Type 2 Diabetes Research At-a-Glance
The ADA is committed to continuing progress in the fight against type 2 diabetes by funding research, including support for potential new treatments, a better understating of genetic factors, addressing disparities, and more. For specific examples of projects currently funded by the ADA, see below.
Greg J. Morton, PhD
University of Washington
Project: Neurocircuits regulating glucose homeostasis
“The health consequences of diabetes can be devastating, and new treatments and therapies are needed. My research career has focused on understanding how blood sugar levels are regulated and what contributes to the development of diabetes. This research will provide insights into the role of the brain in the control of blood sugar levels and has potential to facilitate the development of novel approaches to diabetes treatment.”
The problem: Type 2 diabetes (T2D) is among the most pressing and costly medical challenges confronting modern society. Even with currently available therapies, the control and management of blood sugar levels remains a challenge in T2D patients and can thereby increase the risk of diabetes-related complications. Continued progress with newer, better therapies is needed to help people with T2D.
The project: Humans have special cells, called brown fat cells, which generate heat to maintain optimal body temperature. Dr. Morton has found that these cells use large amounts of glucose to drive this heat production, thus serving as a potential way to lower blood sugar, a key goal for any diabetes treatment. Dr. Morton is working to understand what role the brain plays in turning these brown fat cells on and off.
The potential outcome: This work has the potential to fundamentally advance our understanding of how the brain regulates blood sugar levels and to identify novel targets for the treatment of T2D.
Tracey Lynn McLaughlin, MD
Stanford University
Project: Role of altered nutrient transit and incretin hormones in glucose lowering after Roux-en-Y gastric bypass surgery
“This award is very important to me personally not only because the enteroinsular axis (gut-insulin-glucose metabolism) is a new kid on the block that requires rigorous physiologic studies in humans to better understand how it contributes to glucose metabolism, but also because the subjects who develop severe hypoglycemia after gastric bypass are largely ignored in society and there is no treatment for this devastating and very dangerous condition.”
The problem: Roux-en-Y gastric bypass (RYGB) surgery is the single-most effective treatment for type 2 diabetes, with persistent remission in 85% of cases. However, the underlying ways by which the surgery improves glucose control is not yet understood, limiting the ability to potentially mimic the surgery in a non-invasive way. Furthermore, a minority of RYGB patients develop severe, disabling, and life-threatening low-blood sugar, for which there is no current treatment.
The project: Utilizing a unique and rigorous human experimental model, the proposed research will attempt to gain a better understanding on how RYGB surgery improves glucose control. Dr. McLaughlin will also test a hypothesis which she believes could play an important role in the persistent low-blood sugar that is observed in some patients post-surgery.
The potential outcome: This research has the potential to identify novel molecules that could represent targets for new antidiabetic therapies. It is also an important step to identifying people at risk for low-blood sugar following RYGB and to develop postsurgical treatment strategies.
Rebekah J. Walker, PhD
Medical College of Wisconsin
Project: Lowering the impact of food insecurity in African Americans with type 2 diabetes
“I became interested in diabetes research during my doctoral training, and since that time have become passionate about addressing social determinants of health and health disparities, specifically in individuals with diabetes. Living in one of the most racially segregated cities in the nation, the burden to address the needs of individuals at particularly high risk of poor outcomes has become important to me both personally and professionally.”
The problem: Food insecurity is defined as the inability to or limitation in accessing nutritionally adequate food and may be one way to address increased diabetes risk in high-risk populations. Food insecure individuals with diabetes have worse diabetes outcomes and have more difficulty following a healthy diet compared to those who are not food insecure.
The project: Dr. Walker’s study will gather information to improve and then will test an intervention to improve blood sugar control, dietary intake, self-care management, and quality of life in food insecure African Americans with diabetes. The intervention will include weekly culturally appropriate food boxes mailed to the participants and telephone-delivered diabetes education and skills training. It will be one of the first studies focused on the unique needs of food insecure African American populations with diabetes using culturally tailored strategies.
The potential outcome: This study has the potential to guide and improve policies impacting low-income minorities with diabetes. In addition, Dr. Walker’s study will help determine if food supplementation is important in improving diabetes outcomes beyond diabetes education alone.

