
How to Write a Nursing Care Plan
Nursing care plan components, nursing care plan fundamentals.

Knowing how to write a nursing care plan is essential for nursing students and nurses. Why? Because it gives you guidance on what the patient’s main nursing problem is, why the problem exists, and how to make it better or work towards a positive end goal. In this article, we'll dig into each component to show you exactly how to write a nursing care plan.
A nursing care plan has several key components including,
- Nursing diagnosis
- Expected outcome
- Nursing interventions and rationales
Each of the five main components is essential to the overall nursing process and care plan. A properly written care plan must include these sections otherwise, it won’t make sense!
- Nursing diagnosis - A clinical judgment that helps nurses determine the plan of care for their patients
- Expected outcome - The measurable action for a patient to be achieved in a specific time frame.
- Nursing interventions and rationales - Actions to be taken to achieve expected outcomes and reasoning behind them.
- Evaluation - Determines the effectiveness of the nursing interventions and determines if expected outcomes are met within the time set.
>> Related: What is the Nursing Process?
Get 10% OFF Nursing School Study Guides From nurseinthemaking.com ! Fill out the form to get your exclusive discount.
Before writing a nursing care plan, determine the most significant problems affecting the patient. Think about medical problems but also psychosocial problems. At times, a patient's psychosocial concerns might be more pressing or even holding up discharge instead of the actual medical issues.
After making a list of problems affecting the patient and corresponding nursing diagnosis, determine which are the most important. Generally, this is done by considering the ABCs (Airway, Breathing, Circulation). However, these will not ALWAYS be the most significant or even relevant for your patient.
Step 1: Assessment
The first step in writing an organized care plan includes gathering subjective and objective nursing data . Subjective data is what the patient tells us their symptoms are, including feelings, perceptions, and concerns. Objective data is observable and measurable.
This information can come from,
Verbal statements from the patient and family
Vital signs
Blood pressure
Respirations
Temperature
Oxygen Saturation
Physical complaints
Body conditions
Head-to-toe assessment findings
Medical history
Height and weight
Intake and output
Patient feelings, concerns, perceptions
Laboratory data
Diagnostic testing
Echocardiogram
Step 2: Diagnosis
Using the information and data collected in Step 1, a nursing diagnosis is chosen that best fits the patient, the goals, and the objectives for the patient’s hospitalization.
According to North American Nursing Diagnosis Association (NANDA), defines a nursing diagnosis as “a clinical judgment about the human response to health conditions/life processes, or a vulnerability for that response, by an individual, family, group or community.”
A nursing diagnosis is based on Maslow’s Hierarchy of Needs pyramid and helps prioritize treatments. Based on the nursing diagnosis chosen, the goals to resolve the patient’s problems through nursing implementations are determined in the next step.
Get 5 FREE study guides from Simplenursing.com - fill out the form for instant access! 1. Fluid & Electrolytes study guide 2. EKG Rhythms study guide 3. Congestive Heart Failure study guide 4. Lab Values study guide 5. Metabolic Acidosis & Alkalosis study guide

By clicking download, you agree to receive email newsletters and special offers from Nurse.org & Simplenursing.com. You may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.
Your request has been received. Thanks!
There are 4 types of nursing diagnoses.
Problem-focused - Patient problem present during a nursing assessment is known as a problem-focused diagnosis
Risk - Risk factors require intervention from the nurse and healthcare team prior to a real problem developing
Health promotion - Improve the overall well-being of an individual, family, or community
Syndrome - A cluster of nursing diagnoses that occur in a pattern or can all be addressed through the same or similar nursing interventions
After determining which type of the four diagnoses you will use, start building out the nursing diagnosis statement.
The three main components of a nursing diagnosis are:
Problem and its definition - Patient’s current health problem and the nursing interventions needed to care for the patient.
Etiology or risk factors - Possible reasons for the problem or the conditions in which it developed
Defining characteristics or risk factors - Signs and symptoms that allow for applying a specific diagnostic label/used in the place of defining characteristics for risk nursing diagnosis
PROBLEM-FOCUSED DIAGNOSIS
Problem-Focused Diagnosis related to ______________________ (Related Factors) as evidenced by _________________________ (Defining Characteristics).
RISK DIAGNOSIS
The correct statement for a NANDA-I nursing diagnosis would be: Risk for _____________ as evidenced by __________________________ (Risk Factors).
Step 3: Outcomes and Planning
After determining the nursing diagnosis, it is time to create a SMART goal based on evidence-based practices. SMART is an acronym that stands for,
It is important to consider the patient’s medical diagnosis, overall condition, and all of the data collected. A medical diagnosis is made by a physician or advanced healthcare practitioner. It’s important to remember that a medical diagnosis does not change if the condition is resolved, and it remains part of the patient’s health history forever.
Examples of medical diagnosis include,
Chronic Lung Disease (CLD)
Alzheimer’s Disease
Endocarditis
Plagiocephaly
Congenital Torticollis
Chronic Kidney Disease (CKD)
It is also during this time you will consider goals for the patient and outcomes for the short and long term. These goals must be realistic and desired by the patient. For example, if a goal is for the patient to seek counseling for alcohol dependency during the hospitalization but the patient is currently detoxing and having mental distress - this might not be a realistic goal.
Step 4: Implementation
Now that the goals have been set, you must put the actions into effect to help the patient achieve the goals. While some of the actions will show immediate results (ex. giving a patient with constipation a suppository to elicit a bowel movement) others might not be seen until later on in the hospitalization.
The implementation phase means performing the nursing interventions outlined in the care plan. Interventions are classified into seven categories:
Physiological
Complex physiological
Health system interventions
Some interventions will be patient or diagnosis-specific, but there are several that are completed each shift for every patient:
Pain assessment
Position changes
Fall prevention
Providing cluster care
Infection control
Step 5: Evaluation
The fifth and final step of the nursing care plan is the evaluation phase. This is when you evaluate if the desired outcome has been met during the shift. There are three possible outcomes,
Based on the evaluation, it can determine if the goals and interventions need to be altered. Ideally, by the time of discharge, all nursing care plans, including goals should be met. Unfortunately, this is not always the case - especially if a patient is being discharged to hospice, home care, or a long-term care facility. Initially, you will find that most care plans will have ongoing goals that might be met within a few days or may take weeks. It depends on the status of the patient as well as the desired goals.
Consider picking goals that are achievable and can be met by the patient. This will help the patient feel like they are making progress but also provide relief to the nurse because they can track the patient’s overall progress.
>> Show Me Online RN-to-BSN Programs
Nursing care plans contain information about a patient’s diagnosis, goals of treatment, specific nursing interventions, and an evaluation plan. The nursing plan is constantly updated with changes and new subjective and objective data.
Key aspects of the care plan include,
Outcome and Planning
Implementation
Through subjective and objective data, constantly assessing your patient’s physical and mental well-being, and the goals of the patient/family/healthcare team, a nursing care plan can be a helpful and powerful tool.
*This website is provided for educational and informational purposes only and does not constitute providing medical advice or professional services. The information provided should not be used for diagnosing or treating a health problem or disease.

Kathleen Gaines (nee Colduvell) is a nationally published writer turned Pediatric ICU nurse from Philadelphia with over 13 years of ICU experience. She has an extensive ICU background having formerly worked in the CICU and NICU at several major hospitals in the Philadelphia region. After earning her MSN in Education from Loyola University of New Orleans, she currently also teaches for several prominent Universities making sure the next generation is ready for the bedside. As a certified breastfeeding counselor and trauma certified nurse, she is always ready for the next nursing challenge.

Plus, get exclusive access to discounts for nurses, stay informed on the latest nurse news, and learn how to take the next steps in your career.
By clicking “Join Now”, you agree to receive email newsletters and special offers from Nurse.org. We will not sell or distribute your email address to any third party, and you may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Brooker D. Person-centred dementia care.London: Jessica Kingsley; 2007
What is a nursing intervention: a beginner's guide. 2019. https://tinyurl.com/mh2mwhb6 (accessed 1 November 2021)
Butterworth C. How to achieve a person-centred writing style in care plans. Nurs Older People. 2012; 24:(8)21-26 https://doi.org/10.7748/nop2012.10.24.8.21.c9310
Centre for Policy on Ageing. The effectiveness of care pathways in health and social care. 2014. https://tinyurl.com/3t835kfd (accessed 1 November 2021)
Clinical and service integration. The route to improved outcomes. 2010. https://tinyurl.com/whb87xd6 (accessed 1 November 2021)
Department of Health. Refocusing the Care Programme Approach. Policy and positive practice guidance. 2008. https://tinyurl.com/anyrzhy6 (accessed 3 November 2021)
Department of Health. Personalised care planning: improving care for people with Long term conditions. 2011. https://tinyurl.com/uc3u3tkh (accessed 1 November 2021)
Department of Health. Care planning in the treatment of long term conditions: final report of the CAPITOL Project. 2013a. https://tinyurl.com/7399vphc
Department of Health. Mental health payment by results guidance 2013-2014. 2013b. https://tinyurl.com/9zyfmy87 (accessed 1 November 2021)
Dimond B. Exploring the legal status of healthcare documentation in the UK. Br J Nurs. 2005; 14:(9)517-518 https://doi.org/10.12968/bjon.2005.14.9.18078
Foundations of nursing practice: making the difference, 2nd edn. In: Hogston R, Simpson PM (eds). London: Palgrave Macmillan; 2002
Kozier B, Erb G, Berman A, Snyder S, Lake R, Harvey S. Fundamentals of nursing: concepts, process and practice, 8th edn. Harlow: Pearson Education; 2008
Leach M. Clinical decision making in complementary & alternative medicine.Chatswood (NSW, Australia): Elsevier; 2010
Lloyd M. A practical guide to care planning in health and social care.Maidenhead: Open University Press; 2010
Matthews E. Nursing care planning made incredibly easy!.Philadelphia (PA): Lippincott Williams and Wilkins; 2010
Monitor. Delivering better integrated care: A summary of what delivering better integrated care means and how Monitor is supporting the sector. 2015. https://tinyurl.com/825k8kd6 (accessed 1 November 2021)
NHS website. NHS launches accredited suppliers for electronic patient records. 2019. https://tinyurl.com/4fzs4up5 (accessed 1 November 2021)
National Institute for Clinical Excellence. What to expect during assessment and care planning. 2021. https://tinyurl.com/63hm5vvp (accessed 1 November 2021)
NHS England. Personalised care and support planning handbook: the journey to person-centred care: Core information. 2016a. https://tinyurl.com/9fyrtw45 (accessed 1 November 2021)
NHS England. Mental health clustering booklet v5.0 (2016/17). 2016b. https://tinyurl.com/7p6dfnry (accessed 1 November 2021)
NurseChoice. Nursing smart goals: how to set smart goals for Nursing. 2018. https://tinyurl.com/s292baez (accessed 1 November 2021)
Nursing and Midwifery Council. Future nurse: standards of proficiency for registered nurses. 2018a. http://tinyurl.com/yddpadva (accessed 1 November 2021)
Nursing and Midwifery Council. The code: professional standards of practice and behaviour for nurses, midwives and nursing associates. 2018b. https://tinyurl.com/gozgmtm (accessed 1 November 2021)
Nursing and Midwifery Council. Keep records of all evidence and decisions. 2021. https://tinyurl.com/4pcabhms (accessed 1 November 2021)
Revello K, Fields W. An educational intervention to increase nurse adherence in eliciting patient daily goals. Rehabil Nurs. 2015; 40:(5)320-326 https://doi.org/10.1002/rnj.201
Royal College of Nursing. RCN factsheet on nurse prescribing in the UK. 2014. https://tinyurl.com/hkndnbhv (accessed 3 November 2021)
Nursing process. 2021. https://www.ncbi.nlm.nih.gov/books/NBK499937 (accessed 1 November 2021)
Wing JK, Beevor AS, Curtis RH, Park SGB, Hadden J, Burns A. Health of the Nation Outcome Scales (HoNOS). Br J Psychiatry. 1998; 172:(1)11-18 https://doi.org/10.1192/bjp.172.1.11
World Health Organization. Integrated care models: an overview. 2016. https://tinyurl.com/6encn9a5 (accessed 1 November 2021)
Yeomans D. Clustering in mental health payment by results: a critical summary for the clinician. Adv Psychiatr Treat. 2014; 20:(4)227-234 https://doi.org/10.1192/apt.bp.113.011320
Assessing the patient's needs and planning effective care
Benjamin Ajibade
Senior Lecturer, Mental Health Nursing, Northumbria University
View articles · Email Benjamin

