An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Psychiatry Investig
- v.14(4); 2017 Jul

A Case Report of a 37-Year-Old Alzheimer's Disease Patient with Prominent Striatum Amyloid Retention
Yoo hyun um.
1 Department of Psychiatry, Yeouido St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea.
Woo Hee Choi
2 Department of Radiology, Division of Nuclear Medicine, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Suwon, Republic of Korea.
Won Sang Jung
3 Department of Radiology, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Suwon, Republic of Korea.
Young Ha Park
Chang-uk lee.
4 Department of Psychiatry, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea.
Hyun Kook Lim
With recent advancement in amyloid imaging, diagnostic application of this new modality has become a great interest among researchers. New ligands, such as 18F- florbetaben, florbetapir and flutemetamol, have been discovered to overcome limitations of preexisting ligand Pittsburgh compound B. We report here a case of a 37-year-old male patient whose initial complaints comprised of gradual cognitive decline, apraxia, disorientation and sleep disturbances. 18F-Florbetaben amyloid imaging of the patient showed diffuse amyloid retention with prominent striatal uptake. This finding supports the clinical utility of amyloid imaging in diagnostic process of early-onset AD. Moreover, striatal dominant uptake pattern demonstrated in this patient include some meaningful clinical implications that warrant special attention among clinicians.
INTRODUCTION
Amyloid deposition has long been considered one of the pathognomonic markers of Alzheimer's disease (AD). Moreover, disruption in amyloid hypothesis has been frequently discussed as important targets of intervention for many years. 1 To date, most validated research results have been narrowed down to yield a model for biological trajectory of AD, where amyloid deposition far precedes clinical symptoms. 2 Thus, early detection of amyloid deposition has emerged a major target of intervention in AD patients. In this regard, amyloid imaging has emerged as an effective diagnostic tool that could enable early intervention in patients in AD trajectory, and the clinical utility of amyloid imaging has become a main topic of interest among researchers over the recent years. 3 If validated further, clinical usage of amyloid imaging is expected to extend beyond confirming AD pathology in patients with high risk factors, helping to differentiate AD from various types of dementia in those who present with atypical course or symptoms. 4
Pittsburgh compound B has been the first ligand used to detect amyloid deposition in AD patients. 5 However, its short half-life and resultant limitations in applying it to clinical setting have resulted in the development of new ligands for detecting amyloid deposition, such as 18F-florbetaben, florbetapir and flutemetamol. 6 Amyloid deposition usually initiates from temporal and orbitofrontal cortices, which later extends to frontal, parietal, precuneus, anterior and posterior cingulate cortices. 7 However, differential uptake patterns in autosomal dominant gene carriers have been noted that warrant special clinical attention. While typical amyloid deposition occurs from cortical structures, those with autosomal dominant gene carriers demonstrated initial amyloid deposition in striatum. 8 , 9
We report here a case where a case of early-onset AD patient who received a confirmatory diagnosis of AD by beta-amyloid imaging. There is relatively few evidence on the clinical application of beta-amyloid imaging in early-onset AD patients, and therefore, we expect our case can contribute to this line of inquiry. Moreover, validity of utilizing beta-amyloid imaging in differential diagnosis of dementias will be discussed.
A 37-year old male patient visited outpatient clinic, with complaints of gradual cognitive decline which had started 3 years earlier. Working as an industrial researcher, he started to make serious calculation mistakes that made him quit the job and began working as a manager in a company. However, his frequent forgetfulness, along with aggravation in recent memory impairments hampered him from fulfilling his duties, making him change jobs frequently. Apraxia and apathy had started 2 years before his visit to our clinic, and disorientation to time and person was worsened to a degree which it became impossible to commute daily between his workplace and home. At time of his visit to our clinic, not only he was fired from his recent job, but also he needed frequent reminder from his family to maintain hygiene. His sleep disturbance became prominent, frequently waking up middle of the night self-talking.
Before his visit to our clinic, he had visited two hospitals for evaluation and management of his symptoms, but to no avail. For a thorough examination of his symptoms, he was immediately admitted to our psychiatric ward. His laboratory findings did not reveal any abnormalities, and his tests for human immunodeficiency virus, syphilis all turned out to be negative. Upon his psychiatric admission, a neuropsychological test battery was implemented to evaluate the patient's cognitive status. He scored 22 in Mini-mental status examination, 1 in Clinical dementia rating scale (CDR), 10 and 4.5 in Clinical Dementia Rating-Sum of Box score(CDR-SB). 11 In his cognitive tests, in contrast to his relatively preserved language function, he displayed serious impairments in free recall, 20-minute delayed recall and recognition.
Brain magnetic resonance imaging demonstrated global cerebral atrophy of grade 1 by cortical atrophy scale 12 and notable medial temporal lobe atrophy of grade 2 by medial temporal lobe atrophy visual rating scale ( Figure 1A and B ). 13 Atypically early onset of dementia symptoms made the patient an eligible candidate for amyloid positron emission tomography (PET) imaging. 14 18-Florbetaben PET images revealed diffuse amyloid deposition with score 3 in brain beta-amyloid plaque load (BAPL), 15 with predominant amyloid deposition in the striatum ( Figure 1C and D ).

The patient's history, along with neuroimaging results and cognitive test results all satisfied the National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer's Disease and Related Disorders Association Alzheimer's (NINCDS-ADRDA) criteria16 for probable Alzheimer's disease with high level of evidence. 5 mg of donepezil was prescribed, and the patient was discharged on the 10th day of his admission. To control his persistent cognitive decline even after the discharge, donepezil was increased up to 23 mg with combination of memantine, which was also increased up to 20 mg. His cognitive decline has been relatively plateaued, but we advised the patient and his caregiver to regularly visit the clinic for monitoring of his symptoms.
This is one of the few case reports that demonstrated diagnosis of early-onset AD by 18F-florbetaben PET imaging. The patient demonstrated early onset of cognitive decline with accelerated deterioration. The fact that he meandered along various departments at different hospitals for confirmatory diagnosis reflect major role amyloid imaging played in the diagnostic process of the patient.
Amyloid imaging is usually indicated in patients with progressive MCI with dubious etiology, patients with atypical presentations and clinical course, and patients with early-onset progressive dementias. 14 Considering the patient in the case exhibited dementia symptoms at atypically early age, amyloid imaging was appropriately prescribed to diagnose the etiology of his cognitive decline. Integration of information attained from his history, clinical data indicated his diagnosis to be early-onset AD.
There have been relatively few reports utilizing 18F-labelled amyloid beta PET tracers that include clinical implications related to autosomal dominant AD. One study adopted 18F-florbetaben PET imaging in Down syndrome patients, suggesting potential role of amyloid imaging in identifying population at risk of dementia. 17 Similar study was conducted on patients with Down syndrome, but with 18F-florbetapir tracer. 18 An attempt to differentiate Down Syndrome pathology from AD has also been made with 18F-florbetapir tracer. 19 Future studies on autosomal dominant AD with 18F-labelled amyloid beta PET tracers could increase validity of adopting these new ligands in the diagnostic process.
Most notable test results in the case report arise from uptake patterns of 18F-florbetaben PET imaging. Unlike typical uptake patterns demonstrated by late-onset AD patients, where striatum is usually involved in the later course of illness, there was a dominant striatal uptake pattern in the patient. A previous study conducted on nondemented young adults with Down syndrome compared their results with that of studies conducted on autosomal dominant early-onset AD patients, where two groups of subjects concordantly showed predominant striatal uptake. 8 Indeed, previous studies on autosomal early-onset AD patients consistently showed high striatal amyloid deposition. 20 , 21 The aforementioned finding could explain 18F-florbetaben uptake patterns in the case.