Research Summaries
Keep up with the latest diabetes and diabetes-related studies with these brief overviews. Each summary provides main points, methods, and findings and includes a link to the article.
Diabetes Management and Education
Reaching treatment goals could help people living with type 2 diabetes increase their life expectancy by 3 years or in some cases by as much as 10 years. Read the summary .
Adults who receive diabetes education are more likely to follow recommended preventive care practices that lead to better diabetes management. Read the summary .
In 2017, the total cost of diabetes complications was over $37 billion among Medicare beneficiaries 65 or older with type 2 diabetes. Read the summary .
Kids and teens can get both type 1 and type 2 diabetes. New research shows how diabetes rates in young people may rise by 2060. Read the summary .
New USPSTF and ADA guidelines lower the age for prediabetes and type 2 diabetes screening to 35. This study examined if testing practices aligned with guidelines and which populations were less likely to receive testing. Read the summary .
The SEARCH for Diabetes in Youth study reports trends in young people who are being diagnosed with type 1 and type 2 diabetes. Read the summary .
Recent guidelines recommend newer types of diabetes medications, and most Americans living with type 2 diabetes are eligible. Read the summary .
Chronic Kidney Disease
End-stage kidney disease—kidney failure that requires dialysis or a kidney transplant—can lead to disability and early death, is expensive to treat, and cases are on the rise. Read the summary .
- Reports and Publications
- Research Projects
- US Diabetes Surveillance System
To receive updates about diabetes topics, enter your email address:
- Diabetes Home
- State, Local, and National Partner Diabetes Programs
- National Diabetes Prevention Program
- Native Diabetes Wellness Program
- Chronic Kidney Disease
- Vision Health Initiative
- Heart Disease and Stroke
- Overweight & Obesity
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Clinical Trials
Type 2 diabetes.
Displaying 96 studies
The purpose of this study is to identify changes to the metabolome (range of chemicals produced in the body) and microbiome (intestine microbe environment) that are unique to Roux-en-Y gastric bypass surgery and assess the associated effect on the metabolism of patients with type 2 diabetes.
The purpose of this study is to evaluate the impact of a digital storytelling intervention derived through a community-based participatory research (CBPR) approach on type 2 diabetes mellitus (T2D) outcomes among Hispanic adults with poorly controlled type 2 diabetes mellitus (T2D) in primary care settings through a randomized clinical trial.
The purpose of this study is to assess the impact of a whole food plant-based diet on blood sugar control in diabetic patients versus a control group on the American Diabetics Association diet before having a total hip, knee, or shoulder replacement surgery.
The purpose of this study is to learn more about if the medication, Entresto, could help the function of the heart and kidneys.
The primary aim of this study is to compare the outcome measures of adult ECH type 2 diabetes patients who were referred to onsite pharmacist services for management of their diabetes to similar patients who were not referred for pharmacy service management of their diabetes. A secondary aim of the study is to assess the Kasson providers’ satisfaction level and estimated pharmacy service referral frequency to their patients. A tertiary aim of the study is to compare the hospitalization rates of type 2 diabetes rates who were referred to onsite pharmacist services for management of their diabetes to similar patients ...
To explore the feasibility of conducting a family centered wellness coaching program for patients at high risk for developing diabetes, in a primary care setting.
To determine engagement patterns.
To describe characteristics of families who are likely to participate.
To identify barriers/limitations to family centered wellness coaching.
To assess whether a family centered 8 week wellness coaching intervention for primary care patients at high risk for diabetes will improve self-care behaviors as measured by self-reported changes in physical activity level and food choices.
This study is being done to understand metformin's mechanisms of action regarding glucose production, protein metabolism, and mitochondrial function.
The purpose of this study is to assess the effectiveness of Revita® DMR for improving HbA1c to ≤ 7% without the need of insulin in subjects with T2D compared to sham and to assess the effectiveness of DMR versus Sham on improvement in Glycemic, Hepatic and Cardiovascular endpoints.
The purpose of this study is to evaluate 6 weeks of home use of the Control-IQ automated insulin delivery system in individuals with type 2 diabetes.
This study will evaluate whether bile acids are able to increase insulin sensitivity and enhance glycemic control in T2DM patients, as well as exploring the mechanisms that enhance glycemic control. These observations will provide the preliminary data for proposing future therapeutic as well as further mechanistic studies of the role of bile acids in the control of glycemia in T2DM.
The purpose of this study is to determine if Inpatient Stress Hyperglycemia is an indicator of future risk of developing type 2 Diabetes Mellitus.
The purpose of this study is to assess the effectiveness of a digital storytelling intervention derived through a community based participatory research (CBPR) approach on self-management of type 2 diabetes (T2D) among Somali adults.
The GRADE Study is a pragmatic, unmasked clinical trial that will compare commonly used diabetes medications, when combined with metformin, on glycemia-lowering effectiveness and patient-centered outcomes.
The overall goal of this proposal is to determine the effects of acute hyperglycemia and its modulation by Glucagon-like Peptide-1 (GLP-1) on myocardial perfusion in type 2 diabetes (DM). This study plan utilizes myocardial contrast echocardiography (MCE) to explore a) the effects of acute hyperglycemia on myocardial perfusion and coronary flow reserve in individuals with and without DM; and b) the effects of GLP-1 on myocardial perfusion and coronary flow reserve during euglycemia and hyperglycemia in DM. The investigators will recruit individuals with and without DM matched for age, gender and degree of obesity. The investigators will measure myocardial perfusion ...
The purpose of this study is to test the hypothesis that patients with T2DM will have greater deterioration in BMSi and in cortical porosity over 3 yrs as compared to sex- and age-matched non-diabetic controls; and identify the circulating hormonal (e.g., estradiol [E2], testosterone [T]) and biochemical (e.g., bone turnover markers, AGEs) determinants of changes in these key parameters of bone quality, and evaluate the possible relationship between existing diabetic complications and skeletal deterioration over time in the T2DM patients.
The purpose of this study is to determine the effect of endogenous GLP-1 secretion on islet function in people with Typr 2 Diabetes Mellitus (T2DM).
GLP-1 is a hormone made by the body that promotes the production of insulin in response to eating. However, there is increasing evidence that this hormone might help support the body’s ability to produce insulin when diabetes develops.
The purpose of this study is to assess whether psyllium is more effective in lowering fasting blood sugar and HbA1c, and to evaluate the effect of psyllium compared to wheat dextrin on the following laboratory markers: LDL-C, inflammatory markers such as ceramides and hsCRP, and branch chain amino acids which predict Diabetes Mellitus (DM).
This mixed methods study aims to answer the question: "What is the work of being a patient with type 2 diabetes mellitus?" .
The purpose of this study is to assess penile length pre- and post-completion of RestoreX® traction therapy compared to control groups (no treatment) among men with type II diabetes.
This observational study is conducted to determine how the duodenal layer thicknesses (mucosa, submucosa, and muscularis) vary with several factors in patients with and without type 2 diabetes.
This trial is a multi-center, adaptive, randomized, double-blind, placebo- and active- controlled, parallel group, phase 2 study in subjects with Type 2 Diabetes Mellitus to evaluate the effect of TTP399 on HbA1c following administration for 6 months.
The purpose of this study is to find the inheritable changes in genetic makeup that are related to the development of type 2 diabetes in Latino families.
The objective of this early feasibility study is to assess the feasibility and preliminary safety of the Endogenex Divice for endoscopic duodenal mucosal regeneration in patients with type 2 diabetes (T2D) inadequately controlled on 2-3 non-insulin glucose-lowering medications.
The purpose of this study is to determine the impact of patient decision aids compared to usual care on measures of patient involvement in decision-making, diabetes care processes, medication adherence, glycemic and cardiovascular risk factor control, and use of resources in nonurban practices in the Midwestern United States.
The purpose of this study is to evaluate if breathing pure oxygen overnight affects insulin sensitivity in participants with diabetes.
The purpose of this study is to estimate the risk of diabetes related complications after total pancreatectomy. We will contact long term survivors after total pancreatectomy to obtain data regarding diabetes related end organ complications.
The purpose of this study is to understand nighttime glucose regulation in humans and find if the pattern is different in people with Type 2 diabetes
The study is being undertaken to understand how a gastric bypass can affect a subject's diabetes even prior to their losing significant amounts of weight. The hypothesis of this study is that increased glucagon-like peptide-1 (GLP-1) secretion explains the amelioration in insulin secretion after Roux-en-Y Gastric Bypass (RYGB) surgery.
The investigators will determine whether people with high muscle mitochondrial capacity produce higher amount of reactive oxygen species (ROS) on consuming high fat /high glycemic diet and thus exhibit elevated cellular oxidative damage. The investigators previously found that Asian Indian immigrants have high mitochondrial capacity in spite of severe insulin resistance. Somalians are another new immigrant population with rapidly increasing prevalence of diabetes. Both of these groups traditionally consume low caloric density diets, and the investigators hypothesize that when these groups are exposed to high-calorie Western diets, they exhibit increased oxidative stress, oxidative damage, and insulin resistance. The investigators will ...
The purpose of this research is to find out how genetic variations in GLP1R, alters insulin secretion, in the fasting state and when blood sugars levels are elevated. Results from this study may help us identify therapies to prevent or reverse type 2 diabetes mellitus.
The study purpose is to understand patients’ with the diagnosis of Diabetes Mellitus type 1 or 2 perception of the care they receive in the Diabetes clinic or Diabetes technology clinic at Mayo Clinic and to explore and to identify the healthcare system components patients consider important to be part of the comprehensive regenerative care in the clinical setting.
However, before we can implement structural changes or design interventions to promote comprehensive regenerative care in clinical practice, we first need to characterize those regenerative practices occurring today, patients expectations, perceptions and experiences about comprehensive regenerative care and determine the ...
It is unknown how patient preferences and values impact the comparative effectiveness of second-line medications for Type 2 diabetes (T2D). The purpose of this study is to elicit patient preferences toward various treatment outcomes (e.g., hospitalization, kidney disease) using a participatory ranking exercise, use these rankings to generate individually weighted composite outcomes, and estimate patient-centered treatment effects of four different second-line T2D medications that reflect the patient's value for each outcome.
The purpose of this mixed-methods study is to deploy the tenets of Health and Wellness Coaching (HWC) through a program called BeWell360 model , tailored to the needs of Healthcare Workers (HCWs) as patients living with poorly-controlled Type 2 Diabetes (T2D). The objective of this study is to pilot-test this novel, scalable, and sustainable BeWell360 model that is embedded and integrated as part of primary care for Mayo Clinic Employees within Mayo Clinic Florida who are identified as patients li)ving with poorly-controlled T2D.
To determine if the EndoBarrier safely and effectively improves glycemic control in obese subjects with type 2 diabetes.
Can QBSAfe be implemented in a clinical practice setting and improve quality of life, reduce treatment burden and hypoglycemia among older, complex patients with type 2 diabetes?
Questionnaire administered to diabetic patients in primary care practice (La Crosse Mayo Family Medicine Residency /Family Health Clinic) to assess patient’s diabetic knowledge. Retrospective chart review will also be done to assess objective diabetic control based on most recent hemoglobin A1c.
The purpose of this study is to assess key characteristics of bone quality, specifically material strength and porosity, in patients who have type 2 diabetes. These patients are at an unexplained increased risk for fractures and there is an urgent need to refine clinical assessment for this risk.
Muscle insulin resistance is a hallmark of upper body obesity (UBO) and Type 2 diabetes (T2DM). It is unknown whether muscle free fatty acid (FFA) availability or intramyocellular fatty acid trafficking is responsible for muscle insulin resistance, although it has been shown that raising FFA with Intralipid can cause muscle insulin resistance within 4 hours. We do not understand to what extent the incorporation of FFA into ceramides or diacylglycerols (DG) affect insulin signaling and muscle glucose uptake. We propose to alter the profile and concentrations of FFA of healthy, non-obese adults using an overnight, intra-duodenal palm oil infusion vs. ...
The objectives of this study are to identify circulating extracellular vesicle (EV)-derived protein and RNA signatures associated with Type 2 Diabetes (T2D), and to identify changes in circulating EV cargo in patients whose T2D resolves after sleeve gastrectomy (SG) or Roux-en-Y gastric bypass (RYGB).
This research study is being done to develop educational materials that will help patients and clinicians talk about diabetes treatment and management options.
Assessment of glucose metabolism and liver fat after 12 week dietary intervention in pre diabetes subjects. Subjects will be randomized to either high fat (olive oil supplemented),high carb/high fiber (beans supplemented) and high carb/low fiber diets. Glucose metabolism will be assessed by labeled oral glucose tolerance test and liver fat by magnetic resonance spectroscopy pre randomization and at 8 and 12 week after starting dietary intervention.
To study the effect of an ileocolonic formulation of ox bile extract on insulin sensitivity, postprandial glycemia and incretin levels, gastric emptying, body weight and fasting serum FGF-19 (fibroblast growth factor) levels in overweight or obese type 2 diabetic subjects on therapy with DPP4 (dipeptidyl peptidase-4) inhibitors (e.g. sitagliptin) alone or in combination with metformin.
The purpose of this study is to evaluate whether or not a 6 month supply (1 meal//day) of healthy food choices readily available in the patient's home and self management training including understanding of how foods impact diabetes, improved food choices and how to prepare those foods, improve glucose control. In addition, it will evaluate whether or not there will be lasting behavior change modification after the program.
The purpose of this study is to compare the rate of progression from prediabetes at 4 months to frank diabetes at 12 months (as defined by increase in HbA1C or fasting BS to diabetic range based on the ADA criteria) after transplantation in kidney transplant recipients on Exenatide SR + SOC vs. standard-of-care alone.
The purpose of this study evaluates a subset of people with isolated Impaired Fasting Glucose with Normal Glucose Tolerance (i.e., IFG/NGT) believed to have normal β-cell function in response to a glucose challenge, suggesting that – at least in this subset of prediabetes – fasting glucose is regulated independently of glucose in the postprandial period. To some extent this is borne out by genetic association studies which have identified loci that affect fasting glucose but not glucose tolerance and vice-versa.
The purpose of this study is to learn more about how the body stores dietary fat. Medical research has shown that fat stored in different parts of the body can affect the risk for diabetes, heart disease and other major health conditions.
The purpose of this study is to see why the ability of fat cells to respond to insulin is different depending on body shape and how fat tissue inflammation is involved.
The purpose of this study is to determine the mechanism(s) by which common bariatric surgical procedures alter carbohydrate metabolism. Understanding these mechanisms may ultimately lead to the development of new interventions for the prevention and treatment of type 2 diabetes and obesity.
The purpose of this study is to evaluate the effects of improving glycemic control, and/or reducing glycemic variability on gastric emptying, intestinal barrier function, autonomic nerve functions, and epigenetic changes in subjects with type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) who are switched to intensive insulin therapy as part of clinical practice.
This study is designed to compare an intensive lifestyle and activity coaching program ("Sessions") to usual care for diabetic patients who are sedentary. The question to be answered is whether the Sessions program improves clinical or patient centric outcomes. Recruitment is through invitiation only.
A research study to enhance clinical discussion between patients and pharmacists using a shared decision making tool for type 2 diabetes or usual care.
While the potential clinical uses of pulsed electromagnetic field therapy (PEMF) are extensive, we are focusing on the potential benefits of PEMF on vascular health. We are targeting, the pre diabetic - metabolic syndrome population, a group with high prevalence in the American population. This population tends to be overweight, low fitness, high blood pressure, high triglycerides and borderline high blood glucose.
This is a study to evaluate a new Point of Care test for blood glucose monitoring.
This protocol is being conducted to determine the mechanisms responsible for insulin resistance, obesity and type 2 diabetes.
The purpose of this study is to assess the effects of a nighttime rise in cortisol on the body's glucose production in type 2 diabetes.
The goal of this study is to evaluate a new format for delivery of a culturally tailored digital storytelling intervention by incorporating a facilitated group discussion following the videos, for management of type II diabetes in Latino communities.
The purpose of this study is to determine the metabolic effects of Colesevelam, particularly for the ability to lower blood sugar after a meal in type 2 diabetics, in order to develop a better understanding of it's potential role in the treatment of obesity.
The purpose of this study is to test whether markers of cellular aging and the SASP are elevated in subjects with obesity and further increased in patients with obesity and Type 2 Diabetes Mellitus (T2DM) and to relate markers of cellular aging (senescence) and the SASP to skeletal parameters (DXA, HRpQCT, bone turnover markers) in each of these groups.
Integration of Diabetes Prevention Program (DPP) and Diabetes Self Management Program (DSMP) into WellConnect.
Using stem cell derived intestinal epithelial cultures (enteroids) derived from obese (BMI> 30) patients and non-obese and metabolically normal patients (either post-bariatric surgery (BS) or BS-naïve with BMI < 25), dietary glucose absorption was measured. We identified that enteroids from obese patients were characterized by glucose hyper-absorption (~ 5 fold) compared to non-obese patients. Significant upregulation of major intestinal sugar transporters, including SGLT1, GLU2 and GLUT5 was responsible for hyper-absorptive phenotype and their pharmacologic inhibition significantly decreased glucose absorption. Importantly, we observed that enteroids from post-BS non-obese patients exhibited low dietary glucose absorption, indicating that altered glucose absorption ...
Muscle insulin resistance is a hallmark of upper body obesity (UBO) and Type 2 diabetes (T2DM). It is unknown whether muscle free fatty acid (FFA) availability or intramyocellular fatty acid trafficking is responsible for the abnormal response to insulin. Likewise, we do not understand to what extent the incorporation of FFA into ceramides or diacylglycerols (DG) affect insulin signaling and muscle glucose uptake. We will measure muscle FFA storage into intramyocellular triglyceride, intramyocellular fatty acid trafficking, activation of the insulin signaling pathway and glucose disposal rates under both saline control (high overnight FFA) and after an overnight infusion of intravenous ...
The purpose of this study is to improve our understanding of why gastrointestinal symptoms occur in diabetes mellitus patients and identify new treatment(s) in the future.
These symptoms are often distressing and may impair glycemic control. We do not understand how diabetes mellitus affects the GI tracy. In 45 patients undergoing sleeve gastrectomy, we plan to compare the cellular composition of circulating peripheral mononuclear cells, stomach immune cells, and interstitial cells of Cajal in the stomach.
Muscle insulin resistance is a hallmark of upper body obesity (UBO) and Type 2 diabetes (T2DM), whereas lower body obesity (LBO) is characterized by near-normal insulin sensitivity. It is unknown whether muscle free fatty acid (FFA) availability or intramyocellular fatty acid trafficking differs between different obesity phenotypes. Likewise, we do not understand to what extent the incorporation of FFA into ceramides or diacylglycerols (DG) affect insulin signaling and muscle glucose uptake. By measuring muscle FFA storage into intramyocellular triglyceride, intramyocellular fatty acid trafficking, activation of the insulin signaling pathway and glucose disposal rates we will provide the first integrated examination ...
The goal of this study is to evaluate the presence of podocytes (special cells in the kidney that prevent protein loss) in the urine in patients with diabetes or glomerulonephritis (inflammation in the kidneys). Loss of podocyte in the urine may be an earlier sign of kidney injury (before protein loss) and the goal of this study is to evaluate the association between protein in the urine and podocytes in the urine.
The purpose of this study is to evaluate the effects of multiple dose regimens of RM-131 on vomiting episodes, stomach emptying and stomach paralysis symptoms in patients with Type 1 and Type 2 diabetes and gastroparesis.
The purpose of this study is assess the feasibility, effectiveness, and acceptability of Diabetes-REM (Rescue, Engagement, and Management), a comprehensive community paramedic (CP) program to improve diabetes self-management among adults in Southeast Minnesota (SEMN) treated for servere hypoglycemia by the Mayo Clinic Ambulance Services (MCAS).
The purpose of this study is to determine if a blood test called "pancreatic polypeptide" can help distinguish between patients with diabetes mellitus with and without pancreatic cancer.
The purpose of this study is to create a prospective cohort of subjects with increased probability of being diagnosed with pancreatic cancer and then screen this cohort for pancreatic cancer
The purpose of this study is to evaluate the effectiveness and safety of brolucizumab vs. aflibercept in the treatment of patients with visual impairment due to diabetic macular edema (DME).
Women with gestational diabetes mellitus (GDM) are likely to have insulin resistance that persists long after pregnancy, resulting in greater risk of developing type 2 diabetes mellitus (T2DM). The study will compare women with and without a previous diagnosis of GDM to determine if women with a history of GDM have abnormal fatty acid metabolism, specifically impaired adipose tissue lipolysis. The study will aim to determine whether women with a history of GDM have impaired pancreatic β-cell function. The study will determine whether women with a history of GDM have tissue specific defects in insulin action, and also identify the effect of a ...
Although vitreous hemorrhage (VH) from proliferative diabetic retinopathy (PDR) can cause acute and dramatic vision loss for patients with diabetes, there is no current, evidence-based clinical guidance as to what treatment method is most likely to provide the best visual outcomes once intervention is desired. Intravitreous anti-vascular endothelial growth factor (anti-VEGF) therapy alone or vitrectomy combined with intraoperative PRP each provide the opportunity to stabilize or regress retinal neovascularization. However, clinical trials are lacking to elucidate the relative time frame of visual recovery or final visual outcome in prompt vitrectomy compared with initial anti-VEGF treatment. The Diabetic Retinopathy Clinical Research ...
The purpose of this study is to demonstrate feasibility of dynamic 11C-ER176 PET imaging to identify macrophage-driven immune dysregulation in gastric muscle of patients with DG. Non-invasive quantitative assessment with PET can significantly add to our diagnostic armamentarium for patients with diabetic gastroenteropathy.
The purpose of this study is to assess the safety and tolerability of intra-arterially delivered mesenchymal stem/stromal cells (MSC) to a single kidney in one of two fixed doses at two time points in patients with progressive diabetic kidney disease.
Diabetic kidney disease, also known as diabetic nephropathy, is the most common cause of chronic kidney disease and end-stage kidney failure requiring dialysis or kidney transplantation. Regenerative, cell-based therapy applying MSCs holds promise to delay the progression of kidney disease in individuals with diabetes mellitus. Our clinical trial will use MSCs processed from each study participant to test the ...
This study aims to measure the percentage of time spent in hyperglycemia in patients on insulin therapy and evaluate diabetes related patient reported outcomes in kidney transplant recipients with type 2 diabetes. It also aimes to evaluate immunosuppression related patient reported outcomes in kidney transplant recipients with type 2 diabetes.
The purpose of this study is to look at how participants' daily life is affected by their heart failure. The study will also look at the change in participants' body weight. This study will compare the effect of semaglutide (a new medicine) compared to "dummy" medicine on body weight and heart failure symptoms. Participants will either get semaglutide or "dummy" medicine, which treatment participants get is decided by chance. Participants will need to take 1 injection once a week.
The purpose of this study is to evaluate whether or not semaglutide can slow down the growth and worsening of chronic kidney disease in people with type 2 diabetes. Participants will receive semaglutide (active medicine) or placebo ('dummy medicine'). This is known as participants' study medicine - which treatment participants get is decided by chance. Semaglutide is a medicine, doctors can prescribe in some countries for the treatment of type 2 diabetes. Participants will get the study medicine in a pen. Participants will use the pen to inject the medicine in a skin fold once a week. The study will close when ...
The objectives of this study are to evaluate the safety of IW-9179 in patients with diabetic gastroparesis (DGP) and the effect of treatment on the cardinal symptoms of DGP.
The purpose of this study is to understand why patients with indigestion, with or without diabetes, have gastrointestinal symptoms and, in particular, to understand where the symptoms are related to increased sensitivity to nutrients.Subsequently, look at the effects of Ondansetron on these patients' symptoms.
The purpose of this study is to evaluate the safety, tolerability, pharmacokinetics, and exploratory effectiveness of nimacimab in patients with diabetic gastroparesis.
The purpose of this study is to prospectively assemble a cohort of subjects >50 and ≤85 years of age with New-onset Diabetes (NOD):
- Estimate the probability of pancreatic ductal adenocarcinoma (PDAC) in the NOD Cohort;
- Establish a biobank of clinically annotated biospecimens including a reference set of biospecimens from pre-symptomatic PDAC and control new-onset type 2 diabetes mellitus (DM) subjects;
- Facilitate validation of emerging tests for identifying NOD subjects at high risk for having PDAC using the reference set; and
- Provide a platform for development of an interventional protocol for early detection of sporadic PDAC ...
The purpose of this study is to demonstrate the performance of the Guardian™ Sensor (3) with an advanced algorithm in subjects age 2 - 80 years, for the span of 170 hours (7 days).
The purpose of this study is to look at the relationship of patient-centered education, the Electronic Medical Record (patient portal) and the use of digital photography to improve the practice of routine foot care and reduce the number of foot ulcers/wounds in patients with diabetes.
Diabetes mellitus is a common condition which is defined by persistently high blood sugar levels. This is a frequent problem that is most commonly due to type 2 diabetes. However, it is now recognized that a small portion of the population with diabetes have an underlying problem with their pancreas, such as chronic pancreatitis or pancreatic cancer, as the cause of their diabetes. Currently, there is no test to identify the small number of patients who have diabetes caused by a primary problem with their pancreas.
The goal of this study is to develop a test to distinguish these ...
The primary purpose of this study is to evaluate the impact of dapagliflozin, as compared with placebo, on heart failure, disease specific biomarkers, symptoms, health status and quality of life in patients with type 2 diabetes or prediabetes and chronic heart failure with preserved systolic function.
The primary purpose of this study is to prospectively assess symptoms of bloating (severity, prevalence) in patients with diabetic gastroparesis.
The purpose of this study is to track the treatment burden experienced by patients living with Type 2 Diabetes Mellitus (T2DM) experience as they work to manage their illness in the context of social distancing measures.
To promote social distancing during the COVID-19 pandemic, health care institutions around the world have rapidly expanded their use of telemedicine to replace in-office appointments where possible.1 For patients with diabetes, who spend considerable time and energy engaging with various components of the health care system,2,3 this unexpected and abrupt transition to virtual health care may signal significant changes to ...
The purpose of this study is to evaluate the safety and efficacy of oral Pyridorin 300 mg BID in reducing the rate of progression of nephropathy due to type 2 diabetes mellitus.
The purpose of this study is to evaluate the effect of Aramchol as compared to placebo on NASH resolution, fibrosis improvement and clinical outcomes related to progression of liver disease (fibrosis stages 2-3 who are overweight or obese and have prediabetes or type 2 diabetes).
The purpose of this study is to evaluate the ability of appropriately-trained family physicians to screen for and identify Diabetic Retinopathy using retinal camera and, secondarily, to describe patients’ perception of the convenience and cost-effectiveness of retinal imaging.
The primary purpose of this study is to evaluate the impact of dapagliflozin, as compared with placebo, on heart failure disease-specific biomarkers, symptoms, health status, and quality of life in patients who have type 2 diabetes and chronic heart failure with reduced systolic function.
Hypothesis: We hypothesize that patients from the Family Medicine Department at Mayo Clinic Florida who participate in RPM will have significantly reduced emergency room visits, hospitalizations, and hospital contacts.
Aims, purpose, or objectives: In this study, we will compare the RPM group to a control group that does not receive RPM. The primary objective is to determine if there are significant group differences in emergency room visits, hospitalizations, outpatient primary care visits, outpatient specialty care visits, and hospital contacts (inbound patient portal messages and phone calls). The secondary objective is to determine if there are ...
The purpose of this research is to determine if CGM (continuous glucose monitors) used in the hospital in patients with COVID-19 and diabetes treated with insulin will be as accurate as POC (point of care) glucose monitors. Also if found to be accurate, CGM reading data will be used together with POC glucometers to dose insulin therapy.
The purpose of this study is to evaluate the effect of fenofibrate compared with placebo for prevention of diabetic retinopathy (DR) worsening or center-involved diabetic macular edema (CI-DME) with vision loss through 4 years of follow-up in participants with mild to moderately severe non-proliferative DR (NPDR) and no CI-DME at baseline.
The purpose of this study is to assess painful diabetic peripheral neuropathy after high-frequency spinal cord stimulation.
The purpose of this study is to examine the evolution of diabetic kindey injury over an extended period in a group of subjects who previously completed a clinical trial which assessed the ability of losartan to protect the kidney from injury in early diabetic kidney disease. We will also explore the relationship between diabetic kidney disease and other diabetes complications, including neuropathy and retinopathy.
The purpose of this study is to evaluate the effietiveness of remdesivir (RDV) in reducing the rate of of all-cause medically attended visits (MAVs; medical visits attended in person by the participant and a health care professional) or death in non-hospitalized participants with early stage coronavirus disease 2019 (COVID-19) and to evaluate the safety of RDV administered in an outpatient setting.
Mayo Clinic Footer
- Request Appointment
- About Mayo Clinic
- About This Site
Legal Conditions and Terms
- Terms and Conditions
- Privacy Policy
- Notice of Privacy Practices
- Notice of Nondiscrimination
- Manage Cookies
Advertising
Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
- Advertising and sponsorship policy
- Advertising and sponsorship opportunities
Reprint Permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.
Patient Centered Studies Focused on Type 2 Diabetes Management, Education, and Family Support: A Scoping Review
Affiliations.
- 1 Department of Pharmacy Administration, School of Pharmacy, University of Mississippi, Oxford, MS 38677-1848, USA.
- 2 School of Pharmacy, University of Mississippi, Oxford, MS 38677-1848, USA.
- PMID: 34789134
- DOI: 10.2174/1573399818666211117113026
Background: Although a large amount of research has been conducted in diabetes management, many of the articles do not focus on patient-centered questions and concerns. To address this shortcoming, patients and various other stakeholders from three northern Mississippi communities co-created research questions focused on Type 2 diabetes management.
Objective: To identify the diabetes management literature pertaining to each of the six patient-developed research questions from March 2010 to July 2020.
Methods: A scoping review was conducted via PubMed to identify research articles from March 2010 to July 2020 focused on patient-centered Type 2 diabetes studies relevant to the six research questions.
Results: A total of 1,414 studies were identified via the search strategy and 34 were included for qualitative analysis following article exclusion. For one of the research questions, there were no articles included. For the remaining research questions, the number of articles identified ranged from two to eleven. After analysis of the included articles, it was found that these questions either lacked extensive data or had not been implemented in the practice of diabetes management.
Conclusion: Additional research is warranted for three of the five questions, as current evidence is either lacking or contradictory. In the remaining two questions, it seems that adequate current research exists to warrant transitioning to implementation focused studies wherein data may be generated to improve sustainability and scaling of current programming.
Keywords: IDF; diabetes self-management; insulin; oral medications; patient-centered studies; type 2 diabetes.
Copyright© Bentham Science Publishers; For any queries, please email at [email protected].
Publication types
- Diabetes Mellitus, Type 2* / therapy
- Patient-Centered Care
- Patient Care & Health Information
- Diseases & Conditions
- Type 2 diabetes
Type 2 diabetes is usually diagnosed using the glycated hemoglobin (A1C) test. This blood test indicates your average blood sugar level for the past two to three months. Results are interpreted as follows:
- Below 5.7% is normal.
- 5.7% to 6.4% is diagnosed as prediabetes.