Nurses have an essential role to play in the assessment and planning of patient care. This is emphasised in the Nursing and Midwifery Council's 2018Future Nurse proficiency standards. In this article, the author discusses the importance of person-centred care in assessing needs and highlights the need for all nursing interventions to be evidence based. The topics covered include assessing people's needs, care planning, stages of care planning, benefits of care planning, models of care, care pathways, and care clustering in mental health care. The article also highlights the significance of record-keeping.
The central role of nurses in assessing patient needs and planning care is one of the core areas emphasised in Future Nurse, the Nursing and Midwifery Council's (NMC) (2018a) nursing proficiency standards. The document categorises ‘assessing needs and planning care’ as the third of seven areas of proficiency, which are grouped into ‘platforms’. Future Nurse emphasises that the delivery of person-centred care and evidence-based nursing interventions are vital components for effective patient assessment and care planning. The standards further highlight that the nurse should understand the need to assess each patient's capacity to make their own decisions and to allow them the opportunity to give and withdraw consent.
An assessment is a form of a dialogue between client and practitioner, in which they discuss the needs of the former to promote their wellbeing and what they expect to happen in their daily life ( National Institute for Health and Care Excellence (NICE), 2021 ). Nursing assessment involves collecting data from the patient and analysing the information to identify the patient's needs, which are sometimes described as problems.
The process of planning care employs different strategies to resolve the needs identified as part of an assessment. Ideally, this will include the selection of appropriate evidence-based nursing interventions. When planning care, the patient's needs and wishes should be prioritised, and the individual must be involved in the decision-making process to ensure a person-centred approach. The planned care must take into account the patient's conditions, personal attributes and choices. It is worth noting that the principles of care planning are transferable between hospital, home and care home settings.
Section 2 of the NMC Code highlights the importance of partnership working with patients to ensure the delivery of effective high-quality care and of involving them in their care, which includes empowering patients by enabling them to make their own decisions ( NMC, 2018b ). The patient should be viewed holistically, with importance placed on the physical, psychological, social and spiritual aspects of the person's life, which are inextricable.
The intrinsic factors of a patient's condition will often affect their concordance with the advice and treatment offered. Consequently, it is important to understand the reasons for non-concordance and to tailor treatments/recommendations to each individual, which will improve the quality of care delivered.
Brooker (2007) developed the acronym VIPS to address some of the confusion surrounding what should or should not be perceived as person-centred care. VIPS stresses the following:
- V is a value base that affirms the value of each human being, irrespective of age and cognitive ability. This is the foundation for individualised care
- I is individualised care that considers the individual's distinctiveness and holistic needs
- P is about seeing the world from the patient's perspective, to ensure that the health professional takes the patient's point of view into account when providing care
- S is about maintaining a social environment that supports the patient's psychological needs, including their mental, emotional and spiritual needs.
Health professionals should endeavour to involve the patient in decision-making and enable them to make choices as much as possible, using a range of approaches to achieve this ( Lloyd, 2010 ). Unless proven otherwise, a nurse must assume that a patient has the capacity to make their own decisions, in line with the Mental Capacity Act 2005.
The following draws on the author's experience in mental health nursing but can be applied to other areas of nursing care.
Care planning
Planning care is essential in the delivery of appropriate nursing care. Following assessment of a patient's needs, the next stage is to ‘plan care’ to address the actual and potential problems that have been identified. This helps to prioritise the client's needs and assists in setting person-centred goals. Planned care will change as a patient's needs change and as the nurse and/or other health professionals identify new needs. Care planning assists professionals to communicate information about the patient's care to others ( Department of Health (DH), 2013a ; NICE, 2021 ), to facilitate continuity of care. Communication may be predominantly verbal, but it will also always involve documentation in a variety of formats, including computer-based, handwritten or preprinted care plans.
It is essential for nurses to consider their consultation style when developing a care plan in order to reduce the risk of paternalism when communicating with the patient and discussing their needs. Collaborative consultation encourages patients to participate in their care and improves rapport, while a paternalistic approach will generally minimise an individual's part in, and responsibility for, their own care needs and may compromise care outcomes and concordance ( Leach, 2010 ). A collaborative/partnership consultation style facilitates a person-centred approach by the practitioners and involves the patient in their care. Such an approach can include asking questions such as: ‘We have different types of treatment approaches that could be considered, what are your preferences?’ This is in contrast to a paternalistic consultation style with the health professional announcing any decisions with a statement such as: ‘I am going to prescribe a certain treatment for you.’
When drawing up a care plan with a patient the nurse should take into account a number of considerations ( Box 1 ).
Box 1.Nursing considerations
- The patient should know the reason for the assessment
- The assessment should be flexible and adaptable to the needs of the individual
- The patient must be fully involved and their dignity, independence, and interests should be paramount
- The patient can have someone with them, if preferred
- Appropriate language and terminologies should be used throughout the consultation
- The diversity of the individual client, their beliefs, values, culture and their circumstances must be considered
- It is essential to consider the patient's gender, sexuality, ethnicity, disability and religion as part of the assessment
- Be open to listening to the patient's personal history and life story
- The entire family's needs should be considered, inclusive of the patient and their carers: remember the importance of providing holistic care
- Cost-effectiveness should also be taken into account
Sources: Department of Health, 2011; National Institute for Health and Care Excellence, 2021
Stages of care planning
Care planning has been described as the third stage of the nursing process ( NMC, 2018a ; Toney-Butler and Thayer, 2021 ). It includes assessing the patient's needs, identifying the problem(s), setting goals, developing evidence-based interventions and evaluating outcomes ( Matthews, 2010 ). This will require the health professional to apply high-level critical thinking, decision-making and problem-solving skills. It is important to note that a care plan can be prescriptive: it is devised after a patient has been assessed through the prescription of nursing actions ( Hogston and Simpson, 2002 ) or through collaborative working involving the multidisciplinary team.
In some situations there will be differences between what the nurse sees as a priority in terms of the patient's needs and what the patient wants. An example of this would be a patient with mental health problems who may be at high risk of self-harm, who may need to be put on intermittent 15-minute observation. In such cases, a patient would be deemed as not having capacity to make decisions and the nurse will need to use their clinical judgement to prescribe the best treatment option. The care plan can still be agreed in conjunction with the patient once the nurse has explained the reasons for the interventions and acknowledged in the care plan that this is not the patient's preferred choice.
In situations where the patient has capacity to make decisions, the care plan should be agreed in collaboration with the service user ( NHS England, 2016a ).
Identifying needs
As part of the care planning process, the nurse will identify a patient's needs/problems and propose a set of interventions to address them in order of priority, ensuring that everything is in agreement with the patient. To ensure that appropriate goals are set, a patient's needs will be classified as high, intermediate and low.
Each goal provides an indication as to the expected outcome, along with the proposed interventions required to meet the patient's problems/needs, all of which must be patient centred. It is important, in collaboration with the patient, to set both short-term, achievable goals and longer-term goals that may take days, weeks or months to accomplish. One way nurses can ensure this is to apply the SMART goal-setting approach to ensure that the goals are ( Revello and Fields, 2015 ; NurseChoice, 2018 ):
- M easurable
- A chievable
- T imely (within a defined time frame).
Interventions
Interventions are nursing actions/procedures or treatments built on clinical judgement and knowledge, performed to meet the needs of patients. The actions should be evidence based and indicate who will carry them out, when and how often ( Hogston and Simpson, 2002 ). The scheduled interventions will have been agreed with the patient with the aim of improving their health condition, and each subsequent action should strive to meet the goals set at the previous stage. Brooks (2019) outlined three types of intervention:
- Those independently initiated by nurses
- Those that are dependent on a physician or other health professionals
- Those that are interdependent, that is, those rely on the experience, skills and knowledge of multiple professionals.
Independent nursing interventions are planned and actioned by nurses autonomously ( NMC, 2018a ), and these actions do not require the nurse to have direction from another health professional. When actioning interventions dependent on other health professionals, the nurses must determine the appropriateness of any directions from other health professionals before carrying them out because the nurse remains accountable for the actions, for example, the administration of prescribed medication ( NMC, 2018a ). Due to developments in the nursing profession, some advanced nurse practitioners can now prescribe interventions, eg prescription of medication can be done by nurse independent prescribers or nurse supplementary prescribers ( Royal College of Nursing, 2014 ). Interdependent interventions are usually recorded in collaborative care plans reviewed in multidisciplinary (MDT) meetings and must be agreed by all parties involved. Both the goals and interventions must be communicated in a timely manner to all those involved in the patient's care.
This is the stage when a planned intervention is evaluated to assess whether or not it has been achieved. This can be an ongoing process, and the care plan should document the frequency and time frame for evaluating the intervention. If the initial goal becomes unachievable, the nurse will be required to reassess the patient's needs, and review and revise the interventions.
Benefits of care planning
The DH (2011) highlighted that the aim of care planning is to improve the quality of care and outcomes by respecting individual wishes and enabling patients to acknowledge the ownership of their condition and ensuring they have the ability to influence the outcomes. Health professionals should engage individuals in decision-making and facilitate them to take control of their health by agreeing common goals to improve outcomes. This will have additional benefits for both the patient and health services as it should reduce the number of GP appointments and emergency admissions the patient may require. Promoting self-management of long-term conditions can also help slow progression of illness.
Care planning empowers patients to care for themselves when they are self-managing their health and when they may have difficulty accessing a health professional. This became evident during the pandemic, with patients often having to go for extended periods between appointments with their health professionals. Care planning has really come into its own in community care in the past few years, which became evident during the pandemic—particularly in the field of mental health—because it leads to better patient concordance with treatment and other care needs without the need for constant input by health professionals. This benefits both health professionals and the NHS: it increases job satisfaction, brings efficiency savings and improves the quality of patient care ( DH, 2011 ).
Model of care
Models of care are used to deliver best practice in health care. An integrated services care model is multifaceted and enables the co-ordination of care by different health and social care professionals to meet individual patient needs. It encompasses patient-centred care and enables care staff across different providers to reduce duplication, confusion, delay and gaps in services ( Monitor, 2015 ). In the modern NHS, this is the preferred model of care.
The care plan is an integral part of this model because it enables the creation of shared care plans that map different care processes. It becomes a point of reference for various providers involved in the care of the patients, ensuring the co-ordination of care across services ( Curry and Ham, 2010 ; World Health Organization, 2016 ).
Care pathways
Care pathways, which are also known as critical pathways, clinical pathways, integrated care pathways, care paths and care maps, are used to describe a specific patient journey that dictates the care to be provided or process to be followed for a patient's particular condition or needs. An evidence-based care process is established for specific conditions by considering expert opinion that takes into account the evidence to recommend interventions that have been shown to achieve better health outcomes cost-effectively ( Centre for Policy on Ageing, 2014 ).
Care pathways are often developed at local level and have been shown to be efficacious at meeting local needs. They are also known to improve cross-setting collaborations. Clinical pathways are aimed at providing effective health care appropriate for the patient group of conditions, thereby reducing hospital stays, leading to cost-effective health care ( Kozier et al, 2008 ).
Care clusters
Care clustering is a needs assessment tool that is used to rate a patient's care need against specific scales:
‘A cluster is a global description of a group of people with similar characteristics as identified from a holistic assessment and then rated using the Mental Health Clustering Tool (MHCT).’
NHS England, 2016b
This framework is used to plan and organise mental health services, including the care and support provided to individuals based on their illness and individual needs. One of the care clustering tools used in the NHS is the Health of the Nations Outcome Scales (HoNOS) ( Wing et al, 1998 ; Yeomans, 2014 ; NHS England, 2016b ).
Mental health services were brought under the scope of Payment by Results (PbR) in the NHS in 2012-2013.
‘Payment by Results (PbR) is the transparent rules-based payment system in England under which commissioners pay healthcare providers for each patient seen or treated, taking into account the complexity of the patient's healthcare needs.’
Consequently, as part of the care planning process, nurses need to take into account the cost-effectiveness of any interventions in order to consider how much funding is likely to be available for an initial completion of assessments, during scheduled reassessment and at any subsequent reassessment after a significant change in the patient's needs.
Box 2.Importance of complying with guidelines when undertaking assessment and planning care
- You must be compliant with the Nursing and Midwifery Council (2018b ; 2021 ) guidelines for record and record-keeping
- Adhere to the employing local organisation's policy on record-keeping, eg local trust policy
- Follow the NHS trust Care Programme Approach (CPA) policy ( Department of Health, 2008 )
- Collaborate with all those involved in a patient's care planning process
Importance of record-keeping
Accurate record-keeping is essential in the assessment of needs and planning care. This complies with the NMC (2018b) which states that record-keeping is fundamental to nursing practice, emphasising that records must be accurate and precise.
Health professionals should be aware of the need for legal accountability when documenting care in a written record because such records could be used in any legal proceedings ( Dimond, 2005 ). A record refers to not only a patient's record, but encompasses all records related to an individual nurse's range of practice. It is important to include the person being cared for in the record-keeping process, who should be asked to sign the plan of care, if they have capacity to do so ( NMC, 2021 ).
It is good practice to make an entry in the care documentation if a service user is unable to sign or agree to their planned care and state the reason for this ( Butterworth, 2012 ). In addition to paper-based records, care plans can be entered into the electronic health/patient record system used in the practitioner's service ( NHS website, 2019 ).
Best practice in writing care plans
There are some critical factors to consider when writing a focused person-centred care plan. One of these is to clearly document in detail the needs of the patient and to use the patient's language whenever possible, for example: ‘Mr D likes to dress smart every morning, but has been finding it difficult to make the choice of clothing to wear.’ An example of a poor way to record the same issue might be: ‘Mr D is unable to dress by himself’ and the aim is ‘Mr D will appear to dress smartly’.
The documented goal/aim of the care plan should be determined by applying the SMART acronym. It is therefore vital to ensure that the aim is specific by focusing on issues that can be measured, with goals that are achievable and realistic. It is also important to suggest and record a time frame within which a patient's short-term and long-term goals could be achieved. In relations to Mr D's clothing, a daily time frame might be appropriate. To come to an agreement over this issue, Mr D might be asked: ‘Mr D, would you like to be able to make your own choice of clothes to wear every day with the support of staff?’ The projected daily goal would then be recorded as part of the care plan documentation.
An intervention must specify how a goal/aim will be achieved, including who will be responsible for implementing each task. This could be the staff nurse on duty, team nurse, team leader, the nurse in charge and/or the patient (please put the patient's name). Evaluation should be carried out regularly and documented, and should conform with the proposed time frame outlined as part of the suggested intervention. Evaluations should be undertaken whenever actions are performed in accordance with each proposed intervention, and details of the progress of the patient's problem/needs documented.
In conclusion, the article has discussed the importance of assessing patients' needs, emphasising person-centred care using the VIPS acronym devised by Brooker (2007) . It has stressed the notion for all nursing interventions to be evidence based. The stages of care planning were discussed, and the application of the SMART goal-setting approach was highlighted. Record-keeping is an integral part of care planning in the communication of patient's care and progress. The benefits of care planning in improving quality of care and outcomes, respecting individual wishes, thereby empowering the patient was recognised.
LEARNING OUTCOMES
- Nurses must ensure that assessment of patient needs and care planning are always focused on the person
- All nursing interventions must be evidence based
- The goals set out in a patient's care plan must be achievable and measurable, and should include time frames within which both short- and long-term goals can be achieved
- Record-keeping is a vital component of care planning and is part of communicating aspects of a patient's care, and their progress towards their goals, with other health professionals involved in their care
CPD reflective questions
- In the context of a patient's health, what should you aim to do when care planning?
- Who should you involve in the care planning and why? Should the patient have a copy of the care plan?
- Is it acceptable to destroy care plans or other records?
- When should care plans be reviewed?
Nursing Care Plan for the Aging Patient: Ms. Anderson’s Case Report
Introduction, chosen patient, nursing care plan, educational nursing care plan.
A number of patient assessment tools have been developed for the assessment of older people focusing on the patient’s ability to maintain activities of daily living (Ware, 3-11). These instruments, however, lack a systematic assessment of patient preferences as an important part of successfully initiating patients in making necessary changes in health behavior to regain or maintain capabilities in independent functioning. A holistic perspective nursing adopted as its underlying philosophy the need to integrate patients’ values, beliefs, and goals into nursing care but patient problems have usually been identified from the perspective of health care providers and their assumptions about which problems are important, without verifying these assumptions with the recipient of care – the patient (Moore & Kramer, 163-168). Evidence showed that a successful clinical relationship is one where patient and caregiver arrive at a consensus concerning the problem, physiological processes, prognosis and optimal treatment (Felch, 12) and a negotiated approach to decisions about patient care has been encouraged. In this essay, I will try to demonstrate client assessment from a nursing point of view that includes evaluating body functioning according to the Lorensen’s Self-Care Capability Scale (LSCS) that includes eating, drinking, eliminating, sleeping, moving, bathing, and grooming. Following this, I shall develop a nursing care plan in a case study format. Assessment is the first stage in the nursing process, and in order to conduct it rationally, a nurse must competently collect data from many sources, then analyze and synthesize it, before using the obtained data to develop a healthcare plan followed by the final evaluation. Accurate judgments can then be made about the patient’s health status and the nursing intervention required (Lazerowich, 121-126). The selected patient will be discussed using a model/framework for assessment that is used in practice. Three main needs of the patient will be outlined in the post-operative period following surgery.
Ms. Anderson, a 75-year-old woman presents at her annual physical examination. Her medical history, physical examination, and test results are as follows. In order to gather data about Ms. Anderson, a data collection tool was used. The tool contained the assessment of bodily functions according to LSCS and addressed the need to maintain those functions (see appendix).
Health History
Health History has been smoking heavily for 25 years. Considers herself ill during the course of the last 15 years, when after retirement Ms. Anderson started working as a janitor, where she experienced unfavorable thermal regimens. During her janitor work often experienced an ailment and took sick leaves from work once or twice each year. She left the job in two years, however continued to experience ailment two times annually. The symptoms usually included a fever of 37.6-38.2 o C, coughing with a scanty amount of colorless sputum, accompanied by general weakness and dyspnea at rest. During ten years Ms. Anderson was diagnosed with an acute respiratory viral infection, or acute respiratory disease, and prescribed antibiotics such as erythromycin, which caused the significant improvement. The fever disappeared in 7-8 days. The amount of sputum slightly increased and the coughing faded away. The patient recovered on the 2 nd -3 rd week. Three years ago she went to a different doctor, who arrived at the diagnosis of chronic bronchitis. Within the last three years, the aggravations became more frequent (3-4 times per year). The latest aggravation happened 3 weeks ago when during another exacerbation of chronic bronchitis the overall well-being started to decline (this followed Ms. Anderson going outside on the 5 th day of chronic bronchitis exacerbation): gradual rise of body temperature (38.4 o C in 24 hours), slight Algor and hyperhidrosis, increase of the coughing, the onset of dyspnea.
In 24 hours following these symptoms, Ms. Anderson called the ambulance. At the time of admittance to the hospital, her fever was 39.0 o C. From the patient’s words during the last three winters, her smoker’s cough produced sputum on most days. She complains of fatigue, constant coughing, and shortness of breath at rest. She is limited in her activities of daily living but she states that she is not taking part in any sports. The patient appears to have no asthma, allergies, gastrointestinal, or cardiac symptoms. Her family history revealed that her mother died at the age of 70 from stroke and her father died at age 67 from lung cancer. Both were heavy smokers. One sister aged 42 has breathing difficulties and is taking adrenoceptor agonists (salbutamol). Ms. Anderson has undergone an appendectomy 25 years ago. At about the same time she was in the hospital for removing calculus in both kidneys, and an x-ray revealed a cyst in the left kidney. 20 years ago she has undergone nodular hysteromyoma surgery. Around 22 years ago the patient was diagnosed with primary hypertension, as well as ischaemic heart disease: stenocardia. In 1992 Ms. Anderson survived a cerebrovascular accident.
Physical examination
The general condition of the patient is satisfactory. The consciousness is lucid. The body constitution is normothermic, height – 153 cm, weight – 92 kg, posture is slouchy, limps when walking. The body temperature is 36.8 o C. Facial expression is calm. The skin color is pale, without cyanosis. The skin is dry turgor pressure is low. Mucosal membranes are pale. The nails are without any visible deformations. The subcutaneous fat is well developed, mostly on the abdominal, lumbar, and femoral regions. Insignificant pastousness in the lower leg regions. The main groups of lymphatic nodes are not enlarged during palpation. The muscles are of sufficient development, with low tonicity. Bones are without visible alterations. Joints demonstrate alterations in both radiocarpal, and the left popliteal joint, which is tender during palpation. The patient also complains of paroxysmal pain in the spinal cord. The thyroid gland does not palpate. The respiration is thoracic, symmetrical, and shallow, with 20 breaths per minute. The palpation revealed low elasticity of the thoracic cage. Pectoral fremitus is increased insignificantly. The auscultation of the lungs revealed adverse respiratory murmurs – small bubbling rales in the left axillary and scapular regions. Complains of constricting pains behind the sternum after physical exertion. The arterial pulse rate is 80 beats per minute. The abdomen is slightly enlarged due to fat deposits. The edge of the liver is algesic during palpation. The urogenital system and nervous system are without pathology. The vision acuity and locomotor reactions are lowered.
Test Results
The complete blood cell count revealed: Hemoglobin – 118 g/l (low), erythrocytes 4.4, globular value – 0.85 (low), leukocytes – 6.7/L, monocytes – 6%, eosinophiles – 5%, lymphocytes—26%, blood platelets – 180/L, ESR – 5 mm/h. The biochemical blood assay: total protein – 65g/l, alanine aminotransferase – 24 mmol/l, aspartate aminotransferase – 28 mmol/l, glucose – 5.2 mkmol/l. The urine test showed no traces of erythrocytes or urinary cylinders. The urinary level of leukocytes is 452 mln/l. The sputum test results are as follows: color – gray, type – mucosal, consistency – mucilaginous, eptithelium – small amounts, leukocytes – 25-30 within the visual field. The streptococci from the sputum demonstrated resistance to penicillin, ristomycin, chloramphenicol, and tetracycline. The x-ray of the pectoral region revealed emphysema with diffuse pneumosclerosis. The lung pattern is deformed, as there is lesser circuit hypertension. There are infiltrative alterations in the basal layer of the left lung. Both ventricles of the heart are enlarged equally. The sonographic examination revealed enlarged liver and induration of the kidneys with an insignificant amount of concrements (0.3-0.5 cm). The ECG showed the electrical axis of the heart rotated to the left, and slight hypertrophy of the left ventricle. The conductive function is adequate (P-Q=0.14sec., QRS=0.08 sec). PO 2 = 50 mmHg.
Functional Assessment
Spirometry is compatible with mild obstruction and no significant reversibility. During physical exercise – explicit dyspnea.
Cognitive and mental health assessment
The patient’s consciousness is clear, she is well oriented in time and space, answers the questions adequately, but with delay, does not appear to be talkative. The papillary reaction to light is normal, although the visual acuity is lowered. The face is symmetrical, and there are no signs of meningeal symptoms.
Socio-environmental assessment
Ms. Anderson is retired and is currently residing with her sister. The living conditions are satisfactory.
Nursing Care Plan – based on the history of the current disease, namely that the onset occurred against the background of chronic bronchitis aggravation, it is rational to verify the diagnosis of chronic obstructive bronchitis (Royer, 42). The most informative are Ms. Anderson’s complaints which are indicative of this illness. The most significant assessment data are the results of functional external ventilation tests that indicate an obstructive alteration in the current patient. In such a manner, the chronic obstructive bronchitis diagnosis is based mainly on the history and complaints of the patient, as well as functional ventilation tests (Burke & Laramie, 43). The diagnosis of acute sinister bronchopneumonia of medium severity is based mainly on the patient’s complaints which include fever of 39.2 accompanied by chills, coughing, and heaviness in the left side of the chest, just below the scapula, improvement of the condition after antibiotic therapy. The examination findings, such as respiratory small bubbling rales in the left axillary and scapular regions also contribute to the above diagnosis. The laboratory finding that is evident of inflammation ESR below 20 mm/h. The infiltrative alterations of the left lung on the x-ray are also relevant. Summarizing the above data it is certain that Ms. Anderson has bronchopneumonia that has typical characteristics, such as slight symptoms of intoxication and inflammation (Murray, 18). The x-ray of the chest, as well as auscultation, helped determine the affected side. It is clear that the duration of the disease is of medium severity, as the patient is 75 years old, and has chronic disabling diseases in her medical background (arterial hypertension, chronic obstructive bronchitis).
The diagnosis of respiratory distress is arrived upon based on the patient’s complaints – dyspnea when going up the stairs, or walking for 200 meters, as well as on the external ventilation tests. Based on the above findings Ms. Anderson can be diagnosed with Chronic Obstructive Pulmonary Disease (COPD). When prescribing treatment it is important to note that the patient besides bronchopneumonia and chronic obstructive bronchitis is suffering from arterial hypertension and exertional angina (Shaw, Peterson & Mark, 141-148). It is essential that Ms. Anderson receives her treatment for bronchopneumonia as soon as possible, as in this case, it will be effective. This patient must be hospitalized, as she is over 65 years old, has severe accompanying conditions, and can not be provided with adequate care at home. From a nursing point of view, it is necessary for the patient to follow a strict bed regimen (Ebersole & Hess, 75). This means that her eating, drinking, and elimination needs must be rationally satisfied. The nurses must also take care of the patient’s hygiene. This includes frequent bathing and grooming. The bed regimen may be not as strict, once the signs of intoxication and fever go down. The patient’s general satisfactory condition means and that she moves actively means that there is no need for decubitus ulcer prevention. The treatment that she receives must include primarily penicillin-type antibiotics, for example, intramuscular injections of ampicillin twice a day (Ruben & Stout, 164). It is rational to prescribe combined antibiotic therapy, as there is accompanying pathology and immune deficiency. This additional treatment should include aminoglycosides, such as gentamicin that is injected intramuscularly twice a day.
The duration of the therapy shall depend on signs of improvement, a decrease in the body temperature, and level of intoxication. It is necessary to continue this treatment for five days after the condition improves. Expectorant drugs such as bromhexine are also required to drain the bronchial tree, especially the segmental bronchus in the affected locus. Immune modulators are needed to correct the immune status (Freeman, 64-94). In order to do this, the patient shall be administered ascorbic acid, thiamine, and tocopherol in form of intramuscular injections. A nursing care plan may also include physiotherapy that can be used to rehabilitate Ms. Anderson’s condition after the acute period has passed (Kemp, Brummel-Smith & Plowman, 9). The most effective physiotherapy would be bronchial spasmolytic inhalations. These can include such medications as beta-2 adrenal agonists. There is also a possibility of conducting exercise therapy that will increase tolerance to physical stress. Various coronarodilators can be used to prevent complications of ischemic heart disease and stenocardia. The expectancy of absolute recovery outcome for a patient that had acute bronchopneumonia and chronic obstructive bronchitis is negative (Hart, Laden, Schenker & Garshick, 1013). This is due to the lengthy progressive duration of chronic bronchitis, old age, and accompanying pathology of the heart. The most effective healthcare strategy, in this case, is decreasing the development of major chronic disorders.
Nursing Diagnosis
The patient/client has a problem/potential problem in his/her need for adequate breathing because she is not able to perform the physical exercise without showing signs of explicit dyspnea.
Expected Outcome
The best possible situation that this particular patient/client can achieve in three days is that she will be able to walk without experiencing severe shortness of breath.
Evaluative Criteria
I will know if the expected outcome is achieved if I can observe Mrs. Anderson walking for 200 meters without experiencing dyspnea.
Planned Interventions
The most appropriate way for the patient/client to achieve their Expected Outcome is for the patient/client and me to ensure that Mrs. Anderson has adequate oxygen supply to her lungs.
The reasons I have chosen these particular interventions are because a higher supply of oxygen will cause better oxygenation of hemoglobin in her blood and shall prevent hypoxemia and improve the quality of life, by enabling the patient to perform activities of everyday living. This rationale will also prevent the possible complications of COPD, such as cor pulmonale or pulmonary hypertension. In order to provide better oxygenation of hemoglobin, long-term oxygen therapy (LTOT) must be used as the most effective rationale. There are many forms of administering LTOT, however, in this case, a reservoir, nasal cannula should be used. It will collect the expired gasses and enable the patient to rebreathing the air from the oxygen delivery system during the next breath. The nasal cannula is equipped with a sensor of oxygen pressure in the nose and shall deliver oxygen only during inhalation.
Using the evaluative criteria, what I now observe is an increase in exercise tolerance and improvement of mental functioning, as the patient is able to walk a distance of 200 meters without feeling dyspnea, and also appears to be in a more lively mood and more talkative.
This corresponds with what I anticipated therefore I will advise the patient to continue using LTOT in home conditions after being signed out from the hospital.
In assessing Ms. Anderson, I found that the models discussed above were practical to gain insight into the care and treatment needed. I established that in order to properly provide an effective nursing plan, it is necessary to focus on the patient’s needs, her interpretation or understanding, as well as require or might want to do and can do in order for her to improve her own health.
Burke, M. M., & Laramie, J. A. (2000). Primary Care of the Older Adult: A Multidisciplinary Approach . St. Louis, MO: Mosby (p. 43).
Ebersole, P., & Hess, P. (1998). Toward Healthy Aging: Human Needs and Nursing Response . St. Louis, MO: Mosby (p. 75).
Felch, W. C. (1996). The Secret(s) of Good Patient Care: Thoughts on Medicine in the 21st Century . Westport, CT: Praeger Publishers (p. 12).
Freeman, L. W. (2001). 3 Psychoneuroimmunology and Conditioning of Immune Function. In Mosby’s Complementary Alternative Medicine: A Research-Based Approach (pp. 66-94). St. Louis, MO: Mosby.
Hart, J. E., Laden, F., Schenker, M. B., & Garshick, E. (2006). Chronic Obstructive Pulmonary Disease Mortality in Diesel-Exposed Railroad Workers. Environmental Health Perspectives, 114 (7), 1013+.
Kemp, B., Brummel-Smith, K., & Plowman, V. J. (1989). Geriatric Rehab Program Focuses on Research, Training and Service. The Journal of Rehabilitation, 55 (4), 9+.
Lazerowich, V. (1995). Development of a Patient Classification System For a Home-Based Hospice Program. Journal of Community Health Nursing, 12 (2), 121-126.
Moore S.M. & Kramer F.M. (1996) A comparison of women’s and men’s preferences for cardiac rehabilitation program features. Journal of Cardio-pulmonary Rehabilitation 16 , 163–168.
(1992). Measuring Functioning and Well-Being: The Medical Outcomes Study Approach (A. L. Stewart & J. E. Ware, Ed.). Durham, NC: Duke University Press (p. 41).
Murray, J. F. (2000). Intensive Care: A Doctor’s Journal . Berkeley, CA: University of California Press (p. 18).
Orem D.E. (1995) Nursing: Concepts of practice . Mosby, St Louis. Palmer R.M., Landefeld C.S., Kresevic D. & Kowal J. (1994) A Medical Unit for the acute care of older people. Journal of the American Geriatrics Society 42 , 545–552.
Royer, A. (1998). Life with Chronic Illness: Social and Psychological Dimensions . Westport, CT: Praeger Publishers (p. 42).
Ruben, D. H. & Stout, C. E. (Eds.). (1993). Transitions: Handbook of Managed Care for Inpatient to Outpatient Treatment . Westport, CT: Praeger Publishers (p. 164).
Shaw, L. J., Peterson, E. D., & Mark, D. B. (2002). Chapter 7 Clinical Recognition: Risk Assessment Screening. In Heart Disease in Women (pp. 141-148). New York: Churchill Livingstone.
Ware, J. E. (1992). 1. Measures for A New Era of Health Assessment. In Measuring Functioning and Well-Being: The Medical Outcomes Study Approach , Stewart, A. L. & Ware, J. E. (Eds.) (pp. 3-11). Durham, NC: Duke University Press.
Ziguras, C. (2003). Self-Care: Embodiment, Personal Autonomy, and the Shaping of Health Consciousness . New York: Routledge (p. 41).
LSCS (Lorensen’s Self-Care Capability Scale) was chosen in order to systematically incorporate patients’ preferences in the assessment of older people comprising aspects not found in other instruments. Assessment tools for this patient population include assessing body functioning, such as eating, drinking, eliminating, sleeping, moving, bathing, grooming, Orem’s self-care model as a conceptual framework which is widely known and accepted by nurses.
The model defines three categories of self-care requisites necessary for performing self-care in maintaining life, health and well-being (Orem, 1995) that address the need to maintain bodily functions, such as the need for air, water, food, elimination, rest, solitude, social interaction and prevention of hazards, developmental and health deviation self-care requisites, developmental and cognitive capabilities. These are a prerequisite
to learning new self-care strategies, skills or behaviours (Ziguras, 41) such as the ability to seek appropriate medical assistance, carrying out medically prescribed measures effectively, or altering one’s life-style to promote personal development while living with the effect of pathology and medical measures (Orem, 545-552).
The Royal College of Physicians and the British Geriatrics Society highlighted the need for functional assessment of elderly people as part of routine clinical practice. It recommends the regular use of standardized assessment scales in activities of daily living, communication, cognitive function and memory, depression and quality of life. Regular se of these measures may be useful in planning, clinical care, provision of support services, screening, outcome assessment, clinical audit and casemix.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, March 6). Nursing Care Plan for the Aging Patient: Ms. Anderson's Case. https://ivypanda.com/essays/nursing-care-plan-for-the-aging-patient-ms-andersons-case/
"Nursing Care Plan for the Aging Patient: Ms. Anderson's Case." IvyPanda , 6 Mar. 2024, ivypanda.com/essays/nursing-care-plan-for-the-aging-patient-ms-andersons-case/.
IvyPanda . (2024) 'Nursing Care Plan for the Aging Patient: Ms. Anderson's Case'. 6 March.
IvyPanda . 2024. "Nursing Care Plan for the Aging Patient: Ms. Anderson's Case." March 6, 2024. https://ivypanda.com/essays/nursing-care-plan-for-the-aging-patient-ms-andersons-case/.
1. IvyPanda . "Nursing Care Plan for the Aging Patient: Ms. Anderson's Case." March 6, 2024. https://ivypanda.com/essays/nursing-care-plan-for-the-aging-patient-ms-andersons-case/.
Bibliography
IvyPanda . "Nursing Care Plan for the Aging Patient: Ms. Anderson's Case." March 6, 2024. https://ivypanda.com/essays/nursing-care-plan-for-the-aging-patient-ms-andersons-case/.
- Dyspnea in Cancer Patients
- Dyspnea: Pharmacological Management
- People With Disabilities in the Frida Movie
- Acute Bronchitis Symptoms & Treatment
- A SOAP Note on Bronchitis
- Acute Bronchitis and Pneumonia: How to Differentiate?
- Quantitative Study on Antibiotics for Acute Bronchitis
- Emphysema and Chronic Bronchitis: Compare and Contrast
- Emphysema and Chronic Bronchitis: Treatment
- Chronic Obstructive Pulmonary Disease and Bacterial Bronchitis
- Aging Services in Modern Society
- Community Advocacy Agencies for the Elderly
- Skin Wound Diagnostics and Treatment in Frail Elders
- Gerontology: Preparing for End of Life
- Nursing Home Designs: Health and Wellness of Aging
- Entertainment
- Environment
- Information Science and Technology
- Social Issues
Home Essay Samples Health
Essay Samples on Nursing Care Plan
The art of caring in nursing and its impact on patients.
Nursing is often described as both a science and an art. While the scientific aspect involves medical knowledge and technical skills, the heart of nursing lies in the art of caring. The art of caring goes beyond the application of treatments and medications; it encompasses...
- Nursing Care Plan
What Nursing Means To Me
One of my mentors with regards to nursing who regarded nursing as unique profession aimed at helping individuals—well or unwell—undertake in activities of daily living contributing to health or its recovery (or peaceful death) that the individual will have would have accomplished on their own...
- Nursing Theory
Being A Professional Nurse: Ethics, Law, And Competence
What is a proffesional nurse? This essay will try to answer on this question and discuss various components related to the work of a professional nurse. Such as knowledge of biopsychosocial health conditions and the impact on everyone involved in the case study of 82-year-old...
Nursing Care Plan and Nurses’ Philosophy Influence
This essay aims at critically exploring the philosophies, models, and frameworks that underpin care planning. This will be demonstrated through use of a service user case scenario with a long-term complex care need. The essay begins with an overview of the identified service user and...
The Filters for Prehospital Care of Paramedic
Paramedics are median wellbeing in health science and to maintain the disease. As Everyone depends on quick reactions and quick responses to their work. Every day there are inventions on paramedics to improve this system and develop some serves which have benefits for people. It...
Stressed out with your paper?
Consider using writing assistance:
- 100% unique papers
- 3 hrs deadline option
Nursing Philosophy: The Values And Beliefs Of The Profession
Since I was young, I have always been driven by a caring nature and a desire to help others which has led me to the career choice of nursing. I feel the most accomplished when I serve and help others, and my nursing attitude reflects...
My Nursing Philosophy: The Viewpoint Of Treating Patients
Philosophies are mainly developed from experiences and beliefs. Philosophies give people different meanings to life; they are never the same since we all have our own individual beliefs. Nurses also have their own philosophy. This philosophy is shaped by the nurse’s viewpoint. Philosophies integrate personal...
The Philosophy Of Nursing And Development Of Knowledge In The Profession
Throughout my journey of becoming a nurse, I have started to develop my personal philosophy of what nursing is. My philosophy views nursing as a way of healing others, caring for others, respecting others and treating others the way you would want to be treated....
Nursing Care Plan for Systemic Lupus Erythematosus Patient
The body of a human being is equipped to protect itself against infections and foreign material recognized in the body. This measure occurs through the production of antibodies against the antigen, which is the recognized external component, eliminating it and attaining active immunity against its...
Critical Errors in the Treatment of Lewis Blackman
Helen Haskell starts off her tragic story by describing her son. The reason she recounts all aspects of her son is because he is why we are in nursing. For all of the world war two veteran grandparents with an ejection fraction of ten percent....
- Lewis Blackman
The Psychological Impacts of Infertility
Infertility is defined as the inability for couples to achieve a pregnancy after twelve months of regular, unprotected intercourse when the woman is less than 35 years of age or after 6 months past the age of 35 (Perry, Hockenberry, Lowdermilk, Wilson, Keenan-Lindsay, 2017). Infertility...
- Infertility
Fall Risk: Nursing Strategies to Prevent Falls in the Older Adult
Falls among the older adult population in the United States are a common and serious danger. For many reasons, older adults fall and oftentimes sustain injuries that can set back healing times or in many cases trigger a downward spiral of health complications and injuries....
Managing Conflict In Clinical Practice.
Conflict is unavoidable in nursing environment as nurses need to work with other health workers , care of patients with different personalities, and communicate with patient’s family. Hence, conflict is a significant issue result in stress, turnover and job dissatisfaction. The essay will talk about...
- Conflict Resolution
Delegation In Professional Nursing
Delegation plays an integral role in the nursing profession. In fact, delegating tasks to other appropriate staff members (e. g. patient care techs, LPNS) can be the key component in making sound clinical judgements as a registered nurse; as it also determines the hierarchy of...
Best topics on Nursing Care Plan
1. The Art of Caring in Nursing and Its Impact on Patients
2. What Nursing Means To Me
3. Being A Professional Nurse: Ethics, Law, And Competence
4. Nursing Care Plan and Nurses’ Philosophy Influence
5. The Filters for Prehospital Care of Paramedic
6. Nursing Philosophy: The Values And Beliefs Of The Profession
7. My Nursing Philosophy: The Viewpoint Of Treating Patients
8. The Philosophy Of Nursing And Development Of Knowledge In The Profession
9. Nursing Care Plan for Systemic Lupus Erythematosus Patient
10. Critical Errors in the Treatment of Lewis Blackman
11. The Psychological Impacts of Infertility
12. Fall Risk: Nursing Strategies to Prevent Falls in the Older Adult
13. Managing Conflict In Clinical Practice.
14. Delegation In Professional Nursing
- Mental Illness
- Mindfulness
- Childhood Obesity
- Parkinson's Disease
- Alcohol Abuse
- Infectious Disease
Need writing help?
You can always rely on us no matter what type of paper you need
*No hidden charges
100% Unique Essays
Absolutely Confidential
Money Back Guarantee
By clicking “Send Essay”, you agree to our Terms of service and Privacy statement. We will occasionally send you account related emails
You can also get a UNIQUE essay on this or any other topic
Thank you! We’ll contact you as soon as possible.
- How It Works
- Prices & Discounts
How to Write Nursing Care Plans: Strategies for Academic Success
Table of contents
A care plan is an essential part of nursing school. It’s an important tool that nurses use to organize and document patient care. A well-written care plan includes various details and elements that enable nurses to provide comprehensive care to their patients.
As a student in nursing school, you’ll be required to create nursing care guides from time to time. This will give you a glimpse of how nurses care for patients in real life and prepare you for the job after school.
[FREE] Nursing Care Plan Example
This post will guide you through how to write a care map for nursing school and give you some tips for making your plan more effective and improving your academic success.
What is a nursing care plan?
A nursing care plan is a nursing tool that documents a patient’s needs and the action steps required to improve their health and well-being. Nurses use the tool to assess, plan, and implement care for each patient.
In nursing school, a care plan helps nursing students to reflect on the patient's concerns and analyze the interventions needed to provide quality care. It is an interactive guide that helps students stay organized while analyzing and documenting a hypothetical patient situation.
Additionally, care plans help nursing students to develop clinical analysis and decision-making skills. These invaluable skills will help you effectively plan patient treatment in real life after graduation.
How to Create a Top-Notch Care Plan for Nursing School in Six Easy Steps
Crafting a nursing care plan that is comprehensive, detailed, and effective can be achieved by following six main steps that encompass patient assessment, goal-setting, intervention planning, prioritization, documentation, and evaluation.
Step 1: Assess the patient's case study
The first step is to assess the patient case study. Read through the case study thoroughly and take note of any important information. Pay special attention to the patient's demographics, medical history, current condition, and other relevant information.
Once you understand the patient case study well, you’re ready to move on to the next step of writing the care plan.
Step 2: Analyze and organize the data
The second step is to analyze and organize the data collected from the patient case study. This is where you identify the patient’s problems and prioritize them based on severity. This step will also help you identify patterns or trends in the patient’s data.
Additionally, be careful to identify any gaps in the data that may affect the patient care process. For instance, if there is no information about the patient's family history, that would be considered a gap in the data.
Organize the data into a logical format to make it easy to reference later.
Step 3: Formulate your patient diagnosis
Once you’ve analyzed and organized data from the case study, the next step is to develop a patient diagnosis.
This is where you use the data you collected in step two above to develop a working diagnosis for the patient. Based on this information gathered, what do you believe is wrong with the patient? What is causing their symptoms?
Also, consider the patterns and trends identified to help you make a meaningful diagnosis. In your diagnosis, be sure to include both the problem and the cause of the problem.
Step 4: Write down the patient's goals and expected outcomes
After formulating your diagnosis, it’s time to set some care goals and expected outcomes for the patient. When writing patient goals and expected outcomes.
For instance, a short-term goal might be for the patient to walk independently by discharge time, while a long-term goal might be to regain their full range of motion three months after discharge.
Ensure the goals you set for your patients are SMART— specific, measurable, achievable, relevant, and time-bound.
Step 5: Write down nursing interventions and rationale
Once you’ve written down the goals and expected outcomes, it’s time to identify the most suitable nursing interventions for the patient.
Nursing interventions are the activities nurses perform to help patients reach their goals (both short-term and long-term).
When writing nursing interventions, be specific about what actions should be taken. Also, include a rationale for each intervention so your reader understands why you chose it for the patient.
For instance, if one of your patient's goals is to walk independently by discharge, a nursing intervention might be “Provide physical therapy three times per day” with a rationale of “To increase muscle strength and improve mobility.”