The underlying mechanisms have been discussed in prior studies on the relatively early involvement of the striatum in autosomal dominant early-onset AD patients. Axonal mistrafficking induced by presenillin-1 gene mutation has been suggested as a potential culprit for striatal amyloid deposition in one animal study. 22 Such axonal mistrafficking is considered to stem from disruption in APP processing. 22 Indeed, APP processing patterns differed between autosomal dominant AD patients and sporadic AD patients. 23 Striatal vulnerability to early stages of tau protein accumulation in autosomal dominant AD has also been elucidated, and such phenomenon is considered more toxic to induce significant striatal neuronal injury. 24
The most prominent limitation of our case report is lack of genotype testing in the patient. If the genetic testing had been done, one missing puzzle in the diagnosis of patient would have been complete. Nevertheless, we believe our case report affirms diagnostic usefulness and clinical application of amyloid imaging in the differential diagnosis of early-onset dementia. We expect more prevalent use of amyloid imaging with accumulation of evidences and validation studies over time.
Acknowledgments
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (NRF-2015R1C1A1A02036578).

Dementia Case Study Essay – 3500 words
HEALTH ISSUES FOR OLDER ADULTS.
The Case Study
Previous History: Social
The case study chosen is that of a 74 year old male patient with a history of challenging health issues. John (an assumed name in order to protect the patients identity in accordance with the Code of Professional Conduct as per the Nursing & Midwifery Council, 2006) has been happily married for 54 years and does not have any children. He does belong to a large extended family – he has twelve siblings. He has spent his working life as a plumber. He has been a sociable person enjoying the company of friends and family. Before admission to the Dementia ward he was living with his wife in their family home. His wife is finding it increasingly difficult to deal with John’s behaviour and condition as recently he has become significantly cognitively impaired. On admission, John was clean and tidy and it was obvious that his wife takes very good care of him despite the considerable effort that is required by her. During his stay on the ward John did receive regular visitors and his family and friends showed a great deal of affection for him.
Previous History: Medical
On admission it was noted that John has a long history of ill health.
His main conditions are:
Multi-Infarct Dementia: “MID is a common cause of memory loss in the elderly. MID is caused by multiple strokes (disruption of blood flow to the brain). Disruption of blood flow leads to damaged brain tissue.” (NINDS). This was diagnosed three months ago after John exhibited trademark symptoms such as short term memory loss, confusion, shuffling feet. He also started losing bladder and bowel control. MID is usually found within the 60 – 74 year age group, more often in men than women. A MRI scan showed up this condition.
Cardiac Diverticulitis: a rare congenital heart malformation
Aortic Aneurysm
Hypertension
These conditions cause John great pain and distress. He is currently being administered several pain relieving medications – Morphine, Sevradol, Diclofenic and paracetamol. He also received medication for the hypertension.
John was told 15 months ago that the prognosis for the treatment of his Aortic Aneurysm was not good and it was anticipated that his life expectancy was six months.
The severity of the pain experienced by John results in very aggressive physical and verbal behaviour. This aggression is very difficult for his loved ones to deal with.
He was admitted to the dementia ward for a six week assessment with a view to providing suitable pain relief which could then lessen his challenging behaviour to an extent.
Care assessment
On admission to the ward, John was attended by psychiatric staff who carried out an evaluation on John’s memory. This is known as a Mini Mental State Examination. The MMSE indicates the importance of cognitive stimulation therapy that can be consistently offered to the patient. (Weavers (2007, p.1) (see Appendix 1). The MMSE is a series of questions and tests designed to establish whether a drug treatment would be appropriate. NHS guidelines state that the patient should score 12 points or more out of a maximum of 30 points to be considered for medication. The tests cover orientation to time, registration, naming and reading skills. (Alzheimer’s Society information sheet 436).
John was also assessed in terms of diet and sleep.
The Discomfort Scale-Dementia of the Alzheimers’s Type (DS-DAT) was carried out with John. DS-DAT measures discomfort in elderly patients with dementia who are losing cognitive capacity and communication skills and are increasingly reliant on nursing staff. It was originally conceived to measure discomfort but it can be used to assess pain.
Assessment on John revealed that when he is in pain he is prone to be more aggressive. Staff worked with him to find strategies he could use to alleviate the pain. He received psychological assistance from the Pain Management Specialists. According to research on care of the elderly pain assessment is always an important aspect of what is done to take care of patients with dementia. The pain manifestation in John’s case has been a concern for everyone involved in his care. This is supported by Smith (2005) who says that it is important for healthcare providers to make correct assessment in the treatment of elderly people. There are many deterrents to making correct assessment. The fact that our culture looks at dementia as a disease that is only in the mind and that people with dementia do not experience pain can create a problem because often doctors may not see symptoms as belonging to dementia. Also, as patients begin to lose the ability to understand their internal states, they cannot identify easily “sensations, feelings and experiences” (Smith 2005 p.2). This will also lead to a time when they may not be able to verbalise what they are feeling. When the condition gets to this stage it is important to take care of the comfort needs of the individual. Many healthcare providers assess this by means of a Comfort Checklist. Smith (2005) was able to show professionals that there are several assessment tools that can be used to assess pain levels in patients with dementia.
Kaasalainen (2007) presents another idea of how to assess the pain of patients with dementia by using behaviour observation methods. This literature supports that pain is “underestimated and undertreated” in the older population. Assessment then becomes even more important.
Early pain assessment is important because the patient may start to lose the cognitive ability to let their discomforts be known. A system of behavioural observation would be useful. In order for this to be accurate a system of criteria for behaviour indicators can be set. Some indicators include “rapid blinking and other facial expressions, agitation or aggression, crying or moaning, becoming withdrawn and guarding the body part “
(Kaasalainen, 2007 p.7).
When John starts getting aggressive it can be an indication that he is in pain. “ It is important to find out how patients with dementia communicate about their pain and to determine relevant background information about their pain needs.” McClean (2000) cited in Cunningham (2006) p.5. In order that a full assessment could be made of John and his pain communication and management, he was allocated a nurse to be with him all of the time to achieve an accurate record.
The Discomfort Scale for Patients with Dementia of the Alzheimer’s Type (DS-DAT) previously referred to has been challenged by Kaasalainen (2007). Some of the challenges she stated include:
“ * some of the items measured may be due to other situations and not only dementia.
· the way the tools are scored can be difficult and therefore not easy to use in the clinical setting
· most of the new tools (and other DS-DAT) are in preliminary stages and need more testing
· there is lack of consensus on how pain should be assessed with older adults so verbal reports continue to be used in most situations.
· The concept of discomfort may be due to other facts like infection, hunger, depression or anxiety which means that behavioural observations cannot be the sole basis for giving medication.” (Kaasalainen, 2007 p.8)
Gloth (2001) presented information about pain management in older adults. He stated that it is difficult to make sure that older patients are getting enough medication to manage their pain adequately. Most older patients have at least one chronic condition and take multiple medications which make it harder to tell what they require. For some healthcare providers it becomes more frustrating to make sure the pain is managed properly. Gloth (2001 p.188).
It is important to understand when giving medication that drugs have a different reaction in older adults that they have in younger patients. This must be taken into account when prescribing. When pain is managed well an individual will have ‘secondary gain’ whereby he will feel better and it will help family members stay and visit longer. All of this will help the patient manage his pain. (Gloth 2001 p.189). Gloth (2001) also suggests that clinicians use a variety of methods for pain management including no interventions and alternative therapies where possible.
In the ward the environment is kept as quiet as possible as it is policy not to administer neuroleptic drugs unless really necessary. Pharmacological treatment options are recommended only if behaviour poses an immediate risk to the individual or to others Weaver (2007), McShane et al (1997) cited in Narzarko (2007 p.118) states that researchers have found that people with dementia who are treated with neuroleptic drugs deteriorate more quickly than those who are not treated with such drugs.
Besides having his own individual nursing care, John is offered activities to help him stay as active as possible. It was reported in Jacques et al (2000 p.366) “offering patients the appropriate activity, i.e. Games, exercise, sitting and chatting can reduce boredom and agitation. John responds well to this individual attention and it does have a settling effect. During his working life, John was always working with his hands so he is keen to participate in games and exercise. He does try to engage in social contact with other patients but unfortunately this interaction has not been reciprocated so it has caused him upset and frustration and after a few attempts he now only talks with the nurse caring for him. His physical activity is also hindered by his pain.
John has lost a lot of weight recently so he has been seen regularly by the dietitian who is ensuring that he is eating a healthy nutritional diet. He does have a good appetite.