- 6.5% or higher on two separate tests indicates diabetes.
If the A1C test isn't available, or if you have certain conditions that interfere with an A1C test, your health care provider may use the following tests to diagnose diabetes:
Random blood sugar test. Blood sugar values are expressed in milligrams of sugar per deciliter ( mg/dL ) or millimoles of sugar per liter ( mmol/L ) of blood. Regardless of when you last ate, a level of 200 mg/dL (11.1 mmol/L ) or higher suggests diabetes, especially if you also have symptoms of diabetes, such as frequent urination and extreme thirst.
Fasting blood sugar test. A blood sample is taken after you haven't eaten overnight. Results are interpreted as follows:
- Less than 100 mg/dL (5.6 mmol/L ) is considered healthy.
- 100 to 125 mg/dL (5.6 to 6.9 mmol/L ) is diagnosed as prediabetes.
- 126 mg/dL (7 mmol/L ) or higher on two separate tests is diagnosed as diabetes.
Oral glucose tolerance test. This test is less commonly used than the others, except during pregnancy. You'll need to not eat for a certain amount of time and then drink a sugary liquid at your health care provider's office. Blood sugar levels then are tested periodically for two hours. Results are interpreted as follows:
- Less than 140 mg/dL (7.8 mmol/L ) after two hours is considered healthy.
- 140 to 199 mg/dL (7.8 mmol/L and 11.0 mmol/L ) is diagnosed as prediabetes.
- 200 mg/dL (11.1 mmol/L ) or higher after two hours suggests diabetes.
Screening. The American Diabetes Association recommends routine screening with diagnostic tests for type 2 diabetes in all adults age 35 or older and in the following groups:
- People younger than 35 who are overweight or obese and have one or more risk factors associated with diabetes.
- Women who have had gestational diabetes.
- People who have been diagnosed with prediabetes.
- Children who are overweight or obese and who have a family history of type 2 diabetes or other risk factors.
After a diagnosis
If you're diagnosed with diabetes, your health care provider may do other tests to distinguish between type 1 and type 2 diabetes because the two conditions often require different treatments.
Your health care provider will test A1C levels at least two times a year and when there are any changes in treatment. Target A1C goals vary depending on age and other factors. For most people, the American Diabetes Association recommends an A1C level below 7%.
You also receive tests to screen for complications of diabetes and other medical conditions.
More Information
- Glucose tolerance test
Management of type 2 diabetes includes:
- Healthy eating.
- Regular exercise.
- Weight loss.
- Possibly, diabetes medication or insulin therapy.
- Blood sugar monitoring.
These steps make it more likely that blood sugar will stay in a healthy range. And they may help to delay or prevent complications.
Healthy eating
There's no specific diabetes diet. However, it's important to center your diet around:
- A regular schedule for meals and healthy snacks.
- Smaller portion sizes.
- More high-fiber foods, such as fruits, nonstarchy vegetables and whole grains.
- Fewer refined grains, starchy vegetables and sweets.
- Modest servings of low-fat dairy, low-fat meats and fish.
- Healthy cooking oils, such as olive oil or canola oil.
- Fewer calories.
Your health care provider may recommend seeing a registered dietitian, who can help you:
- Identify healthy food choices.
- Plan well-balanced, nutritional meals.
- Develop new habits and address barriers to changing habits.
- Monitor carbohydrate intake to keep your blood sugar levels more stable.
Physical activity
Exercise is important for losing weight or maintaining a healthy weight. It also helps with managing blood sugar. Talk to your health care provider before starting or changing your exercise program to ensure that activities are safe for you.
- Aerobic exercise. Choose an aerobic exercise that you enjoy, such as walking, swimming, biking or running. Adults should aim for 30 minutes or more of moderate aerobic exercise on most days of the week, or at least 150 minutes a week.
- Resistance exercise. Resistance exercise increases your strength, balance and ability to perform activities of daily living more easily. Resistance training includes weightlifting, yoga and calisthenics. Adults living with type 2 diabetes should aim for 2 to 3 sessions of resistance exercise each week.
- Limit inactivity. Breaking up long periods of inactivity, such as sitting at the computer, can help control blood sugar levels. Take a few minutes to stand, walk around or do some light activity every 30 minutes.
Weight loss
Weight loss results in better control of blood sugar levels, cholesterol, triglycerides and blood pressure. If you're overweight, you may begin to see improvements in these factors after losing as little as 5% of your body weight. However, the more weight you lose, the greater the benefit to your health. In some cases, losing up to 15% of body weight may be recommended.
Your health care provider or dietitian can help you set appropriate weight-loss goals and encourage lifestyle changes to help you achieve them.
Monitoring your blood sugar
Your health care provider will advise you on how often to check your blood sugar level to make sure you remain within your target range. You may, for example, need to check it once a day and before or after exercise. If you take insulin, you may need to check your blood sugar multiple times a day.
Monitoring is usually done with a small, at-home device called a blood glucose meter, which measures the amount of sugar in a drop of blood. Keep a record of your measurements to share with your health care team.
Continuous glucose monitoring is an electronic system that records glucose levels every few minutes from a sensor placed under the skin. Information can be transmitted to a mobile device such as a phone, and the system can send alerts when levels are too high or too low.
Diabetes medications
If you can't maintain your target blood sugar level with diet and exercise, your health care provider may prescribe diabetes medications that help lower glucose levels, or your provider may suggest insulin therapy. Medicines for type 2 diabetes include the following.
Metformin (Fortamet, Glumetza, others) is generally the first medicine prescribed for type 2 diabetes. It works mainly by lowering glucose production in the liver and improving the body's sensitivity to insulin so it uses insulin more effectively.
Some people experience B-12 deficiency and may need to take supplements. Other possible side effects, which may improve over time, include:
- Abdominal pain.
Sulfonylureas help the body secrete more insulin. Examples include glyburide (DiaBeta, Glynase), glipizide (Glucotrol XL) and glimepiride (Amaryl). Possible side effects include:
- Low blood sugar.
- Weight gain.
Glinides stimulate the pancreas to secrete more insulin. They're faster acting than sulfonylureas. But their effect in the body is shorter. Examples include repaglinide and nateglinide. Possible side effects include:
Thiazolidinediones make the body's tissues more sensitive to insulin. An example of this medicine is pioglitazone (Actos). Possible side effects include:
- Risk of congestive heart failure.
- Risk of bladder cancer (pioglitazone).
- Risk of bone fractures.
DPP-4 inhibitors help reduce blood sugar levels but tend to have a very modest effect. Examples include sitagliptin (Januvia), saxagliptin (Onglyza) and linagliptin (Tradjenta). Possible side effects include:
- Risk of pancreatitis.
- Joint pain.
GLP-1 receptor agonists are injectable medications that slow digestion and help lower blood sugar levels. Their use is often associated with weight loss, and some may reduce the risk of heart attack and stroke. Examples include exenatide (Byetta, Bydureon Bcise), liraglutide (Saxenda, Victoza) and semaglutide (Rybelsus, Ozempic, Wegovy). Possible side effects include:
SGLT2 inhibitors affect the blood-filtering functions in the kidneys by blocking the return of glucose to the bloodstream. As a result, glucose is removed in the urine. These medicines may reduce the risk of heart attack and stroke in people with a high risk of those conditions. Examples include canagliflozin (Invokana), dapagliflozin (Farxiga) and empagliflozin (Jardiance). Possible side effects include:
- Vaginal yeast infections.
- Urinary tract infections.
- Low blood pressure.
- High cholesterol.
- Risk of gangrene.
- Risk of bone fractures (canagliflozin).
- Risk of amputation (canagliflozin).
Other medicines your health care provider might prescribe in addition to diabetes medications include blood pressure and cholesterol-lowering medicines, as well as low-dose aspirin, to help prevent heart and blood vessel disease.
Insulin therapy
Some people who have type 2 diabetes need insulin therapy. In the past, insulin therapy was used as a last resort, but today it may be prescribed sooner if blood sugar targets aren't met with lifestyle changes and other medicines.
Different types of insulin vary on how quickly they begin to work and how long they have an effect. Long-acting insulin, for example, is designed to work overnight or throughout the day to keep blood sugar levels stable. Short-acting insulin generally is used at mealtime.
Your health care provider will determine what type of insulin is right for you and when you should take it. Your insulin type, dosage and schedule may change depending on how stable your blood sugar levels are. Most types of insulin are taken by injection.
Side effects of insulin include the risk of low blood sugar — a condition called hypoglycemia — diabetic ketoacidosis and high triglycerides.
Weight-loss surgery
Weight-loss surgery changes the shape and function of the digestive system. This surgery may help you lose weight and manage type 2 diabetes and other conditions related to obesity. There are several surgical procedures. All of them help people lose weight by limiting how much food they can eat. Some procedures also limit the amount of nutrients the body can absorb.
Weight-loss surgery is only one part of an overall treatment plan. Treatment also includes diet and nutritional supplement guidelines, exercise and mental health care.
Generally, weight-loss surgery may be an option for adults living with type 2 diabetes who have a body mass index (BMI) of 35 or higher. BMI is a formula that uses weight and height to estimate body fat. Depending on the severity of diabetes or the presence of other medical conditions, surgery may be an option for someone with a BMI lower than 35.
Weight-loss surgery requires a lifelong commitment to lifestyle changes. Long-term side effects may include nutritional deficiencies and osteoporosis.
People living with type 2 diabetes often need to change their treatment plan during pregnancy and follow a diet that controls carbohydrates. Many people need insulin therapy during pregnancy. They also may need to stop other treatments, such as blood pressure medicines.
There is an increased risk during pregnancy of developing a condition that affects the eyes called diabetic retinopathy. In some cases, this condition may get worse during pregnancy. If you are pregnant, visit an ophthalmologist during each trimester of your pregnancy and one year after you give birth. Or as often as your health care provider suggests.
Signs of trouble
Regularly monitoring your blood sugar levels is important to avoid severe complications. Also, be aware of symptoms that may suggest irregular blood sugar levels and the need for immediate care:
High blood sugar. This condition also is called hyperglycemia. Eating certain foods or too much food, being sick, or not taking medications at the right time can cause high blood sugar. Symptoms include:
- Frequent urination.
- Increased thirst.
- Blurred vision.
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS). This life-threatening condition includes a blood sugar reading higher than 600 mg/dL (33.3 mmol/L ). HHNS may be more likely if you have an infection, are not taking medicines as prescribed, or take certain steroids or drugs that cause frequent urination. Symptoms include:
- Extreme thirst.
- Drowsiness.
- Dark urine.
Diabetic ketoacidosis. Diabetic ketoacidosis occurs when a lack of insulin results in the body breaking down fat for fuel rather than sugar. This results in a buildup of acids called ketones in the bloodstream. Triggers of diabetic ketoacidosis include certain illnesses, pregnancy, trauma and medicines — including the diabetes medicines called SGLT2 inhibitors.
The toxicity of the acids made by diabetic ketoacidosis can be life-threatening. In addition to the symptoms of hyperglycemia, such as frequent urination and increased thirst, ketoacidosis may cause:
- Shortness of breath.
- Fruity-smelling breath.
Low blood sugar. If your blood sugar level drops below your target range, it's known as low blood sugar. This condition also is called hypoglycemia. Your blood sugar level can drop for many reasons, including skipping a meal, unintentionally taking more medication than usual or being more physically active than usual. Symptoms include:
- Irritability.
- Heart palpitations.
- Slurred speech.
If you have symptoms of low blood sugar, drink or eat something that will quickly raise your blood sugar level. Examples include fruit juice, glucose tablets, hard candy or another source of sugar. Retest your blood in 15 minutes. If levels are not at your target, eat or drink another source of sugar. Eat a meal after your blood sugar level returns to normal.
If you lose consciousness, you need to be given an emergency injection of glucagon, a hormone that stimulates the release of sugar into the blood.
- Medications for type 2 diabetes
- GLP-1 agonists: Diabetes drugs and weight loss
- Bariatric surgery
- Endoscopic sleeve gastroplasty
- Gastric bypass (Roux-en-Y)
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Careful management of type 2 diabetes can reduce the risk of serious — even life-threatening — complications. Consider these tips:
- Commit to managing your diabetes. Learn all you can about type 2 diabetes. Make healthy eating and physical activity part of your daily routine.
- Work with your team. Establish a relationship with a certified diabetes education specialist, and ask your diabetes treatment team for help when you need it.
- Identify yourself. Wear a necklace or bracelet that says you are living with diabetes, especially if you take insulin or other blood sugar-lowering medicine.
- Schedule a yearly physical exam and regular eye exams. Your diabetes checkups aren't meant to replace regular physicals or routine eye exams.
- Keep your vaccinations up to date. High blood sugar can weaken your immune system. Get a flu shot every year. Your health care provider also may recommend the pneumonia vaccine. The Centers for Disease Control and Prevention (CDC) also recommends the hepatitis B vaccination if you haven't previously received this vaccine and you're 19 to 59 years old. Talk to your health care provider about other vaccinations you may need.
- Take care of your teeth. Diabetes may leave you prone to more-serious gum infections. Brush and floss your teeth regularly and schedule recommended dental exams. Contact your dentist right away if your gums bleed or look red or swollen.
- Pay attention to your feet. Wash your feet daily in lukewarm water, dry them gently, especially between the toes, and moisturize them with lotion. Check your feet every day for blisters, cuts, sores, redness and swelling. Contact your health care provider if you have a sore or other foot problem that isn't healing.
- Keep your blood pressure and cholesterol under control. Eating healthy foods and exercising regularly can go a long way toward controlling high blood pressure and cholesterol. Take medication as prescribed.
- If you smoke or use other types of tobacco, ask your health care provider to help you quit. Smoking increases your risk of diabetes complications. Talk to your health care provider about ways to stop using tobacco.
- Use alcohol sparingly. Depending on the type of drink, alcohol may lower or raise blood sugar levels. If you choose to drink alcohol, only do so with a meal. The recommendation is no more than one drink daily for women and no more than two drinks daily for men. Check your blood sugar frequently after drinking alcohol.
- Make healthy sleep a priority. Many people with type 2 diabetes have sleep problems. And not getting enough sleep may make it harder to keep blood sugar levels in a healthy range. If you have trouble sleeping, talk to your health care provider about treatment options.
- Caffeine: Does it affect blood sugar?
Alternative medicine
Many alternative medicine treatments claim to help people living with diabetes. According to the National Center for Complementary and Integrative Health, studies haven't provided enough evidence to recommend any alternative therapies for blood sugar management. Research has shown the following results about popular supplements for type 2 diabetes:
- Chromium supplements have been shown to have few or no benefits. Large doses can result in kidney damage, muscle problems and skin reactions.
- Magnesium supplements have shown benefits for blood sugar control in some but not all studies. Side effects include diarrhea and cramping. Very large doses — more than 5,000 mg a day — can be fatal.
- Cinnamon, in some studies, has lowered fasting glucose levels but not A1C levels. Therefore, there's no evidence of overall improved glucose management.
Talk to your health care provider before starting a dietary supplement or natural remedy. Do not replace your prescribed diabetes medicines with alternative medicines.
Coping and support
Type 2 diabetes is a serious disease, and following your diabetes treatment plan takes commitment. To effectively manage diabetes, you may need a good support network.
Anxiety and depression are common in people living with diabetes. Talking to a counselor or therapist may help you cope with the lifestyle changes and stress that come with a type 2 diabetes diagnosis.
Support groups can be good sources of diabetes education, emotional support and helpful information, such as how to find local resources or where to find carbohydrate counts for a favorite restaurant. If you're interested, your health care provider may be able to recommend a group in your area.
You can visit the American Diabetes Association website to check out local activities and support groups for people living with type 2 diabetes. The American Diabetes Association also offers online information and online forums where you can chat with others who are living with diabetes. You also can call the organization at 800-DIABETES ( 800-342-2383 ).
Preparing for your appointment
At your annual wellness visit, your health care provider can screen for diabetes and monitor and treat conditions that increase your risk of diabetes, such as high blood pressure, high cholesterol or a high BMI .
If you are seeing your health care provider because of symptoms that may be related to diabetes, you can prepare for your appointment by being ready to answer the following questions:
- When did your symptoms begin?
- Does anything improve the symptoms or worsen the symptoms?
- What medicines do you take regularly, including dietary supplements and herbal remedies?
- What are your typical daily meals? Do you eat between meals or before bedtime?
- How much alcohol do you drink?
- How much daily exercise do you get?
- Is there a history of diabetes in your family?
If you are diagnosed with diabetes, your health care provider may begin a treatment plan. Or you may be referred to a doctor who specializes in hormonal disorders, called an endocrinologist. Your care team also may include the following specialists:
- Certified diabetes education specialist.
- Foot doctor, also called a podiatrist.
- Doctor who specializes in eye care, called an ophthalmologist.
Talk to your health care provider about referrals to other specialists who may be providing care.
Questions for ongoing appointments
Before any appointment with a member of your treatment team, make sure you know whether there are any restrictions, such as not eating or drinking before taking a test. Questions that you should regularly talk about with your health care provider or other members of the team include:
- How often do I need to monitor my blood sugar, and what is my target range?
- What changes in my diet would help me better manage my blood sugar?
- What is the right dosage for prescribed medications?
- When do I take the medications? Do I take them with food?
- How does management of diabetes affect treatment for other conditions? How can I better coordinate treatments or care?
- When do I need to make a follow-up appointment?
- Under what conditions should I call you or seek emergency care?
- Are there brochures or online sources you recommend?
- Are there resources available if I'm having trouble paying for diabetes supplies?
What to expect from your doctor
Your health care provider is likely to ask you questions at your appointments. Those questions may include:
- Do you understand your treatment plan and feel confident you can follow it?
- How are you coping with diabetes?
- Have you had any low blood sugar?
- Do you know what to do if your blood sugar is too low or too high?
- What's a typical day's diet like?
- Are you exercising? If so, what type of exercise? How often?
- Do you sit for long periods of time?
- What challenges are you experiencing in managing your diabetes?
- Professional Practice Committee: Standards of Medical Care in Diabetes — 2020. Diabetes Care. 2020; doi:10.2337/dc20-Sppc.
- Diabetes mellitus. Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/diabetes-mellitus-dm. Accessed Dec. 7, 2020.
- Melmed S, et al. Williams Textbook of Endocrinology. 14th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Dec. 3, 2020.
- Diabetes overview. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diabetes/overview/all-content. Accessed Dec. 4, 2020.
- AskMayoExpert. Type 2 diabetes. Mayo Clinic; 2018.
- Feldman M, et al., eds. Surgical and endoscopic treatment of obesity. In: Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 11th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed Oct. 20, 2020.
- Hypersmolar hyperglycemic state (HHS). Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/hyperosmolar-hyperglycemic-state-hhs. Accessed Dec. 11, 2020.
- Diabetic ketoacidosis (DKA). Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/diabetic-ketoacidosis-dka. Accessed Dec. 11, 2020.
- Hypoglycemia. Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/hypoglycemia. Accessed Dec. 11, 2020.
- 6 things to know about diabetes and dietary supplements. National Center for Complementary and Integrative Health. https://www.nccih.nih.gov/health/tips/things-to-know-about-type-diabetes-and-dietary-supplements. Accessed Dec. 11, 2020.
- Type 2 diabetes and dietary supplements: What the science says. National Center for Complementary and Integrative Health. https://www.nccih.nih.gov/health/providers/digest/type-2-diabetes-and-dietary-supplements-science. Accessed Dec. 11, 2020.
- Preventing diabetes problems. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/all-content. Accessed Dec. 3, 2020.
- Schillie S, et al. Prevention of hepatitis B virus infection in the United States: Recommendations of the Advisory Committee on Immunization Practices. MMWR Recommendations and Reports. 2018; doi:10.15585/mmwr.rr6701a1.
- Diabetes prevention: 5 tips for taking control
- Hyperinsulinemia: Is it diabetes?
Associated Procedures
News from mayo clinic.
- Mayo study uses electronic health record data to assess metformin failure risk, optimize care Feb. 10, 2023, 02:30 p.m. CDT
- Mayo Clinic Minute: Strategies to break the heart disease and diabetes link Nov. 28, 2022, 05:15 p.m. CDT
- Mayo Clinic Q and A: Diabetes risk in Hispanic people Oct. 20, 2022, 12:15 p.m. CDT
- The importance of diagnosing, treating diabetes in the Hispanic population in the US Sept. 28, 2022, 04:00 p.m. CDT
- Mayo Clinic Minute: Managing Type 2 diabetes Sept. 28, 2022, 02:30 p.m. CDT
Products & Services
- A Book: The Essential Diabetes Book
- A Book: The Mayo Clinic Diabetes Diet
- Assortment of Health Products from Mayo Clinic Store
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Open access
- Published: 30 April 2022
A qualitative study exploring the barriers to attending structured education programmes among adults with type 2 diabetes
- Imogen Coningsby 1 , 2 ,
- Ben Ainsworth 1 &
- Charlotte Dack 1
BMC Health Services Research volume 22 , Article number: 584 ( 2022 ) Cite this article
5283 Accesses
5 Citations
1 Altmetric
Metrics details
Diabetes self-management education, a universally recommended component of diabetes care, aims to support self-management in people with type 2 diabetes. However, attendance is low (approx. 10%). Previous research investigating the reasons for low attendance have not yet linked findings to theory, making it difficult to translate findings into practice. This study explores why some adults with type 2 diabetes do not attend diabetes self-management education and considers how services can be adapted accordingly, using Andersen’s Behavioural Model of Health Service Utilisation as a framework.
A cross-sectional semi-structured qualitative interview study was carried out. Semi-structured interviews were conducted by telephone with 14 adults with type 2 diabetes who had verbally declined their invitation to attend diabetes self-management education in Bath and North East Somerset, UK, within the last 2 years. Data were analysed using inductive thematic analysis before mapping the themes onto the factors of Andersen’s Behavioural Model.
Two main themes were identified: ‘perceived need’ and ‘practical barriers’ . The former theme explored participants’ tendency to decline diabetes education when they perceived they did not need the programme. This perception tended to arise from participants’ high self-efficacy to manage their type 2 diabetes, the low priority they attributed to their condition and limited knowledge about the programme. The latter theme, ‘ practical barriers’ , explored the notion that some participants wanted to attend but were unable to due to other commitments and/or transportation issues in getting to the venue.
Conclusions
All sub-themes resonated with one or more factors of Andersen’s Behavioural Model indicating that the model may help to elucidate attendance barriers and ways to improve services. To fully understand low attendance to diabetes education, the complex and individualised reasons for non-attendance must be recognised and a person-centred approach should be taken to understand people’s experience, needs and capabilities.
Peer Review reports
Introduction
Type 2 diabetes has the fastest rising prevalence of any long-term condition [ 1 ]. Self-management, defined as a set of skilled behaviours one engages in to manage an illness [ 2 ], plays a central role in keeping blood glucose within a safe threshold in people with type 2 diabetes [ 3 ]. The knowledge and skills needed to self-manage one’s type 2 diabetes are diverse and include numerous daily activities, such as carbohydrate counting, exercise and self-monitoring of blood glucose levels [ 4 ]. When blood glucose levels rise above the normal threshold, this can lead to serious complications such as blindness, renal failure and amputation [ 5 ].
In the UK, diabetes self-management education (DSME) is a recommended component of diabetes care which aims to improve individuals’ knowledge, skills and confidence enabling them to self-manage their type 2 diabetes and improve self-care and clinical outcomes including glycaemic control (level of glucose in the blood) [ 6 ]. DSME has an evidence-based and theory-driven curriculum that is delivered in groups by trained educators [ 6 ]. In the UK, examples of DSME include X-PERT diabetes [ 7 ], a 6-week programme in sessions of 2.5 hours and DESMOND [ 8 ], a 1 or 2 day programme lasting 6 hours in total.
There is strong evidence that DSME confers significant benefits on self-management behaviours as well as clinical, lifestyle and psychosocial outcomes in adults with type 2 diabetes. For example, a randomised controlled trial [ 9 ] found that participation in the DSME programme, X-PERT, led to improvements in a range of outcomes at 14 month follow-up such as glycaemic control, body mass index, waist circumference, cholesterol, diabetes knowledge and psychosocial adjustment. These findings have also been replicated in a national audit of X-PERT diabetes programmes [ 10 ]. Systematic reviews with meta-analysis have also conferred similar positive effects [ 11 , 12 ]. For example, a systematic review [ 13 ] of DSME for people with type 2 diabetes found that, at 1-year follow-up, patient satisfaction and body weight had significantly improved and, at 2-year follow-up, there were significant improvements in blood glucose levels and diabetes knowledge. These findings indicate that DSME is a well-supported intervention to improve clinical, lifestyle and psychosocial outcomes in adults with type 2 diabetes.
However, attendance to DSME is low [ 10 , 14 ]. Approximately 90% of those invited to DSME do not attend [ 10 ]. Low DSME attendance is a major concern given that DSME can have positive effects on health outcomes [ 12 , 13 ]. Moreover, individuals who do not attend or do not complete DSME are more likely to have reduced adherence to self-management activities and glycaemic control and are at a fourfold increased risk of having complications than those who attend and complete DSME [ 15 , 16 ]. It is therefore paramount that the reasons for non-attendance are well-understood among health professionals, commissioners and policy makers. This will help identify ways attendance can be optimised, as well as establish the effectiveness of DSME whilst taking into consideration who does and doesn’t engage with DSME and why. A more nuanced understanding of the barriers to DSME may also help elucidate whether for some people alternative support (e.g. social/emotional/psychological support) would be more appropriate and beneficial.
Recent research has highlighted various psychosocial, cultural and practical barriers to attendance [ 14 , 17 ]. For example, a recent systematic review [ 14 ] found reasons for non-attendance included logistical, medical, financial, emotional and cultural barriers, as well as a lack of perceived benefit and feeling that oneself has sufficient knowledge of their condition. Similarly, a recent qualitative report [ 17 ] reported additional barriers including a lack of knowledge of the existence and benefits of DSME among people with type 2 diabetes and their healthcare providers, and poor integration within existing healthcare.
However, the lack of application of previous findings to theory makes it difficult to interpret and translate findings into practice as there lacks a framework for identifying key areas for improvement [ 18 ]. Andersen’s Behavioural Model of Health Service Utilisation [ 19 , 20 ] (ABM) may be useful to explain and predict non-attendance because it acknowledges both individual and contextual characteristics that may facilitate or impede health service utilisation. The ABM proposes that an individual’s use of health services depends on three characteristics: predisposing factors (sociocultural and psychological characteristics of individuals that exist prior to their illness such as sex, age, culture, values and attitudes towards health and health services), enabling factors (practical aspects of obtaining care such as the means and know how to access health services, income, travel, extent and quality of social relationships, knowledge about services, as well as available health personnel and waiting times) and need factors (conditions perceived by the patient or evaluated by health professionals as requiring the use of health services) [ 19 ]. ABM has been used to explain and predict the use of a range of health services required for tertiary disease management (e.g. cardiac rehabilitation [ 21 ] and HIV medication adherence [ 22 ]). Therefore, ABM is an appropriate model to help elucidate barriers to DSME attendance and identify priority areas to increase uptake.
This study explored reasons for non-attendance to DSME among adults with type 2 diabetes in Bath and North East Somerset, UK, as well as assess the utility of ABM as a framework for elucidating barriers to DSME attendance and highlighting key areas to improve local services.
A semi-structured qualitative interview study was conducted. Due to the Coronavirus (COVID-19) pandemic present during data collection, all interviews were conducted via telephone. The study was conducted in accordance with the British Psychological Society recommendations for research. Ethical approval was received from the University of Bath Psychology Ethics Committee (reference number: 20–133). The COnsolidated criteria for REporting Qualitative research (COREQ) [ 23 ] was used to guide reporting ( appendix A ).
Participants
Convenience sampling was used to ensure participants met the following eligibility criteria:
Over 18 years old
Live in Bath and North East Somerset, UK
Diagnosed with type 2 diabetes
Verbally declined their invite to attend the DSME programme, X-PERT, within the last 2 years
Eligible individuals were phoned by the researcher and asked if they would be interested in participating. Out of the 55 individuals eligible to participate, 20 were willing to take part. 28 declined due to disinterest, lack of time, denial of their type 2 diabetes and beliefs that their type 2 diabetes was not important. Seven individuals could not be contacted. Prospective participants were sent an information sheet and consent form via email. Two participants did not respond, and four participants declined due to lack of time. In total, 14 participants gave written and verbal informed consent and were interviewed (Fig. 1 ).
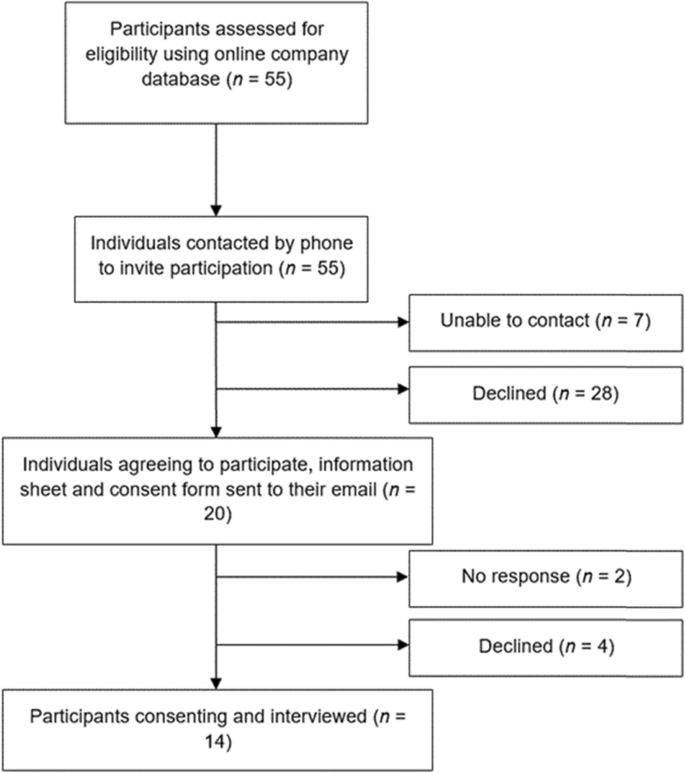
Recruitment strategy
Of the 14 participants, five were women and nine were men. Participants were aged between 27 and 80 years ( M = 57, SD = 15.5). The length of time since diagnosis varied between 3 months and 40 years ( M = 4.6 years). According to participants’ BMI, three participants were classified as overweight, nine were obese and one was extremely obese (see Table 1 for participants’ demographics).
Interviews were conducted by telephone in June 2020 by author IC, a female Health Psychology Masters student who had received formal training in qualitative research. The interviewer had no previous relationship with participants and started each interview by thanking the participant for their time and providing an overview of the research and its aims. Participants were given the opportunity to ask questions before being asked to give verbal informed consent. After obtaining informed consent the interview commenced with only the interviewer and participant present. All individuals who participated in this study gave informed consent prior to participation.
A semi-structured interview schedule (developed by author IC) was used to flexibly guide the interviews. It was piloted and adapted during the first three interviews to ensure questions were clear and not misinterpreted. The question “what would your ideal diabetes programme look like?” was discarded as participants reported being unable to answer due to their limited understanding of DSME. The final interview schedule had two main topics reflecting the aims of this study: 1) Barriers to attending DSME; and 2) Programme improvements ( appendix B ). Interviews lasted, on average, 31 minutes (shortest = 15; longest = 52), and were audio-recorded.
After the interview, participants were thanked for their time, verbally debriefed and given the opportunity to ask any further questions before being emailed a debrief sheet. The interview was then transcribed verbatim, anonymized and imported into the software package QSR NVivo to record field notes and facilitate data analysis. Transcripts were not returned to participants for comment or correction.
Analytic approach
Data were analysed using reflexive thematic analysis to enable the identification of patterns/themes related to barriers to DSME attendance [ 24 ]. An inductive approach was used whereby interviews were exploratory and analysis was driven by participants’ accounts [ 25 ]. In the final interviews, no new major insights emerged from the data. Therefore, it was believed data saturation had been reached [ 26 ].
To improve rigour, Braun and Clarke’s six phases of thematic analysis [ 25 ] were used to generate themes from the data. In accordance with their recommendations, analysis was iterative, moving bi-directionally through the phases to provide a thorough analysis of the data. Analysis began with data familiarisation whereby author IC listened to the audio files and read the transcripts several times. IC then generated codes inductively in NVivo before collating the codes into provisional themes by considering their different relationships, similarities and differences. Authors BA and IC reviewed provisional themes by checking each code and its associated data fit with the theme before defining and naming the themes. Sub-themes were created where themes were large or incorporated nuances in meaning within the data. Participants were not asked for feedback on the findings.
After the final themes had been agreed, sub-themes were mapped onto the factors of ABM (Table 2 ). This required the researchers to re-read data within the sub-themes and assign the sub-themes to appropriate factors. Occasionally, data coded under one sub-theme could be assigned to more than one factor. All sub-themes could be applied to at least one factor. This approach ensured the analysis was data driven and meant that the robustness of ABM in explaining the data could be tested against the themes during this mapping process.
