, and patients receiving peritoneal dialysis treated with statins have all reported reductions in proteinuria and kidney function preservation. Therefore, statin use can be considered in the subset of these patient groups with elevated LDL-cho, particularly those with nephrotic proteinuria [ 16 ]. Controversially, only the use of rosuvastatin for patients without diabetes and proteinuria was questioned because of its possibility to intensify proteinuria by the high concentration of rosuvastatin and its metabolites in the kidney, especially at high doses in a post hoc analysis to compare statins [ 16 ]. Our nondiabetic patient started to use the usual dose of 2.5 mg rosuvastatin, which might have benefited from the antiproteinuric effect of the statin.
It is interesting that the antiproteinuric effect of the statin, combined with enalapril, appeared only in 17 days. Notably, a relatively low PSI of 0.2 at admission was suggestive of a charge-barrier defect in the glomeruli. However, it is uncertain if the short-term hypoalbuminemia recovery suggests the case’s charge-barrier recovery after medical treatment. Dapagloflizin treatment would synergistically work with combined medications. A case study demonstrated the antiproteinuric effect of dapagliflozin on a diabetic patient with nephrotic syndrome [ 18 ]. The efficacy of SGLT2 inhibitors on nondiabetic nephrotic syndrome has still been unclear. However, the protective effect of dapagliflozin on kidney function was reported in nondiabetic patients [ 19 ]. It is reasonable to use dapagliflozin to prevent the progression of end-stage kidney disease in this patient.
There are a few reports of thin GBM concurrent with MCD or FSGS [ 20 , 21 , 22 ]. Our case did not demonstrate the clinical and pathological findings consistent with MCD as follows: (1) a lack of typical effacement of podocytes on EM findings, which is seen in MCD; (2) occult hematuria started 3 years before the onset of nephrotic syndrome; and (3) fluctuating proteinuria after the onset, remission at 1 month, and relapse at 10 months without steroid treatment, which is atypical for MCD. Additionally, our case was not compatible with the features of FSGS for the same reasons. Moreover, the pattern of thin GBM is diffused in this patient compared with focal thin GBM observed in MCD or other glomerulonephritis in a previous report [ 3 ]. In this case, the authors and the pathologist definitively ruled out MCD, both clinically and pathologically.
Our patient might be a variant carrier of COL4A3 or COL4A4 mutations, which can lead to late-onset nephropathy with thin GBM, namely, autosomal dominant Alport syndrome considering the absence of extrarenal symptoms and the patterns of renal histopathologic findings [ 23 ]. Additionally, some case reports described aortic aneurysms related to Alport syndrome, although COL4 dysfunction has not yet been considered as an independent risk factor of aortic aneurysms [ 24 ]. To date, none of her family members have presented with asymptomatic hematuria or aortic diseases; however, careful observation of them is necessary. The evidence of effectiveness of renin–angiotensin system inhibitors for Alport syndrome to delay the development of renal impairment justifies the use of enalapril in this patient. However, the effectiveness of lipid-lowering agents and SGLT2 inhibitors are unknown in Alport syndrome.
This case illustrated the novel outcomes of combining medical treatment without steroid use for nephrotic syndrome with thin GBM disease. At the time of writing this report, the patient’s renal function was stable for 2 years and she was free of edema, although moderate proteinuria and occult hematuria persisted. However, it would be reasonable to consider steroid therapy if we can exclude a COL4 defect in this case when her nephrotic syndrome relapses, causing renal function deterioration. The final diagnosis was uncertain because of the lack of genetic investigation; however, the response to the aforementioned medical treatment suggests the effectiveness of the supportive therapy.
Availability of data and materials
The datasets used and analyzed in the current study are available from the corresponding author upon reasonable request.
Abbreviations
Membranous nephropathy
Minimal change glomerular disease
Focal segmental glomerulosclerosis
Mesangioproliferative glomerulonephritis
Membranoproliferative glomerulonephritis
Glomerular basement membrane
Thin basement membrane
Electron microscopy
Collagen IV
Thoracic endovascular aortic repair
Total cholesterol
Low-density lipoprotein cholesterol
Proteinuria selectivity index
Light microscopy
Immunofluorescence
Immunoglobulin
Chronic kidney disease
Hull RP, Goldsmith DJA. Nephrotic syndrome in adults. BMJ. 2008;336:1185–9.
Article PubMed PubMed Central Google Scholar
Suryawanshi M, Karnik S, Roy S. Clinicopathological analysis of glomerular disease of adult onset nephrotic syndrome in an Indian cohort—a retrospective study. J Clin Diagn Res. 2017;11:25–30.
Google Scholar
Uzzo M, Moroni G, Ponticelli C. Thin basement membrane: an underrated cause of end-stage renal disease. Nephron. 2023. https://doi.org/10.1159/000528243 .