John’s sleep pattern has been erratic the last several months. “Many people with dementia are restless at night and find it difficult to sleep. Dementia can affect people’s body clocks so that they might get up during the night, get dressed or even go outside. Ensure that the person has enough exercise during the day and that they use the toilet before bed.(Alzheimer’s information sheet 525). John was gently reminded that it was night-time and that he should go back to sleep. A sleep diary was also kept to record the level of restlessness.
There are two types of carers involved in looking after John – those who work within the clinical setting and those family members who must care for a chronically ill family member. The family member is predominately John’s wife.
Rasin and Kautz (2007) carried out a study that focused on caregivers in assisted living facilities. The National Centre for Assisted Living (NCAL) estimates that “42% to 50% of residents in assisted living facilities have dementia and 34% of them exhibit behavioural symptoms of dementia at least once a week.” NCAL (2006) cited in Rasin and Kautz (2007 p.2). They found that caregiver training was different depending on the state in which the individual lived and many were not formally trained to work with dementia patients – instead they received training either on the job or through life experience. The study used focus groups for data collection. Carers said that there were two types of knowledge that caregivers had that were effective in dealing with dementia patients: behavior centred knowledge – knowing recommended approaches to use with specific behavioural symptoms of dementia and person centred knowledge – knowing the residents well enough that they could look beyond the behaviour of the person (Rasin and Kautz. 2007 p.33-34).
They felt that the person centred knowledge was the strongest and most effective in caring for a person with dementia. From this study they made several recommendations for nursing:
· get to know the resident so you can determine what might be causing the disruptive behaviour.
· Giving individualised care for the residents can increase their quality of life.
· Caregivers should be taught how to incorporate patients life stories into their treatment plans to help them understand why the behaviour is being exhibited.
· Caregivers who understand and use person centred knowledge need to be acknowledged (Rasin and Kautz p.36).
A person centred approach was used in John’s treatment. He was encouraged to talk about his past and his wife was able to provide a lot of useful details which allowed John to be seen and treated as a ‘whole person’. It did also allow staff to make sense of some of the behaviour displayed by John.
Hepburn et al (2007) researched another way of effectively educating family members. They looked at a transportable psycho-education program geared towards helping to reduce caregivers stress. Several programs are spotlighted in this article. What they found was that a one to one behaviour management program given by home support team help to reduce the burden on caregivers and help to reduce depression. This program combined education with counselling. With the knowledge given to families, it was possible to delay the hospitalisation of the patient with dementia. (Hepburn et al, p.31-35)
Most caregivers are women, at least partly because it is a role that all women are expected to play in most societies. Doress-Wortens (1994) researched the effects of caregivers’ stress on women who already had multiple roles. They found that the stress in certain types of care giving situations were higher than others – e.g. when the caregiver involved personal care or dealing with a family member with dementia, they tended to experience more stress. A family member who was physically frail and needed minimal help was less stressful. John’s wife stress levels decreased with experience of looking after him – this information was apparent from reading of previous case notes. From this study it was apparent that women handle many different situations and they need coping strategies when they add the care of an ill family member to the set of tasks they perform.
Evaluation:
It is important to evaluate John’s care plan with regard to establishing the best possible attention for him. This has been done with reference to the National Institute for Health and Clinical Excellences (2006). According to NICHE (2006) there were 700,000 cases of dementia in the United Kingdom and there are approximately a million caregivers for them. As a result of these figures NICHE provided recommendations for those dealing with patients who have dementia.
NICHE Recommendation 1 : A coordinated and integrated approach between health and social care to treat and care for patients with dementia and carers.
John’s care : John has received the care of a specialist team who are trained to coordinate the day to day assessment and management of his condition. This comprised doctors, nurses, psychiatric team. Each professional provides guidance and support both for John and his family. His wife receives education and assistance with techniques on how to handle his aggression at home. Because she is his main carer at home, she has been given details of support groups where she will be able to get additional advice.
NICHE Recommendation 2 : The needs of carers should be assessed and support should be offered as part of the overall plan.
John’s care : It is important for staff from the dementia ward to offer support and help John’s wife deal with his physical and verbally aggressive behaviour. Caplan, G.A. Et al (2006) states that families need to be given clear information about the disease trajectory , complications of dementia and limited treatment available.
John and his wife have been married for 54 years and have no children. The emotions of the medical prognosis need to be dealt with. Schulz et al (2003) cited in Ouldred and Bryant (2008) has found that the progression of dementia confronts families with difficult decisions and they need to be supported through this difficult period. It is important to receive pre-bereavement counselling which can lead to better adjustment post-bereavement. Bright (2008) researched the quality of elderly care of those who have dementia as they move into end of life situations. He pointed out that palliative care is not as developed for dementia as it is for cancer so levels of care will vary between different geographical regions.
It is difficult for John’s wife to deal with the stress that comes from living with a man she has known for so many years as his life deteriorates. She has been advised where to gain support where needed. Support groups can bring enormous relief and help to deal with some of the challenges of the caring role.
NICHE Recommendation 3 : Memory assessment should be given to all patients with dementia.
John’ care : The Pain Management Team kept close observations using the Abbey Rating Scale and weekly evaluations on John were used to get his pain under control (see attachment 2). Wood (2002) states that the nurse’s role in pain management is vital, therefore, nurses should be fully educated and trained to recognise when patients are in pain.
NICHE Recommendation 4: People with dementia should not be denied services they need because of their age.
John’s care : The dementia ward is staffed by healthcare workers who are trained to work with patients with dementia and there is an understanding of what is required in each situation. This works on the person centred approach. Staff work with John on a regular basis and many get to know him well. The staff can see when he is getting anxious and angry and can intervene as appropriate. As stated by Fitzpatrick and Roberts (2004) healthcare professionals caring for older people require a range of core skills and knowledge, with explicit attention to the principles of patient and family-centred care, promoting autonomy, dignity and respect, along with good communication skills.
In conclusion, there has been a positive outcome after John’s assessment on the dementia ward. Aggressive outbursts are less frequent and this makes a better quality of time for John with his wife, family and friends. He still tries hard to be independent.

Alzheimer’s Society Information sheet 436, 525. Available to download from:
hhtp:/www.alzheimers.org.uk
Bright, L. (2005). Palliative care for people with dementia. Management Matters Available to download from
http:// . [28 March2008}
Bephage, G. (2005). Quality sleep in older people: the nursing care role. British Journal of Nursing. Vol. 14 (4) pp.205-210
Bephage, G. (2007). Care approaches to sleeplessness & dementia. Nursing & Residential Care. Vol. 9 (12) pp. 571-573.
Caplan, G.A., Meller, A., Squires, B., Chan, S., Willet, W. (2006). Advance care planning and hospital in the nursing home. Age Ageing. Vol. 35 (6) pp. 581-585.
Chambers, M. & Conner, S.L. (2002). User-friendly technology to help family carers cope. Journal of Advanced Nursing . Vol. 40 (5) pp. 568-577.
Cook, A.K., Niven, C.A., Downs, M.G. (1999). Assessing the pain of people with cognitive impairment. International Journal of Geriatric Psychiatry . Vol. 14 (6) pp.421-425.
Cunningham, C. (2006). Managing pain in patients with dementia in hospital. Nursing Standard. Vol. 20 (46) pp.54-59
Doress-Wortes, P.B. (1994). Adding elder care to women’s multiple roles: a critical review of the caregiver stress and multiple roles literatures. Journal of Research . Vol. 31. pp.1-6.
Fitzpatrick, J.M. & Roberts, J.D. (2004). Challenges for care homes: Education and training of healthcare assistants. British Journal of Nursing . Vol. 13 (21) pp.1258-1260
Gloth, F.M. (2001). Pain management in older adults: prevention and treatment. Journal of the American Geriatric Society. Vol. 49 (2) pp.188-199.
Jaques, A. Jackson, G.A. (2000) Understanding Dementia 3 rd ed Churchill, Livingstone, London. pp.235-269, p. 336
Hepburn, K. Lewis, M. Tomatore, J. Sherman, C.W. & Bremner, K.L. (2007). The savvy caregivers program: The demonstrated effectiveness of a transportable dementia caregiver psycho education program. Journal of Gerontological Nursing. (2007)
Vol. 33 pp. 30-37.