Two themes, in relation to barriers to attendance, were identified; ‘ perceived need’ and ‘practical barriers’. Each theme had several sub-themes (Table 2 ). Illustrative quotes are referenced using pseudonyms (Table 1 ).
Theme 1: perceived need
A key reason for not attending DSME was individuals’ perception they did not need to attend DSME: “I don’t really need this” (John). This was evident among those who had high self-efficacy to manage their type 2 diabetes (sub-theme 1), attributed a low priority to their type 2 diabetes (sub-theme 2) and/or had limited knowledge about DSME (sub-theme 3).
Self-efficacy to manage diabetes
Two frequently reported reasons for declining DSME were already being well informed and having acquired sufficient knowledge about diabetes and how to manage it. This negated the need to attend DSME.
“I wasn’t sure that it would contribute anything. I know all about controlling diet and controlling blood sugars. I mean I’ve seen it in spades, and did I want to hear it all again? Well no not really.” (Edward)
There was a sense of animosity and monotony towards attending as individuals did not want to listen to information they had already heard and knew.
“I wasn’t going to sit with ten other people just sitting listening to someone preaching to me what I should and shouldn't do when I already know what I should and shouldn't do.” (Alex)
For some, there was a sense of pleasure by declining the course because it provided a space to others who “ needed it more ” (Alex). They perceived themselves as highly knowledgeable of their condition and as differing from others who may be less knowledgeable and therefore more in need of support. They explained non-attendance as an altruistic act of freeing up space for another individual.
“I did already know it all! So to me it just seemed like a waste of everybody's time and a valuable space for somebody who really needed it.” (Julie)
Participants reported engaging in a variety of activities to manage their type 2 diabetes such as dieting, exercising and testing their blood glucose. Improvements in biomedical indices, such as blood pressure, cholesterol and glycaemic level, led to a sense of personal achievement and gave individuals credible and objective evidence that their type 2 diabetes was under control, and thus, did not warrant the need for them to seek additional help.
“I felt like I was making apparently decent progress. Not only the sugar levels had dropped, but I improved my cholesterol and blood pressure, so I felt like I was controlling things reasonably well” (Mark)
In addition to biomedical indices, perceived disease severity was also influenced by physicians’ assessment of one’s type 2 diabetes. Several participants described being reassured by their GP or nurse that their type 2 diabetes was not harmful at the current time. This positive assessment and framing of their condition as ‘borderline’ (Mark) or ‘ marginal’ (Andrew), as stated by some participants, led people with type 2 diabetes to believe, and perhaps correctly so, that they did not need to take further action.
“They [the nurses] don’t seem to be too worried about me and my condition. They can’t see any danger signals like “you got to do something really serious about this now because your body is telling us that things don’t look too good”. So really I haven’t been worried enough to think oh I ought to do something.” (John)
One reason for not attending DSME arose from the pre-existing receipt of adequate support and care from their physician. Participants did not feel the need to seek out additional education as they were already satisfied with the care they were receiving.
“I just thought well I’m quite happy with the way I’m being looked after thank you very much and that’s the reason I didn’t want to get too involved.” (Harry)
In many instances, individuals used regular healthcare appointments with their physician to monitor their condition and inform them if further action is required. This suggests some individuals do not see self-management as only their responsibility, but a set of skills to be built collaboratively with a health care professional.
“ I will go and see the nurse every so often who does the annual “you’ve got worse or better”. I'm kind of in the rota now for every so often going along and being listened to and talked to as well about things that I might need to do or things that perhaps might be getting worse.” (Julie)
Low prioritisation of diabetes
Another barrier to attending DSME was that their type 2 diabetes took a low priority with some participants saying it was “just another thing” and “ not very important ” (Derek). This was particularly common among those who had one or more comorbidities. Individuals with comorbidities considered their comorbidity as more important or requiring more attention than their type 2 diabetes.
“I’ve got other health issues that are more demanding at the moment to me and affect me rather than type 2 diabetes which is just something else and I don’t really need it.” (John)
The low priority some participants attributed to their type 2 diabetes may reflect attempts to avoid or deny their condition by minimising its importance. Indeed, one participant stated going through a “period of denial” (Lisa) in the early stages of her diagnosis. Avoidance and denial are coping strategies that protect an individual from the stress of an external experience, in this case, being diagnosed and living with type 2 diabetes [ 27 ]. Attending DSME might challenge this coping strategy if they perceive they will be exposed to the reality of their own stress.
For some individuals, the low prioritisation of their type 2 diabetes arose from their fatalistic attitudes towards their condition. Fatalistic attitudes (beliefs something is predetermined and one is powerless to change [ 28 ]) were most common in older participants. For example, Derek (age 79) stated “ my sell by date has gone for that [DSME]. I feel like it’s too late ”, illustrating that some older individuals believe that lifestyle changes made as a result of attending DSME would have limited benefit on their type 2 diabetes and that attendance is a waste of time. Similarly, another participant stated:
“I was approaching eighty and if the X-PERT programme was trying to prolong my life I acknowledged that I didn’t have much that you could prolong” (Edward, 80 years old)
Together these extracts illustrate that some individuals with type 2 diabetes may weigh up the time spent attending DSME against the time gained from attending to inform their decision about whether attendance would be worthwhile.
Limited knowledge of DSME
Another key barrier to attendance was limited information about the content of the sessions, the reason for their referral or the personal benefits of attending DSME. This prevented individuals from deciding whether they needed to attend as they were unable to identify the purpose of DSME or what they could gain.
“I got a leaflet through the post about it [DSME] so I kind of understood what it was about in general terms I think but I wasn’t really sure what each of the sessions would address. It would be nice to know and understand a bit more about it.” (Andrew)
Nearly all participants who reported having limited knowledge about DSME stated they would be more likely to attend if they had received more information about what they could gain from attending. This suggests that perceiving positive benefits from participating in DSME may play an important role in people’s decision to participate.
“My GP should have given me a better understanding of what it’s going to offer me. If I was confident and convinced that it was going to help me manage things like diet and lifestyle then my mind feels like it might be beneficial” (Andrew).
A deficit of information about DSME was typically attributed to the GP or nurse caring for the individual. This suggests that primary care physicians are a key source of information and have the potential to play an important role in an individual’s decision to attend DSME. This may also reflect individuals’ perception of a doctor-patient relationship whereby their physician is an expert whose role is to provide knowledge, inform and educate them about treatment.
“It was like well “why are you referring me?”, “why aren’t you taking the time?”. You’re my doctor and you know my history. I think an explanation and maybe a little bit more understanding towards me as to why it was happening.” (Becky)
“It’s [DSME] not really something I’ve got a lot of knowledge about anyway which I think falls down to the GP. I think my GP should have explained it more” (Alice)
Theme 2: practical barriers
Numerous practical barriers prevented individuals from being able to attend DSME. These barriers included the programme schedule (sub-theme 1) and transportation issues (sub-theme 2).
Programme schedule
A frequently cited barrier to attendance were other commitments, such as work and childcare, that conflicted with the programme’s hours of operation. These commitments prevented individuals from being able to attend, despite them expressing motivation to do so.
“I was quite interested in going, but unfortunately the times didn’t match with my work life.” (Becky)
Some participants could not commit to attending each session. Unsurprisingly, this was common among those who worked shifts, irregular hours or abroad.
“I had to attend the same class every week [ … ] well I don’t have that flexibility because my rota changes on a weekly basis.” (Alice)
Several participants reported that online DSME would help them overcome barriers associated with work, childcare and commitment because it would enable them to complete the programme at their own convenience; as one participant stated: “ You don’t have to be in a particular place at a particular time. ” (Andrew).
Similarly, another barrier to attending DSME was the programme’s schedule which often impeded or interrupted individuals’ limited free time which they did not want to sacrifice. Free time was perceived highly ‘ valuable’ (Edward) and ‘ precious’ (Andrew) and attending the programme would require an investment of time which would draw away from other highly valued activities such as hobbies and family life.
“I knew there was a weekend course and the main two things for me were taking up my time at the weekend because I work away quite a lot and I like to spend weekends with my kids.” (Alex)
Transportation issues
Difficulties travelling to DSME was another impediment to attendance, particularly if the individual had work commitments or needed public transport to get to the programme’s venue.
“A lot of it was buses and the times wouldn’t have got me back in time to go to work. Hanging about for buses … it’s just awkward.” (Shelley)
Some individuals could not attend DSME due to a comorbidity which presented mobility and transportation issues in getting to the venue. Comorbidities cited in this study included severe back or leg problems, cancer, stroke, chronic obstructive pulmonary disease, amputation and arthritis.
“The flare up of the rheumatoid arthritis was so bad at one point that I had difficulty pulling up my own pants so, if you can imagine, having to actually walk anywhere was very painful.” (Julie)
For people with a physical comorbidity, attending DSME may require the aid of others to get to the venue. This was associated with logistical barriers (e.g. time and availability of carer/driver) as well as the mental burden of hassling another person. For people with mobility-limiting comorbidities, these barriers may outweigh the benefits of attending.
“Being disabled I need to summon up Dave my driver who can take me wherever I need to go [ … ] it’s too much of a hassle [ … ] just trying to gauge how long the meeting would take and how much a question and answer would be and then getting the driver to pick me up at the right time without wasting anybody’s time is a difficult issue.” (Edward)
This study conducted interviews to gather insights into the reasons for not attending DSME among adults with type 2 diabetes. One of the two main reasons for non-attendance identified in this study was participants’ perception they did not need DSME. This arose from individuals’ self-efficacy to manage their condition, the low priority they gave their type 2 diabetes and having limited information/knowledge about DSME. The second main reason for non-attendance were practical barriers and these encompassed structural issues relating to transport and the programme’s schedule. This discussion chapter will focus on how these barriers relate to the constructs in ABM and previous literature, as well as consider the ways in which attendance to DSME can be optimised.
Individuals’ self-efficacy regarding control over their type 2 diabetes and knowledge about their condition were frequently cited as reasons for non-attendance in the current study. These findings support previous research that has found perceptions of knowledge and competency in self-managing one’s type 2 diabetes as barriers to DSME attendance [ 29 , 30 ]. According to ABM, ‘ predisposing factors’ which can impede health service use include high self-efficacy such as knowledge of one’s health condition and ability to manage one’s condition [ 19 ]. This construct, therefore, mirrors the findings in the current study whereby key reasons for non-attendance included having good knowledge about one’s condition and the necessary skills to self-manage their type 2 diabetes.
The present study also found that health professionals may influence individuals’ perceived need to attend DSME. Physicians who conveyed to individuals that their condition was not serious often led individuals to believe they did not need to take further action. This suggests individual factors (e.g. self-efficacy) are not the sole determinants of perceived need but external factors, such as a physician’s assessment, also play a role in individuals’ appraisal of whether they need to attend DSME. These findings are congruent with the ‘ need factors’ construct of ABM which specifically distinguishes the difference between health professionals’ and individuals’ judgement of health status and, in turn, recognises the influence health professionals can have on individuals’ engagement with a particular health service [ 19 ]. This supports the use of ABM in mapping out the reasons for not attending DSME. In light of this, it is important that health professionals accurately assess and convey to individuals the status of their health and do not undermine or over-emphasise the severity of an individual’s type 2 diabetes. Undermining the severity of an individual’s diabetes may, as our study suggests, undermine motivation to attend DSME. On the other hand, over-emphasising the severity of an individual’s type 2 diabetes may lead to undue anxiety [ 31 ]. Health professionals therefore play a key role in helping an individual understand the severity of their type 2 diabetes and, in turn, influencing individuals’ decision about whether to participate in DSME.
A novel barrier to attendance arising from the current study was the pre-existing receipt of support from a primary care physician. This finding is congruent with the ‘ enabling factors’ category of ABM which outlines that the availability and nature of support can facilitate or impede health service utilisation [ 19 ]. However, it contrasts with previous findings in the field which have found lack of support and poor physician-patient relationships as barriers to attendance [ 32 ]. Our findings may be explained by a study by Gucciardi and colleagues [ 33 ] which found that some individuals perceive primary care physicians to provide the same coverage of diabetes education and lifestyle modification skills training as DSME. Similarly, another study found that individuals reported missing diabetes clinic appointments because they were already seeing a family physician or diabetes specialist [ 34 ]. These findings suggest that individuals who already feel well looked after and monitored may have their needs being met already and therefore, do not need to attend DSME. In such a situation, it may be beneficial for the individual, using their knowledge of their type 2 diabetes and self-management behaviours, and the physician, using their knowledge of DSME, to work together to consider whether DSME can offer any additional benefits over and above their pre-existing care and support – and whether such benefits are worth the costs of attending (e.g. time, finance).
The low prioritisation of one’s type 2 diabetes was also found to be a reason for non-attendance among some individuals. This is in line with the ‘ predisposing factors’ construct of ABM which outlines that attitudes towards one’s health and service use can facilitate or impede health service utilisation [ 19 ]. Attributing a low priority towards one’s type 2 diabetes has been cited as a key reason for non-attendance elsewhere in the literature [ 30 , 35 ].
In the current study, low prioritisation of one’s type 2 diabetes was evident among individuals with a comorbidity whereby they perceived some conditions as more serious than others and prioritised another health condition over their type 2 diabetes. This supports similar findings that the burden associated with having and managing a comorbidity can impede resources and motivation to manage one’s type 2 diabetes [ 36 ], particularly when the disease and treatment burdens are greater for the comorbid condition than the burdens of type 2 diabetes [ 37 , 38 ].
Disease and treatment burden from comorbid conditions can also have significant detrimental impacts on mental health and wellbeing [ 39 ]. This emphasises the need to acknowledge (and manage) such comorbidities when individuals are referred to DSME – particularly given associations between greater life satisfaction and wellbeing and improved treatment adherence [ 40 ].
The low prioritisation some people give their type 2 diabetes may also reflect a culture that perceives type 2 diabetes to be the ‘mild’ form of diabetes, despite its high morbidity and mortality rates [ 41 ]. The experiences of individuals in other cultures may differ depending on different cultural perceptions of type 2 diabetes. These findings suggest that health professionals may wish to raise awareness of the complications that could arise from their type 2 diabetes and help facilitate healthy behaviours that can benefit both their type 2 diabetes and comorbidities. Motivational interviewing which involves health professionals working alongside individuals to explore their views about their condition and behaviours, rather than immediately giving advice or referring them to DSME, may also help to better understand the unique views, needs and capabilities of the individual with comorbidity and assess whether DSME would be beneficial [ 42 , 43 ]. Motivational interviewing can also be used to help people reflect on any ambivalence towards self-management and to help people prioritise what is most important to them in their lives [ 44 ].
Limited knowledge about the content, purpose and benefits of SDE also acted as a barrier to attendance. This finding is in line with the ‘ enabling factors’ construct of ABM which outlines that inadequate personal resources, such as limited knowledge about a service, can impede health service utilisation [ 19 ]. It also corroborates previous qualitative literature which cite a lack of familiarity and knowledge about DSME as common barriers to attendance [ 45 ]. A novel finding in this study was that individuals often attributed limited information about DSME to their primary care physician. Interestingly, however, several studies have found that physicians may feel unable to discuss the benefits, goals and expectations of DSME due to their own lack of knowledge of DSME [ 46 , 47 ]. This highlights the need to empower individuals with type 2 diabetes to seek information about DSME themselves, rather than relying on their primary care physician as a main source of knowledge. Physicians who have a basic understanding of key sources where people can go to find out more information about DSME would likely be beneficial [ 47 ].
Previous research has also highlighted that a lack of familiarity and knowledge about DSME may stem from information about DSME that is inaccessible [ 47 ]. It is therefore crucial that information about DSME, as well as the programme itself, is made available in accessible and acceptable formats such as other languages, easy-read, British Sign Language and audio. The provision of DSME in other languages is highly relevant given that the prevalence of type 2 diabetes is three to five times higher in minority ethnic groups compared to the white British population and approximately 10–12 years earlier onset [ 48 ]. There is also strong evidence that health literacy – a person’s ability to understand and use information to make decisions about their health – is a strong predictor of health-related knowledge, illness self-management, health service use, health, and survival in people with type 2 diabetes [ 49 ]. People with low health literacy levels are more likely to have lower health-related knowledge [ 50 , 51 ] and self-management [ 52 , 53 ]. It is therefore critical that information about DSME (e.g. aims, benefits etc.) is provided in a format that is accessible and engaging to people with varying levels of health literacy [ 54 ]. The need to adopt and provide an adequate service for all societal groups also supports why a person-centred approach to overcoming barriers and increasing engagement with DSME is of paramount importance.
The final barrier to attending DSME identified in this study were the practical barriers associated with attending, namely conflicts between the programme’s schedule and other commitments and transportation issues with getting to the venue. Both of these barriers have been cited in previous literature [ 14 ] and are in line with the ‘ enabling factors’ category of ABM which outlines that practical barriers to obtaining care (e.g. income, other responsibilities) can impede health service utilisation [ 19 ].
Alternative methods of delivering DSME, such as offering the course online or via a mobile application, was well-received by participants and may help to alleviate barriers of time, commitment, mobility and transportation by enabling people to access DSME at their own convenience. This may be particularly pertinent for individuals who work shifts or on zero-hour contracts where it may be difficult or not possible for them to get paid time off work to attend DSME. Indeed, such individuals tend to be those with lower socio-economic status and, in turn, also at risk of poorer self-management outcomes [ 55 ]. An additional benefit of online DSME is that it can also be made available to large numbers of individuals at minimal cost [ 56 ]. An online DSME programme, called X-PERT Health, has demonstrated significant benefits to a range of diabetes outcomes, such as glycaemic control, body weight, blood pressure and cholesterol [ 57 ]. Similarly, in a randomised control trial, a web-based self-management programme for people with type 2 diabetes (called HeLP-Diabetes) improved glycaemic control over 12 months [ 58 ]. The offer of online DSME may therefore help to increase attendance and retain individuals by offering DSME at a time and place that suits people’s individual needs.
However, it is important to recognise that some individuals, particularly those with very low socioeconomic status, may be unable or find it difficult to engage with online DSME due to an absence of internet and/or technology (e.g. laptop, tablet, smart phone). To overcome this, additional funding and resources would be beneficial in order to assist individuals in accessing online DSME (e.g. provision of a tablet, free Wi-Fi), or increasing the frequency of DSME so that barriers of time and the programme’s schedule are minimised [ 59 ].
A strength of this research is its use of ABM as a well-supported model to illuminate the barriers to attending DSME. All three constructs of ABM were congruent with individuals’ reasons for not attending DSME. In particular, ABM specifically distinguishes the influence that health professionals’ judgement of health status can have on someone’s decision to engage with a particular health service – a key finding in this study. Our research therefore supports ABM in helping to map out the reasons for non-attendance to DSME.
A key limitation is that participants were recruited by phoning eligible people and inviting them to participate. Some individuals who declined the invite to participate held highly negative attitudes towards their type 2 diabetes. For example, some said their type 2 diabetes was shameful, burdensome and that they did not want to talk about it. It is therefore important to be aware that the views of individuals with such attitudes towards their diagnosis may not be fully captured in this study, and that these negative attitudes towards one’s diagnosis may have been a barrier to attendance in themselves.
In summary, the reasons for not attending DSME found in this study are wide-ranging, complex and individualised, providing further support to existing literature on the barriers to DSME attendance. The findings mirrored the constructs in ABM indicating that ABM is a well-supported model to help map out the barriers to DSME attendance. There is no one-size-fits-all solution to increasing attendance. Instead, a more person-centred approach to understanding people’s experience, needs and capabilities is essential to help identify and overcome barriers to attendance. This is in line with the evidence-base that person-centred approaches to health care and promotion are highly effective at overcoming barriers and increasing engagement [ 60 ].
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Diabetes self-management education
Andersen’s Behavioural Model of Health Service Utilisation
World Health Organisation. Diabetes. https://www.who.int/news-room/fact-sheets/detail/diabetes . Accessed 12 Jan 2021.
Glasgow RE, Anderson RM. In diabetes care, moving from compliance to adherence is not enough. Diabetes Care. 1999;22(12):2090–2.
Article CAS PubMed Google Scholar
Ruggiero L, Glasgow R, Dryfoos JM, Rossi JS, Prochaska JO, Orleans CT, et al. Diabetes self-management: self-reported recommendations and patterns in a large population. Diabetes Care. 1997;20(4):568–76.
Ahola AJ, Groop PH. Barriers to self-management of diabetes. Diabet Med. 2013;30(4):413–20.
Stolar M. Glycemic control and complications in type 2 diabetes mellitus. Am J Med. 2010;123(3):3–11.
Article CAS Google Scholar
National Institute of Clinical Excellence. Type 2 diabetes in adults: management. https://www.nice.org.uk/guidance/ng28/chapter/1-Recommendations#individualised-care . Accessed 12 Jan 2021.
Deakin T. Structured education programmes improve control in diabetes. J Diabetes Nurs. 2012;16(7):266–72.
Google Scholar
Skinner TC, Carey ME, Cradock S, Daly H, Davies MJ, Doherty Y, et al. Diabetes education and self-management for ongoing and newly diagnosed (DESMOND): process modelling of pilot study. Patient Educ Couns. 2006;64(1–3):369–77.
Article PubMed Google Scholar
Deakin TA, Cade JE, Williams R, Greenwood DC. Structured patient education: the diabetes X-PERT Programme makes a difference. Diabetic Med. 2006;23(9):944–54.
National Health Service. National Diabetes Audit, 2017–18. https://files.digital.nhs.uk/88/F1E544/National%20Diabetes%20Audit%202017-18%20Full%20Report%201%2C%20Care%20Processes%20and%20Treatment%20Targets.pdf . Accessed 12 Jan 2021.
Norris SL, Engelgau MM, Narayan KV. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care. 2001;24(3):561–87.
Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25(7):1159–71.
Steinsbekk A, Rygg L, Lisulo M, Rise MB, Fretheim A. Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with meta-analysis. BMC Health Serv Res. 2012;12(1):1–9.
Article Google Scholar
Horigan G, Davies M, Findlay-White F, Chaney D, Coates V. Reasons why patients referred to diabetes education programmes choose not to attend: a systematic review. Diabet Med. 2017;34(1):14–26.
Malcolm JC, Maranger J, Taljaard M, Shah B, Tailor C, Liddy C, et al. Into the abyss: diabetes process of care indicators and outcomes of defaulters from a Canadian tertiary care multidisciplinary diabetes clinic. BMC Health Serv Res. 2013;13(1):1–9.
Nicolucci A, Cavaliere D, Scorpiglione N, Carinci F, Capani F, Tognoni G, et al. A comprehensive assessment of the avoidability of long-term complications of diabetes. A case-control study. SID-AMD Italian study Group for the Implementation of the St. Vincent declaration. Diabetes Care. 1996;19(9):927–33.
McSharry J, Dinneen SF, Humphreys M, O’Donnell M, O'Hara MC, Smith SM, et al. Barriers and facilitators to attendance at type 2 diabetes structured education programmes: a qualitative study of educators and attendees. Diabet Med. 2019;36(1):70–9.
Winkley K, Evwierhoma C, Amiel SA, Lempp HK, Ismail K, Forbes A. Patient explanations for non-attendance at structured diabetes education sessions for newly diagnosed type 2 diabetes: a qualitative study. Diabet Med. 2015;32(1):120–8.
Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Q. 2005;83(4):1–28.
Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;1:1–0.
Johnson JE, Weinert C, Richardson JK. Rural residents’ use of cardiac rehabilitation programs. Public Health Nurs. 1998;15(4):288–96.
Holtzman CW, Shea JA, Glanz K, Jacobs LM, Gross R, Hines J, et al. Mapping patient-identified barriers and facilitators to retention in HIV care and antiretroviral therapy adherence to Andersen's behavioral model. AIDS Care. 2015;27(7):817–28.
Article PubMed PubMed Central Google Scholar
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health C. 2007;19(6):349–57.
Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Health. 2019;11(4):589–97.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Faulkner SL, Trotter SP. Theoretical saturation. Int Ency of Commun Res Meth. 2017;24:1–2.
Lo R, MacLean D. The dynamics of coping and adapting to the impact when diagnosed with diabetes. Aust J Adv Nurs. 2001;19(2):26–32.
CAS PubMed Google Scholar
Egede LE, Bonadonna RJ. Diabetes self-management in African Americans: an exploration of the role of fatalism. Diabetes Educ. 2003;29(1):105–15.
Coates V, Slevin M, Carey M, Slater P, Davies M. Declining structured diabetes education in those with type 2 diabetes: a plethora of individual and organisational reasons. Patient Educ Couns. 2018;101(4):696–702.
Gucciardi E, Chan VW, Lo BK, Fortugno M, Horodezny S, Swartzack S. Patients’ perspectives on their use of diabetes education centres in Peel-Halton region in southern Ontario. Can J Diabetes. 2012;36(4):214–7.
Wens J, Vermeire E, Van Royen P, Sabbe B, Denekens J. GPs’ perspectives of type 2 diabetes patients’ adherence to treatment: a qualitative analysis of barriers and solutions. BMC Fam Pract. 2005;6(1):1–0.
Findlay-White F, Slevin M, Carey ME, Coates V. “What’s the point?”: understanding why people with type 2 diabetes decline structured education. Clin Diabetes. 2020;38(2):166–75.
Gucciardi E, DeMelo M, Offenheim A, Stewart DE. Factors contributing to attrition behavior in diabetes self-management programs: a mixed method approach. BMC Health Serv Res. 2008;8(33):1–11.
Lloyd J, Sherriff R, Fisher M, Burns-Cox C. Non-attendance at the diabetic clinic. Pract Diabetes Int. 1990;7(5):228–9.
Kerr EA, Heisler M, Krein SL, Kabeto M, Langa KM, Weir D, et al. Beyond comorbidity counts: how do comorbidity type and severity influence diabetes patients’ treatment priorities and self-management? J Gen Intern Med. 2007;22(12):1635–40.
Beverly EA, Wray LA, Chiu CJ, Weinger K. Perceived challenges and priorities in co-morbidity management of older patients with type 2 diabetes. Diabet Med. 2011;28(7):781–4.
Article CAS PubMed PubMed Central Google Scholar
Sav A, King MA, Whitty JA, Kendall E, McMillan SS, Kelly F, et al. Burden of treatment for chronic illness: a concept analysis and review of the literature. Health Expect. 2015;18(3):312–24.
Heckman BW, Mathew AR, Carpenter MJ. Treatment burden and treatment fatigue as barriers to health. Curr Opin Psychol. 2015;5:31–6.
Ducat L, Philipson LH, Anderson BJ. The mental health comorbidities of diabetes. JAMA. 2014;312(7):691–2.
Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2000;160(21):3278–85.
Cooper HC, Booth K, Gill G. Patients’ perspectives on diabetes health care education. Health Educ Res. 2003;18(2):191–206.
Britt E, Hudson SM, Blampied NM. Motivational interviewing in health settings: a review. Patient Educ Couns. 2004;53(2):147–55.
Miller WR, Rollnick S. Motivational interviewing: helping people change. 3rd ed. New York: Guilford Press; 2013.
Schäfer I, Pawels M, Küver C, Pohontsch NJ, Scherer M, van den Bussche H, et al. Strategies for improving participation in diabetes education. A qualitative study. Plos One. 2014;9(4):e95035.
Hardy KJ, O'Brien SV, Furlong NJ. Information given to patients before appointments and its effect on non-attendance rate. BMJ. 2001;323(7324):1298–300.
Ross J, Stevenson FA, Dack C, Pal K, May CR, Michie S, et al. Health care professionals’ views towards self-management and self-management education for people with type 2 diabetes. BMJ Open. 2019;9(7):e029961.
Winkley K, Upsher R, Keij SM, Chamley M, Ismail K, Forbes A. Healthcare professionals’ views of group structured education for people with newly diagnosed type 2 diabetes. Diabet Med. 2018;35(7):911–9.
Goff LM. Ethnicity and type 2 diabetes in the UK. Diabet Med. 2019;36(8):927–38.
Greenhalgh T. Health literacy: towards system level solutions. BMJ. 2015;24(350):1026.
Al Sayah F, Majumdar SR, Williams B, Robertson S, Johnson JA. Health literacy and health outcomes in diabetes: a systematic review. J Gen Int Med. 2013;28(3):444–52.
Bains SS, Egede LE. Associations between health literacy, diabetes knowledge, self-care behaviors, and glycemic control in a low income population with type 2 diabetes. Diabetes Technol Ther. 2011;13(3):335–41.
Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288(4):475–82.
Van der Heide I, Uiters E, Rademakers J, Struijs JN, Schuit AJ, Baan CA. Associations among health literacy, diabetes knowledge, and self-management behaviour in adults with diabetes: results of a Dutch cross-sectional study. J Health Commun. 2014;19(sup2):115–31.
Rowsell A, Muller I, Murray E, Little P, Byrne CD, Ganahl K, et al. Views of people with high and low levels of health literacy about a digital intervention to promote physical activity for diabetes: a qualitative study in five countries. J Med Internet Res. 2015;17(10):e230.
Bihan H, Laurent S, Sass C, Nguyen G, Huot C, Moulin JJ, et al. Association among individual deprivation, glycemic control, and diabetes complications: the EPICES score. Diabetes Care. 2005;28(11):2680–5.
Li J, Parrott S, Sweeting M, Farmer A, Ross J, Dack C, et al. Cost-effectiveness of facilitated access to a self-management website, compared to usual care, for patients with type 2 diabetes (HeLP-diabetes): randomized controlled trial. J Med Internet Res. 2018;20(6):e9256.
Deakin T. X-PERT Audit Results. https://www.xperthealth.org.uk/wp-content/uploads/2020/11/X-PERT-Audit-Award-Report-November-2020.pdf . Accessed 12 Jan 2021.
Murray E, Sweeting M, Dack C, Pal K, Modrow K, Hudda M, et al. Web-based self-management support for people with type 2 diabetes (HeLP-diabetes): randomised controlled trial in English primary care. BMJ Open. 2017;7:e016009.
Office for National Statistics. Exploring the UK’s digital divide. https://www.ons.gov.uk/peoplepopulationandcommunity/householdcharacteristics/homeinternetandsocialmediausage/articles/exploringtheuksdigitaldivide/2019-03-04 . Accessed 28 March 2021.
Yardley L, Ainsworth B, Arden-Close E, Muller I. The person-based approach to enhancing the acceptability and feasibility of interventions. Pilot Feasibility Stud. 2015;1(37):1–7.
Download references
Acknowledgements
With thanks to Sarah Button and the team at the Wellbeing Service, Virgin Care Limited (now called HCRG Care Group) for their support throughout the project.
There was no external funding for this project. The study was conducted as part of an unfunded MSc placement project.
Author information
Authors and affiliations.
Department of Psychology, University of Bath, Bath, BA2 7AY, UK
Imogen Coningsby, Ben Ainsworth & Charlotte Dack
Present Address: Public Health and Preventative Services, Bath and North East Somerset Council, Keynsham Civic Centre, Market Walk, Keynsham, BS31 1FS, UK
Imogen Coningsby
You can also search for this author in PubMed Google Scholar
Contributions
IC developed the research question, gathered literature, created the study materials, gained ethical approval, recruited participants, conducted and transcribed the interviews, analysed the data and wrote up the report. BA and CD assisted with gathering literature, obtaining ethical approval, analysing and interpreting the data and writing the final manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Ben Ainsworth .
Ethics declarations
Ethics approval and consent to participate.
The study was conducted in accordance with the British Psychological Society recommendations for research. Ethical approval was received from the University of Bath Psychology Ethics Committee (reference number: 20–133). All participants gave written and verbal consent before participating in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Coningsby, I., Ainsworth, B. & Dack, C. A qualitative study exploring the barriers to attending structured education programmes among adults with type 2 diabetes. BMC Health Serv Res 22 , 584 (2022). https://doi.org/10.1186/s12913-022-07980-w
Download citation
Received : 16 August 2021
Accepted : 19 April 2022
Published : 30 April 2022
DOI : https://doi.org/10.1186/s12913-022-07980-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Type 2 diabetes
- Diabetes mellitus
- Patient non-attendance
- Self-management
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]