Article PubMed Google Scholar
Hamilton P, Myers J, Gillham J, Ayers G, Brown N, Venning M. Urinary protein selectivity in nephrotic syndrome and pregnancy: resurrection of a biomarker when renal biopsy is contraindicated. Clin Kidney J. 2014;7(6):595–8.
Article CAS PubMed PubMed Central Google Scholar
Hommos MS, Zeng C, Liu Z, Troost JP, Rosenberg AZ, Palmer M, et al . Global glomerulosclerosis with nephrotic syndrome; the clinical importance of age adjustment. Kidney Int. 2018;93:1175–82.
Mubarak M, Kazi JI. IgM nephropathy revisited. Nephrourol Mon. 2012;4:603–8.
Kfoury H, Arafah M. The pathological spectrum associated with the ultrastructural finding of thin glomerular basement membrane: a tertiary medical city experience and review of the literature. Ultrastruct Pathol. 2017;41:51–4.
Cosio FG, Falkenhain ME, Sedmak DD. Association of thin glomerular basement membrane with other glomerulopathies. Kidney Int. 1994;46:471–4.
Article CAS PubMed Google Scholar
Fervenza FC, Sethi S. Focal segmental glomerulosclerosis: clinical features and diagnosis. In: Glassock RJ, Rovin BH, editors. UpToDate. Waltham: UpToDate Inc; 2023.
Savige J, Lipska-Zietkiewicz BS, Watson E, Hertz JM, Deltas C, Mari F, et al . Guidelines for genetic testing and management of Alport syndrome. Clin J Am Soc Nephrol. 2022;17:143–54. Erratum in: Clin J Am Soc Nephrol. 2023;18:510.
Rusu E-E, Zilisteanu D-S, Ciobotaru L-M, Gherghiceanu M, Procop A, Jurcut RO, et al . The impact of kidney biopsy for Fabry nephropathy evaluation on patients’ management and long-term outcomes: experience of a single center. Biomedicines. 2022;10:1520.
Kondo M, Mori T, Oshita T, Ohashi A, Sohara E, Uchida S, et al . Case of hereditary kidney disease presenting thin basement membrane with a single heterozygous variant of Intersectin 2. J Rural Med. 2023;18:143–8.
Pusey CD, Segelmark M. Anti-GBM (Goodpasture) disease: pathogenesis, clinical manifestations, and diagnosis. In: Glassock RJ, Fervenza FC, editors. UpToDate. Waltham: UpToDate Inc; 2023.
Gansevoort RT, Sluiter WJ, Hemmelder MH, de Zeeuw D, de Jong PE. Antiproteinuric effect of blood-pressure-lowering agents: a meta- analysis of comparative trials. Nephrol Dial Transplant. 1995;10:1963–74.
CAS PubMed Google Scholar
The GISEN Group (Gruppo Italiano di Studi Epidemiologici in Nefrologia). Randomised controlled trial of effect of ramipril on decline in glomerular filtration rate and risk of terminal renal failure in proteinuric, non diabetic nephropathy. Lancet. 1997;349:1857–63.
Article Google Scholar
Vaziri ND, Anzalone DA, Catini J. Statins in Chronic Kidney Disease: when and when not to use them. J Fam Pract. 2016;65: supp_az_0816.
PubMed Google Scholar
Kong X, Yuan H, Fan J, Li Z, Wu T, Jiang L. Lipid-lowering agents for nephrotic syndrome. Cochrane Database Syst Rev. 2013;12: CD005425.
Murashima R, Sai E, Tagawa Y, Yanagawa H, Ishiwata S, Kawaguchi Y, et al . Usefulness of dapagliflozin for nephrotic syndrome secondary to diabetic kidney disease. Intern Med. 2022;61:3699–702.
Heerspink HJL, Stefánsson BV, Correa-Rotter R, Chertow GM, Greene T, Hou FF, et al . Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020;383:1436–46.
Ogawa R, Miyoshi K, Nagao T, Jotoku M, Irita J, Okura T, et al . Ultrastructure of glomerular podocyts in the incipient phase of minimal change nephrotic syndrome with thin basement membrane disease. Nihon Jinzo Gakkai Shi. 2012;54:1192–6.
Chiba Y, Nagasawa T, Kin S, Takahashi K, Yoshida M, Oe Y, et al . Spontaneous remission of minimal change nephrotic syndrome in an elderly man. CEN Case Rep. 2021;10:301–7.
van Paassen P, van Breda Vriesman PJ, van Rie H, Tervaert JW. Signs and symptoms of thin basement membrane nephropathy: a prospective regional study on primary glomerular disease—The Limburg Renal Registry. Kidney Int. 2004;66:909–13.