Kaasalainen, S. (2007) Pain assessment in older adults with dementia: Using behavioural observation methods in clinical practice. Journal of gerontological Nursing Vol. 33 (6) pp. 6-10
Lewis, M.M. & Trzinski,A. (2006). Counselling older adults with dementia who are dealing with death: Innovative interventions for practitioners. Death Studies . Vol .30 (8)npp. 777-787
National Institute for health and Clinical Excellence (NHS) and Social Care Institute for Excellent (SCIE) (2006) NICE SCIE guidelines to improve care of people with dementia. Available to download from http://www.nice.org.uk/nice/media/pdf/2006-052 [Assessed 13/03/08]
National Institute of Neurological Disorders and Stroke NINDS Multi-Infarct Dementia Information Page. Available to download from http:/wwwninds.nih.gov/disorders
Nazarko, L. (2007). Behaviour that challenges: types and treatment. British Journal Of Healthcare Assistants . Vol. 1 (3) pp116-119
Ouldred, E. & Bryant, C. (2008). Dementia Care. Part 3: end-of-life care for people with advanced dementia. British Journal of Nursing. Vol. 17 (5) pp. 308-314
Rasin,J & Kautz, D. (2007). Knowing the resident with dementia: Perspectives of assisted living facility caregivers. Journal of Gerontological Nursing. Vol. 33 (9) pp.30-36.
SA Carers. (2005). Understanding the role of the family carers in healthcare. Available to download from http://www.carers-sa.asn.au/pdf_files . [Assessed 15/03/08]
Scottish Intercollegiate Guidelines Network (2006) Guideline 86: Management of Patients With Dementia. Edinburgh, SIGN.
Smith, M. (2005). Pain assessment in nonverbal older adults with advanced dementia. Perspectives in Psychiatric Care. Vol 41 Available to download from http://www.questia.com
Stokes, G. (2000). Challenging Behaviour In Dementia. A Person Centred Approach. Oxon Winslow-press Ltd. pp.206
Weaver, D. (2007). Behavioural Changes: Dementia & Its interventions. Nursing & Residential Care. Vol. 9 (8) pp. 375-377
Woods, S. (20020. Nursing care & implications for nursing. Nursing Times. Vol. 98 (40) pp. 39-42
Bibliography
Abbey, J. (2004).The Abbey pain scale: a 1-minute numerical indicator for people with end-stage dementia. International Journal of Palliative Nursing. Vol.10 (1) pp6-13
DeWaters, T. & Popovich, J. (2003). An evaluation of clinical tools to measure pain in older people with cognitive impairment. British Journal of Community Nursing. Vol. 8 (5) pp226-234
Dingwall, L. (2007). Medication issues for nursing older people (part 1). Nursing Older People. Vol. 19 (1) pp25-35
Evers, C. (2008). Positive dementia care: taking perspective. Nursing & Residential Care. Vol. 10 (4) pp184-187
Hobson, P. (2008). Understanding dementia: developing person-centred communication. British Journal of Healthcare Assistants. Vol. 2 (4) pp162-164
Kirkwood, T. Dementia Reconsidered: A person comes first. (2004). Open University Press U.K.
Inter-Professional Healthcare Collaboration: 72-Year-Old Dementia Patient Case Study
This paper will discuss a case study of Loretta, a 72-year-old Australian diagnosed with dementia, describing a woman’s clinical condition by using ICF terminology and structure and outlining the measures which need to be imposed for providing her with effective interventions and enhancing the professionalism of the involved exercise physician.
Description of a clinical condition
Body structures and functions.
Loretta is a 72-year-old Australian citizen living in Melbourne who is diagnosed with dementia. The pathological neurofibrillary changes in her central nervous system caused the structural impairments and had a devastating impact upon her cognitive functions, including the impaired memory and semantic processes which in their turn affected Loretta’s communicative abilities. The conversational difficulties in Loretta were caused by the decline of the mental processes essential to the communicative functions, including the functions of recognition and usage of language signs. The impairments of declarative memory resulted in communication difficulties, repetitive questions, and word-finding problems.
Activities and participation
The impaired cognitive abilities in Loretta significantly reduced her skills of learning applying knowledge and communicating with others. The communicative difficulties limited Loretta’s participation in the community and social life and threatened her interpersonal interactions and relationships. It made Loretta passive and uninvolved in domestic and community life.
Environment and contextual factors
Loretta’s communication disability can be regarded as the outcome of her ineffective interaction with her environment. She lacked interpersonal support because her husband and children perceived her clinical cognition as the loss of self. Having problems communicating with large groups of people and strangers, Loretta isolated herself and rejected any contacts.
Intervention project
An effective treatment program for Loretta’s condition requires developing multi-component interventions with special emphasis put upon physical training, psychosocial and emotional support through educating the family caregivers and involving the community in the treatment of patients with dementia. This approach would allow considering the body structures along with the environmental factors for providing complex treatment for the patient diagnosed with dementia.
Taking into account the fact that elderly individuals with dementia are under the threat of decline in their physical functioning, it can be stated that the physical training component is significant for developing an effective intervention program for Loretta. The multi-component physical training interventions, including the exercises intended to enhance the patient’s endurance, strength and balance have proven to be effective for improving the participants’ physical functioning, regardless of the stage of disease (Blankevoort, van Heuvelen, Boersma, Luning, and Scherder, 2010, p. 393; Flicker, Liu-Ambrose, & Kramer, 2011, p. 466). Moreover, the best intervention outcomes can be received from the programs with the largest training volume.
Due to the significant impact of environmental factors upon the condition of patients diagnosed with dementia, their passivity and segregation from the rest of the community, educating their relatives and community members and encouraging them to provide the patients with psychosocial support is of paramount importance for receiving a positive outcome from the intervention program. Burton (2010) pointed out the importance of creating dementia-friendly neighborhoods instead of focusing on the internal environment of dementia care homes. Taking into account the fact that conversational difficulties caused by cognitive impairments traditionally result in the patient’s passivity, understanding, and support of the surrounding people are critical in terms of palliative care. Another influential factor is the people’s misconceptions concerning the patients with dementia, their communicative needs, and abilities. These stereotypes need to be overcome through educational measures.

Three characteristics of professionalism
The three characteristics of professionalism that are essential for conducting the above-discussed intervention program successfully include the skills of an exercise physiologist to develop an appropriate training program for every individual patient, inter-professional collaboration, and addressing exercise as medicine clearly understanding its role in a complex intervention program.
Recognizing the significant impact that physical exercises can have upon the patient’s condition, an exercise physiologist has to make the right prescription for each person (Boone, 2011). Thus, Loretta’s physical functioning at the moment when the prescription is made needs to be taken into consideration for developing an appropriate multi-component physical intervention project.
With the current tendencies of professionalization in the exercise physiology domain, exercise physiologists need to gain a clear understanding of their role in the overall system of modern healthcare services. It would allow them to convince the patients with dementia and their relatives of the importance of appropriate physical training for the palliative care of patients with dementia, Due to the fact that dementia interventions require a complex approach and a combination of measures, it can be stated that inter-professional collaboration is critical for developing effective projects. Thus, exercise physiologists should realize the importance of their role in developing the intervention programs without understating the importance of inter-professional collaboration with other specialists.
The role of another professional
As it has been stated above, the recognition of the role of other professionals is significant for improving the outcomes of the intervention projects. Thus, the role of social workers and nurses in the implementation of an effective intervention project is as important as the role of exercise physicians (Perry, Draskovic, Lucassen, Vernooij-Dassen, van Achterberg, & Olde Rickert, 2011; Stevens, Lancer, Smith, & McGee, 2009 ). In that regard, their successful teamwork, information exchange, and recognition of the fact that the interventions need to be multi-component are essential to the quality of the provided services. To develop a specific training program for Loretta, an exercise physician will need to consider the impact of other interventions to make the components complementary.