Step 6: Compile the patient evaluation plan
The final step in writing a nursing care plan is to compile an evaluation plan. This plan outlines how you’ll determine whether or not your nursing interventions successfully helped your patient reach their goals.
Just like the patient goals, your evaluation criteria should be specific, measurable, achievable, relevant, and time-bound (SMART). Ensure you include objective (quantitative) and subjective (qualitative) measures in your evaluation plan.
The goals you set for your patient should always be specific and be tailored to the specific needs of the patient. Ensure the goals are achievable and measurable so that you can track progress over time.
For instance, an evaluation criterion for our previous goal might be “the patient will walk 100 feet independently within 10 days”.
Once you have compiled your evaluation criteria, your nursing care plan is complete! It’s a good idea to customize your nursing care plan for every individual patient. When writing, always consider factors like age, gender, lifestyle, current medications, family history, and other factors that might influence their treatment plan.
The 5 Must-Have Parts of a Nursing Care Plan
An academic nursing care plan is an essential tool that outlines the care a patient will receive during their hospital stay or recovery period. For your nursing care plan to be effective for your patients, it must include five essential components that are critical for providing appropriate care.
Part 1: Patient health assessment
The first essential component of an academic nursing care plan is the patient health assessment. This includes information about the patient’s physical and mental condition, medical history, and current symptoms.
It also includes other relevant information like the patient’s social history or family dynamics that could impact their health. The initial patient health assessment should be thorough as it forms the basis for the rest of the nursing care plan.
Before creating your nursing care plan, you must comprehensively understand the patient’s health history and current physical condition. This will help you identify any areas needing special attention or additional interventions.
Part 2: Patient diagnosis
The second component is a diagnosis based on the patient information gathered. A patient diagnosis focuses on identifying underlying issues affecting the patient’s health.
A detailed diagnosis should identify physical problems, mental health issues, and any lifestyle factors impacting the patient’s well-being. With this diagnosis, it’s easy to determine what interventions will best improve the patient’s health and well-being.
Part 3: Nursing interventions
An ideal nursing care plan should also have a section for nursing interventions. These are actions that nurses should take or procedures they should implement to treat and care for the patient.
Nursing interventions may include medications or therapies, changes in lifestyle habits, or referrals for additional support like counseling or nutrition services.
Each intervention should include specific instructions for implementation and monitoring to ensure effectiveness in improving the patient’s health.
Part 4: Expected outcome
Another essential component of a nursing care plan is the ‘Expected outcomes.’ This section establishes expectations around how the nursing interventions will affect the patient’s overall health over time.
Expected outcomes should also be specific and reflect short-term expectations and long-term goals for sustained improvement. They should also be realistic and measurable.
Part 5: Evaluation
Finally, your nursing care plan should always have a section for evaluations.
After implementing interventions and establishing expectations, evaluating how well the patient responds is important.
An evaluation plan compares the expected outcomes with the actual results. As mentioned, an idea evaluation plan should include qualitative and quantitative measures to be more effective.
Final thoughts
A patient care map is an essential part of nursing school. It helps you organize your thoughts and provides a roadmap for caring for your patients.
When starting nursing school, having a care plan template or a guide to follow when writing your patient care plans can be helpful. This will ensure that you include all the necessary information and that your care plan is well-organized.
It’s also important to keep it short and precise. Longer and more wordy plans can be difficult to follow through. This can lead to delays in treatment or missed interventions. Use specific keywords with unnecessary details or descriptions. That way, your final care plan will be simple and easy to understand.
Understanding how to write a care plan for nursing school will prepare you to provide the best possible care for your patients during internships or after graduation.
If you’re in a fix and don’t know where to begin, contact Writers Per Hour. Our team of proficient writers are experts in writing care plans for nursing school. When you hire a nursing essay writer from us, you’re sure to receive an original, high-quality paper on time and as per your strict requirements.
Share this article
Achieve Academic Success with Expert Assistance!
Crafted from Scratch for You.
Ensuring Your Work’s Originality.
Transform Your Draft into Excellence.
Perfecting Your Paper’s Grammar, Style, and Format (APA, MLA, etc.).
Calculate the cost of your paper
Get ideas for your essay