NURS 5367 Evidence-Based Practice
- Create a PICO
- PICO Keyword Search Strategy
- PICO Keyword Search
- PICO Subject Heading Search
- Combining Keyword and Subject Heading Searches
- Adding Filters/Limiters
- Video Review of Steps
- Finding Clinical Guidelines This link opens in a new window
- Poster Presentations This link opens in a new window

Form a Keyword Search Strategy Using PICO
Example pico question: , do type 2 diabetics (p) get better glycemic control (o) with exercise as the primary treatment (i) than those who get drug therapy as a primary treatment (c).
Follow these steps to form your search strategy:
- (P) type 2 diabetes
- (I) exercise
- (C) drug therapy
- (O) glycemic control
- Brainstorm and list the main topics and alternative keywords (synonyms) from each part of your PICO that can be used for your search. For many terms, there will be more than 3 synonyms.
- (P) type 2 diabetes OR type 2 diabetes mellitus OR t2dm OR t2d OR niddm OR non-insulin dependent diabetes mellitus
- (I) exercise OR physical activity OR fitness OR aerobic training OR strength training OR cardiovascular training OR workout OR active OR movement
- (C) drug therapy OR drug intervention OR pharmacologic therapy OR pharmacologic intervention
- (O) glycemic control OR hba1c OR blood sugar OR blood glucose
- << Previous: Create a PICO
- Next: PICO Keyword Search >>
- Last Updated: Dec 8, 2023 10:05 PM
- URL: https://libguides.uta.edu/EBP
University of Texas Arlington Libraries 702 Planetarium Place · Arlington, TX 76019 · 817-272-3000
- Internet Privacy
- Accessibility
- Problems with a guide? Contact Us.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Mini Review
- Published: 13 May 2020
Metabolism and metabolomics
Diabetes and COVID-19: evidence, current status and unanswered research questions
- Ritesh Gupta 1 ,
- Akhtar Hussain 2 , 3 &
- Anoop Misra ORCID: orcid.org/0000-0001-5785-5833 1 , 4 , 5
European Journal of Clinical Nutrition volume 74 , pages 864–870 ( 2020 ) Cite this article
26k Accesses
110 Citations
67 Altmetric
Metrics details
- Diabetes complications
- Epidemiology
Patients with diabetes who get coronavirus disease 2019 (COVID-19) are at risk of a severe disease course and mortality. Several factors especially the impaired immune response, heightened inflammatory response and hypercoagulable state contribute to the increased disease severity. However, there are many contentious issues about which the evidence is rather limited. There are some theoretical concerns about the effects of different anti-hyperglycaemic drugs. Similarly, despite the recognition of angiotensin converting enzyme 2 (ACE2) as the receptor for severe acute respiratory syndrome coronavirus 2 (SARS CoV-2), and the role of ACE2 in lung injury; there are conflicting results with the use of angiotensin converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARB) in these patients. Management of patients with diabetes in times of restrictions on mobility poses some challenges and novel approaches like telemedicine can be useful. There is a need to further study the natural course of COVID-19 in patients with diabetes and to understand the individual, regional and ethnic variations in disease prevalence and course.
Similar content being viewed by others