Two strategies for making the practice person-centered
Taking into account the fact that the conversational difficulties in individuals diagnosed with dementia predetermine their passivity and segregation from the community, the person-centered approach is the most appropriate strategy for creating more comfortable conditions for individuals with dementia. The two strategies of person-centered care include looking at the world from the point of view of a patient diagnosed with dementia and creating a positive social environment for them.
There is evidence that person-centered strategies have a positive impact on the intervention outcomes (Kontos, Mitchell, & Baloon, 2010; Robinson, Bamford, Briel, Spencer, & Whitty, 2010). Empathy is critical for effective care for Loretta and other patients diagnosed with dementia. Looking at the surrounding world and community through the patients’ eyes would enhance understanding of the underlying problems and processes. Regarding the strategy aimed at creating a positive social environment, it should be noted that the community involvement and recognition of the problem of dementia in elderly people is critical for arriving at an appropriate resolution.
Two strategies for professional development
The two strategies which can be implemented for the professional development of an exercise physician include an evidence-based approach to professional practice and enhancing one’s knowledge in the related disciplines. Implementing the results of the recent research in professional practice can be beneficial for improving the outcomes and increasing one’s professional level. As to the importance of acquiring knowledge on the related professional domains, it would allow enhancing the effectiveness of the teamwork and improving the patients’ outcomes from the complex interventions in general.
In general, it can be concluded that interventions for Loretta diagnosed with dementia should comprise several components, including those of physical training educational and social work, and effective inter-professional work is required for improving the patient’s outcomes.
Blankevoort, C., van Heuvelen, M., Boersma, F., Luning, H., and Scherder, E. (2010). Review of effects of physical activity on strength, balance, mobility and ADL performance in elderly subjects with Dementia. Dementia and Geriatric Cognitive Disorders , 30(5), 392-402.
Boone, T. (2011). Contemporary exercise physiology: The big picture. Professionalization of Exercises Physiology Online, 14(3), 1-17. Web.
Burton, E. (2010). Designing dementia-friendly neighborhoods: Helping people with dementia to get out and about. Journal of Integrated Care , 18(6), 11-18.
Flicker, L., Liu-Ambrose, T. & Kramer, A. (2011). Why so negative about preventing cognitive decline and dementia? The jury has already come to the verdict for physical activity and smoking cessation. British Journal of Sports Medicine , 45(6), 465-467.
Kontos, P., Mitchell, G., & Baloon. B. (2010). Using drama to improve person-centered dementia care. International Journal of Older People Nursing, 5(2), 159-168.
Perry, M., Draskovic, I., Lucassen, P., Vernooij-Dassen, M., van Achterberg, T & Olde Rickert, M. (2011). Effects of educational interventions on primary dementia care: A systematic review. International Journal of Geriatric Psychiatry , 26(1), 1-11.
Robinson, L., Bamford, C., Briel, R., Spencer, J., & Whitty, P. (2010). Improving patient-centered care for people with dementia in medical encounters: An educational intervention for old age psychiatrists. International Psychogeriatrics , 22(1), 129-138.
Stevens, A., Lancer, K., Smith, E., & McGee, R. (2009). Engaging communities in evidence-based interventions for dementia caregivers. Family & Community Health , 32(1), S83-S92.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, June 29). Inter-Professional Healthcare Collaboration: 72-Year-Old Dementia Patient. https://ivypanda.com/essays/inter-professional-health-case-study/
"Inter-Professional Healthcare Collaboration: 72-Year-Old Dementia Patient." IvyPanda , 29 June 2022, ivypanda.com/essays/inter-professional-health-case-study/.
IvyPanda . (2022) 'Inter-Professional Healthcare Collaboration: 72-Year-Old Dementia Patient'. 29 June.
IvyPanda . 2022. "Inter-Professional Healthcare Collaboration: 72-Year-Old Dementia Patient." June 29, 2022. https://ivypanda.com/essays/inter-professional-health-case-study/.
1. IvyPanda . "Inter-Professional Healthcare Collaboration: 72-Year-Old Dementia Patient." June 29, 2022. https://ivypanda.com/essays/inter-professional-health-case-study/.
Bibliography
IvyPanda . "Inter-Professional Healthcare Collaboration: 72-Year-Old Dementia Patient." June 29, 2022. https://ivypanda.com/essays/inter-professional-health-case-study/.
- Gastrointestinal Bleeding: 72-Year-Old Male Patient
- Shock State in a Patient with Symptoms of Fever
- Atypical Symptoms in Older Adults
- American Public Health & Minimum Housing Standards
- Loretta Perfectus Walsh: First Female Chief in the Navy
- Early Education: "Art Play" by McWilliams et al.
- Person-Centered Strategy of Diabetes and Dementia Care
- The Person-Centered Care in Nursing
- Interprofessional Collaboration in Healthcare
- Childhood Obesity: Review and Recommendations
- Nursing Interventions and Hemoglobin Levels
- Patient Compliance to Health Care Recommendations
- Health Research and Educational Trust
- Pre-Operative Education and Postoperative Pain
- Evidence Based Medicine
Dementia case study essay sample
- Published: September 12, 2022
- Updated: September 12, 2022
- University / College: The University of Newcastle, Australia (UON)
- Language: English
- Downloads: 44
Dementia is a dreaded neurodegenerative disorder that causes progressive decline in cognitive or mental functions. Alzheimer’s disease is the most common type of dementia and the two terms are often used interchangeably. Dementia is an impairment that gets worse over time, and cannot be reversed by medication or surgery (Levine 2006, p 12). Science has not yet found a cure for Alzheimer’s; it remains one of the most mysterious illnesses of the brain, one that continues to baffle experts. Dementia starts off as your typical type of memory loss that is common among the elderly. Because AD has mild and subtle symptoms in the beginning, it is often diagnosed at the latter stages when the person manifests the most recognizable symptoms. Early detection is an area that science must work on because while there is no cure for dementia yet, it can be managed with early intervention programs such as occupational therapy and medications. (Buijssen 2005, p. 87).
Among the hallmarks of Alzheimer’s is the failure to remember salient details about one’s life, which includes the inability to recognize family and friends. Apart from this severe loss of recognition, patients with dementia also manifest profound deterioration in communication and cognitive abilities, and by extension, their physical dexterity and coordination as well. Patients also exhibit extreme mood swings and distemper, as well as the inability to keep personal habits (Kitwood 1997, p. 43). Age is the number one risk factor for Alzheimer’s and most patients with dementia are the elderly. During the early stages of AD, neural cell death occurs in areas that control and store memory. After some time, neurons in areas controlling language and reasoning die as well. Brain cells continue to die until death takes place secondary to severe loss of brain function. The exact causes and the mechanism behind the development of dementia remain unknown and is the main focus of current research, alongside early detection and diagnosis (Manthorpe & Iliffe 2004, p. 23).
Dementia can have profound effects, not only for the patients and loved ones, but for the caregivers as well. Health services for people suffering from dementia are one of the biggest drivers of costs for the British welfare system. For people with dementia, the most significant problems take place secondary to the progressive degeneration of cognitive functioning (Moniz-Cook E et al 1998, p. 209). These include loss of independence and the inability to participate in social activities. All of these things adversely affect the quality of life, well-being, and safety not just of the patient, but their loved ones and carers as well (Swift 2001). Towards this end occupational therapists and case managers should focus on reducing dependency by retraining and enhancing daily functioning, which then improves the quality of life of everyone involved in the case. To achieve this, occupational therapists should engage and maximize positive social support through friends and loved ones as well as through support and advocacy organizations (Pratt & Wilkinson 2003, p 187).
Going by the figures of the Alzheimer’s Society of the United Kingdom (2007), there are about 700, 000 people with dementia. In terms of health care costs, this translates to almost £17 billion that the British government has to shoulder (NAO 2007). These figures are believed to be a great underestimation because the numbers are based on patients who are actually seeking medical services (Evans 2005, p. 122). A greater number remain undiagnosed because they are still in the very early stages of dementia (Guttman 2003, p. 174). By conservative estimates, people with dementia will rise to over one million some fifteen years from now. Of these numbers almost seventy percent are women.