ESSAY SAUCE
FOR STUDENTS : ALL THE INGREDIENTS OF A GOOD ESSAY
Essay: Assessment of a patient and plan of care
Essay details and download:.
- Subject area(s): Coursework
- Reading time: 9 minutes
- Price: Free download
- Published: 1 October 2019*
- File format: Text
- Words: 2,530 (approx)
- Number of pages: 11 (approx)
Text preview of this essay:
This page of the essay has 2,530 words. Download the full version above.
INTRODUCTION
The purpose of this essay is to carry out an assessment of a patient and present a plan of care of a specific problem that the patient has encountered. The model chosen to guide the care plan is the Roper, Logan and Tierney’s ‘Elements of Nursing’. This will enable me to develop my skills in assessment, problem-solving and planning care.
I will describe and explain the nursing model and provide an rationale for my choice. An overview of the assessment process will be given followed by an introduction and history of the chosen patient. An assessment of the patient will be carried out using the model to identify any problems the patient may have or encounter. Then a plan of care will be detailed relating to a specific problem identified in the assessment. Finally, I will reflect on the process of carrying out a care plan and discuss the nurse/patient relationship.
NURSING MODEL
I have chosen Roper, Logan and Tierney’s model, as it identifies and groups nursing activities in relation to the process of living. The model believes individuals carry out a series of daily activities that are fundamental to normal functioning. The philosophy of care is based on living, not illness. (Walsh 1999). The model views individuals holistically and shows awareness of cultural environmental, political and economical factors. (Roper et al 1996). It emphasises on prevention and helps patients with problems relating to activities of living. The model consists of two parts, ‘A Model for Living’ and ‘A Model for Nursing’. The Model for Living has five interrelated elements, twelve activities of living lifespan, independence-dependence continuum, influencing factors and individuality. (Roper et al 2001).
The activities are based on the idea of basic human needs and can be used as the criteria for assessment. (Roper et al 1996). Lifespan influences the individual’s behaviour in each activity of living, as each person has a lifespan from birth to death such as childhood and adolescence. It views ‘living’ as a process and recognizes individual’s abilities and requirements at their stage of life. (Roper et al 2001). The dependence-independence continuum identifies the patient’s status, as it is subject to change during illness and incapacity. Dependence is assessed at each activity acknowledging need for nursing intervention. (Roper et al 1996). The influencing factors, which are physical, psychological, sociocultural, and environmental, and politicoeconomic, provide a structure enabling a full account to be taken of the circumstances of the patient. (Walsh 1999).
The Model for Nursing contains the same elements as the Model for Living apart from individuality, where it is replaced with individual nursing. (Tierney 1998). The model will help me to provide systematic care and the knowledge gained by using the model will give me greater insight into problems affecting patients.
Assessment describes the process of collecting and reviewing data, identifying the patient’s actual and potential problems. It is the initial stage of the nursing process, followed by planning, implementation and evaluation and is a continuous and ongoing activity. (Murray and Atkinson 2000). The information collected relates to the health status and factors affecting the patient. This information can come from sources such as the patient, family, significant others, health care professionals and health records. (Heath 2000a).
The assessment enables nursing care to be planned and implemented, prioritising the patients problems. (Alfaro-Lefevre 2002). It requires to be reviewed frequently to reappraise problems as the patients condition changes. (Heath 2000b), (Rowe 1999).
Subjective and objective information are gathered during the assessment. Subjective information is reported from the patient concerning their thoughts and feelings. Objective information is observed and measured by the nurse such as temperature and pulse. (Alfaro-Lefevre 2002).
My preceptor and I discussed a suitable candidate, on which to carry out an assessment. Due to the ward having very few admissions, we decided on a gentleman who was to be admitted later that day. Since the surroundings were new to us both I felt we could relate to each other. As required by the Nursing and Midwifery Council guidelines, a pseudonym of Albert will be used to protect his identity. (NMC 2002). I introduced myself to Albert in private, as a nursing student and explained the nature and purpose of my assignment. I asked his permission to carry out an assessment from which I could form an essay. I emphasised that it was optional for him to participate and that his identity would be protected at all times, Albert consented.
The Roper, Logan and Tierney model will be implemented to the assessment and relate to the lifespan, dependence-independence continuum, and influencing factors.
Albert is an 83 year-old widower and lives alone in a bungalow in the city. He stated he has had a good life with many memories; he had travelled to several countries in his time with the Royal Navy. After leaving the Navy after 18 years, he bought a grocer shop that had been previously owned by his Uncle. He had enjoyed going to dance halls and outdoor bowling. Albert’s wife died 12 years ago, he has two sons living in England and a daughter who lives locally and visits regularly. There was no medical history relevant to his current admission.
Before admission to hospital, Albert stated he was independent and active; he regularly took his dog long for walks. Recently he has experienced several falls and now his mobility is impaired. He complained of nausea and feeling generally unwell. Albert decided to be admitted to hospital for investigations. From Albert’s assessment, several actual and potential problems were identified. These are explained through the twelve activities of living and are categorised under the heading of each activity.
Maintaining a safe environment .
Albert is unable to maintain a safe environment independently. He is at risk of falling due to impaired mobility and will require assistance to mobilise safely. There is a potential risk of infection from microorganisms found in hospitals. (Filetoth 2003).
Communicating
Albert was alert and orientated. He fully understood the reasons for his admission to hospital and asked many questions relating to his stay. He has no speech or hearing difficulties and wears glasses for reading.
Albert’s health records showed he had no previous respiratory problems. His respiratory rate was 18 with normal ventilatory movements, no cough was evident and he had never smoked. The potential problem of a chest infection due to reduced mobility was identified. Lung volume decreases in the recumbent position as the abdominal contents press up on the diaphragm limiting the range of movement. (Redfern and Ross 2001). This increases the risk of accumulation of secretions in the airways, which are a medium for bacterial growth. (Heath 2000a).
Eating and drinking
Albert has had a poor appetite; he felt nauseated and has lost interest in food in the last fortnight. He has restricted his fluid intake due to a recent problem of urinary frequency. Albert is 1.64m and weighs 48kg. His Body mass index is currently at 18, indicating he is underweight for his height. (Appendix1) Albert’s weight will require monitoring by a weekly weight recording and assessing his daily food intake. (Redfern and Ross 2001). Due to insufficient food consumption Albert may be undernourished and at risk of pressure sores. (Redfern and Ross 2001). Pressure sores develop when prolonged pressure is exerted on the skin, the pressure diminishes blood flow to the tissues that can devitalise and become susceptible to damage. (Alexander et al 2001). There is a potential problem of dehydration, which can cause constipation due to inadequate fluids. (Woodrow 2002), (Madden 2000).
Elimination
Albert has a problem of urinary frequency and occasional incontinence. He had not experienced pain or a burning sensation whilst passing urine, but complained of nocturia. This is a term to describe passing urine during the night. (Chasens and Umlauf 2003). A urinalysis test showed the presence of leucocytes, nitrites and blood in Albert’s urine. This indicates the presence of a urinary tract infection. (Heath 2000a), (Hope et al 1998). Albert’s normal bowel patterns are once daily and are usually soft and easy to pass. Unusually for Albert his bowels have not opened for approximately seven days and has been straining to defecate, he feels constipated. This can be due to his impaired mobility and lack of fluid and dietary fibre consumption. (Madden 2000).
Personal cleansing and dressing
Albert’s impaired mobility will reduce his ability in carrying out this activity safely and independently. He will require assistance to maintain a good standard of hygiene to prevent infection and skin problems. Albert’s skin is dry and discoloured, but remains intact. A pressure sore risk tool, the Waterlow scale showed Albert to be of high risk at 15. (Appendix 2). Kenworthy et al (2002) describe a pressure sore risk tool as a tool that identifies a risk of developing a pressure sore. Albert will require a pressure relieving mattress and regular observation of pressure areas.
Controlling body temperature
Albert had a raised temperature of 37.8C, the normal adult temperature is between 36 C- 37.5C. (Redfern and Ross 2001).The raise in temperature can indicate the presence of infection. (Alexander et al 2001). Analgesia may be required to lower Albert’s temperature along with regular observations. (Hope et al 1998).
Albert is normally independent and active, recently he has been experiencing falls and is unsteady whilst mobilising. He will require assistance of a nurse or a mobilator when mobilising and physiotherapy input. The use of a mobilator may cause a psychological problem by a loss of self-identity and self-worth. (Bourret et al 2002).There is a potential risk of the loss of joint motion known as joint contractures. When muscles are disused they shorten by fibrosis and joint fixations occur. (Larson 1999). Thrombo-embolism is a potential risk, as a slow or reduced flow of blood, due to reduced mobility, within the veins can lead to a deep vein thrombosis or a pulmonary embolism. (Seely et al 2002). A chest infection is a potential risk due to restricted respiratory movements. Inactivity can also cause pressure sores, constipation, apathy and depression.(Redfern and Ross 2001).
Working and playing
Albert is at risk of loneliness and anxiety as admission to hospital has altered his usual routine. Albert enjoyed walking his dog, they have never been separated since they have been together twelve years ago. Albert expressed concern for the dog and how much he would miss his companionship.
Expressing sexuality
Albert dressed appropriate to age and gender and was well groomed. Sexual activity was not discussed as Albert had stated that his wife was the only woman for him and he had no desire to meet anyone else. Marx oppressed cal1966’s structuralism idea.
Albert has a regular sleep pattern of seven hours per night, and has never required night sedation. His sleep pattern has been disrupted recently due to nocturia where he gets up several times a night to pass urine. Weber enveloped
Albert’s condition did not indicate that death was imminent. However he clearly expressed that he has no fear in dying as he looks forward to the day he can see his wife again.
The focus for the care plan is constipation, which was identified in the activity of ‘elimination’. I have chosen constipation as it has a significant impact on an individual’s physical, psychological and social well being.(Ross 1998). Norton (1996) defines constipation as decreased or difficult evacuation of dry, hard faeces that are painful to pass. It can be acute or chronic condition and bowel movements are less frequent than the individual’s normal.( Redfern and Ross 2001). Constipation is distressing, undignified and embarrassing; nurses approaching the subject require tact and sensitivity. (Whinney 1999), (Murray 1997).
The planning stage of the nursing process is setting realistic achievable goals and selecting nursing interventions to achieve these goals. (Alfaro-Lefevre 2002). Due to impaired mobility and an insufficient dietary fibre and fluid intake, Albert is suffering from constipation. Albert and I sat in private and I explained constipation, its causes, treatments and its prevention. Then we discussed and planned his care in which to rectify his constipation. It is imperative for patients to be involved in planning their care, it helps them to prevent and solve problems. It empowers them and compliance is more likely to be achieved. (Potter and Perry 2001).
Goals provide a focus for nursing interventions and determine the effectiveness of the interventions. (Heath 2000a). The short-term goals were for Albert’s bowels to move in 48 hours without difficulty and to increase his fluid intake by 1500mls daily. The long-term goals were for Albert to exhibit regular patterns of bowel elimination before discharge and for him to recognise measures that will prevent a recurrence.
Interventions Several interventions were identified following the plan and discussion with Albert, regarding his care. Albert will increase his physical activity, within his own limits, as activity stimulates peristalsis in the colon and increases muscle tone that facilitates voluntary contraction during defaecation.(Whinney 1999). Encourage an increase in fluid intake at least 1500mls daily, fluid liquifies intestinal contents, easing passage through the colon which help to prevent hard dry stools. (Whinney 1998). Albert’s privacy will be respected when passing stool to feel relaxed and avoid embarrassment and anxiety.(Schaefer and Cheskin 1998). Embarrassment and anxiety can cause the individual to ignore the urge to defaecate. (Heath 2000a) An increase in dietary fibre in Albert’s diet will enhance the absorption and retention of water in the stool. This will make the stool softer and pass easily. (Bottomley and Lewis 2003). Ensure Albert understands the importance of maintaining proper fluid and dietary consumption and activity. (Schaefer and Cheskin 1998).
Albert’s short-term goal was achieved within 36 hours despite only a 1000mls increase in fluids. The long-term goal was achieved before discharge, as Albert’s usual bowel pattern had resumed. He fully comprehended the measures to be taken to prevent a recurrence and implemented them with encouragement
Nursing models provide a framework to facilitate nurses in caring for patients effectively and consistently in the clinical setting. The ‘Elements of Nursing’ model guided me to collect relevant data in a systematic way, relating to the ‘activities of living’. It enabled some measurement such as a baseline to determine what point the patient was on the dependence – independence continuum and identify actual and potential problems. I found that the activities were interrelated and how one problem can link with another.
The assessment process is the beginning point for all nursing interventions and is an essential component of the nursing process. Developing a relationship with the patient is essential, good interpersonal skills are required in order for the patient to disclose personal information. I felt I had began to build up a relationship with Albert, he appeared keen to gave me the information I required and was not afraid to show his vulnerabilities. Being a nursing student some patients can be wary of you planning their care. Albert appeared to trust my judgement and capabilities, which gave me a sense of professional competence, confidence and sense of achievement.
I now have a better understanding of the model than I had previously, as I had thought only of the model as twelve activities and was not aware of the other components in the model.
Having an increased knowledge of the model, I can confidently apply it to practice and plan/deliver care more effectively.
...(download the rest of the essay above)
About this essay:
If you use part of this page in your own work, you need to provide a citation, as follows:
Essay Sauce, Assessment of a patient and plan of care . Available from:<https://www.essaysauce.com/coursework/present-a-plan-of-care/> [Accessed 04-04-24].
These Coursework have been submitted to us by students in order to help you with your studies.
* This essay may have been previously published on Essay.uk.com at an earlier date.
Essay Categories:
- Accounting essays
- Architecture essays
- Business essays
- Computer science essays
- Criminology essays
- Economics essays
- Education essays
- Engineering essays
- English language essays
- Environmental studies essays
- Essay examples
- Finance essays
- Geography essays
- Health essays
- History essays
- Hospitality and tourism essays
- Human rights essays
- Information technology essays
- International relations
- Leadership essays
- Linguistics essays
- Literature essays
- Management essays
- Marketing essays
- Mathematics essays
- Media essays
- Medicine essays
- Military essays
- Miscellaneous essays
- Music Essays
- Nursing essays
- Philosophy essays
- Photography and arts essays
- Politics essays
- Project management essays
- Psychology essays
- Religious studies and theology essays
- Sample essays
- Science essays
- Social work essays
- Sociology essays
- Sports essays
- Types of essay
- Zoology essays
Home — Essay Samples — Nursing & Health — Nursing Care Plan — Final Care Coordination Plan
Final Care Coordination Plan
- Categories: Nursing Care Plan
About this sample