Matthaiou A, Poulli T, Deltas C. Prevalence of clinical, pathological and molecular features of glomerular basement membrane nephropathy caused by COL4A3 or COL4A4 mutations: a systematic review. Clin Kidney J. 2020;13:1025–36.
Kamiar A, Alitter Q, Capcha JMC, Saad A, Webster KA, Shehadeh LA. Ascending aortic aneurysm and histopathology in Alport syndrome: a case report. BMC Nephrol. 2023;24:1–6.
Download references
Acknowledgements
The authors would like to thank Dr. Akira Hashimoto, MD, in Okayama Kyoritsu General Hospital for contributing to the renal biopsy and clinical advice. We also thank Dr. Makio Kawakami, MD, in Japanese Red Cross Narita Hospital for the electron microscopy exams and valuable advice on the diagnosis.
None applicable.
Author information
Authors and affiliations.
Okayama Kyoritsu General Hospital, 8-10, Akasaka-Honmachi, Naka-ku, Okayama, 703-8511, Japan
Arisa Mizukawa Yoshida, Naohi Isse, Ryoma Shioji & Kazuharu Sunami
You can also search for this author in PubMed Google Scholar
Contributions
AMY, NI, RS, and KS diagnosed and provided clinical care. AMY and NI designed the study and wrote the manuscript. NI revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Naohi Isse .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Yoshida, A.M., Isse, N., Shioji, R. et al. Remission induced by renal protective therapy in nephrotic syndrome with thin basement membrane in an older patient: a case report. J Med Case Reports 18 , 237 (2024). https://doi.org/10.1186/s13256-024-04564-6
Download citation
Received : 29 November 2023
Accepted : 13 April 2024
Published : 03 May 2024
DOI : https://doi.org/10.1186/s13256-024-04564-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nephrotic syndrome
- Thin glomerular basement membrane
- Rosuvastatin
- Dapagliflozin
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Description of Case. A 21-year-old pregnant woman, gravida 2 para 1, presented with hypertension and proteinuria at 20 weeks of gestation. She had a history of pre-eclampsia in her first pregnancy one year ago. During that pregnancy, at 39 weeks of gestation, she developed high blood pressure, proteinuria, and deranged liver function.
Case 1 • 33 yo G4P3003 @ 28w2d with chronic hypertension on labetalol 600 mg TID. The patient presents to the OB office with BP logs concerning for severe range HTN as an outpatient 170s/80s, although her office BP was noted to be 135/80. She has no other symptoms. • OBHx: 3 uncomplicated pregnancies, cesarean section x3 • PMHX:
Dr. Andrea L. Utz (Endocrinology): A 35-year-old pregnant woman (gravida 2, para 1) was admitted to this hospital at 19 weeks and 6 days of gestation because of the recent onset of hypertension ...
First, more aggressive treatment of hypertension in pregnancy prevents the development of severe hypertension, as demonstrated by both a systematic review of randomized trials 152 and CHIPS (Control of Hypertension in Pregnancy Study), in which the average BP achieved by tight control was 133/85 mm Hg. 14 Although comparison of less tight ...
The prevalence of hypertension in reproductive-aged women is estimated to be 7.7%. 1 Hypertensive disorders of pregnancy, an umbrella term that includes preexisting and gestational hypertension, preeclampsia, and eclampsia, complicate up to 10% of pregnancies and represent a significant cause of maternal and perinatal morbidity and mortality. 2 ...
"Pregnancy-induced hypertension" is a term referring to hypertensive disorders of pregnancy in general, but lacks the specificity of the other terms, and so the Brighton definitions will refer only to "eclampsia," "preeclampsia," and "gestational hypertension." ... Case/study participant identifiers (e.g. first name initial ...
Being multigravida and age during current pregnancy between 25-30 years which have a significant association with pregnancy-induced hypertension with case to control ratio 1:2 and Odds ratio (OR) = 4 and using the following assumptions: power 80%, confidence level 95% (Table 1). The final sample size was taken from the women who were ...
To investigate the risk factors and maternal and fetal outcomes of preeclampsia after pregnancy in patients with primary chronic hypertension. A total of 500 singleton pregnant women with a history of hypertension who were admitted for delivery at our Hospital from March 2015 to May 2022 were retrospectively collected by random sampling and divided into the non-occurrence group (n = 200) and ...
Hypotension in pregnant women: a population-based case-control study of pregnancy complications and birth outcomes. Hypertens Res. 2011; 34:55-61. doi: 10.1038/hr.2010.172 Crossref Medline Google Scholar; 43. Li HT, Xue M, Hellerstein S, Cai Y, Gao Y, Zhang Y, Qiao J, Blustein J, Liu JM.
Pregnancy-induced hypertension (PIH) is associated with preterm delivery but its independent impact on neonatal outcomes remains unclear. ... Cohort and case-control studies published in English ...