In the United Kingdom, dementia other mental disorders are managed under primary care or care in patient’s home or in a care facility (Liebman et al 2005, p. 43). Those with mild mental disorders are the ones that can benefit most from primary care and management such as occupational therapy because whilst they do not have any acute medical condition that require emergency or hospital care, they nevertheless have physical limitations that require constant provision of care (Evans et al 2005, p. 345). These people require social and health services to help them live as independently and autonomously as possible, and occupational therapy is among the best management programs that can help provide that independence (Hilgendorf 1996, p. 36). Because hospital or emergency care costs more than primary care or health management at home, primary and preventive care for patients with dementia becomes a priority (ADI 1992; Evans 2005, p. 344). The British government is seeing the value of improving the delivery of primary health care and management to people with dementia, including the design of standard models of care and increase in community-based support for the patients (Dunleavy et al 2003).
A cornerstone of this primary care programs for people with dementia is the provision of occupational therapy services. In particular, community-based programs including education, support programs and cognitive and occupational therapy for people with dementia has been found to improve daily functional activities, especially for those in the early stages of dementia (Noyes et al 2000, p. 310). The improvement in functioning creates a cascade of benefits that includes the reduction of burden on caregivers (Graff et al 2007, p. 1196). It is important that carers be given support as well because their job can be very taxing and emotionally draining. When patients improve functionality and physical autonomy, they lessen their dependence on caregivers. The carers are given the chance to rest and relax and are thus able to attend to their jobs with less stress (Swansburg 2002, p 133).
Caregivers play crucial roles in ensuring the health and safety of people with dementia and their effectiveness in their roles help ease the burden on the health care costs by delaying the need for formal care (Graff 2006, p. 73). However, in the course of performing their duties as carers, their own health and well-being may suffer in the process (MHA 1983). This is where occupational therapy comes in. By directly addressing the patient’s disabilities and impairments by improving functionality in activities of daily living (ADL), occupational therapists provide direct benefits to the patients and indirect benefits by reducing the burden of caregivers. Moreover, the significant and clinically relevant improvements in the patient’s ability to perform daily functional activities encourage both the patients and their loved ones, and heighten the morale and sense of competence among carers (Graf 2008). This sense of success and emotional boost can have profound health benefits that deserve careful study.
Community occupational therapy intervention for people with dementia, including the provision of primary care has been proven to reduce health care costs because the patients are able to function better without the need for added health services such as medication and hospital care (Graff 2008). Other risks associated with dementia such as falls are also greatly reduced because of better functioning. Occupational therapy has proven to be a key element of a successful risk management package, especially for patients with dementia receiving primary care at home (Brody, 2006). To such ends, occupational therapists work with a multi-disciplinary team, including inputs from the patient and their family, to design activities that are meaningful to the patient (Corcoran & Gitlin 1992, p. 804). These includes the use of the patient’s own interests and activities to create a therapy programme that improves physical strength, dexterity, coordination, and movement, to include and improve the patient’s cognitive and emotional domains as well. The main goal is to achieve as much independence as possible, with emphasis on the safety and dignity of patients (ADI 2003). Aside from designing relevant therapeutic activities, occupational therapists will also guide caregivers and loved ones in making the physical environment more responsive to the needs of the patient. By exploring the different ways of performing functional tasks, occupational therapists are thus able to find one approach that works best for their clients.
Occupational therapists take a holistic approach in order to keep patients highly functional in spite of their physical and mental impairments (Watkins 2000, p. 99). By employing a client–centered approach, occupational therapists are thus able to design a program that is tailor-made to adapt to the patient’s unique needs and circumstances. Occupational therapy provides for patient’s needs by lessening their disabilities and dependency, while advocating for the dignity of the patient as human beings, regardless of age, gender, race, sexuality, social class, education, lifestyle, and religious or political beliefs (NMC 2002). As part of a risk managemet program, an occupational therapy program must recognize that patients suffering from dementia require long-term management, including constant assessment and reassessment of needs and risks, with the ultimate goal of lessening dependency and functional mainstreaming in society (Watkins 2000, p. 113).
Occupational therapy, especially when given very early, has greater chances of success compared with pharmacological and other psychosocial interventions. In a study conducted by Graff et al (2006), patients with dementia who were given occupational therapy showed marked improvements that far exceed the benefits of drugs and other interventions. One of the most important duties of an occupation therapist is to be able to provide risk management programs that allow citizens to be empowered as far as their health is concerned. Apart from providing health care, community practitioners should also aim to prevent health problems with proper risk and needs assessment, including the health needs of the carers and family members of the sick and elderly. Health care providers should not just react to the presence of a health problem but take proactive roles in preventing such problems from happening in the first place, and this is where occupational therapists come in, providing early intervention in order to prevent other health and safety complications. The challenge for future researches is to be able to improve current diagnostic procedures in order to provide the earliest intervention as possible.
Alzheimer’s Disease International (ADI), 2003 Charter of principles For the care of people with dementia and their carers, Retrieved on April 22, 2008 from http://www. alz. co. uk./adi/pdf/charter. pdf
Alzheimer’s Disease International ADI, 1992, Planning and design guide for community-based day care centres, Retrieved on April 22, 2008 from http://www. alz. co. uk./adi/pdf/daycarecentre. pdf
Buijssen, H 2005, The Simplicity Of Dementia: A Guide For Family And Carers, Jessica Kingsley Publishers.
Dunleavy, P et al 2003, Developments in British Politics 7, Palgrave Macmillan.
Corcoran M, Gitlin L 1992, Dementia management: an occupational therapy home-based intervention for caregivers, American Journal of Occupational Therapy, 46: 801-8.
Evans, C et al 2005, Practice nurses and older people: a case management approach to care, Journal of Advanced Nursing, Vol. 51 Issue 4, pp. 343-352, Retrieved on April 22, 2008 from http://web. ebscohost. com/ehost/viewarticle? data= dGJyMPPp44rp2%2fdV0%2bnjisfk5Ie46bRJsqy3UbKk63nn5Kx95uXxjL6prUq2pbBIrq6eSa6wsEi4qbc4zsOkjPDX7Ivf2fKB7eTnfLujtUmxq7BRsa%2byPurX7H%2b72%2bw%2b4ti7ee7epIzf3btZzJzfhruntU%2byqLdItZzkh%2fDj34y75uJ%2bxOvqhNLb9owA&hid= 22.
Graff MJ et al 2006, How can occupational therapy improve the daily performance and communication of an older patient with dementia and his primary caregiver? A case study, Dementia 2006, 5: 503-32.
Graff MJ et al 2007, Effects of community occupational therapy on quality of life, mood, and health status in dementia patients and their caregivers: a randomized controlled trial, ournals of Gerontology. Series A: Biological Sciences and Medical Sciences. 62A(9), 1002-9.
Graff, MJ et al 2008, Community occupational therapy for older patients with dementia and their care givers: cost effectiveness study, BMJ, 336: 134-138
Guttman, R 2003, Case Management of the Frail Elderly in the Community, Clinical Nurse Specialist: The Journal for Advanced Nursing Practice, July 2003 Volume 13 Number 4 Page 174, April 22, 2008 from http://www. nursingcenter. com/library/JournalArticle. asp? Article_ID= 101884.
Hilgendorf, P 1996, Profile of the successful home health nurse case manager, Nursing Management, Vol. 27, Num. 10, pp. 32Q-R, 32U-V. Retrieved on March 29, 2008 from http://web. ebscohost. com/ehost/viewarticle? data= dGJyMPPp44rp2%2fdV0%2bnjisfk5Ie46bRJsqy3UbKk63nn5Kx95uXxjL6prUq2pbBIrq6eSa6wsEi4qbc4zsOkjPDX7Ivf2fKB7eTnfLujtUmxq7BRsa%2byPurX7H%2b72%2bw%2b4ti7ivjepIzf3btZzJzfhrunt1G0prFPr6iyPuTl8IXf6ruI4tzEjeri0n326gAA&hid= 22
Mental Health Act (MHA) 1983, Code of Practice, UK, Department of Health Retrieved on April 22, 2008 from http://www. dh. gov. uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4005756
Manthorpe J & Iliffe S 2004, Early recognition of dementia — the next stage of awareness, Journal of Dementia Care, 12(5): 22-4.