Words: 722 |
Published: Jan 31, 2024
Words: 722 | Pages: 2 | 4 min read
Table of contents
Overview of the final care coordination plan, identification of the interdisciplinary team, assessment of the patient's needs, development of the care plan, implementation of the care plan, evaluation and monitoring of outcomes, communication and collaboration.
- Agency for Healthcare Research and Quality. (2014). Care coordination. https://www.ahrq.gov/ncepcr/care/coordination.html
- American College of Physicians. (2007). Care coordination in the medical neighborhood: Critical components of effective partnerships between patients , primary care physicians, and specialists. https://www.acponline.org/acp_policy/policies/care_coordination_in_the_medical_neighborhood_2013.pdf
- Institute of Medicine. (2003). Priority areas for national action: Transforming Health Care Quality. https://www.ncbi.nlm.nih.gov/books/NBK221455/

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr. Karlyna PhD
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
4 pages / 1739 words
1 pages / 582 words
1 pages / 498 words
3 pages / 1241 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Nursing Care Plan
A Better NHS. (2011). Patient autonomy and choice. Retrieved from 71-77.
Ball J. & Pike G. (2009). Shift length: A literature review. Nursing Management (Harrow), 16(4), 22-25.Bogossian, F., Winters-Chang, P., & Tuckett, A. (2014). Extended work shifts and the impact on patient safety, productivity, [...]
Program design and implementation play a critical role in shaping the delivery of healthcare services and improving patient outcomes. In this essay, we will explore the expertise of nurses in program design and implementation [...]
The Symitar Episys system is a core processing solution designed specifically for credit unions. It offers a wide range of features and capabilities to help credit unions manage their operations efficiently and effectively. In [...]
This essay will be exploring communication as an aspect of nursing care which is an indispensable skill in a role of service provision such as nursing. Through the development of fundamental mental health nursing skills and the [...]
Community health nurses play a vital role in the health and well-being of a community (Stanhope, Lancaster, Jakubec, & Pike-MacDonald, 2017). Thorough analysis of a community is foundational work done by the community health [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
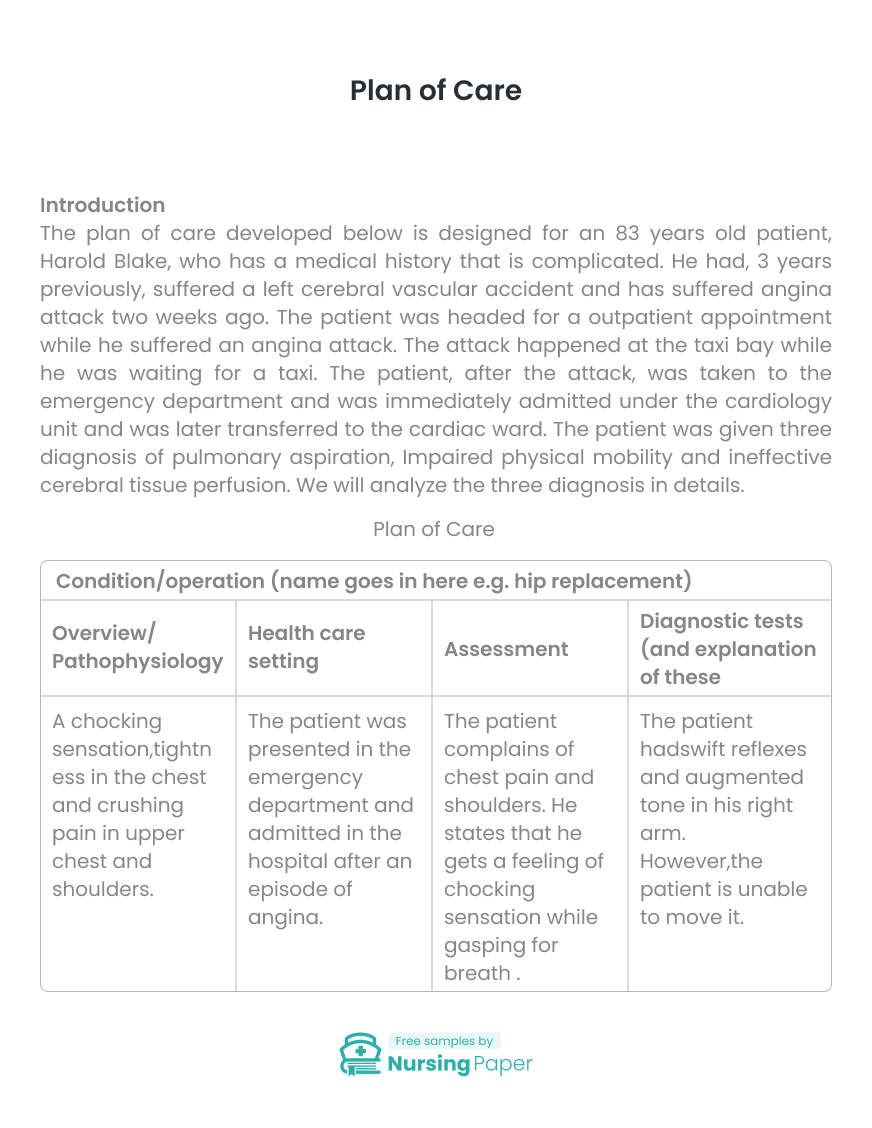
Plan of Care
Introduction, pulmonary aspiration, impaired physical mobility, ineffective cerebral tissue perfusion, legal and ethical consideration, inter-professional consideration.
The plan of care developed below is designed for an 83 years old patient, Harold Blake, who has a medical history that is complicated. He had, 3 years previously, suffered a left cerebral vascular accident and has suffered angina attack two weeks ago. The patient was headed for a outpatient appointment while he suffered an angina attack. The attack happened at the taxi bay while he was waiting for a taxi. The patient, after the attack, was taken to the emergency department and was immediately admitted under the cardiology unit and was later transferred to the cardiac ward. The patient was given three diagnosis of pulmonary aspiration, Impaired physical mobility and ineffective cerebral tissue perfusion. We will analyze the three diagnosis in details.