COVID-19 and diabetes mellitus: from pathophysiology to clinical management
Soo Lim, Jae Hyun Bae, … Michael A. Nauck
Association of COVID-19 with diabetes: a systematic review and meta-analysis
Paddy Ssentongo, Yue Zhang, … Djibril M. Ba

Hypertension and related diseases in the era of COVID-19: a report from the Japanese Society of Hypertension Task Force on COVID-19
Shigeru Shibata, Hisatomi Arima, … Hiroshi Itoh
The high prevalence of diabetes globally makes it a frequent comorbidity in patients with coronavirus-associated disease 2019 (COVID-19). Though diabetes increases the risk of infection in general, most studies have reported prevalence of diabetes almost similar to that in general population in patients with COVID-19. A meta-analysis of eight trials in China showed that diabetes was present in 8% of 46,248 patients with COVID-19 [ 1 ]. Understandably, prevalence of diabetes in patients with COVID-19 varies by region, age and ethnicity. It is not known whether patients with diabetes with well-controlled blood glucose levels have an increased risk of infection with severe acute respiratory syndrome coronavirus 2 (SARS CoV-2).
Why patients with diabetes have increased severity and mortality?
Patients with diabetes who develop COVID-19 have been seen to have a worse prognosis and increased mortality in most studies. In 201 Chinese patients with diabetes a hazard ratio of 2.34 (95% CI, 1.35–4.05; p = 0.002) for acute respiratory distress syndrome (ARDS) [ 2 ] has been reported. Further, meta-analysis of nine studies from China ( n = 1936) showed a significant correlation between severity of COVID-19 and diabetes (OR, 2.67, 95% CI; 1.91–3.74; p < 0.01) [ 3 ]. Similarly, case fatality rate was 7.3% in patients with diabetes as opposed to 2.3% in those without diabetes in a report of 44,672 patients of COVID-19 by Chinese Centre for Disease Control [ 4 ]. A recent study in 1122 patients with COVID-19 in 88 centres across the USA found diabetes to be associated with more than fourfold increase in mortality [ 5 ].
How diabetes increases severity of COVID-19 is unclear, though several factors may be responsible (Table 1 ). Poor glycaemic control impairs several aspects of the innate and adaptive immune response to viral infections and to the potential secondary bacterial infection in the lungs [ 6 , 7 ]. Defects in immunity namely inappropriate T-cell action, impaired natural killer cell activity and defects in complement action could reduce viral clearance [ 8 ]. Interestingly, ARDS in patients with COVID-19 is driven by severe hypoxaemia despite relatively well-preserved lung mechanics. Pre-existing proinflammatory state could accentuate the cytokine storm, which is believed to be responsible for ARDS as well as multi-organ dysfunction in COVID-19 [ 9 ]. In this context, it is important to note that there is strong association between type 2 diabetes, obesity and abnormal secretion of adipokines and cytokines like TNF-alfa and interferon, which may further impair immunity and predispose to severe infection [ 10 ]. Further, diabetes is associated with increased plasminogen levels which has been postulated to increase the virulence of SARS CoV-2 [ 11 ]. Presence of these inflammation and prothrombotic factors has been shown in a study in 174 patients hospitalised with COVID-19 in Wuhan, China; significantly higher serum levels of interleukein 6, erythrocyte sedimentation rate, C‐reactive protein, ferritin, fibrinogen and D‐dimer were reported in patients with diabetes compared with those without diabetes [ 12 ]. Increased viral replication in diabetes may also due to an increase in furin, which is a type‐1 membrane‐bound protease involved in the entry of coronaviruses into the cell [ 13 ]. In addition, pre-existing comorbidities associated with diabetes like hypertension, coronary artery disease and chronic kidney disease further worsen the prognosis. Lastly, hypoglycaemia which could occur during treatment of diabetes may additionally worsen the clinical outcomes.
In this respect role of angiotensin converting enzyme 2 (ACE2) receptor in pathogenesis of COVID-19 in patients with diabetes is intriguing. SARS CoV-2 enters the cell by binding to ACE2, a process which involves many steps and several enzymes and proteins [ 14 ]. There is experimental evidence for downregulation of ACE2 in diabetes [ 15 ], which may predispose to more severe lung injury. On the other hand, ACE2 is a receptor for SARS CoV-2 and this downregulation might reduce the entry of virus into cells. These issues are further discussed below in context of use of anti-hyperglycemic and anti-hypertensive drugs.
Anti-hyperglycaemic drugs: correct selection and potential problems
The precise effect of treatment with various oral anti-hyperglycaemic agents on the severity of COVID-19 is not known, though there are some theoretical considerations. Metformin has shown modest benefits in lower respiratory tract infections and pulmonary tuberculosis [ 16 ], though gastrointestinal tolerability in sick patients is of concern. Thiazolidinediones have been shown to increase ACE2 levels [ 17 ]. However, propensity of thiazolidinediones to cause fluid retention and the risk of congestive heart failure in COVID-19 would make these agents unfavourable for treatment. Glucagon-like peptide-1 agonists have has been shown to increase ACE2 and increase surfactant in experimental animals [ 18 ]. Practical significance of changes in ACE2 levels with use of thiazolidinediones and glucagon-like peptide-1 agonists is not known. Sulfonylureas are effective, but the risk of hypoglycaemia especially in the setting of irregular meals might preclude their use. Nevertheless, sulfonylureas can be considered whenever blood glucose monitoring is possible.
There is some data regarding use of dipeptidyl peptidase 4 (DPP4) inhibitors from previous viral epidemics. DPP4 is the prime receptor for Middle East respiratory syndrome coronavirus responsible for its entry into cell [ 19 ]. Hence the possibility of DPP4 facilitating the entry of SARS CoV-2 into the cell cannot be ruled out. In that context, it is an interesting postulation that widespread use of DPP4 inhibitors in India and many other countries might be protecting individuals with diabetes from this infection. On the other hand, DPP4 inhibitors can potentially interfere with immune response which may be harmful, but clinical data from DPP4 inhibitors has shown that this is generally not the case [ 20 ].
There is increasing use of sodium glucose cotransporter 2 (SGLT-2) inhibitors worldwide and in India. Interestingly, SGLT-2 inhibitors could also activate ACE2 indirectly especially if used along with ACE inhibitors [ 21 ]. There is a hypothetical possibility of SGLT-2 inhibitors reducing lactate production because of reduction in oxygen demand of tissues, which could reduce viral entry by raising cytosolic pH [ 22 ]. Further, caution about dehydration and the possibility of euglycaemic ketoacidosis need to be observed when using SGLT-2 inhibitors in sick patients with COVID-19. Insulin has also been shown to increase ACE2 expression by attenuating the effect of a disintegrin and metalloprotease (ADAM-17) [ 23 ]. Practical relevance of these findings is not known at present. In any case, insulin remains the agent of choice to control sugars in hospitalised patients with COVID-19. This however necessitates frequent monitoring of blood glucose and poses some practical concerns in terms of increasing the exposure of healthcare provider to the COVID-19 patient. Strategies like single dose of basal insulin and self-monitoring of glucose by patients are worth considering in that context. Further, technologies like remote continuous glucose monitoring and insulin pump could be useful.
Thus, it appears safe to continue the usual anti-hyperglycemic medications in most patients who have mild infection, good general condition and normal oral intake. However, SGLT-2 inhibitors might need discontinuation due to the risk of dehydration and euglycaemic ketoacidosis. Metformin may also need to be stopped if there is vomiting or poor oral intake. Doses of other anti-hyperglyacemic drugs like sulfonylureas and insulin may have to be altered depending upon the blood glucose levels. Hospitalised patients especially those requiring intensive care would need insulin for glycaemic control.
Drugs for treatment of comorbidities in diabetes
Angiotensin converting enzyme (ace) inhibitors/angiotensin receptor blockers (arb).
These are commonly used drugs in patients with diabetes, especially in those with hypertension and kidney dysfunction. There have been a lot of literature and debate whether these drugs could benefit or harm patients having COVID-19 infection. This issue is discussed below.
Scientific experimental data that support potential harm duet to ACE inhibitors/ARB in COVID-19
There has been a lot of interest in ACE inhibitors and ARBs following the identification of ACE2 as the receptor for SARS CoV-2. ACE inhibitors and ARBs increase the levels of ACE2 by inhibiting the conversion of angiotensin 1 to angiotensin 2. Increased ACE2 expression could theoretically increase viral binding and entry into cell, though there is no clinical evidence to support this otherwise attractive hypothesis. Reduced angiotensin 2 as a result of ACE inhibition and increased angiotensin 1–7 as a result of increased activity of ACE2 could reduce the cytosolic pH, which could result in more favourable environment for viral endocytosis [ 24 ]. Also, angiotensin 1–7 has been shown to increase sympathetic activity by acting on Mas receptors in the brainstem, which could contribute to cardiovascular morbidity observed in these patients [ 25 ]. However, most of these concerns are hypothetical with minimal evidence.
Scientific experimental data that support benefit due to ACE inhibitors/ARB in COVID-19
Increased ACE2 might not result in increased viral entry because of the limited availability of the serine protease TMPRSS2, which is required for viral binding [ 20 ]. Increased ACE2 and consequently angiotensin 1–7 have vasodilatory and antifibrotic effects and have been shown to be protective against lung injury in animals [ 26 ]. Treatment with ARBs was reported to reduce mortality in Ebola virus infection [ 27 ]. Previously, a small study in ten patients with ARDS showed that recombinant ACE2 was well tolerated and led to an increase in angiotensin (1–7) levels [ 28 ].
Clinical studies with ACE inhibitors/ARBs in COVID-19
There are no controlled studies on the use of ACE inhibitors and ARBs in patients with COVID-19.
The clinical evidence is inconclusive. While one study in China did not find any association of ACE inhibitor use with severity of disease, there was an increased mortality in patients with COVID-19 receiving ACE inhibitors and ARBs in another study [ 29 , 30 ]. One study in the USA did not find any significant difference in mortality in patients who received ACE inhibitors and ARBs and those who did not [ 31 ]. A recently published study in 1128 patients hospitalised with COVID-19 in nine hospitals in Hubei, China showed significantly reduced all-cause mortality with the use of ACE inhibitors or ARBs compared with other anti-hypertensive drugs [ 32 ].
Many patients with COVID-19 have shown hypokalemia indicating activation of RAS [ 33 ], and ACE inhibitors and ARBs may have a role [ 34 ].
In this subject situation is far from clear and there are too many unknown factors, which might be operative in the interaction between ACE2, diabetes, ACE inhibitors/ARBs and lung injury. The lack of evidence for either benefit or harm has prompted European Society of Cardiology Council on Hypertension, European Society of Hypertension and American Heart Association to advise continuing with ACE inhibitors and ARBs in case a patient develops COVID-19 [ 35 ]. A clinical trial is underway to study the ARB losartan and recombinant human ACE2 in patients with COVID-19.
Unanswered questions
There have been several commentaries on the relationship between diabetes and COVID-19 [ 36 ]. However, several unanswered questions remain, about which the knowledge and information is limited. Clearly, further research could lead to important insights (Table 2 ). Some of these are discussed below.
What is the natural history of COVID-19 in patients with diabetes? The natural course of the disease after infection of patients with diabetes with SARS CoV-2 has not been documented well. For example, we don’t know if the incubation period is different in people with diabetes. It is also possible those patients of diabetes who are young, have short duration of diabetes, and well controlled may have less severe COVID-19 infection. There is a possibility of reduced viral clearance in diabetes as has been reported in patients who are on corticosteroids [ 37 ]. This could have public health implications as the patients with diabetes could remain infectious for a longer period than those without diabetes.
Use of drugs in treatment of COVID-19 which could have effect on glycaemia:
Chloroquine has also been licensed for use in India for patients with type 2 diabetes. Although the efficacy of chloroquine is not proven; it has been used in patients with COVID-19 [ 38 ]. Chloroquine has a weak anti-hyperglycaemic effect and there is a theoretical risk of hypoglycaemia when used in combination with other anti-hyperglycaemic drugs.
Corticosteroids, though neither effective nor recommended, are frequently used in ARDS and sepsis and would worsen glycemic levels.
COVID-19 and pancreatic beta cells: there is significant expression of ACE2 receptors in pancreatic islets and hyperglycaemia lasting up to 3 years has been reported in patients with SARS [ 39 ]. Direct injury to beta cells is a possibility and patients recovering from COVID-19 might need major changes in anti-hyperglycaemic regimen. Recently, new-onset diabetes has been reported in patients with COVID-19 [ 11 ].
Suboptimal lifestyle measures and other issues during lockdown:
There are restrictions on movement of people and ‘lockdowns’ in several parts of the world in order to contain the pandemic. This poses some challenges in the evaluation and treatment of patients with diabetes. There are limited opportunities for exercise as regular walks and visits to gyms or swimming pools are not possible. Dietary irregularity could occur because of staying at home.
There is considerable mental stress because of the unpredictability of the disease as well as social immobility as brought out in an excellent study in healthy people in China at the time when there was a huge burden of COVID-19 there [ 40 ].
Patients may find it difficult to procure healthy foods, medicines, insulin, needles and glucose strips etc. because of partial or complete lockdowns. The problem becomes more pronounced with elderly, poor and disadvantaged sections of society.
There could be underreporting of symptoms because of the perceived need to avoid visiting hospitals.
All these factors could cause glucose dysregulation and could predispose patients to complications like infections, hyperosmolar coma, ketoacidosis and even acute cardiac events. A prediction model of the effect of lockdown in India on blood glucose showed a 3.6% increase in HbA1c at the end of 45 days of lockdown and future increase in diabetes-related complications [ 41 ].
Use of remote education and advice: Telemedicine (also emails, texts) can be very helpful in these times to impart education and has been shown to improve glycaemia. Telemedicine guidelines for physicians in India have been published [ 42 ]. Patients need to be educated about the need to visit the hospital urgently in emergency situations like vomiting, drowsiness, shortness of breath, chest pain, weakness of limbs, altered sensorium, etc [ 43 ].
COVID-19 testing for all patients with diabetes? Given the increased severity of COVID-19 in patients with diabetes, a case could be made for testing of all people with diabetes for the presence of disease. That would be a humongous task considering the high prevalence of diabetes. High-risk groups like those with high HbA1c, those with comorbidities, long duration of diabetes or elderly could be chosen for testing, however, utility of this approach remains to be proven, There are frequent false negative tests and repeated testing may be required in asymptomatic individuals. Since there is no treatment currently recommended for asymptomatic people, therefore apart from isolating them, detecting these patients might not prove meaningful clinically.
Ethnic variations in severity of COVI19 in patients with diabetes? In the United States, the disease has caused disproportionately more fatalities in Blacks and Asians compared with Whites [ 44 ]. South Asia, Africa and Korea have seen much lower mortality than rest of the world. Whether it is because of the different approaches topublic health measures, innate immunity or due to some ethnicity-specific variability in response to viral infection, or availability of good medical resources, remains to be studied. Interactions between ethnicity, diabetes and severity of COVID-19 will be of interest, considering the racial disparities in the prevalence of diabetes. According to a recent report, prevalence of COVID-19 and mortality due to the disease correlated significantly with frequency of D allele in ACE gene [ 45 ]. Such polymorphisms in ACE gene as well as several other genes involved in the pathophysiology of COVID-19 might be responsible for individual and ethnic variations in disease course.
Benefits of lockdown? There could be some positive effects of the social restrictions.
Patients have more time for self-care and could pay more attention to diet and exercise if motivated.
Some people have stopped or reduced alcohol and smoking because of non-availability.
There has been significant fall in air pollution as a result of reduced industrial and vehicular emissions [ 46 ]. Increase in blood glucose has been reported with short-term rise in pm 10 (particulate matter <10 microns in diameter) and glycaemic improvement could occur with the fall in pollution [ 47 ].
In view of the issues highlighted above, it is important to recognise the importance of diabetes as a vital comorbidity in patients with COVID-19. There are several contentious issues and the ongoing research will hopefully shed more light on the behaviour of COVID-19 in patients with diabetes.
Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence ofcomorbidities in the novel Wuhan coronavirus (COVID-19) infection: asystematicreview and meta-analysis. Int J Infect Dis. 2020. pii: S1201-9712(20)30136-3. https://doi.org/10.1016/j.ijid.2020.03.017 .
Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020. https://doi.org/10.1001/jamainternmed.2020.0994 .
Chen Y, Gong X, Guo J. Effects of hypertension, diabetes and coronary heart disease on COVID-19 diseases severity: a systematic review and meta-analysis. 2020. https://www.medrxiv.org/content/10.1101/2020.03.25.20043133v1 .
Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020. https://doi.org/10.1001/jama.2020.2648 .
Bode B, Garrett V, Messler J, McFarland R, Crowe J, Booth R, et al. Glycemic characteristics and clinical outcomes of COVID-19 patients hospitalized in the United States. J Diabetes Sci Technol. 2020. https://doi.org/10.1177/1932296820924469 .
Carey IM, Critchley JA, DeWilde S, Harris T, Hosking FJ, Cook DG. Glycemic control and risk of infections among people with type 1 or type 2 diabetes in a large primary care cohort study. Diabetes Care 2018;41:513–21. https://doi.org/10.2337/dc17-2131 .
Article PubMed Google Scholar
Ferlita S, Yegiazaryan A, Noori N, Lal G, Nguyen T, To K, et al. Type 2 diabetes mellitus and altered immune system leading to susceptibility to pathogens, especially mycobacterium tuberculosis. J Clin Med. 2019;8:2219. https://doi.org/10.3390/jcm8122219 .
Article CAS PubMed Central Google Scholar
Nyambuya TM, Dludla PV, Mxinwa V, Nkambule BB. T-cell activation and cardiovascular risk in adults with type 2 diabetes mellitus: A systematic review and meta-analysis. Clin Immunol. 2020;210:108313. https://doi.org/10.1016/j.clim.2019.108313 .
Article CAS PubMed Google Scholar
Maddaloni E, Buzzetti R. Covid-19 and diabetes mellitus: unveiling the interaction of two pandemics. Diabetes Metab Res Rev. 2020:e33213321. https://doi.org/10.1002/dmrr.3321 .
Huttunen R, Syrjänen J. Obesity and the risk and outcome of infection. Int J Obes. 2013;37:333–40.
Article CAS Google Scholar
Ji HL, Zhao R, Matalon S, Matthay MA. Elevated Plasmin(ogen) as a common risk factor for COVID-19 susceptibility. Physiol Rev. 2020;100:1065–75. https://doi.org/10.1152/physrev.00013.2020 .
Article PubMed PubMed Central Google Scholar
Guo W, Li M, Dong Y, Zhou H, Zhang Z, Tian C, et al. Diabetes is a risk factor for the progression and prognosis of COVID‐19. Diabetes Metab Res Rev. 2020:e3319. https://doi.org/10.1002/dmrr.3319 .
Fernandez C, Rysa J, Almgren P, Nilsson J, Engström G, Orho-Melander M, et al. Plasma levels of the proprotein convertase furinandincidence of diabetes and mortality. J Intern Med. 2018;284:377–87. https://doi.org/10.1111/joim.12783 .
Article CAS PubMed PubMed Central Google Scholar
Hoffmann M, Kleine-Weber H, Krüger N, Müller M, Drosten C, Pöhlmann S. The novel coronavirus 2019 (2019-nCoV) uses the SARS-coronavirus receptor ACE2 and the cellular protease TMPRSS2 for entry into target cells. 2020. https://doi.org/10.1101/2020.01.31.929042 .
Li XC, Zhang J, Zhuo JL. The vasoprotective axes of the renin-angiotensin system:physiological relevance and therapeutic implications in cardiovascular, hypertensive and kidney diseases. Pharm Res. 2017;125:21–38.
Mendy A, Gopal R, Alcorn JF, Forno E. Reduced mortality from lower respiratory tract disease in adult diabetic patients treated with metformin. Respirology. 2019;24:646–51.
Article Google Scholar
Zhang W, Xu YZ, Liu B, Wu R, Yang YY, Xiao XQ, et al. Pioglitazone upregulates angiotensin converting enzyme 2 expression in insulin-sensitive tissues in rats with high-fat diet-induced nonalcoholic steatohepatitis. Sci World J. 2014:603409. https://doi.org/10.1155/2014/603409 .
Romaní-Pérez M, Outeiriño-Iglesias V, Moya CM, Santisteban P, González-Matías LC, Vigo E, et al. Activation of the GLP-1 receptor by liraglutide increases ACE2 expression, reversing right ventricle hypertrophy, and improving the production of SP-A and SP-B in the lungs of type 1 diabetes rats. Endocrinology. 2015;156:3559–69.
Arabi YM, Balkhy HH, Hayden FG, Bouchama A, Luke T, Baillie JK, et al. Middle east respiratory syndrome. N Engl J Med. 2017;376:584–94. https://doi.org/10.1056/NEJMsr1408795 .
Yang W, Cai X, Han X, Ji L. DPP-4 inhibitors and risk of infections: a meta-analysis of randomized controlled trials. Diabetes Metab Res Rev. 2016;32:391–404. https://doi.org/10.1002/dmrr.2723 .
Filippatos TD, Liontos A, Papakitsou I, Elisaf MS. SGLT2 inhibitors cardioprotection: a matter debate and multiple hypotheses. Postgrad Med. 2019;131:82–88. https://doi.org/10.1080/00325481.2019.1581971 .
Couselo-Seijas M, Agra-Bermejo RM, Fernández AL, Martínez-Cereijo JM, Sierra J, Soto-Pérez M. High released lactate by epicardial fat from coronary artery disease patients is reduced by dapagliflozin treatment. Atherosclerosis. 2020;292:60–69. https://doi.org/10.1016/j.atherosclerosis.2019.11.016 .
Salem ESB, Grobe N, Elased KM. Insulin treatment attenuates renal ADAM17 and ACE2 shedding in diabetic Akita mice. Am J Physiol-Ren Physiol. 2014;306:F629–39.
Cure E, Cumhur Cure M. Comment on “organ-protective effect of angiotensin-converting Enzyme 2 and its effect on the prognosis of COVID-19”. J Med Virol. 2020. https://doi.org/10.1002/jmv.25848 .
Bilodeau MS, Leiter JC. Angiotensin 1-7 in the rostro-ventrolateral medulla increases blood pressure and splanchnic sympathetic nerve activity in anesthetized rats. RespirPhysiolNeurobiol. 2018;247:103–11.
CAS Google Scholar
Yang P, Gu H, Zhao Z, Wang W, Cao B, Lai C, et al. Angiotensin converting enzyme 2 (ACE2) mediates influenza H7N9 virus-induced acute lunginjury. Sci Rep. 2014;4:7027.
Fedson DS, Jacobson JR, Rordam OM, Opal SM. Treating the host response to Ebola virus disease with generic statins and angiotensin receptor blockers. mBio. 2015;6:e00716. https://doi.org/10.1128/mBio.00716-15 .
Khan A, Benthin C, Zeno B, Albertson TJ, Boyd J, Christie JD, et al. A pilot clinical trial of recombinant human angiotensin converting enzyme 2 in acute respiratory distress syndrome. Crit Care. 2017;21:234.
Peng YD, Meng K, Guan HQ, Leng L, Zhu RR, Wang BY, et al. Clinical characteristics and outcomes of 112 cardiovascular disease patients infected by 2019-nCoV. Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48:E004. https://doi.org/10.3760/cma.j.cn112148-20200220-00105 .
Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, et al. Cardiovascular Implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;27:e201017. https://doi.org/10.1001/jamacardio.2020.1017 .
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020. https://doi.org/10.1001/jama.2020.6775 .
Zhang, Zhu L, Cai L, Lei F, et al. Association of inpatient use of angiotensin converting enzyme inhibitors and angiotensinii receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res. 2020. https://doi.org/10.1161/CIRCRESAHA.120.317134 .
Chen D, Li X, Song Q, Hu C, Su F, Dai J, et al. Hypokalemia and clinical implications in patients with coronavirus disease 2019 (COVID-19). 2020. https://doi.org/10.1101/2020.02.27.20028530 .
Zhang, Zhu L, Cai L, Lei F, Qin JJ, Xie J, et al. Association of inpatient use of angiotensin converting enzyme inhibitors and angiotensinii receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res. 2020. https://doi.org/10.1161/CIRCRESAHA.120.317134 .
Gupta R, Misra A. Contentious issues and evolving concepts in the clinical presentation and management of patients with COVID-19 infection with reference to use of therapeutic and other drugs used in Co-morbid diseases (Hypertension, diabetes etc). Diabetes Metab Syndr. 2020;14:251–4. https://doi.org/10.1016/j.dsx.2020.03.012 .
Hussain A, Bhowmik B, do Vale Moreira NC. COVID-19 and diabetes: knowledge in progress. Diabetes Res Clin Pract. 2020:108142. https://doi.org/10.1016/j.diabres.2020.108142 .
Han Y, Jiang M, Xia D, He L, Lv X, Liao X, et al. COVID-19 in a patient with long-term use of glucocorticoids: A study of a familial cluster. Clin Immunol. 2020;214:108413. https://doi.org/10.1016/j.clim.2020.108413 .
Singh AK, Singh A, Shaikh A, Singh R, Misra A. Chloroquine and hydroxychloroquine in the treatment of COVID-19 with or without diabetes: a systematic search and a narrative review with a special reference to India and other developing countries. Diabetes Metab Syndr. 2020;14:241–6. https://doi.org/10.1016/j.dsx.2020.03.011 .
Yang JK, Lin SS, Ji XJ, Guo LM. Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes. Acta Diabetol. 2010;47:193–9. https://doi.org/10.1007/s00592-009-0109-4 .
Zhang SX, Wang Y, Rauch A, Wei F. Unprecedented disruption of lives and work: health, distress and life satisfaction of working adults in China one monthinto the COVID-19 outbreak. Psychiatry Res. 2020;288:112958. https://doi.org/10.1016/j.psychres.2020.112958 .
Ghosal S, Sinha B, Majumder M, Misra A. Estimation of effects of nationwide lockdown for containing coronavirus infection on worsening of glycosylated haemoglobin and increase in diabetes-related complications: a simulation model using multivariate regression analysis. Diabetes Metab Syndr. 2020;14:319–23. https://doi.org/10.1016/j.dsx.2020.03.014 .
Ghosh A, Gupta R, Misra A. Telemedicine for diabetes care in India during COVID19 pandemic and national lockdown period: guidelines for physicians. Diabetes Metab Syndr. 2020;14:273–6. https://doi.org/10.1016/j.dsx.2020.04.001 .
Gupta R, Ghosh A, Singh AK, Misra A. Clinical considerations for patients with diabetes in times of COVID-19 epidemic. Diabetes Metab Syndr. 2020;14:211–2. https://doi.org/10.1016/j.dsx.2020.03.002 .
APM Research Lab. The color of coronavirus, COVID-19 deaths by race and ethnicity in the U.S. APM Research Lab; 2020. https://www.apmresearchlab.org/covid/deaths-by-race .
Delanghe JR, Speeckaert MM, De Buyzere ML. The host’s angiotensin-converting enzyme polymorphism may explain epidemiological findings in COVID-19 infections. Clin Chim Acta. 2020;505:192–3. https://doi.org/10.1016/j.cca.2020.03.031 .
Dutheil F, Baker JS, Navel V. COVID-19 as a factor influencing air pollution? Environ Pollut. 2020;263:114466. https://doi.org/10.1016/j.envpol.2020.114466 .
Yang BY, Fan S, Thiering E, Seissler J, Nowak D, Dong GH. et al. Ambientair pollution and diabetes: a systematic review and meta-analysis. Environ Res. 2020;180:108817. https://doi.org/10.1016/j.envres.2019.108817 .
Download references
Author information
Authors and affiliations.
Fortis CDOC Hospital, Chirag Enclave, New Delhi, India
Ritesh Gupta & Anoop Misra
Chronic Disease—Diabetes, NORD University, Stjørdal, Norway
Akhtar Hussain
Medicine, Federal University of Ceara (UFC), Ceara, Brazil
National Diabetes, Obesity and Cholesterol Foundation, New Delhi, India
Anoop Misra
Diabetes Foundation (India), New Delhi, India
You can also search for this author in PubMed Google Scholar
Contributions
RG and AM planned the outline of manuscript. RG reviewed the literature and wrote the manuscript. RG, AM and AH edited the manuscript.
Corresponding author
Correspondence to Anoop Misra .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Gupta, R., Hussain, A. & Misra, A. Diabetes and COVID-19: evidence, current status and unanswered research questions. Eur J Clin Nutr 74 , 864–870 (2020). https://doi.org/10.1038/s41430-020-0652-1
Download citation
Received : 19 April 2020
Revised : 23 April 2020
Accepted : 28 April 2020
Published : 13 May 2020
Issue Date : June 2020
DOI : https://doi.org/10.1038/s41430-020-0652-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
The role of sars-cov-2-mediated nf-κb activation in covid-19 patients.
- Qiaoqiao Zhou
- Gongxuan Chen
Hypertension Research (2024)
COVID-19: A novel holistic systems biology approach to predict its molecular mechanisms (in vitro) and repurpose drugs
- Marzieh Sameni
- Seyed Amir Mirmotalebisohi
- Hakimeh Zali
DARU Journal of Pharmaceutical Sciences (2023)
Interpretable machine learning analysis to identify risk factors for diabetes using the anonymous living census data of Japan
- Hiroyuki Suzuki
- Takashi Obi
Health and Technology (2023)
SELF-CARE AND QUALITY OF LIFE PEOPLE WITH TYPE 2 DIABETES DURING THE COVID-19: CROSS-SECTIONAL STUDY
- Hema Malini
- Sonia Zhahara
- Zifriyanthi Miranda Putri
Journal of Diabetes & Metabolic Disorders (2022)
Influenza co-infection associated with severity and mortality in COVID-19 patients
- Bandar Alosaimi
- Adnan Zafar
Virology Journal (2021)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

Living With Diabetes
Warning signs of diabetes, types of diabetes, type 1 vs type 2 diabetes, type 1 diabetes, type 1 diabetes causes, type 1 diabetes symptoms, is there a cure for type 1 diabetes, type 2 diabetes, type 2 diabetes treatment.