Moniz-Cook E et al 1998, A preliminary study of the effects of early intervention with people with dementia and their families in a memory clinic, Aging & Mental Health, Aug; 2(3), 199-211.
NAO , National Audit Office UK, 2007, Improving services and support for people with dementia, Report by the comptroller and auditor general, The Stationary Office.
Noyes LE. Daley P. French K. 2000 Community-based services help people in the early stages of Alzheimers disease and other cognitive impairments, American Journal of Alzheimers Disease and Other Dementias, 15(5): 309-13.
Pratt, R & Wilkinson, H 2003, A Psychosocial Model of Understanding the Experience of Receiving a Diagnosis of Dementia, Dementia Sage Publications, 2; 181-99.
Swift G,, 2001. Care of older people: falls in late life and their consequences-implementing effective services. British Medical Journal, vol. 322, iss. 7290.

This work, titled "Dementia case study essay sample" was written and willingly shared by a fellow student. This sample can be utilized as a research and reference resource to aid in the writing of your own work. Any use of the work that does not include an appropriate citation is banned.
If you are the owner of this work and don’t want it to be published on AssignBuster, request its removal.
- Chicago (A-D)
- Chicago (N-B)
AssignBuster . (2022) 'Dementia case study essay sample'. 12 September.
AssignBuster. (2022, September 12). Dementia case study essay sample. Retrieved from https://assignbuster.com/dementia-case-study-essay-sample/
AssignBuster . 2022. "Dementia case study essay sample." September 12, 2022. https://assignbuster.com/dementia-case-study-essay-sample/.
1. AssignBuster . "Dementia case study essay sample." September 12, 2022. https://assignbuster.com/dementia-case-study-essay-sample/.
Bibliography
AssignBuster . "Dementia case study essay sample." September 12, 2022. https://assignbuster.com/dementia-case-study-essay-sample/.
"Dementia case study essay sample." AssignBuster , 12 Sept. 2022, assignbuster.com/dementia-case-study-essay-sample/.
- Alzheimer’s disease and dementia
- Dementia: alzheimer’s disease and people
- Alzheimers disease and dementia disease
- The unmet needs of carers in the australian society today literature review
- Dementia diagnosis case review
- Grand challenges in dementia 2010
- Strategies for elderly care and dementia
- Policy analysis on dementia care

Please, let us know if you have any ideas on improving Dementia case study essay sample, or our service. We will be happy to hear what you think: [email protected]

Case study 3: Joan
Download the Full Case Study for Joan PDF file (58KB)
Download the Vignette for Joan PDF file (49KB)
Name: Joan O’Leary
Gender: Female
Ethnicity: White Irish
Religion: Catholic
Disability: dementia with Lewy Bodies
First language: English
Family: estranged and in Ireland
Location: village in South West
Joan lives in a house in a small village. She has lived there for 28 years. She has two dogs and 11 chickens. Joan has always been quite private but is well known in her village. She goes to the nearby town on the bus to church, visits the local shop and community café, and goes away frequently. Joan goes for a long walk with her dogs each day. Joan hadn’t been to her GP for 6 years.
The café owner, Margaret, was worried about Joan. Joan has appeared very forgetful and disorientated. She has been seen in the village wearing her slippers and her neighbours have seen her out late at night with her dogs. Margaret went to Joan’s house and wasn’t allowed in but thought there was quite a strong smell.
Margaret phoned the GP in the village who went round to Joan’s house and persuaded her to have some tests. She has been diagnosed with moderate dementia with Lewy Bodies.
The GP phoned social services and you go out to do an assessment.
Download the Ecogram for Joan PDF file (48KB)
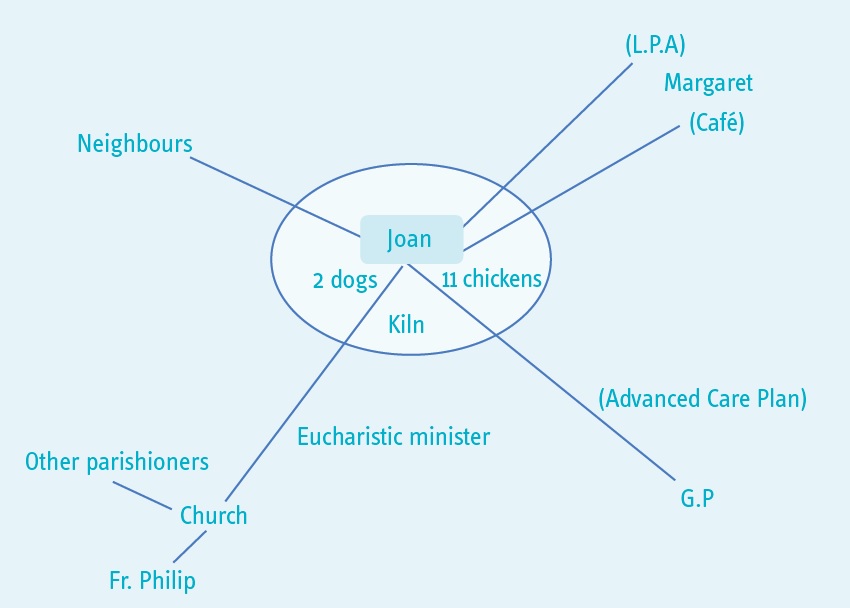
You told me that you didn’t really want to have an assessment. I explained that your GP had asked me to talk to you about what is happening for you at the moment because you have been diagnosed with dementia. You agreed to the assessment but you don’t want to have lots of information about you written down. These are the main things that you were happy for me to know.
At the moment you have capacity to make decisions about whether to have support or not. In the future you may find it more difficult to make decisions or not be able to make a particular decision. We talked about you arranging a lasting power of attorney and also doing an advanced care plan.
What’s important to you?
You said that you are quite a private person. You have two dogs and 11 chickens. You like to walk the dogs, go to the café and go to church in Lyme Regis. You take eggs to the café for Margaret (the owner) to sell.
You are a talented artist and have a small pottery shed and kiln in the garden.
You like to plan trips to different local areas and travel using the bus.
Your family is in Ireland and you haven’t seen them for many years. Your Catholic faith is important to you. You are a Eucharistic minister and you take holy communion to parishioners who can’t get to church.
What’s happening for you at the moment?
Your GP asked me to come and see you because you have been diagnosed with moderate dementia with Lewy Bodies.
You told me that you understand this is similar to Parkinson’s disease. You have noticed that your muscles have been aching and that you are not sleeping well.
The GP explained to me that you might find that you are unsteady at times or have tremors, and you might have some hallucinations, as these are common with this kind of dementia.
Margaret told me that you have been into the village wearing your slippers and that your neighbours have noticed you being out late at night which you agreed is unusual for you. However, you also told me that what you do is your own business. We talked about the risks that are attached to you going out late or not wearing appropriate clothing. You told me that you don’t think it is a problem, as you have always walked a lot and always find your way home. Also you said that you have the dogs with you when you are out and they know their way home. You already used reminders around the house so you said you would put a reminder on the front door to check your coat and shoes.
We talked about how you were managing day to day. You told me that you think you are managing well. However you haven’t been able to put the rubbish out or to clean out the chickens. You also have not been able to clean the bathroom. This is because you sometimes feel dizzy and your arms ache.
What is the impact on you?
You are concerned that people, like me, might start interfering with your life because of your illness.
What would you like to happen in the future?
You said that you want to continue to live in your home, looking after your animals, and doing the things that you currently do. We talked about what you think will happen and you said that you knew you will become less well. If you did need help in the future, you would like to arrange this yourself. We talked about having a personal assistant in the future.
How might we achieve this?
We talked about the importance of you having the right support in the future. You agreed that I could share this assessment with Margaret and your GP so that if you are not well enough to ask for advice or assistance in the future, they can ring the council. You will discuss a lasting power of attorney for finances, and health and care for Margaret. And you will do an advanced care plan with your GP. You will also talk to your GP about any medical support that might be available now, for example memory clinic and help with sleeping.