Pulmonary aspiration is the entry of materials from the gastrointestinal tract into the lower respiratory system. The foreign materials may be inhaled or delivered into the trachea system Nason, 2015). When pulmonary aspiration occurs during feeding, then it is considered as food going down the wrong pipe. Pulmonary aspiration symptoms include coughing, difficulty in breathing and in some cases the patient can exhibit signs of chocking. In our case, the patient, Harold Blake, upon admission showed the symptoms of choking, shortness of breath, crushing pain in the upper chest and chest tightness. The symptoms that the patient showed were similar to those of pulmonary aspiration and thus it was rational to diagnose the disease since it could be a possibility.
Impaired physical mobility is the restriction in the self-reliant physical motion of the body or one of the functions of the body. When impaired physical mobility happens, it can turn to be a complex health issue that involves different healthcare team. The happening of this disease continues to rise with the increase in the age of an individual. After discharge from hospitals in most cases, the patient is moved to a rehabilitation center or goes home with a physical therapy (Wu, Han, Xu, Lu, Cong, Zheng, & Sun, 2014). In this case, the patient had previously suffered a left cerebral vascular accident. Upon admission, the doctor had noted that he was drowsy, drooling, and is having difficulty speaking. Upon observation, the patient ’s right limbs were moderately weak and sluggish as compared to their left counterparts which were possible leads to impaired physical mobility.
1. Crawford A., & Harris, H. (2016). Caring for adults with impaired physical mobility. Nursing. 46, 36-41.
2. Green SM, Mason KP, & Krauss BS. (2017). Pulmonary aspiration during procedural sedation: a comprehensive systematic review. British Journal of Anaesthesia. 118, 344-354.
3. Hasanin, A., Mukhtar, A., & Nassar, H. (2017). Perfusion indices revisited. Journal of Intensive Care. 5.
4. Iskhandar Shah, L., & Christensen, M. (2012). Ineffective cerebral perfusion related to increased intracranial pressure secondary to subarachnoid haemorrhage: An examination of nursing interventions. Singapore Nursing Journal. 39, 15-24.
5. Manolis, A. J., Poulimenos, L. E., Ambrosio, G., Kallistratos, M. S., Lopez-Sendon, J., Dechend, R., Mancia, G., & Camm, A. J. (2016). Medical treatment of stable angina: A tailored therapeutic approach. International Journal of Cardiology. 220, 445-453.
6. Marik PE. (2011). Pulmonary aspiration syndromes. Current Opinion in Pulmonary Medicine. 17, 148-54.
7. Mckenna CJ, & Sugrue DD. (2015). The medical management of chronic stable angina. National Institute of Health 38, 131-136
8. Nason, K. S. (2015). Acute Intraoperative Pulmonary Aspiration. Thoracic Surgery Clinics. 25, 301-307.
- AACN Synergy Model
- Advanced Practice Nurse (ADN)
- American Nurses’ Association (ANA)
- Communication

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Qual Health Care
Person-centered care (PCC): the people’s perspective
Gro rosvold berntsen.
Norwegian Center for E-Health Research, University Hospital of North Norway, NSE, PB 35, Tromsø 9038, Norway
Institute of community medicine, UiT The Arctic University of Norway, Tromsø, UiT, PO Box 6050 Langnes, Tromsø N-9037, Norway
The Cochrane Collaboration, St. Albans House, 57-59 Haymarket, London SW1Y 4QX, UK
Reach to recovery, Israeli Cancer Association, St Revivim 7, Givatayim 5348505, Israel
Patient for Patient Safety, World Health Organization, Avenue Appia 20, Geneva 1211, Switzerl
The International Society for Quality in Healthcare (ISQua), Huguenot House, 35-38 St. Stephens Green, Dublin 2 D02 NY63 IE, Ireland
Morgan Chetty
Independent Practitioner Association Foundation (IPAF), 61 Juniper Road, Overport, Durban 4067, South Africa
Kwazulu-Natal Doctors Healthcare Coalition (KZNDHC), 61 Juniper Road, Overport, Durban 4067, South Africa
Carolyn Canfield
Department of Family Practice Faculty of Medicine, The University of British Columbia, Vancouver, 320 - 5950 University Blvd, British Columbia BC V6T 1Z3, Canada
Louis Ako-Egbe
Health System Strengthening Cluster, WHO Country Office, One UN House, PAP, 2nd Street Sinkor, Monrovia, Montserrado 1000, Liberia
University Medical Center, 215 Hồng Bàng, phường 11, Quận 5, Ho Chi Minh, Vietnam
Caitriona Curran
Isabela castro.
Global Patient & Family Advisory Board, The Beryl Institute, 831 12th Avenue South, #212, Nashville, Tennessee TN 37203, USA
Planetree International, 130 Division St, Derby, Connecticut CT 06418, USA
Associated Data
Not applicable.
Introduction
The call for person-centered care (PCC) is not new, yet despite a high priority over many decades and numerous frontline interventions, a lack of PCC persists [ 1 ]. We hypothesize that PCC will continue to be a secondary feature until PCC is a widely understood to be at the core of care quality.
Why is PCC important?
We have witnessed enormous progress in biomedical care. Yet, both patients and health professionals have repeatedly voiced a concern that health-care systems (HCSs) do not sufficiently respect the individuality and human dignity of persons who seek their help. Even though the intertwined nature of person and body is well understood, in understanding a health challenge, the professional often comes to disregard identity and personhood. Ignoring the person in the patient is a profoundly troubling phenomenon. It undermines mutual understanding, empathy, trust and co-production and threatens PCC’s favorable clinical outcomes [ 2 ].
What is PCC?
PCC is the art of embracing the patient as an equal partner in the design and co-production of care. PCC is a stepwise process following these concepts and principles:
- HCSs’ goal is to improve and maintain ‘health’ understood as a resource for ‘what matters’ to the person in their context and life [ 3 ].
- A patient journey (PJ) is the ensemble of care events organized by time across all diagnoses and providers to improve or maintain health for one patient. The PJ is the HCS core product [ 4 ].
- There are three roles in every PJ: the patient, the professional(s) and a governance/payer, hereafter ‘the PJ partners.’
- The governance/payer is an omnipresent third party, which shapes the PJ through design, funding and regulation of the HCS [ 5 ].
- Establish aim of PJ and concrete goals: a sensitive and empathic exploration of ‘what matters’ to the person [ 6 ], followed by a translation into relevant and realistic goals for care within professional, legal, ethical, and economic constraints set by governance/payer.
- Co-production: PJ partners co-produce PJ goals, plans, delivery and evaluation of care, in alignment with ‘what matters’.
- One person one plan: the professional(s) contribute condition-specific expertise and best practices across all conditions and help merge these into one care plan that serves PJ goals.
- Proactive care: care plans build on the strengths of the patient, include self-care and self-management, anticipate needs and seek to prevent costly clinical crises in both human and economic terms.
- Loyalty to plan: the PJ partners co-create care delivery according to the co-produced plan.
- Evaluation, learning, and adjustment: the PJ partners evaluate care plan, delivery and goal attainment, as often as needed, in light of ‘what matters’ to learn and adjust the PJ.
Why is it so hard?
Patients are persons who are already powerful in their lives. However, inherent features of health care contribute to disempowerment and distancing between patient and professionals, which results in incomplete professional knowledge of the person’s values, needs, preferences and context. The systematic focus on disease/condition/malfunction and professionally defined outcomes promote a paternalistic approach that may be distressing to the person [ 7 ]. Change relies on active identification of and counteraction against the depersonalizing side effects of professionalism.
Sustainable and lasting system change
Frontline health-care professionals who deliver PCC often do so because it is the ‘right thing to do,’ not because it is a system feature. Change requires explicit system attention to PCC.
Managing PCC means measuring and observing person centeredness. HCS must build patient-led evaluations of the PCC process at the individual and system levels, map disempowerment and de-personalization factors, complement measurements with user conversations and include those who belong to, or speak for, marginalized and vulnerable groups. These observations must be used actively in the plan for change.
Plan and do
Reconfigure HCS so that regulatory, funding, organizational and information systems leverage PCC. Information systems should document, share and link ‘what matters’ to care decisions and delivery, goal attainment and clinical outcomes. Train for co-production at micro, meso, and macro levels and use economic and regulatory feedback to boost PCC achievements. Share the good stories. Research effective interventions, including effects on outcomes for patients, professionals and payers.
Continuously evaluate and measure progress, cycling between Observe-Plan-Do-Adjust, until patients’ reports of high-quality PCC become the norm [ 8 ].
Conclusion—beacons of light
The current profession-centric HCS is built with the best of intentions but fails in terms of PCC. The paradigm change is already happening, as PCC emerges at the center of quality measurement [ 9 ] and care re-design [ 10 ]. In the new paradigm, care professionals are conscious of their role as “visitors” in the patient’s life. The patient is the host, guide and enabler of the healing journey. The goal is to enable the person to thrive in their life, with as little intervention from health care as possible.
Acknowledgements
We are truly grateful to the support from ISQUA and the Norwegian E-health research center, which made the work on this paper possible.
Contributor Information
Gro Rosvold Berntsen, Norwegian Center for E-Health Research, University Hospital of North Norway, NSE, PB 35, Tromsø 9038, Norway. Institute of community medicine, UiT The Arctic University of Norway, Tromsø, UiT, PO Box 6050 Langnes, Tromsø N-9037, Norway.
Sara Yaron, The Cochrane Collaboration, St. Albans House, 57-59 Haymarket, London SW1Y 4QX, UK. Reach to recovery, Israeli Cancer Association, St Revivim 7, Givatayim 5348505, Israel. Patient for Patient Safety, World Health Organization, Avenue Appia 20, Geneva 1211, Switzerl. The International Society for Quality in Healthcare (ISQua), Huguenot House, 35-38 St. Stephens Green, Dublin 2 D02 NY63 IE, Ireland.
Morgan Chetty, Independent Practitioner Association Foundation (IPAF), 61 Juniper Road, Overport, Durban 4067, South Africa. Kwazulu-Natal Doctors Healthcare Coalition (KZNDHC), 61 Juniper Road, Overport, Durban 4067, South Africa.
Carolyn Canfield, Department of Family Practice Faculty of Medicine, The University of British Columbia, Vancouver, 320 - 5950 University Blvd, British Columbia BC V6T 1Z3, Canada.
Louis Ako-Egbe, The International Society for Quality in Healthcare (ISQua), Huguenot House, 35-38 St. Stephens Green, Dublin 2 D02 NY63 IE, Ireland. Health System Strengthening Cluster, WHO Country Office, One UN House, PAP, 2nd Street Sinkor, Monrovia, Montserrado 1000, Liberia.
Phuk Phan, University Medical Center, 215 Hồng Bàng, phường 11, Quận 5, Ho Chi Minh, Vietnam.
Caitriona Curran, The International Society for Quality in Healthcare (ISQua), Huguenot House, 35-38 St. Stephens Green, Dublin 2 D02 NY63 IE, Ireland.
Isabela Castro, Independent Practitioner Association Foundation (IPAF), 61 Juniper Road, Overport, Durban 4067, South Africa. Global Patient & Family Advisory Board, The Beryl Institute, 831 12th Avenue South, #212, Nashville, Tennessee TN 37203, USA. Planetree International, 130 Division St, Derby, Connecticut CT 06418, USA.
This work was supported by the Norwegian Center for e-health research, at the University Hospital of North Norway and The International Society for Quality in health care (ISQUA).
Data availability
Contributorship.
The authors are all members of the International Society for Quality in health care (ISQUA) working group for a white paper on PCC. All authors have contributed to the original idea and content for the paper. The first author (G.R.B.) Berntsen is the guarantor of the manuscript. She has written up drafts, circulated the manuscript to co-authors and collected feedback in regular meetings with co-authors. All authors and have read the last version of the manuscript.
Shedding Light on Healthcare Algorithmic and Artificial Intelligence Bias
Impact of artificial intelligence in contemporary medicine.
When people go to a medical facility for help, they expect the doctor to make appropriate health decisions for their optimal health and outcome.
Doctors and other health care providers are increasingly using healthcare algorithms (a computation, often based on statistical or mathematical models, that helps medical practitioners make diagnoses and decisions for treatments) and artificial intelligence (AI) , to diagnose patient illnesses, suggest treatments, predict health risks, and more. In some cases, this is fine. However, using healthcare algorithms and AI can sometimes worsen things for people from certain ethnic or racial groups. This is because algorithms and AI are based on data from one set of the population that may not work well for others.
Awareness of Bias
Healthcare algorithms and AI bias can contribute to existing health disparities for certain populations based on race, ethnicity, gender, age, or other demographic factors.
One reason for healthcare algorithm and AI bias is the lack of diversity in the data used to train computer programs. It is important to use data from patients with diverse demographic factors when creating AI computer programs to ensure the algorithm works well for everyone.
Another way bias can enter healthcare algorithms and AI is through the assumptions made by the people who create them. For example, if developers assume that some symptoms are more common in non-Hispanic White women than in Black/African American women. This can lead to algorithms producing unfair or inaccurate results for Black/African American women with those symptoms.
A Case Study
If a woman has had a cesarean delivery, also known as a C-section, there is a chance that a subsequent delivery can be attempted through a vaginal birth, which is known as Vaginal Birth after Cesarean Delivery or VBAC. However, there are known risks associated with attempting VBAC, such as uterine rupture or other complications.In 2007, the VBAC algorithm was designed to help healthcare providers assess the likelihood of safely giving birth through vaginal delivery. The algorithm considers many things, such as the woman's age, the reason for the previous C-section, and how long ago it happened. However, in 2017, in a study by Vyas, et al., researchers found the original algorithm was not correct. It predicted that Black/African American and Hispanic/Latino women were less likely to have a successful vaginal birth after a C-section than non-Hispanic White women. This caused doctors to perform more C-sections on Black/African American and Hispanic/Latino women than on White women.
After years of work by researchers, advocates, and clinicians, changes were made to the algorithm. The new version of the algorithm no longer considers race or ethnicity when predicting the risk of complications from VBAC. This means that doctors can make decisions based on more accurate and impartial information that works for all women, providing more equitable care regardless of race or ethnicity. To access more information about this case study, visit: Challenging the Use of Race in the Vaginal Birth after Cesarean Section Calculator .
The Treatment Plan for Bias
There are best practices that healthcare data scientists and developers can incorporate to address the challenges of using algorithms and AI. These include:
- Have a more diverse body of people review and supervise the algorithms and AI.
- Use methods or techniques to best manage situations where there is not enough information available, like using synthetic data.
- Work with diverse communities to ensure the algorithms are helpful and don't cause harm.
- Introduce the algorithms gradually and carefully instead of all at once.
- Create ways for people to provide feedback and improve the algorithms over time.
- Involve diverse members of your workforce in developing the algorithms and validating patient data from various racial and ethnic backgrounds.
The Office of Minority Health (OMH) is focused on helping to reduce differences in health outcomes, known as health disparities, for racial and ethnic minority populations and American Indian and Alaska Native communities. By encouraging equity in the lifecycle of algorithms and AI, OMH and other federal agencies aim to lower the risk of bias and improve healthcare outcomes for everyone.
The Center for Open Data Enterprise (CODE). (2019). Sharing And Utilizing Health Data for A.I. Applications: Roundtable Report . U.S. Department of Health and Human Services. https://www.hhs.gov/sites/default/files/sharing-and-utilizing-health-data-for-ai-applications.pdf
U.S. Government Accountability Office & The National Academy of Medicine. (2020). Artificial Intelligence in Health Care Benefits and Challenges of Technologies to Augment Patient Care . U.S. Government Accountability Office, Science, Technology Assessment, and Analytics. https://www.gao.gov/assets/gao-21-7sp.pdf
United States Department of Health and Human Services (HHS) (2022). Artificial Intelligence (AI) at HHS. Retrieved from: https://www.hhs.gov/about/agencies/asa/ocio/ai/index.html
Davenport, and Kalakota (2019). The potential for artificial intelligence in healthcare. Free article: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6616181/
Bohr, and Memarzadeh (2020). The rise of artificial intelligence in healthcare applications. Free article: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7325854/
Norori, et al. (2021). Addressing bias in big data and AI for health care: A call for open science. Free article: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8515002/
National Institute for Health Care Management (NIHCM) Foundation (2021). Racial Bias in Health Care Artificial Intelligence. Free article: https://nihcm.org/publications/artificial-intelligences-racial-bias-in-health-care
Jackson, M. C. (2021). Artificial Intelligence & Algorithmic Bias: The Issues with Technology Reflecting History & Humans. Journal of Business, 19. Free article: https://digitalcommons.law.umaryland.edu/cgi/viewcontent.cgi?article=1335&context=jbtl
Harris, L. A. (2021). Artificial Intelligence: Background, Selected Issues, and Policy Considerations. Congressional Research Service. https://crsreports.congress.gov/product/pdf/R/R46795
Huang, J., Galal, G., Etemadi, M., & Vaidyanathan, M. (2022). Evaluation and Mitigation of Racial Bias in Clinical Machine Learning Models: Scoping Review. JMIR Medical Informatics, 10(5), e36388. Free PMC article: http://www.ncbi.nlm.nih.gov/pmc/articles/pmc9198828/
Schwartz, R., Vassilev, A., Greene, K., Perine, L., Burt, A., & Hall, P. (2022). Towards a Standard for Identifying and Managing Bias in Artificial Intelligence. U.S. Department of Commerce, National Institute of Standards and Technology. https://nvlpubs.nist.gov/nistpubs/SpecialPublications/NIST.SP.1270.pdf
Bernstam, E. V., Shireman, P. K., Meric-Bernstam, F., N. Zozus, M., Jiang, X., et al. (2022). Artificial Intelligence in Clinical and Translational Science: Successes, Challenges, and Opportunities. Clinical and Translational Science, 15(2), 309–321. Free PMC article: http://www.ncbi.nlm.nih.gov/pmc/articles/pmc8841416/
Marcus, J. L., Sewell, W. C., Balzer, L. B., & Krakower, D. S. (2020). Artificial Intelligence and Machine Learning for HIV Prevention: Emerging Approaches to Ending the Epidemic. Current HIV/AIDS Reports, 17(3), 171–179. Free PMC article: http://www.ncbi.nlm.nih.gov/pmc/articles/pmc7260108/
Solomonides, A. E., Koski, E., Atabaki, S. M., Weinberg, S., Mcgreevey, J. D., et al. (2022). Defining AMIA’s Artificial Intelligence Principles. Journal of the American Medical Informatics Association (JAMIA), 29(4), 585–591.
Lee, E. W. J., & Viswanath, K. (2020). Big Data in Context: Addressing the Twin Perils of Data Absenteeism and Chauvinism in the Context of Health Disparities Research. Journal of Medical Internet Research, 22(1), e16377. Free PMC article: http://www.ncbi.nlm.nih.gov/pmc/articles/pmc6996749/
Lin, S. (2022). A Clinician’s Guide to Artificial Intelligence (AI): Why and How Primary Care Should Lead the Health Care AI Revolution. Journal of the American Board of Family Medicine, 35(1), 175. Free article: https://doi.org/10.3122/jabfm.2022.01.210226
Nadkarni, P. M., Ohno-Machado, L., & Chapman, W. W. (2011). Natural Language Processing: An Introduction. Journal of the American Medical Informatics Association (JAMIA), 18(5), 544–551. Free PMC article: http://www.ncbi.nlm.nih.gov/pmc/articles/pmc3168328/
Vyas, Jones, Meadows, et al. (2019). Challenging the Use of Race in the Vaginal Birth after Cesarean Section Calculator. Free PMC article: https://pubmed.ncbi.nlm.nih.gov/31072754/