Abstract. Background: Pregnancy-induced hypertension (PIH) is a leading cause of maternal and fetal morbidity and mortality. Although case management programs have been proposed to improve maternal and fetal outcomes in high-risk pregnancies, limited data are available regarding the effect of case management on women with PIH. Purpose: The aim ...
Pregnancy-induced hypertension (PIH) is one of the leading causes of maternal and fetal morbidity and mortality from conception to birth [1,2,3].Increasing evidence has shown that PIH can lead to ...
INTRODUCTION. Pregnancy Induced Hypertension (PIH) is one of the commonest causes of both maternal 1 as well as neonatal mortality 2 and morbidity that develops as a result of pregnancy and generally regresses after delivery, affecting about 5-8 % of pregnant women, moreover 5-22% of pregnancies especially in developing countries. 3. The mortality is closely associated with the severity of ...
Pregnancy-induced hypertension (PIH) is regarded as a multi-system disorder that is defined as persistent hypertension of more than 140/90 mmHg during the gestational period. 1, ... However, a case-control study in Tunisian women suggested that the frequencies of genotypes and alleles rs699947, rs833061, rs1570360, rs2010963, ...
Pregnancy-induced hypertension (PIH) affects 6%-10% of pregnant women worldwide ... Curry et al. (2006) conducted a nurse case management study targeting pregnant women at risk for abuse. Women were randomly assigned to the routine-care control group or the experimental group, with members of the latter group provided with videos, telephone ...
Hence a study was undertaken to assess the impact of Pregnancy Induced Hypertension on fetal outcomes among mothers with PIH who delivered at tertiary care hospital, Dadra & Nagar Haveli. Method: It was a cross sectional study conducted at Shri Vinoba Bhave Civil Hospital, Silvassa, Dadra & Nagar Haveli from September to November 2020.The ...
Background. Hypertensive disorders are a leading cause of mortality and morbidity during pregnancy. Despite multiple national and international clinical guidelines and a plethora of research in the field of optimising management, there has been limited research describing the perspectives and experiences of pregnant women with the management of hypertensive disorders of pregnancy (HDP).
JACC Heart Fail 2023;May 10: [Epub ahead of print]. In a large, nationwide, retrospective cohort study, the rate of HF in women with pregnancy-induced hypertension was higher compared to normotensive women (HR, 1.8; 95% CI, 1.6-2.0). The risk for both ischemic (ICM) and nonischemic cardiomyopathy (NICM) was increased with pregnancy-induced ...
Being multigravida and age during current pregnancy between 25-30 years which have a significant association with pregnancy-induced hypertension with case to control ratio 1:2 and Odds ratio (OR) = 4 and ... Maternal and foetal outcomes in Pregnancy Induced Hypertension-A hospital based study. International journal of pharmaceutical science ...
Background Hypertensive disorders are a leading cause of mortality and morbidity during pregnancy. Despite multiple national and international clinical guidelines and a plethora of research in the field of optimising management, there has been limited research describing the perspectives and experiences of pregnant women with the management of hypertensive disorders of pregnancy (HDP ...
Modified date: September 2, 2020. Pregnancy-induced hypertension (PIH) is one of the most common complications of pregnancy. This occurs during the 20 th week of gestation or late in the second trimester of pregnancy. This is a health condition wherein there is a rise in the blood pressure and disappears after the termination of pregnancy or ...
Chronic hypertension during pregnancy increases the risk of poor pregnancy and birth outcomes. 3,4 Although consensus exists to use antihypertensive therapy to treat severe hypertension (systolic ≥160, diastolic ≥105-110 mmHg) during pregnancy, the benefits and safety for treating mild chronic hypertension during pregnancy are unclear.
Prevalence of pregnancy induced hypertension: The prevalence of pregnancy induced hypertension among women attending delivery service in the three hospitals of this study was 33(7.9%). The mean of systolic blood pressure was 110.72±15.315 with range of 90 mmHg to 210 mmHg, and the mean of diastolic blood pressure was 72.71±13.093 with range ...
Adult nephrotic syndrome is a well-known kidney disease that causes heavy proteinuria, hypoalbuminemia, hypercholesterolemia, edema, and hypertension. The treatment varies according to its underlying cause but often faces medication resistance or adverse drug effects. A Japanese woman in her 80s presented with nephrotic syndrome after a 3 year latent period of urinary protein and occult blood.
A ratio of pregnancy-induced hypertension cases to controls 1:2, power 80, confidence level 95%, and odds ratio 4.10 by considering multiple pregnancy that had significant association with pregnancy-induced hypertension, and the proportion of exposure among controls is 4.5% from a study conducted in Ethiopia, Tigray region public hospitals . We ...