Educate teachers, school personnel and other child care providers about taking care of your child with type 1 diabetes. Download this helpful guide now.
Type 2 Diabetes is a serious condition which causes higher than normal blood sugar levels. It affects people from all social, economic, and ethnic backgrounds.
It is estimated that more than 34 million Americans have diabetes, including approximately 7 million who have the disease but have not yet been diagnosed. Worldwide, it is estimated that over 463 million people are living with some form of the disease.
Diabetes mellitus (type 2 diabetes), the medical term for the condition, occurs when the body cannot make or effectively use its own insulin, a hormone produced by special cells in the pancreas called islet (eye-let) cells. Insulin is like a key that opens the door of a cell so that food, or glucose, can enter. Without insulin, this glucose builds up in the blood and leads to starvation of the body’s cells, as well as dehydration and break down of body tissue.
There are multiple forms of diabetes. Type 2 diabetes is the most common form. Approximately 90 percent of those with diabetes have type 2. Unlike type 1 diabetes, in which all the insulin-producing cells are destroyed, people with type 2 diabetes are able to produce some of their own insulin, but their bodies are unable to use this insulin to completely control blood sugar levels. This is known as insulin resistance.
Who gets type 2 diabetes?
Type 2 diabetes usually develops after the age of 35, although it can occur in younger people as well, especially if they are overweight and have a sedentary lifestyle.
Commonly referred to as “adult onset” diabetes, 80% of those with this form of diabetes are overweight and have a family history of type 2 diabetes.
Certain ethnic groups have a higher risk of developing this form of the disease, including African Americans, Hispanics and American Indians. In addition, women who had diabetes during pregnancy (gestational diabetes) are also at greater risk of developing type 2 diabetes later in life.
What are the symptoms of type 2 diabetes?
Knowing the warning signs of type 2 diabetes is helpful for early diagnosis. Symptoms can include:
- Increased thirst
- Increased urination
- Unexplained weight loss
- Extreme hunger
- Extreme weakness or fatigue
- Blurred vision
- Infections which are slow or difficult to heal
The symptoms of type 2 diabetes usually happen over time, unlike the symptoms of type 1 diabetes which are sudden and often too severe to overlook. That’s why many people mistakenly overlook the warning signs of type 2, and often think the symptoms are signs of other conditions, such as aging, overworking, or hot weather. Because these symptoms are often ignored, it is estimated that more than seven million people in the United States have diabetes and are not aware of it.
Individuals who have undiagnosed or untreated diabetes for several years may develop some complications, such as nerve damage, pain or numbness in their hands and feet, or changes in their eyes or kidneys. People who are over 35, overweight, have a family history of diabetes, or who belong to a high-risk group should be checked at least once a year to detect diabetes at its earliest stages.
What is the treatment for type 2 diabetes?
The treatment for type 2 diabetes focuses on improving the person’s ability to more effectively use the insulin his/her own body produces to normalize blood sugar levels. A treatment program including diet, exercise, and weight loss will help decrease insulin resistance and, in turn, lower blood sugar levels. If blood sugar levels are still high, there are many medications which can help to either stimulate more insulin production in the pancreas or help the body better use the insulin it makes. Insulin injections may be needed if these oral medications, along with diet and exercise, do not lower blood sugar levels enough.
What are the problems associated with type 2 diabetes?
New advances in research and treatment methods are helping people with type 2 diabetes live full, active and healthy lives. However, it is important to remember that diabetes is a serious, chronic condition with potential short-term and long-term complications. Frequent self-monitoring of blood sugar levels and carefully following an individualized meal and exercise program is a good course of action.
People with undiagnosed, untreated or long-term diabetes are at risk of developing complications, including nerve and blood vessel damage. These potential complications, which can affect the eyes, kidneys, limbs, heart, brain, and stomach, may occur after many years of living with diabetes. Early detection, improved medications, and new technologies may help prevent or minimize diabetes-related complications.
Can type 2 diabetes be prevented?
The key to success is in preventing pre-diabetes and type 2 diabetes. Identifying risk means asking yourself the following key questions:
- Am I aged 35 years or older?
- Am I overweight?
- Do I have high blood pressure or cholesterol?
- Do I have a family history of diabetes?
- Am I African American, Hispanic, American Indian or Asian?
- Do I have a history of diabetes occurring during pregnancy?
- Did I deliver a baby weighing more than 9 pounds?
If you answered “yes” to any of these questions, then you should make an appointment with your physician to be screened. To lower your risk of pre-diabetes and type 2 diabetes try the following:
- Look for opportunities to move more during the day
- Exercise 30 minutes at least five times per week
- Eat a healthy meal plan including grains, cereals, fresh fruit and vegetables, low fat dairy and lean meat
- Reduce fat intake
- Reduce food portions
- Maintain an ideal body weight

Get more answers to your questions about type 1 diabetes, type 2 diabetes and gestational diabetes symptoms and treatments. (In Spanish: ¿Que es La Diabetes?).

Educate teachers, school personnel and other child care providers about taking care of your child with type 1 diabetes.

Get news about research toward a cure, diabetes management tips, information for parents of children with type 1 diabetes and more. Sign up and become a DRI Insider today!
Keep Up With Our Progress Toward A Cure & More

Many type 2 diabetes patients lack potentially lifesaving knowledge about their disease, researchers find
T he body's inability to produce enough insulin or use it effectively often results in type 2 diabetes (T2D), a chronic disease affecting hundreds of millions of people around the globe. Disease management is crucial to avoid negative long-term outcomes, such as limb amputation or heart disease. To counteract adverse consequences, it is crucial that patients have good knowledge about the day-to-day management of the disease.
A team of researchers in Portugal has now assessed how many patients—both insulin-treated and not insulin-treated—have this crucial knowledge about T2D. They published their findings in Frontiers in Public Health .
"Our main motivation was to contribute to the reduction of the existing disparity in the knowledge that diabetic patients have regarding their disease," said first author Prof. Pedro Lopes Ferreira, director of the Center for Health Studies and Research of the University of Coimbra. "With this study we evidenced the need to improve the disease knowledge of type 2 diabetic patients."
Knowledge levels vary widely
To assess diabetes knowledge, the researchers used a knowledge test developed for people with type 1 or type 2 diabetes. Among other questions, the test includes sections about nutrition, signs and symptoms, and medication control. A total of 1,200 people with diabetes participated in the study, of whom almost 40% were insulin-treated. The rest of the sample adhered to specific diets with some of them additionally taking non-insulin oral antidiabetics, while others relied on diet alone.
The results showed that many participants (71.3%) could answer food-related questions correctly, and that more than four out of five respondents demonstrated good knowledge of the positive impact of physical activity. More than 75% of respondents also knew about the best method for testing blood sugar levels.
In other areas, however, the researchers found that knowledge was severely lacking. For example, when asked which food item should not be used to treat low blood sugar levels, only 12.8% of participants answered correctly. The lowest percentage (4.4%) of correct answers was on a question concerning the symptoms of ketoacidosis, a potentially life-threatening, late-stage T2D complication.
"One of the main reasons for this disparity in knowledge is probably the behavior of health professionals and the areas that are prioritized when informing patients," Lopes Ferreira explained.
Equipping patients with knowledge
The researchers found that the use of medication was one factor that impacted T2D knowledge. The percentage of correct answers was 51.8% for non-insulin treated patients, and 58.7% for patients using insulin. Looking at socioeconomic and demographic factors, being younger than 65 years, having a higher education, not living alone, and following a specific diet had a positive impact on disease knowledge.
The researchers said that their results highlight the need to improve T2D knowledge about certain aspects of the disease, for example blood sugar monitoring, which can help to avoid spikes in blood sugar levels that are associated with acute and chronic complications. Knowledge gaps within individual sections of the test are also something that needs to be addressed urgently, the team pointed out.
They also stated that studies with even more participants could help to better understand the role of the socioeconomic and clinical determinants of the disease.
"We focused on patients' own knowledge of their disease, rather than disease management being based solely on biological indicators. We hope that the results obtained will allow professionals to change the way they inform patients," Lopes Ferreira concluded.
More information: Knowledge about type 2 diabetes: its impact for future management, Frontiers in Public Health (2024). DOI: 10.3389/fpubh.2024.1328001
Provided by Frontiers

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Equity Health

‘Learning to shape life’ – a qualitative study on the challenges posed by a diagnosis of diabetes mellitus type 2
Astrid fink.
Martin-Luther-University Halle-Wittenberg, Medical Faculty, Institute of Medical Sociology, Magdeburger Str. 8, 06112 Halle (Saale), Germany
Eva-Maria Fach
Sara lena schröder, associated data.
The datasets generated and/or analysed during the current study are not publicly available because we have ruled out data transfer to the participants.
Diabetes mellitus type 2 is a central challenge for health policy and healthcare in all advanced countries. For the affected persons, living with a diagnosis of type 2 diabetes is difficult because the disease and its treatment have a considerable effect on daily life. The aim of this study was to investigate the challenges associated with a diagnosis of type 2 diabetes for those affected and the range, depth and complexities of the subjective perspectives of the patients under the conditions of the German healthcare system.
A cross-sectional qualitative study was conducted using a sample of 19 adult patients with type 2 diabetes mellitus. Patients were recruited successively from two specialized diabetological practices, three general practitioner’s offices, and two hospitals. The patients were interviewed once in person using semi-structured interviews. All interviews were recorded, transcribed, and analysed based on grounded theory.
Persons affected by diabetes mellitus type 2 seem to feel responsible for managing their disease. Two strategies of action could be identified: 1) patients strictly followed the recommendations of the physicians, or 2) they showed that they are knowledgably managing their diabetes mellitus type 2. The action strategy to address the disease seemed to be influenced by patients’ confidence in themselves, the effectiveness of the interventions, or the patients’ locus of control. Minor differences in educational status could be discovered, and patients who were less educated tended to follow the recommendations of the physicians very strictly and seemed to place more emphasis on being compliant, which goes hand in hand with a life with prohibitions and restrictions. In contrast, being perceived as competent patients who make their own rules to manage the disease in daily life appeared to be more important for people with higher education levels.
Patient education and self-management programmes for diabetes mellitus type 2 should take different types of learners into account. Giving less-educated patients specific recommendations for successful diabetes self-management is particularly important.
Trial registration
German clinical trial register (DRKS-ID: DRKS00007847 ).
Electronic supplementary material
The online version of this article (10.1186/s12939-019-0924-3) contains supplementary material, which is available to authorized users.
Diabetes mellitus type 2 (T2DM) is a central challenge for health policy and healthcare in Germany and other advanced countries [ 1 , 2 ]. This fact is first attributable to the frequency of the disease: the Diabetes Atlas of the International Diabetes Federation (IDF) estimated that the global prevalence of diabetes mellitus among adults aged 20–79 years was approximately 8.8% (CI 95 7.2–11.3%) in 2017 with a rate of 6.8% in European countries and 11.0% in North American and Caribbean regions. Of these diabetes cases, 90% were classified as type 2 diabetes [ 3 ]. In Germany, the prevalence of T2DM could be estimated at 7 to 8.6% of adults on the basis of population-related surveys and billing data from individual health insurance funds. The results varied depending on the age group studied and the database used [ 2 , 4 ]. Second, the special significance of the disease is also due to the increased mortality from the disease. The proportion of people who died from diabetes in 2017 before the age of 60 was 32.9% in European countries and 45% in Northern America or Caribbean regions. The age and sex standardized mortality rate ratio among persons aged 45 years or older was 1.82 (CI 95% 1.45 to 2.28) for T2DM in Germany [ 5 ]. In addition to the challenges posed to the healthcare system, living with a diagnosis of T2DM is difficult. T2DM is a chronic condition that has a considerable effect on daily life. On the one hand, affected persons should implement the lifestyle modifications and if necessary, drug treatment, that the physician has recommended to them. On the other hand, people who have been diagnosed with T2DM have to take personal responsibility for managing the illness, and they have to find a responsible way to live with it [ 6 , 7 ]. To live with the disease and avoid complications, which can be life threatening, people with T2DM need to learn self-management techniques and complex care activities [ 6 – 9 ]. In addition to these challenges, it is sometimes aggravating that patients receive misinformation from friends, relatives, and the media/internet on how to best manage diabetes [ 10 ].
Cross-disease self-management can be understood as a patient’s ability to address the symptoms, treatment, physical and psychosocial consequences, and lifestyle changes associated with a chronic disease [ 11 , 12 ]. Self-management is considered to be of central importance in the treatment of T2DM [ 13 , 14 ]. Diabetes self-management encompasses all activities where patients are involved in caring for their disease, promoting health, expanding their physical, social and emotional resources and preventing the long- and short-term effects of diabetes [ 14 ]. Specifically, this management includes healthy eating and physical activity, sustainable weight loss, foot care, and knowledge of glycaemic control. Some of these techniques depend on the form of individual therapy and the body mass index of the affected person [ 6 , 7 , 15 ]. These tasks show that a diagnosis of T2DM suddenly confronts a patient’s life with additional challenges of routines and everyday actions. Patients’ perspectives on the self-management of T2DM were presented in a meta-syntheses by Gomersall et al. 2011 [ 13 ]. The authors concluded that the development of diabetes-related experiences are dependent on social and political conditions and that diabetes care should pay attention to the internal world of persons with T2DM.
Structured patient education and self-management programmes are available for learning self-management. National and international expert associations recommend making structured diabetes education accessible to all persons with T2DM [ 16 – 18 ]. The training courses are aiming at patient empowerment, i.e., those affected learn to actively influence the course of diabetes by acquiring knowledge about health-promoting behaviours such as healthy nutrition, exercise and cardiovascular risk factors. This knowledge should lead to the successful implementation of diabetes-specific therapy requirements in everyday life [ 6 , 17 , 19 , 20 ]. In addition, people with T2DM gain knowledge about secondary illnesses as well as the ability to recognize signs of complications (e.g., self-examination of the feet for early detection of diabetic foot syndrome). Structured and quality-assured patient education training is an internationally recognized measure with proven positive effects on parameters relevant to therapy such as blood sugar, glycated haemoglobin A1c (HbA1c) [ 21 – 24 ], blood pressure and body weight [ 6 , 9 , 25 ], as well as indicators of good quality of care, e.g., the frequency of screening for diabetic retinopathy [ 22 , 25 ]. Several systematic reviews examining the effectiveness of self-management programmes found robust data demonstrating the effectiveness of these programmes evidenced by a statistically significant decrease in HbA1c levels [ 26 ]; HbA1c, fasting blood glucose, body weight, waist circumference, triglyceride levels and diabetes knowledge [ 27 ]; and HbA1c, diabetes knowledge, and self-care practices with short-term to long-term follow-ups [ 28 ].
Evidence indicates that persons with low socioeconomic status (a composite measure of an individual’s economic and sociological standing in relation to others) and T2DM have more barriers to diabetes self-management that are less pronounced [ 29 , 30 ] and that they participate less frequently in diabetes education programmes [ 31 , 32 ]. Furthermore, low individual socioeconomic status or residential area deprivation is often associated with worse process indicators and worse intermediate outcomes [ 33 , 34 ]. The prevalence of T2DM in population groups with low socioeconomic status is also higher [ 35 – 37 ], and thus, these groups are often doubly disadvantaged (higher prevalence of T2DM and worse course of disease). These socioeconomic differences in treatment and the demand for considering diabetes care within the context of every patient [ 13 ] lead to the conclusion that diabetes-related experiences should be considered to be dependent on social conditions as well as on the specific features of the healthcare system [ 13 ]. Diabetes care should, as already noted, pay attention to the “inner” world of persons affected by T2DM.
To the best of our knowledge, no qualitative study in Germany has yet investigated the challenges associated with the diagnosis of T2DM for those affected and the range, depth and complexities of the subjective perspectives. To address these issues, a qualitative health care study was conducted from the patients’ point of view. Through analysing the patients’ experiences with their chronic disease and with treatment, this study aimed first, to explore and understand the challenges associated with a diagnosis of T2DM and how people adjust to the diagnosis and incorporate it into their lives under the conditions of the German healthcare system and second, to assess whether there were differences in patient experiences according to the different educational backgrounds of the participants, as the state of research suggests.
Material and methods
Study design.
This exploratory qualitative study was based on the elements of grounded theory [ 38 ]. This research was considered suitable for capturing the subjective experiences of persons with T2DM within their social and cultural contexts and reviewing these experiences to arrive at an understanding of individuals’ perceptions of the disease and their adjustment to the diagnosis. The study was conducted as a single-centre, cross-sectional qualitative study in Halle/Saale, Saxony-Anhalt, Germany, a high-risk area for T2DM morbidity [ 39 ].
Research team
Interviews were conducted by three female members of the team (AB, AF, EMF), who were researchers at the Institute of Medical Sociology. AB is a young medical anthropologist, and AF and EMF are experienced medical sociologists (AF: PhD in rehabilitation medicine and EMF: MA in sociology). All of them had undergone training in qualitative methods. Prior to her scientific career, the principal investigator (AF) worked as a dietician in healthcare, and in this capacity, she was responsible for educating patients with T2DM about nutrition. MW, a male student assistant, supported the project throughout its course.
Participant recruiting
Participants were recruited from ambulatory medical practices (three general practitioners, one of them in rural area and two urban specialists in diabetology) and two hospitals (one urban and one rural). The inclusion criteria for participating in the study were 1) being 18 years and over; 2) having a diagnosis of T2DM; and 3) being able to speak and understand German. Two sampling methods were combined to use the strengths of the respective methods [ 40 ]. In keeping with the principles of theoretical sampling, the participants were recruited successively during alternating phases of data collection, development of theoretical categories and additional data collection [ 38 ]. Depending on the state of category and theory development, a decision was made by the team about which person should be interviewed next. Socioeconomic inequalities in prevalence, secondary diseases and mortality of T2DM are known to negatively affect socially disadvantaged individuals [ 35 , 41 – 45 ], and persons with low socioeconomic status participate less frequently in studies [ 46 ]. Therefore, a qualitative sampling plan was additionally used to ensure that men and women from different socioeconomic groups would be represented. We decided to use education as a proxy for socioeconomic status. Participants were assigned to a group with high or low education based on their years of formal education and occupational training qualification. The classification was based on German epidemiological standards for the measurement and quantification of sociodemographic characteristics in epidemiological studies [ 47 ]. During the study, health care professionals identified eligible participants and gave brief information about the study. The patients who agreed to be contacted by the study team received a telephone call from a researcher who answered their questions and scheduled the interviews. Nineteen adult patients with T2DM participated in the study between July 2015 and June 2016, at which point theoretical saturation was reached. Because the first screening was held in doctors’ offices or hospitals, no statements can be made about patients refusing to participate.
Participants
Nineteen patients were interviewed: 7 women and 12 men. They ranged in age from 47 to 87 years, and all were of German nationality. Their characteristics are summarized in Table 1 .
Patients’ characteristics ( n = 19)
Data collection
The interviews were conducted face-to-face in a private, quiet room in the hospital, an office at the university or the participant’s home. They lasted 25–80 min and were audiotaped with the interviewees’ permission. No repeat interviews were conducted. Prior to the interview, participants were given an information sheet and a verbal explanation of the study and were encouraged to ask any questions. Then, the participants provided written informed consent. Interviews were semi-structured around a topic guide and included narrative-generating questions on the history and treatment of diabetes and its impact on daily life.
The topic guide was tested with four persons with T2DM. The purpose of the pre-test was to examine whether narratives were created and to elicit the participants’ reactions to the questions. The topic guide was revised after the pre-test and throughout the study, following the iterative process of data collection and analysis of grounded theory. To gather the participants’ sociodemographic data, questions about age, sex, nationality, marital status, education, professional qualifications, and occupation were raised subsequent to the interview. A situation report was prepared for each interview, and first memos were recorded after the conversation.
Data analysis
A transcription agency transcribed the recordings verbatim. Pseudonyms were used to protect personal data. We used MAXQDA software for data management and analyses. We followed grounded theory analysis [ 48 ]. Open coding of the data began with the first two authors. The data were broken down into discrete parts, examined and compared for similarities and differences, and then clarified in discussions of prominent themes that had emerged. The transcripts were analysed by being coded into categories, which were then reduced by pattern coding (grouping categories into conceptual sets). The axial coding procedure was structured by Strauss and Corbin’s coding paradigm. Aspects of this paradigm are the causal conditions that lead to the phenomenon, the attributes of the context of the phenomenon, additional intervening conditions, action strategies to handle the phenomenon and the consequences of actions. This procedure led to carefully elaborated categories from which the theory is formulated in the course of selective coding. All authors (AF, MW, and AMF) iteratively conducted open and axial coding, and the principal investigator (AF) conducted selective coding by using abductive reasoning. The development and final application were discussed by the research team and in additional interpretation workshops. The phenomena were derived from the data and not determined in advance. Internal quality and credibility were attained by having three researchers independently code the data and by obtaining consensus through analysis and in discussions at additional interpretation workshops. A professional translation agency translated the passages from the interviews cited in this paper.
Ethics and patients’ consent
Full ethical approval for the study was granted by the Ethical Review Committee of the Medical Faculty at Martin-Luther-University, Halle-Wittenberg. Participation was voluntary, and participants were informed that they could withdraw from the study at any point without giving reasons. They were also informed that the data would be pseudonymized and that the results might be published in a scientific journal. All participants gave written informed consent prior to the interview.
Through exploring the patients’ experiences with their chronic disease, T2DM, and with treatment, we found that the focus was on how to cope with the disease in everyday life and how to adapt the life. In this result section, we first describe the path of “learning to shape life” (our developed model, Fig. 1 ) and then show small differences in adaptations in people with different education levels.