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
HHS Releases White Paper Focused on Preventing Drug Shortages
Today, the U.S. Department of Health and Human Services (HHS) released a white paper highlighting steps HHS has taken to prevent and mitigate drug shortages and proposing additional solutions for policymakers to consider. Drug shortages have occurred in the nation’s health care system for several decades, largely due to market failures and misaligned incentives. With today’s white paper, HHS offers solutions and stands ready to work with Congress to ensure no patient faces the devastating consequences of drug shortages or goes without needed medicines.
“All across our Department, we are working to ensure that millions of Americans will have access to medication, treatment, and services that save lives and improve health outcomes. That’s why advancing and implementing solutions to the nation’s drug shortages are so important, and why we want members of Congress and all actors in the supply chain to consider and act on the policy options presented in today’s white paper,” said HHS Secretary Xavier Becerra.
Through the Assistant Secretary for Planning and Evaluation (ASPE), Administration for Strategic Preparedness and Response (ASPR), the Food and Drug Administration (FDA), the Centers for Medicare & Medicaid Services (CMS), and others, HHS has been working to improve how the department monitors the pharmaceutical supply chain and responds to disruptions. HHS has established a new Supply Chain Resilience and Shortage Coordinator role to strengthen implementation of strategies to enhance supply chain resilience for pharmaceuticals and other medical products, and has issued guidance to increase supply chain transparency, while continuing to consider additional long and short-term solutions. FDA discloses certain inspection information to provide the public with an understanding of actions the Agency takes to protect public health and is also developing a quality management maturity framework that may support adoption of manufacturing practices that are more resilient. HHS has also collaborated with other government agencies on this critical issue. For example, last month HHS and the Federal Trade Commission jointly issued a Request for Information to better understand the causes – and potential solutions – of generic drug shortages.
HHS has also taken steps to increase resilience and redundancy within the market. This work includes supporting domestic manufacturing of key ingredients and drugs to address various vulnerabilities. ASPR has invested $500 million to date to support active pharmaceutical ingredient (API) manufacturing, and is exploring how it can utilize new authorities authorized by the President last year to promote the onshoring of essential medicines, medical countermeasures, and their critical ingredients. Moreover, HHS is developing policies to foster resiliency by considering Medicare payments, and additional requirements, to support a more diverse supply chain.
While the above progress is important, HHS concludes that effective longer-term solutions may require additional authorities and resources to align market incentives in order to reward investment in supply chain resilience. Developing and implementing a Manufacturer Resiliency Assessment Program and a Hospital Resilient Supply Program will advance us toward these goals.
Today’s white paper outlines how these programs could operate and help address the broader market issues that lead to drug shortages. The white paper focuses on the generic sterile injectable (GSI) drugs that form the basic layer of hospital care and make up the majority of shortages – which occur across therapeutic areas. However, HHS recognizes that these challenges affect other medical products, and expects the concepts and solutions that this white paper discusses may be relevant for other markets as well.
Key highlights of the white paper include:
- Drug shortages impact patients, families, caregivers, pharmacists, hospitals, nursing homes, hospices, and other individuals and entities across the health care system.
- Drug shortages are a decades-old problem arising, in part, from market forces that touch stakeholders across the drug supply chain—providers and pharmacies, manufacturers, and the middlemen in the system. Key issues include a broad lack of transparency, concentration among middlemen, and prices for generic drugs that are driven to levels so low that they create insufficient incentives for redundancy or resilience-oriented manufacturing, distribution, and purchasing. These market failures lead to pharmaceutical supply chains that are brittle, disruption-prone, and too slow to recover from shortages.
- Supply chain resilience involves fostering processes that are less likely to face disruptions, as well as establishing the ability to withstand and mitigate disruptions so their impact—when they occur—is limited. This resilience also comes from diversification of supply—both in redundancy of manufacturing capacity and a balance of domestic and diversified foreign sourcing—and the presence of reliable, efficient, and sustainable, robust manufacturing practices.
- HHS has made significant strides in shoring up the system’s ability to respond to shortages. Nevertheless, more impactful and enduring solutions require additional statutory authorities and funding to resolve underlying causes of shortages. All supply chain participants play a part in these solutions.
- This paper describes policy concepts for consideration, including collaboration with the private sector to develop and implement a Manufacturer Resiliency Assessment Program (MRAP) and a Hospital Resilient Supply Program (HRSP). As described, the combination of these programs would bring transparency into the market, link purchasing and payment decisions to supply chain resilience practices, and incentivize investments in supply chain resilience and diversification in the supply chain—including domestic manufacturing—at a scale that would drive impactful change in the market. This paper focuses on generic sterile injectable medicines used in inpatient settings, given their importance to acute inpatient care, and their relative risk of supply disruptions—though HHS recognizes that these challenges affect other products, and therefore, the solutions described here may be applicable in other markets.
The white paper, “Policy Considerations to Prevent Drug Shortages and Mitigate Supply Chain Vulnerabilities in the United States”, is available at https://aspe.hhs.gov/reports/preventing-shortages-supply-chain-vulnerabilities .
Sign Up for Email Updates
Receive the latest updates from the Secretary, Blogs, and News Releases
Subscribe to RSS
Receive latest updates

Related News Releases
Readout of biden-harris administration convening with health care community concerning cyberattack on change healthcare, letter to health care leaders on cyberattack on change healthcare, health resources and services administration takes historic new steps to transform the organ transplant system to better serve patients, related blog posts.

Reflecting on Cybersecurity Awareness Month
The u.s. department of health and human services is taking action to strengthen primary care, navigating section 752: insights from program managers on success, challenges, and tools for change, media inquiries.
For general media inquiries, please contact [email protected] .
Mobile Menu Overlay
The White House 1600 Pennsylvania Ave NW Washington, DC 20500
FACT SHEET: White House Task Force on Reproductive Healthcare Access Announces New Actions and Marks the 51st Anniversary of Roe v. Wade
Biden-Harris Administration Announces New Actions to Help Strengthen Access to Contraception, Protect Access to Medication Abortion, and Ensure Patients Receive Emergency Medical Care
Today, on what would have been the 51st anniversary of Roe v. Wade , women’s health and lives hang in the balance due to extreme state abortion bans. These dangerous state laws have caused chaos and confusion, as women are being turned away from emergency rooms, forced to travel hundreds of miles, or required to go to court to seek permission for the health care they need. In the face of the continued threats to reproductive freedom, President Biden will convene the fourth meeting of the Task Force on Reproductive Healthcare Access, where agencies will announce new actions to protect access to reproductive health care. The Task Force will also hear directly from physicians who are on the frontlines of the fallout from the overturning of Roe v. Wade . Also today, the Vice President is launching her nationwide Fight for Reproductive Freedoms tour to continue fighting back against extreme attacks throughout America. During the Task Force meeting, members will report on ongoing implementation of the President’s three Executive Orders and a Presidential Memorandum on access to reproductive health care and announce new steps to:
- Strengthen Contraception Access and Affordability for Women with Private Health Insurance. The Administration is committed to ensuring that women have access to contraception—an essential component of reproductive health care that has only become more important in the wake of the Supreme Court’s decision to overturn Roe v. Wade —and reducing barriers that women face in accessing contraception prescribed by their provider. The Departments of the Treasury, Labor, and Health and Human Services (HHS) are issuing new guidance to clarify standards and support expanded coverage of a broader range of FDA-approved contraceptives at no cost under the Affordable Care Act. This action builds on the progress already made by the Affordable Care Act to expand access to affordable contraception for millions of women nationwide. In addition, the Office of Personnel Management will strengthen access to contraception for federal workers, retirees, and family members by issuing guidance to insurers participating in the Federal Employee Health Benefits Program that incorporates the Departments’ guidance. OPM will also newly require insurers that participate in the Federal Employee Health Benefits Program to take additional steps to educate enrollees about their contraception benefits.
- Reinforce Obligations to Cover Affordable Contraception. The Secretary of HHS is issuing a letter to private health insurers, state Medicaid and Children’s Health Insurance Programs, and Medicare plans about their obligations to cover contraception for those they serve. The letter targets a wide range of payers to advance compliance with existing standards and underscore the Administration’s commitment to ensuring that women across the country can access affordable contraception. The letter also highlights recent HHS action to expand coverage and improve payment for contraceptives for Medicare beneficiaries, improving access for women with disabilities.
- Educate Patients and Health Care Providers on Their Rights and Obligations for Emergency Medical Care. The Administration is committed to helping ensure all patients, including women who are experiencing pregnancy loss and other pregnancy-related emergencies, have access to emergency medical care required under the Emergency Medical Treatment and Labor Act (EMTALA). The Administration has long taken the position that the required emergency care can, in some circumstances, include abortion care. The Department of Justice (DOJ) is defending that interpretation of the law before the Supreme Court, which is expected to rule by June. To increase awareness of EMTALA and improve the procedures for ensuring that patients facing all types of medical emergencies receive the care to which they are entitled, HHS is announcing today a comprehensive plan to educate all patients about their rights and to help ensure hospitals meet their obligations under federal law. This effort will include the launch of new accessible and understandable resources about rights and protections for patients under EMTALA and the process for submitting a complaint. HHS will also disseminate training materials for health care providers and establish a dedicated team of experts who will increase the Department’s capacity to support hospitals and providers across the country in complying with federal requirements—to help ensure that every patient receives the emergency medical care required under federal law.
- Protect Access to Safe and Legal Medication Abortion. One year ago today, President Biden issued a Presidential Memorandum directing further efforts to support patients, providers, and pharmacies who wish to legally access, prescribe, or provide medication abortion—including by taking steps to safeguard their safety and security. Today, the Department of Health and Human Services, the Department of Justice, and the Department of Homeland Security will report on their implementation of this Presidential Memorandum, including the resources they have disseminated to health care providers, including pharmacies, to support safe access to legal medication abortion.
Today’s announcements build on the Administration’s strong record of taking action since the Supreme Court’s decision to overturn Roe v. Wade . These ongoing efforts to defend reproductive rights include: Protecting Access to Abortion, including Medication Abortion
- Defend FDA Approval of Medication Abortion in Court. The Food and Drug Administration (FDA) and DOJ are defending access to mifepristone—a safe and effective drug used in medication abortion that FDA first approved more than twenty years ago—and FDA’s independent, expert judgment in court, including in a lawsuit before the Supreme Court that attempts to curtail access nationwide. The Administration will continue to stand by FDA’s decades-old approval and regulation of the medication and by FDA’s ability to review, approve, and regulate a wide range of prescription medications. Efforts to impose outdated restrictions on mifepristone would limit access to reproductive health care in every state in the country.
- Protect Access to Safe and Legal Medication Abortion. On what would have been the 50th anniversary of Roe v. Wade , President Biden issued a Presidential Memorandum directing agencies to consider further efforts to protect access to medication abortion. This Presidential Memorandum was issued in the face of attacks by state officials to prevent women from accessing mifepristone and discourage pharmacies from becoming certified to dispense the medication. These attacks followed independent, evidence-based action taken by FDA to allow mifepristone to continue to be prescribed by telehealth and sent by mail as well as to enable interested pharmacies to become certified.
- Partner with State Leaders on the Frontlines of Abortion Access. The White House continues to partner with leaders on the frontlines of protecting access to abortion—both those fighting extreme state legislation and those advancing proactive policies to protect access to reproductive health care, including for patients who are forced to travel out of state for care. The Vice President has led these efforts, traveling to 20 states and meeting with more than 250 state legislators, health care providers, and advocates in the past year. Today, she is kicking off her nationwide Fight for Reproductive Freedoms tour in Wisconsin.
- Ensure Access to Emergency Medical Care. Republican elected officials in states across the country have put women’s lives at risk by banning abortion even when her doctor determines that an abortion is necessary to prevent serious health consequences. The Administration is committed to ensuring all patients, including women who are experiencing pregnancy loss and other pregnancy-related emergencies, have access to the full rights and protections for emergency medical care afforded under federal law—including abortion care when that is the stabilizing treatment required. HHS issued guidance and Secretary Becerra sent letters to providers affirming the Administration’s view that EMTALA preempts conflicting state law restricting access to abortion in emergency situations. The Department of Justice has taken action defend and enforce these protections in court, including in a case currently before the Supreme Court.
- Provide Access to Reproductive Health Care for Veterans. The Department of Veterans Affairs (VA) issued an interim final rule to allow VA to provide abortion counseling and, in certain circumstances, abortion care to veterans and VA beneficiaries. VA provides abortion services when the health or life of the patient would be endangered if the pregnancy were carried to term or when the pregnancy is a result of rape or incest. When working within the scope of their federal employment, VA employees may provide abortion services as authorized by federal law regardless of state restrictions. DOJ will support and provide representation to any VA providers whom states attempt to prosecute for violations of state abortion laws where those providers were appropriately carrying out their duties under VA’s interim final rule.
- Support Access to Care for Service Members. The Department of Defense (DoD) has taken action to ensure that Service members and their families can access reproductive health care and that DoD health care providers can operate effectively. DoD has released policies to support Service members and their families’ ability to travel for lawful non-covered reproductive health care and to bolster Service members’ privacy and afford them the time and space needed to make personal health care decisions.
- Defend Reproductive Rights in Court. DOJ created a Reproductive Rights Task Force, which monitors and evaluates state and local actions that threaten to infringe on federal protections relating to the provision or pursuit of reproductive health care, impair women’s ability to seek abortion care where it is legal, impair individuals’ ability to inform and counsel each other about the care that is available in other states, ban mifepristone based on disagreement with FDA’s expert judgment about its safety and efficacy, or impose criminal or civil liability on federal employees who provide legal reproductive health services in a manner authorized by federal law.
Supporting Women’s Ability to Travel for Medical Care
- Defend the Right to Travel. On the day of the Supreme Court’s decision to overturn Roe v. Wade , President Biden reaffirmed the Attorney General’s statement that women must remain free to travel safely to another state to seek the care they need. In November 2023, DOJ filed a statement of interest in two lawsuits challenging the Alabama Attorney General’s threat to prosecute people who provide assistance to women seeking lawful out-of-state abortions. DOJ explained that the threatened Alabama prosecutions infringe the constitutional right to travel and made clear that states may not punish third parties for assisting women in exercising that right. DOJ continues to monitor states’ efforts to restrict the constitutional right to travel across state lines to receive lawful health care.
- Support Patients Traveling Out of State for Medical Care. HHS issued a letter to U.S. governors inviting them to apply for Section 1115 waivers to expand access to care under the Medicaid program for women traveling from a state where reproductive rights are under attack and women may be denied medical care. HHS continues to encourage state leaders to consider and develop new waiver proposals that would support access to reproductive health care services.
Safeguarding Access to Contraception
- Following FDA’s approval of the first daily oral contraceptive in the United States without a prescription, the Departments of the Treasury, Labor, and HHS issued a Request for Information to solicit public input on how to best ensure coverage and access to over-the-counter preventive services, including contraception, at no cost and without a prescription from a health care provider.
- Vice President Harris and the Department of Education convened representatives from 68 college and university leaders in 32 states to hear promising strategies from leaders of postsecondary institutions for protecting and expanding access to contraception for their students and on campus.
- The Gender Policy Council, Domestic Policy Council, and leaders from the Departments of the Treasury, Labor, and HHS convened private sector leaders to stress the need to continue to build on the significant progress already made under the Affordable Care Act in expanding access to contraception and call on participants to take robust additional actions to improve access.
- The Health Resources and Services Administration proposed new data measures for federally funded health centers that, once finalized, will help ensure that patients are screened for contraception needs. Screening and data measures will help enhance the overall delivery of voluntary family planning and related services, which is a required primary health care service under federal law.
- The Office of Personnel Management launched a public education campaign to highlight contraception benefits available to federal employees and their family members.
- HHS is continuing its public-private partnership to expand access to contraception with Upstream, a national nonprofit organization that provides health centers with free patient-centered, evidence-based training and technical assistance to eliminate provider-level barriers to offering the full range of contraceptive options. To date, HHS has connected Upstream to nearly 100 health care clinics, resulting in partnerships that will help Upstream accelerate their national expansion to reach 5 million women of reproductive age every year.
- Clarify Protections for Women with Private Health Insurance. Under the Affordable Care Act, most private health plans must provide coverage for contraception and family planning counseling with no out-of-pocket costs. The Departments of the Treasury, Labor, and HHS convened a meeting with health insurers and employee benefit plans. These agencies called on the industry to meet their obligations to cover contraception as required under the law. Following this conversation, these agencies issued guidance to clarify protections for contraceptive coverage under the Affordable Care Act.
- Expand Access Under the Affordable Care Act. The Departments of the Treasury, Labor, and HHS proposed a rule to strengthen access to contraception under the Affordable Care Act so all women with private health coverage who need and want contraception can obtain it without cost sharing. Millions of women have already benefited from this coverage, which has helped them save billions of dollars on contraception.
- Support Title X Clinics. Last year, HHS provided $263 million to over 4,000 Title X clinics across the country to provide a wide range of voluntary, client-centered family planning and related preventive services. The Title X Family Planning Program remains a critical part of the nation’s safety net, providing free or low-cost services for 2.6 million clients in 2022.
- Promote Access to Contraception for Service Members and Their Families and Certain Dependents of Veterans. To improve access to contraception at military hospitals and clinics, DoD expanded walk-in contraceptive care services for active-duty Service members and other Military Health System beneficiaries, and eliminated TRICARE copays for certain contraceptive services. And VA proposed a rule to eliminate out-of-pocket costs for certain types of contraception through the Civilian Health and Medical Program of the Department of Veterans Affairs.
Promoting Safety and Security of Patients, Providers, and Clinics
- Promote Safety and Security of Patients, Providers and Clinics. DOJ continues to robustly enforce the Freedom of Access to Clinic Entrances Act, which protects the right to access and provide reproductive health services.
Safeguarding Privacy and Sensitive Health Information
- Strengthen Reproductive Health Privacy under HIPAA. HHS issued a proposed rule to strengthen privacy protections under the Health Insurance Portability and Accountability Act (HIPAA). As proposed, this rule would prevent an individual’s information from being disclosed to investigate, sue, or prosecute an individual, a health care provider, or a loved one simply because that person sought, obtained, provided, or facilitated legal reproductive health care, including abortion. By safeguarding sensitive information related to reproductive health care, the rule will strengthen patient-provider confidentiality and help health care providers give complete and accurate information to patients. Prior to the proposed rule , HHS issued guidance reaffirming HIPAA’s existing protections for the privacy of individuals’ protected health information.
- Take Action Against Illegal Use and Sharing of Sensitive Health Information. The Federal Trade Commission (FTC) has committed to enforcing the law against illegal use and sharing of highly sensitive data, including information related to reproductive health care. Consistent with this commitment, the FTC has taken several enforcement actions against companies for disclosing consumers’ personal health information, including highly sensitive reproductive health data , without permission.
- Help Consumers Protect Their Personal Data. The Federal Communications Commission (FCC) launched a new guide for consumers on best practices for protecting their personal data, including geolocation data, on mobile phones. The guide follows a Notice of Proposed Rulemaking issued by FCC that would strengthen data breach rules to provide greater protections to personal data. Separately, HHS issued a how-to guide for consumers on steps they can take to better protect their data on personal cell phones or tablets and when using mobile health apps, like period trackers, which are generally not protected by HIPAA.
- Protect Students’ Health Information. ED issued guidance to over 20,000 school officials to remind them of their obligations to protect student privacy under the Family Educational Rights and Privacy Act (FERPA). The guidance helps ensure that school officials—at federally funded school districts, colleges, and universities—know that, with certain exceptions, they must obtain written consent from eligible students or parents before disclosing personally identifiable information from students’ educational records, which may include student health information. The guidance encourages school officials to consider the importance of student privacy, including health privacy, with respect to disclosing student records. ED also issued a know-your-rights resource to help students understand their privacy rights for health records at school.
- Safeguard Patients’ Electronic Health Information. HHS issued guidance affirming that doctors and other medical providers can take steps to protect patients’ electronic health information, including their information related to reproductive health care. HHS makes clear that patients have the right to ask that their electronic health information generally not be disclosed by a physician, hospital, or other health care provider. The guidance also reminds health care providers that HIPAA’s privacy protections apply to patients’ electronic health information.
Reinforcing Nondiscrimination Protections under Federal Law
- Protect Students from Discrimination Based on Pregnancy. The Department of Education (ED) released a resource for universities reiterating their responsibilities not to discriminate on the basis of pregnancy or pregnancy-related conditions, including termination of pregnancy. This guidance reminds schools of their existing and long-standing obligations under Title IX.
- Strengthen Nondiscrimination in Healthcare. HHS issued a proposed rule to strengthen nondiscrimination in health care. The proposed rule would implement Section 1557 of the Affordable Care Act and affirms protections consistent with President Biden’s Executive Orders on nondiscrimination based on sexual orientation and gender identity.
Providing Access to Accurate Information and Legal Resources
- Ensure Easy Access to Reliable Information. HHS launched and maintains ReproductiveRights.gov , which provides timely and accurate information on people’s right to access reproductive health care, including contraception, abortion services, and health insurance coverage, as well as how to file a patient privacy or nondiscrimination complaint . DOJ also launched justice.gov/reproductive-rights, a webpage that provides a centralized online resource on the Department’s ongoing work to protect access to reproductive health care services under federal law.
- Hosted a Convening of Lawyers in Defense of Reproductive Rights. DOJ and the Office of White House Counsel convened more than 200 lawyers and advocates from private firms, bar associations, legal aid organizations, reproductive rights groups, and law schools across the country for a convening of pro-bono attorneys, as directed in the first Executive Order. Following this convening, reproductive rights organizations launched the Abortion Defense Network to offer abortion-related legal defense services, including legal advice and representation.
Promote Research and Data Collection
- Use Data to Track Impacts on Access to Care. HHS convened leading experts to discuss the state of existing reproductive health research and what the data tells us about the impact of the overturning of Roe v. Wade , as well as the future of research on reproductive health care access. These convenings helped identify research gaps, opportunities for collaboration, and ways to bolster research efforts for both Federal agencies and external partners.
Stay Connected
We'll be in touch with the latest information on how President Biden and his administration are working for the American people, as well as ways you can get involved and help our country build back better.
Opt in to send and receive text messages from President Biden.

Bernie Sanders, Biden share plan to cut 'outrageous' health care costs
President Joe Biden was joined by Sen. Bernie Sanders at the White House Wednesday to highlight the administration's efforts to lower health care costs for Americans.
The remarks were at an official event, but came as Biden makes cracking down on corporate greed and relieving financial burdens for American families a key pillar of his 2024 reelection campaign.
"You and I have been fighting this for 25 years," Biden said to Sanders. "Finally, we beat Big Pharma, finally."
The support from Sanders, Biden's rival for the Democratic nomination in 2020, comes as Biden faces mounting anger from the party's progressive wing over his handling of the Israel-Hamas war . Reporters attempted to shout questions at Biden about Gaza and the Israeli strike that killed World Central Kitchen aid workers in the strip, but he did not take any questions.
Sanders opened his remarks Wednesday by saying Americans are united, regardless of political affiliation, in being "sick and tired of paying, by far, the highest prices in the world for prescription drugs."
"Here is some good news, despite all of the incredible wealth and political power of the pharmaceutical industry … despite all of that, the Biden administration and Democrats in Congress are beginning to make some progress," the independent senator said.
Among the accomplishments highlighted by Biden and Sanders were the Inflation Reduction Act provisions capping insulin costs at $35 for Medicare patients and out-of-pocket spending on brand-name drugs for Medicare beneficiaries to $2,000 yearly.
They also touted the ability of Medicare, for the first time, to negotiate with pharmaceutical companies on the price of certain prescription drugs.
"Not one Republican in the entire Congress -- it surprised me, I have to admit to you -- not one single Republican voted for it," Biden said of the Inflation Reduction Act. "Not one single one to give us authority to take on and beat Big Pharma."
He also took several swipes at congressional Republicans and his "predecessor" for their views on Social Security, the Affordable Care Act, the national deficit, abortion access and more. Without saying Donald Trump's name, he criticized him for his "brags" on striking down Roe v. Wade.
"I promise you with a Democratic Congress, Kamala and I will make Roe v. Wade the law of the land again," he said. "I promise you."
Another point of celebration between Biden and Sanders was their work to lower the costs of inhalers. Sanders, the chairman of the Senate Committee on Health, Education, Labor, and Pension, led the charge in launching an investigation into the prices of the widely used products. Since then, three of the four major companies (GSK, AstraZeneca and Boehringer Ingelheim) have limited out-of-pocket costs for their inhalers to $35.
"My impression is that these companies as well as many others in the pharmaceutical industry are beginning to catch onto the fact that the American people are tired of being ripped off and paying astronomical prices for the prescription drugs they need to stay alive or ease their pain," Sanders said.
Biden noted while Americans were paying as much as $600 for inhalers, the same product and medication were available in the United Kingdom for $49.
"It's outrageous, but we're doing something about it finally," he said.
Still, both Biden and Sanders said more work needs to be done. They advocated for expanding Medicare's price negotiations to 50 drugs (the first 10 drugs subject to negotiations were unveiled last year ) and for capping out-of-pocket costs for prescription drugs to $2,000 for all Americans.
"With Bernie's help we are showing how health care should be a right, not a privilege, in America," Biden said.
ABC News' Molly Nagle and Michelle Stoddart contributed to this report.


IMAGES
VIDEO
COMMENTS
Nursing team collaboration. Writing a care plan allows a team of nurses (as well as physicians, assistants, and other care providers) to access the same information, share opinions, and collaborate to provide the best possible care for the patient. Documentation and compliance. A well-written care plan allows nurses to measure the effectiveness ...
Essay Patient Care Plan. Care planning is very important part of nursing. According to the Department of Health (2007) it is a holistic approach that recognises that medical needs are not the only issue with a person that is in hospital. It helps people to achieve the outcomes they want for themselves through truly personalised services and ...
In addition to the initial purpose, the goal of the care plan is to help the patient achieve a specific outcome or set of outcomes. 2:01. As such, the care plan should be written with the outcomes in mind. 2:05. Care plans are grounded in evidence gathered from two points of view: subjective and objective. 2:11.
Step 1: Assessment. The first step in writing an organized care plan includes gathering subjective and objective nursing data. Subjective data is what the patient tells us their symptoms are, including feelings, perceptions, and concerns. Objective data is observable and measurable. This information can come from,
Nursing Care Plan Essay Topics and Outline Examples Essay Title 1: Nursing Care Plans: Enhancing Patient-Centered Care and Clinical Outcomes. Thesis Statement: This essay explores the pivotal role of nursing care plans in delivering patient-centered care, improving healthcare outcomes, and ensuring effective communication and coordination among healthcare teams.
Planning care is essential in the delivery of appropriate nursing care. Following assessment of a patient's needs, the next stage is to 'plan care' to address the actual and potential problems that have been identified. This helps to prioritise the client's needs and assists in setting person-centred goals. Planned care will change as a patient's needs change and as the nurse and/or other ...
2724 Words. 11 Pages. 12 Works Cited. Open Document. This essay will explore a needs orientated approach to the care that is delivered to a patient and examine the significance of the use of models and frameworks in the nursing process. It is intended to identify a patient with biopsychosocial needs that requires nursing intervention.
Nursing Care Plan for Diabetic Neuropathy. The major symptoms of peripheral neuropathy are severe pain in foot, circulation problem that result to feet numbness and reduced knee jack reflexes. We will write. a custom essay specifically for you by our professional experts. 809 writers online.
Future plan) The Nursing diagnostic is done based on the nursing assessments obtained from the lab values. The patient has various signs and symptoms such as her pain scale is 8 out of 10. The heart rate is 122, current blood pressure is 165/56, and oxygen level is 99% in SPO2. Goals:
A nursing care plan may also include physiotherapy that can be used to rehabilitate Ms. Anderson's condition after the acute period has passed (Kemp, Brummel-Smith & Plowman, 9). The most effective physiotherapy would be bronchial spasmolytic inhalations. These can include such medications as beta-2 adrenal agonists.
The aim of this assignment is to analyse a case study and create a nursing care plan based on the patient's issues. Initially background information regarding the patient's medical diagnosis is provided and seven prioritised nursing problems have been identified. Focus is made on the key nursing problem-immobility, and discussion is made as ...
Nursing Care Plan and Nurses' Philosophy Influence. This essay aims at critically exploring the philosophies, models, and frameworks that underpin care planning. This will be demonstrated through use of a service user case scenario with a long-term complex care need. The essay begins with an overview of the identified service user and...
The nursing process consists of four stages, the assessment, planning, implementing and evaluation. This problem solving approach will be adopted to structure, organise, and present the nursing intervention. A fully detailed client's profile will be given. The "mental health assessment and plan" process will also be addressed.
Step 1: Assess the patient's case study. The first step is to assess the patient case study. Read through the case study thoroughly and take note of any important information. Pay special attention to the patient's demographics, medical history, current condition, and other relevant information. Once you understand the patient case study well ...
The purpose of this essay is to carry out an assessment of a patient and present a plan of care of a specific problem that the patient has encountered. The model chosen to guide the care plan is the Roper, Logan and Tierney's 'Elements of Nursing'. This will enable me to develop my skills in assessment, problem-solving and planning care.
Final Care Coordination Plan. Effective care coordination plays a crucial role in providing high-quality healthcare services to patients. It involves the organization and facilitation of healthcare activities and resources to provide timely and efficient care to patients. In this essay, we will discuss the importance of care coordination in ...
treatment. But if care is to be truly patient centred, health professionals have to acknowledge that patient stories - the ill-ness narrative - that arise from their per-sonal encounters with health and social care, should be the dominant voice. 5 key points 1Patients' narratives can make a significant contribution to patient-centred care
Patient- and family-centered care encourages the active collaboration and shared decision-making between patients, families, and providers to design and manage a customized and comprehensive care plan. Most definitions of patient-centered care have several common elements that affect the way health systems and facilities are designed and ...
Nursing Care Plan Mrs Brown Nursing Essay. Mrs. Brown, an 80 year old female was admitted into the coronary care unit two days after having cardiac surgery to replace her aortic valve with a porcine valve. Mrs. Brown is overweight and has a history of coronary artery disease, hypertension, CHF and chronic bronchitis.
Care planning policy often emphasises the importance of taking account of the entirety of a person's conditions, circumstances, attitudes and preferences in developing an effective care plan. Multimorbidity among long term conditions is common ( Valderas et al., 2009 ). Patients with multiple long term conditions report difficulties in ...
Introduction. The plan of care developed below is designed for an 83 years old patient, Harold Blake, who has a medical history that is complicated. He had, 3 years previously, suffered a left cerebral vascular accident and has suffered angina attack two weeks ago. The patient was headed for a outpatient appointment while he suffered an angina ...
The patient-centered care is a basic shift in healthcare in our country resulting in expensive healthcare with poor health results for both the patients and the clinicians. This policy has developed a "2020 vision" which will bring affordable health insurances for all and access to high-quality care. (Davis et al, 2005).
A patient journey (PJ) is the ensemble of care events organized by time across all diagnoses and providers to improve or maintain health for one patient. The PJ is the HCS core product [ 4 ]. There are three roles in every PJ: the patient, the professional (s) and a governance/payer, hereafter 'the PJ partners.'.
Access the Worksheet and Directions in Word (25 KB) and Worksheet and Directions in PDF (157 KB). Plan-Do-Study-Act Directions and Examples. The Plan-Do-Study-Act (PDSA) method is a way to test a change that is implemented. Going through the prescribed four steps guides the thinking process into breaking down the task into steps and then evaluating the outcome, improving on it, and testing again.
Doctors and other health care providers are increasingly using healthcare algorithms (a computation, often based on statistical or mathematical models, that helps medical practitioners make diagnoses and decisions for treatments) and artificial intelligence (AI), to diagnose patient illnesses, suggest treatments, predict health risks, and more. In some cases, this is fine. However, using ...
Drug shortages have occurred in the nation's health care system for several decades, largely due to market failures and misaligned incentives. With today's white paper, HHS offers solutions and stands ready to work with Congress to ensure no patient faces the devastating consequences of drug shortages or goes without needed medicines.
SWBC co-founder and Chairman Charlie Amato serves as vice chairman for CHRISTUS Santa Rosa Health Care Corporation and was past chairman in the early 2000s. From 2013 to 2014, Amato served as chairman of the campaign cabinet for CHRISTUS Children's.
By safeguarding sensitive information related to reproductive health care, the rule will strengthen patient-provider confidentiality and help health care providers give complete and accurate ...
President Joe Biden stands with Sen. Bernie Sanders, I-Vt., after speaking about lowering health care costs in the Indian Treaty Room at the Eisenhower Executive Office Building on the White House ...
The Centers for Medicare & Medicaid Services April 2 released its final rule for qualified health plans offered through the health insurance marketplaces for 2025. Beginning in plan year 2025, CMS will require plans participating in state-based marketplaces to comply with time and distance network adequacy standards that are at least as stringent as those for the federally facilitated marketplace.