Categories and their connections of “learning to shape life”
Diabetes mellitus type 2 affected both professional and private life. A central challenge for persons who received a diagnosis of T2DM seemed to be the management of the disease in daily living. In addition to adjustments in professional and private life, people needed to learn a great deal about self-care activities related to disease management. These included adapting one’s lifestyle in terms of physical activity and nutrition as well as the use of medication. The patient managed the adaptation well if he or she had sufficient knowledge about the disease, secondary diseases and measures to influence the disease. The professional health care system remained on the theoretical level in dealing with the disease, whereas the affected person was responsible for the implementation. This process of learning to shape life was the central phenomenon drawn from the narratives of the participants interviewed.
The main reason for “learning to shape life” seemed to be “accepting the challenge of the disease”. People with T2DM seemed to feel responsible for managing their disease. This feeling may have been influenced by the contextual aspects “conditions and types of shaping” . The action strategy of patients with T2DM could be influenced by the core phenomenon and by their own “confidence in the action” (intervening condition). This confidence seemed to be determined by the patients’ confidence in themselves, the effectiveness of interventions, or the patients’ locus of control. The two action strategies can be described as follows: 1) patients very strictly followed the recommendations of the physicians, or 2) they showed that they were knowledgably managing their T2DM. The consequence of the action strategies and learning to shape life could result in “acceptance and life with the disease” . As a chronic disease that is not always stable, T2DM requires adjustments. For this reason, the model of the path from the consequence “acceptance and life with the disease” is drawn back to the “accepting the challenge of the disease”. The categories and their connections are shown in Fig. Fig.1, 1 , the derivation of the categories in Additional file 1 .
“Learning to shape life”
During the analysis, “learning to shape life” emerged from the interviews as the core phenomenon (story line). Learning how to shape one’s life is an ongoing process. With changes in illness or life situations, new situations arise to which one must react, so that the process may never be completed.
Because it’s not just diabetes, it’s also going into the professional and private spheres, because such diabetes doesn’t, as they say so nicely, allow life to be so pronounced, but changes the body and everything. Yes, that’s not from eating habits, it goes all the way to, let’s say, even sexual. That’s all connected with it. (Participant 6, male, 50 years old).
So and then I had a job with a security company, also a *security company, there I had to supervise alone night shifts 12 h things. And where they found out about diabetes and so on, they said, the doctor said it already, so: “For God’s sake, you’re not in a position, to do that”. […] I also have, as I said, great difficulties with the job centre there a suitable job again, because you want to get back into work, but there are great problems, because there are so great restrictions from the doctor. (Participant 15, male, 60 years old).
Well, but that’s just one of those areas where I say, yes, on the one hand I know physical activities, food and so on. And the/The ball, I always have the feeling, the ball is with me, I would have to do something there, but really then just to play the ball again, there are a bit of difficulties. But I don’t think that’s necessarily a question for the practice or the doctors now, but that’s also the case, maybe also a little bit, I see it a little bit as a personal matter, where I say I’m on the radar. (Participant 3, male, 50 years old).
Accepting the challenge of the disease, conditions and types of shaping
The causal condition of learning to shape one’s life seemed to be accepting the challenge that the disease brings to the person who has received the diagnosis.
“Yes, Dr. Martin put it simply then: ‘First we try with tablets, and if they don’t work and it gets worse, you’ll have to inject.’ That was a clear warning which made me pay attention.” (Participant 13, male, 72 years old)
“I take note of that and say: Well, then you have to stick to it. I felt that way then, your mother had it now, you have it now too. Well, that/yes, I have this/I did not panic or something and thought: You have to! I just took note of that.” (Participant 9, female, 80 years old)
We found that there was a learning process to shaping one’s life to adjust to T2DM. This contextual factor raised questions about the conditions and types of such shaping. What motivations were there for learning? What encouraged learning? What hindered it? In the narratives of our participants, we found two different motivations for accepting the challenges of the disease. One of the motivations was linked to the negative emotion of fear, namely, “learning out of fear”. The other motivation was associated with an optimistic point of view, namely, “learning to keep going”. Fear seemed to be a motivator for learning and adaptation. Many of our participants had a family history of diabetes mellitus, and they reported that when they were diagnosed, they immediately thought something such as diabetes put my mother in a wheelchair (participant 6, 50 years old) and I do not want that, so I have to do something (participant 16, male, 47 years old). Fear affected several aspects in our model. First, it affected the causal condition “accepting the challenge of the disease” . Second, fear could be considered an intervening or maintaining condition. Finally, fear could be considered as a context because the patient’s knowledge of the disease affected his or her actions. Our participants expressed fears of an increase in therapy, secondary diseases, loss of independence, or loss of social ties.
“And that is the problem that I get such problems with the legs by the sugar because the experience I had to make through my mother, who was also diabetic, for almost over 30 years and ended up in a wheelchair. I don’t want to go there.” (Participant 6, male, 50 years old)
“So, thank God, I do not need to inject. I also hope that I will not have to.” (Participant 1, female, 76 years old)
The issue we describe as “learning to keep going” focused on having as few restrictions as possible through good disease management. To manage their disease, persons affected by T2DM needed knowledge from their doctors or specialists or from self-education.
“As I just said, you get yourself some material. And get some reading material from the doctors, which they provided me. And I read everything myself, and then tried to do as it said.” (Participant 4, male, 73 years old)
“So, my general practitioner has explained to me, what influence for example my diet or physical activity has on the diabetes and the interactions, what happens in the body with the blood glucose and how can it be regulated with the medicines.” (Participant 16, male, 47 years old)
Our participants described very different barriers to learning. A great deal of individual initiative seemed to be required, and patients did not necessarily perceive their health insurance companies as supportive. Another barrier to learning seemed to be scheduling times and dates for patient education and training. Working people, in particular, described problems arranging regular training sessions, which were frequently held in the afternoon. Training seemed to be time consuming and related to the amount of time required for care, such as regular check-ups with T2DM and other specialists, meal preparation and physical activity.
“Not at all, that's all personal interest and commitment.” (Participant 18, female, 60 years old)
“The course with the specialist doctor wasn't bad, either, but because of work I could only go every 14 days. So I missed half of it.” (Participant 16, male, 47 years old)
Participants seemed to perceive an insufficient number of blood glucose measuring strips as a significant barrier to learning. Most of our participants possessed a glucometer supplied by their doctor. Regular self-monitoring for insulin treatment was standard practice, but some participants reported monitoring more often than doctors recommended or considered necessary. This additional measurement was often not compatible with the number of measuring strips supplied by doctors for self-monitoring, and the cost of measuring strips could influence these patients’ approaches to treatment. The problem seemed to be even more serious for patients who had received a glucometer but whose oral antidiabetic therapy did not provide self-monitoring of blood glucose. The effects of physical activity or certain foods seemed to be difficult to interpret for these patients, and they reported feeling not well informed about their condition; indeed, some seemed to suffer from this loss of control. These persons felt hindered in learning because they could not determine and interpret their blood glucose levels as fully as they wished.
“No, no, that's because of the not very cheap measuring strips in there, that is. So, I do it at certain times when I think again, how was it today or something, but just not regularly.” (Participant 3, male, 49 years old)
“You get a month, no, in a quarter by 50 pieces. And if you buy strips, then each pack is about 25 euros, yes? This is natural, of course, that is much money, of course. So, I always try to get measuring strips somewhere else.” (Participant 7, male, 56 years old)
Implementation process: “Follow recommendations very strictly” – “Free design as a competent patient”
In the narratives of our participants, we identified two courses of action. One course seemed to be following the daily recommendations to the letter. The patients who did this seemed to have the highest regard for the authority of their physicians. These participants explained in detail how they have changed their lifestyle and how they have implemented the therapeutic requirements even though the result was a “life with prohibitions”, in which they saw more limitations than possibilities.
“And here I eat cucumber, tomato, what I've grown in the garden myself, or lettuce, and actually it agrees with me, I'm managing well.” (Participant 1, female, 76 years old)
“And I have to discipline myself a bit, too, although it's hard, I admit.” (Participant 9, female, 80 years old)
The other course of action seemed to be more flexible. These participants could be described as persons who did not want their T2DM to take over their lives, so they set their own rules and goals and tried to compensate for doing something that was not recommended. Even in training sessions, they thought about the means that they would and would not implement.
“No, no, no, no, no, that makes even less sense, if you can't enjoy life anymore.” (Participant 12, male, 71 years old)
“I eat too, I really enjoy a piece of cake, and I used to [laughs] always have one on hand. And then you could compensate for it, for instance, by eating less in the evening or injecting more. But I did, what I could and I've always had everything under control.” (Participant 11, male, 64 years old)
Both groups reported the same perception of check-ups. This time-consuming commitment seemed to be positive for patients because these check-ups could give them the certainty that nothing was wrong, and this assurance could be reassuring for patients who learn from fear and possibly relieve their anxiety. However, patients who interpret their actions more freely reported benefits from this confirmation as well.
“Confidence in the action”
The action strategies “Follow recommendations very strictly” versus “Free design as a competent patient” seemed to be influenced either by patients’ confidence in themselves or the effectiveness of the interventions. On the one hand, some patients seemed to have a stronger external locus of control and prefer to blame genetics or external circumstances for their T2DM. These participants claimed that they were not always successful at disease management despite their efforts and that the measures that they learned did not necessarily work.
“I inherited it too, the whole thing.” (Participant 17, male, 56 years old)
“And you see how the sugar goes mad sometimes.” (Participant 15, male, 50 years old)
“He [the doctor] also sees that he gets the diabetes or the sugar down now.” (Participant 8, female, 64 years old)
On the other hand, some patients seemed to have a high internal locus of control and a high expectation of self-efficacy. These persons described taking some leeway in managing their T2DM to maintain their quality of life.
“I am, and have, actually been able to deal with the diabetes well so far, without my/ It's not restricted me in any way, right? I've been able to join in all the parties and everything, and also to go abroad, it's all gone well, because everything was under control.” (Participant 11, male, 64 years old)
“I see that you may be able get around it here and there, but how you can manage it properly, that I just don't/ But I define it rather, and I take responsibility for it, so I say: yes, it's a fact.” (Participant 3, male, 49 years old)
“Acceptance and living with the disease”
The effects of the different learning processes and the actions or strategies that the participant developed could be described as “acceptance and living with the disease”. Ideally, persons affected by T2DM acquired sufficient self-management skills or could interpret these skills and were not severely restricted by their illness. These ideal conditions did not apply to all patients; information and knowledge alone did not induce changes in behaviour. In some cases, the learning process seemed to be delayed, especially for people who could not attend training sessions because of work and those whose management of their lifestyle and therapy had to accommodate their schedules. Patients also reported feeling unable to control the disease if they could not monitor it themselves, e.g., their form of treatment did not allow for self-monitoring so they have to buy their own blood glucose strips. Some of our participants could not afford them and seemed to feel guilty about not being able to monitor their blood glucose. The inability to monitor may have been associated with uncertainty and dissatisfaction.
Educational inequalities in the results
In our study, we observed two courses of action: “follow recommendations very strictly” and “free design as a competent patient”. Furthermore, minor differences in educational status could be observed. Patients who were less educated tended to place more emphasis on being compliant, which goes hand in hand with a life with prohibitions and restrictions. In contrast, being perceived as competent patients who imparted more freedom to their lives and disease management appeared to be more important for people with higher education levels. The differences between the two courses concerned the implementation of new daily routines. Patients with less education described their new routines in detail, placing more emphasis on complying with the restrictions and prohibitions, and seemed to value the authority of their physicians. In contrast, well-educated people with T2DM seemed to want to be perceived by the research team as knowledgeable in daily life and in their interaction with the physicians. At the same time, the locus of control showed minute differences. Predominantly well-educated persons with a high internal locus of control and a high expectation of self-efficacy were found to take some leeway in managing their diabetes to maintain their quality of life.
The results presented here were from a study drawing attention to the perspectives of persons with T2DM in different care settings and considered the patient experience in Germany’s healthcare system. We gained insight into the different experiences of the disease, especially the perceived challenges in adapting to a diagnosis of T2DM.
In our study, adaptation of the previous lifestyle to a life with disease seemed to be central to the disease experience of persons with T2DM. Two possible ways of accepting the challenge of the adaptation processes dominated: 1. learning from fear and 2. learning such that life goes on well. These different motivations were associated with different emotions. Learning from fear was based on negative emotions, while learning was based on a positive, optimistic mood. Even though the relationship between learning and emotions does not seem as simple as positive emotions result in learning well and negative emotions result in learning badly [ 49 , 50 ], some evidence indicated that positive affective processes underlie positive health behaviour change [ 51 ] and may beneficial in most cases [ 49 ]. Furthermore, two implementation processes were observed. One group described itself as very faithful to therapy and strictly adhered to the implementation of the expert recommendations in their daily living. These patients seemed to be more strongly tied to the authority of their physicians. The second group tried to deal more autonomously with T2DM and lead a responsible but well-organized life with the disease. Both groups seemed to be linked to different attribution styles; the first group tended to have a more external attribution style, whereas the second group had an internal style. The resulting lifestyles differed in that the group with external attribution styles had a life with rules and prohibitions. However, the persons with an internal attribution style had lives in which they felt less restricted by the disease and reported fewer perceived limitations in quality of life.
In 2008, Funnel and Anderson described the change in diabetes therapy from compliance to the self-management model [ 14 ]. In our study, the patient group with a lower level of education strongly emphasized their compliance, and the narratives from the patients indicated that some did not fully understand the opportunities and challenges of self-management. With patients following recommendations so strictly, living with diabetes meant a greater limitation for them than for patients who managed their disease more freely. Whether patients who value compliance did not accept the self-management model or whether it was not offered to them by the doctor remained unclear. Evidence has shown that people with low health literacy were perceived by healthcare professionals as uninvolved and less motivated, as well as having less understanding of self-management [ 12 ]. On the basis of our study, we could not determine whether self-reported compliance actually led to good disease management behaviour or whether there were discrepancies with self-perception. The literature showed that secondary diseases and poorer process parameters were more frequently found in socially disadvantaged groups with lower socioeconomic status [ 33 , 35 , 52 , 53 ], so that an effective health behaviour could not be assumed in principle.
The inductive approach brought the study result strongly towards self-management. However, not all dimensions that were categorized as self-management were reported by patients, making it difficult to classify these results into the extensive literature on self-management [ 6 , 14 , 26 , 54 ]. When reporting on their experiences with T2DM and its treatment, patients seemed to place great importance on several components of self-management as they built the core phenome of their viewpoints. These components were physical exercise, blood glucose self-monitoring, and diet. However, other aspects of self-management, such as weight monitoring, foot care, and keeping a diabetes diary, were not mentioned. The stronger emphasis on diet, blood glucose monitoring and physical activity can also be found in other studies [ 55 , 56 ]. These themes may simply be more closely linked to diabetes treatment for patients than, for example, foot care, and these issues may also be frequently discussed with doctors, families and the public. These reasons may explain why diet, physical exercise, blood glucose self-monitoring were so much in the focus of our participants. Looking more closely at the other topics (weight monitoring, foot care, and keeping a diabetes diary) and reinforcing their importance in training and consulting may be necessary.
Professional associations recommend that all persons with T2DM participate in structured patient education [ 15 – 18 ]. However, not every person with T2DM actually takes part in patient education training [ 57 – 59 ]. In our study, almost all patients reported earlier participation in training. However, the findings were interpreted and implemented in different ways. The learning processes for managing the disease proceeded very differently [ 8 , 60 ]. The learning needs suggested that diverse social groups cope with T2DM differently and experience diabetes in various ways. Assessing how patient education addresses the different types of learning and whether all patients benefit equally from the training might be interesting.
In addition, the delivery of glucometers to patients who were not treated with insulin should be critically considered. The patient may assume that blood glucose monitoring is an important part of diabetes self-management. Although this practice is not consistent with medical guidelines, patients may think that they are not being treated adequately if they are not given testing strips, which may have tainted their perception of the medical care that they have received. To this end, there have been changes in the German healthcare system since we carried out our study. Glucometers are no longer supplied free of charge, although whether and in what form this action supports patient is currently still open.
Even though the research team performed the study with great care, the study has some limitations. First, we recruited patients only from Central Germany, in particular Halle/Saale and the surrounding area. Patients in other regions might have other experiences if the supply situation is different. Another limitation is that we did not have participants who had migrated from other countries. The proportion of immigrants in our region is not as high as that found elsewhere, especially in what was formerly West Germany, and we did not encounter them in the recruitment phase. However, as cultural factors seem to be a separate theme in immigrants’ health service utilization [ 61 ], we did not specifically look for immigrants in sampling. The third limitation is that due to the first screening in the doctors’ offices or hospitals, no statements can be made about patients refusing to participate. Our project was designed to explore the patient’s perspective, which also included the importance of family behaviour, the wider social environment and caregivers for dealing with the disease from the patient’s perspective. Due to the project planning, these important reference groups could not be specifically asked what constitutes a further limitation and will be addressed in subsequent projects. Lastly, we performed all steps of the grounded theory thoroughly. However, the process led us to results that give insight into different experiences of the disease, especially perceived challenges in adapting to the diagnosis of T2DM, even if we had not addressed the question so concretely. Nonetheless, the results described were obtained in a rigorous manner.
The persons affected by T2DM who participated in our study seemed to have accepted the need for education and utilized the training offered by the T2DM management programmes. Different types of learning were associated with disparities in education. However, working people should have better access to T2DM education, and the needs of patients with lower educational levels should be considered. Different forms of structured diabetes training, which also take into account the conditions of modern life, are urgently needed in Germany. Further studies should analyse and evaluate patient education and apply it to different types of learners. Specific recommendations on T2DM self-management for patients with less education are necessary. The identification of different learning styles could clarify the association between socioeconomic and healthcare disparities. Some patients seemed to feel incapable of controlling their T2DM if they did not have glucose measuring strips. This observation requires general practitioners, specialists for diabetes, clinicians, and policy makers to ask whether those uncertainties are warranted. Should glucometers be available to everyone being treated for T2DM? These topics are important for further discussion.
Additional file
Derivation of categories. (PDF 598 kb)
Acknowledgements
The authors are grateful to all participating patients for being part of the study and for talking frankly to us about their experiences and feelings. Further, the authors thank the healthcare professionals in the doctors’ offices and hospitals for their support in recruiting the patients. Further on, the authors thank the Qualitative Methods Working Group at the Institute of Medical Sociology and the interpretation group “Grounded Theory in Central Germany”. Finally, the authors thank Amelie Baumann and Maximilian Werner for their support in the early stage of the study. We acknowledge the financial support within the funding programme Open Access Publishing by the German Research Foundation (DFG).
This work is supported by the German Research Foundation (Deutsche Forschungsgemeinschaft) as part of their third academy for early-career researchers in health services research for a period of 12 months, starting April 1, 2015, grant number FI 2057/1–1.
Availability of data and materials
Abbreviations, authors’ contributions.
AF, EMF, SLS. AF is the principal investigator and was responsible for the conception of the project, leading the grant application. She conducted interviews, analysed the data and wrote the initial draft of this manuscript. EMF recruited patients, conducted interviews, and analysed the data. SLS supported and advised the project throughout the whole process. All authors have read and approved the final version of the manuscript.
Ethics approval and consent to participate
The Ethical Review Committee of the Medical Faculty of Martin Luther University, Halle-Wittenberg approved the study (No: 2015–13). All participants gave written informed consent to participate in the study prior to the interview.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Astrid Fink, Email: [email protected] .
Eva-Maria Fach, Email: [email protected] .
Sara Lena Schröder, Email: [email protected] .

IMAGES
COMMENTS
The indicative questions formed a subsequent interim survey to which 1506 people responded and ranked their top ten questions. The top ten questions ranked by people with type 2 diabetes and carers, health-care professionals, and BAME groups were combined with equal weighting into a shortlist of 24 questions.
Type 2 diabetes mellitus has been identified as one of the most challenging chronic illnesses to manage. Since the management of diabetes is mainly accomplished by patients and families, self-management has become the mainstay of diabetes care. ... Priority research questions include asking what affects self-management in persons with diabetes ...
The chronic complications of type 2 diabetes are a major cause of mortality and disability worldwide [ 1, 2 ]. Clinical research is the main way to gain knowledge about long-term diabetic complications and reduce the burden of diabetes. This allows for designing effective programs for screening and follow-up and fine-targeted therapeutic ...
ten questions ranked by people with type 2 diabetes and carers, health-care professionals, and BAME groups were combined with equal weighting into a shortlist of 24 questions. New representatives of people with type 2 diabetes and carers, health-care professionals, and BAME groups were brought together in a final workshop
Introduction. Diabetes is a major health problem worldwide. The prevalence of global, age-standardized diabetes is 9% in men and 7.9% in women, with the number having risen around the globe from 108 million in 1980 to 422 million in 2014 [].Type 2 diabetes mellitus (T2DM) is a main driver of the increase, accounting for approximately 90% of all diabetes cases [2-4].
Type 2 diabetes mellitus, the most frequent subtype of diabetes, is a disease characterized by high levels of blood glucose (hyperglycaemia). ... Research 21 Mar 2024 European Journal of Clinical ...
Determining the role of BPA in type 2 diabetes risk. ... Dr. Mezuk had two primary research questions: (1) What is the geographic and demographic reach of the program? and (2) Is the program effective at improving diabetes management and health outcomes in participants? Over a 12-week study period, Dr. Mezuk found that there was broad ...
Type 2 diabetes is a global health problem posing substantial burdens on human health 1. The diagnosis of type 2 diabetes is based on elevated blood glucose coupled with the absence of clinical ...
Of the questions on diabetes, 152 from 101 patients were about T2DM and these questions were retained for our analysis. Although only 1 to 2 questions were asked for, 2 patients gave 3 questions each. Most of the patients attending the clinic had T2DM (95%). These questions are given in S1 File. Table 1.
Diabetes mellitus (DM) is a chronic health condition that comprises different groups of heterogeneous diseases and has an increasing global prevalence 1,2.To provide high quality care for people ...
The ADA is committed to continuing progress in the fight against type 2 diabetes by funding research, including support for potential new treatments, a better understating of genetic factors, addressing disparities, and more. For specific examples of projects currently funded by the ADA, see below. Greg J. Morton, PhD.
An Additional 12 Million US Adults Become Eligible for Diabetes Screening. New USPSTF and ADA guidelines lower the age for prediabetes and type 2 diabetes screening to 35. This study examined if testing practices aligned with guidelines and which populations were less likely to receive testing. Read the summary.
A Comparative Effectiveness Study of Major Glycemia-lowering Medications for Treatment of Type 2 Diabetes Rochester, MN. The GRADE Study is a pragmatic, unmasked clinical trial that will compare commonly used diabetes medications, when combined with metformin, on glycemia-lowering effectiveness and patient-centered outcomes.
Background: Although a large amount of research has been conducted in diabetes management, many of the articles do not focus on patient-centered questions and concerns. To address this shortcoming, patients and various other stakeholders from three northern Mississippi communities co-created research questions focused on Type 2 diabetes management.
The study was designed as a three-round modified Delphi online survey 19 aligning with that used to determine the top 10 national research priorities in type 2 diabetes in the UK. 9 20 The working group leading this research included Australian researchers, health professionals and consumers in the field of DFD ('the authors') appointed by ...
140 to 199 mg/dL (7.8 mmol/L and 11.0 mmol/L) is diagnosed as prediabetes. 200 mg/dL (11.1 mmol/L) or higher after two hours suggests diabetes. Screening. The American Diabetes Association recommends routine screening with diagnostic tests for type 2 diabetes in all adults age 35 or older and in the following groups:
Background Diabetes self-management education, a universally recommended component of diabetes care, aims to support self-management in people with type 2 diabetes. However, attendance is low (approx. 10%). Previous research investigating the reasons for low attendance have not yet linked findings to theory, making it difficult to translate findings into practice. This study explores why some ...
Glasgow RE. In: Handbook of Psychology and Diabetes: a guide to psychological measurement in diabetes research and practice. Chur BC, editor. ... 2 diabetic patients: right answer, but wrong question: self-monitoring of blood glucose can be clinically valuable for noninsulin users. ... on glycemic control and body mass in type 2 diabetes ...
Example PICO Question: Do type 2 diabetics (P) get better glycemic control (O) with exercise as the primary treatment (I) than those who get drug therapy as a primary treatment (C)? Follow these steps to form your search strategy: Identify key terms from your PICO. These terms become the foundation of your search. (P) type 2 diabetes (I) exercise
Patients with diabetes who develop COVID-19 have been seen to have a worse prognosis and increased mortality in most studies. In 201 Chinese patients with diabetes a hazard ratio of 2.34 (95% CI ...
Type 2 Diabetes is a serious condition which causes higher than normal blood sugar levels. It affects people from all social, economic, and ethnic backgrounds. ... Get more answers to your questions about type 1 diabetes, type 2 diabetes and gestational diabetes symptoms and treatments. ... 2023 Diabetes Research Institute Foundation A 501(c)(3 ...
Diabetes mellitus (DM) is a chronic metabolic disorder characterized by persistent hyperglycemia. It may be due to impaired insulin secretion, resistance to peripheral actions of insulin, or both. According to the International Diabetes Federation (IDF), approximately 415 million adults between the ages of 20 to 79 years had diabetes mellitus in 2015.[1] DM is proving to be a global public ...
To assess diabetes knowledge, the researchers used a knowledge test developed for people with type 1 or type 2 diabetes. Among other questions, the test includes sections about nutrition, signs ...
Of these diabetes cases, 90% were classified as type 2 diabetes . In Germany, the prevalence of T2DM could be estimated at 7 to 8.6% of adults on the basis of population-related surveys and billing data from individual health insurance funds. The results varied depending on the age group studied and the database used [2, 4]. Second, the special ...