We also called your Parish Priest, Father Philip, and let him know that you have been diagnosed with dementia. He will ask a parishioner to give you a lift to church if you aren’t able to go on the bus.
You agreed to some help with keeping the animals and putting the rubbish out. Margaret and you will make an advert to put in the café window.
What strengths and support networks do you have to help you?
You said you are a very independent person. You have managed your home and finances for many years. You are managing well despite your illness and have strategies in place for things you might forget. You are active and have wide interests and talents. You also earn money through selling eggs. You contribute to the community through the parish. You are familiar with your local area and are used to travelling around.
You have a good relationship with Margaret, with your parish priest and with your GP. They are all willing and able to offer support.
Social care assessor conclusion
You have recently been diagnosed with dementia. This is starting to have an impact on your life and because of the nature of the illness the impact will increase as time goes on.
You have a lot of strengths to draw on and a good support network. You want to remain independent and, although there are some concerns about how you are managing, these are currently relatively minor and you have identified how to minimise them.
It is important that you plan ahead so that you remain in control of what happens and so that you can continue to achieve what matters to you for as long as possible.
Eligibility decision
You are not currently eligible for care and support under the Care Act 2014 because you can currently manage all day to day activities, apart from needing some help with maintaining your home. However, we have done a care and support plan that says what you will do to get help with the house and to plan for the future.
What’s happening next
See care and support plan .
Download the care and support plan document PDF file (178KB)

- Equal opportunities
- Complaints procedure
- Terms and conditions
- Privacy policy
- Cookie policy
- Accessibility

Alzheimer’s Case Studies
The Alzheimer’s Association reports that by the year 2025, 7. 1 million people 65 and older will be suffering from Alzheimer’s disease. Alzheimer’s is a form of dementia and its devastating that there will be roughly 7. 1 million diagnosed with one specific form of dementia. With this skyrocketing increase will come the need for more intervention and prevention projects to help the number of individuals suffering from all forms of dementia. Even though there is an umbrella of different forms of dementia, dementia its self is a term used to describe a disease that is chronic , progressive, and terminal.
Most individuals who are suffering from dementia get diagnosed later in the disease. The quantities of individuals who are getting diagnosed early in the disease are slim to none, because the symptoms of dementia are often confused with signs of normal aging. What is sad is people who are late in the disease are individuals who are being put into nursing homes , because they require 24 hour care. These individuals typically cannot remember who they are, where they are from, and sadly who their loved ones are.
Generally speaking, they are the ones who make moaning sounds in nursing homes and who sit in a chair all day because they becoming stiff. They have lost all ability to remember, think, communicate, and take care of their most basic life needs. What is important for caregivers to know is it does not have to be this way. Early detection of dementia is essential as it provides a means to access appropriate agencies and support networks for the dementia suffer. It also allows for the prevention of behavior and psychology symptoms. This means the progression of the disease can be delayed with early detection and prevention.
A lot of individual’s caring for their elderly loved ones will ask how they can look for sings of dementia. Signs start in early stage dementia. Early stage is the earliest detection and there are a variety of signs that are often over looked, because again the signs are mistaken for normal aging. However, sings include memory loss , cognitive impairments, and behavior deterioration. A lot of the signs have to do with changes in the memory and this is due to the fact that dementia is damage to the brain, it literally is the brain dying, and shrinking away.
This damage creates the lack of ability of cells to communicate with each other. Therefore, individuals who have been diagnosed with dementia are going to be going through major changes as the brain dwindles away. However, it is important to note is that dementia is not just a memory problem, it impairs cognition and deteriorates behavior , but memory loss is where it all begins and is an early detection of dementia because it interferes with complex actives of daily living, basic activities like cooking, housekeeping, shopping, and even handling money (Steeman, 2006, American Psychiatric Association, 198).
If there are problem with completing tasks that are minute and repetitive, there is something wrong. And being that tasks, as such, are basic and tasks one spends a large portion of their week doing, a suffer will become frustrated, uncertain, and fearful (Hutchinson et al. 1997). It can even make the individual feel embarrassed and humiliated (Gillies, 2000). This embarrassment and humiliation can increase when an individual experiences more than just memory loss; it can deepen when cognitive impairments begin. Cognitive impairments can include many different things.
For instance, Jorn (1986) believes some of these impairments can include individuals experiencing difficulty with repetition of sentence, reading, and naming common objects, grammatical deterioration and deficits in tasks requiring synaptic and sematic knowledge, deterioration in ones ability to process information. Impairments in automatic processes and controlled processes, the ability to repeat questions decreased. The ability to find words to organize sentences becomes a problem. Tse and his researchers found similar findings in their research on three attention tasks (2010).
Tse and his researchers conducted a study to see whether or not individuals with dementia had more trouble with attention tasks than that of younger adults and healthy older adults. The three attention tasks that were looked at included Stroop, Simon, and switching tasks, all of which require full cognitive ability. The results of their study indicated that individuals who were clinically diagnosed with dementia overall had about twice as many errors when it take to each of these three attention tasks.
What is important about Tse study was even in the trials where the attention task at hand was repetitive, the individuals with dementia had a significantly higher error rate than that of the younger adults and even more so than healthy older adults. Researchers have also found that individuals with early stage dementia have signs of behavior deterioration. These include deterioration in basic self-care behaviors, such as bathing, dressing, grooming, toileting, continence, transfers, and feeding (Lawton & Brody, 1969).
To export a reference to this essay please select a referencing style below:
Related essays:
- Alzheimers Disease, Complex Illness
- Alzheimers Disease, Slowly Progressive, Degenerative Disorder Of The Brain
- Alcoholic Dementia Research Paper
- Abstracts Essay Examples
- Alzheimer’s disease
- Difference Between Delirium And Dementia
- Delivering Patient Care: A Case Study Essay
- Alzheimer’s Disease
- Alzheimer’s Research Papers
- Alzheimers Disease, Nursing
- Assistive Technology Essay
- Windows NT vs Unix As An Operating System

Bruce Willis’ family missed a common early dementia symptom—and they're not alone. 5 ways to tell if it's more serious than normal aging
A third of people who notice dementia symptoms in themselves or a loved one keep quiet about it for a month or longer, according to a new survey out of the U.K.
Only 15% of the 1,100 patients and caregivers surveyed brought up their observations right away, and 11% still haven’t, according to the survey, released Monday by the London-based Alzheimer's Society . Participants included diagnosed dementia patients and their caregivers, as well as potential dementia patients and their caregivers.
Nearly a quarter of those surveyed waited more than six months before seeking medical help, the survey found. The most common reason for staying silent wasn’t anxiety about the condition, which is generally progressive. Rather, those affected weren’t sure exactly which symptoms are associated with normal aging and which are associated with dementia.
Case in point: Legendary actor Bruce Willis. In a May 31 essay in Vogue, daughter Tallulah Willis opened up about her dad’s 2022 diagnosis with aphasia, which impairs the ability to speak, understand speech, and to read and write. She also discussed his broader diagnosis of frontotemporal dementia, which typically occurs in people ages 45 to 64. Unusual behaviors, trouble managing emotions, and difficulty communicating and walking are hallmarks of the condition, according to the National Institute of Aging.
Like so many other caregivers, she says the signs of her father’s cognitive decline are clear, looking back. At the time, however, she chalked up his “vague unresponsiveness” to “Hollywood hearing loss.”
“I’ve known that something was wrong for a long time,” she confessed, adding that family members would often encourage each other to “speak up! Die Hard messed with Dad’s ears.”
“Later that unresponsiveness broadened, and I sometimes took it personally,” she added.
Confusion, stigma, and anxiety around dementia—which will affect a third of individuals over their lifetime—delay diagnosis and treatment, Kate Lee, CEO of the Alzheimer’s Society, said in a news release about the study.
“We can’t continue to avoid the ‘d’ word,” she said. “We need to face dementia head on.”
How to tell the difference between aging and dementia
“Dementia is definitely not normal aging,” Dr. John Schumann —executive medical director of Oak Street Health, a chain of primary care clinics that serve older adults—tells Fortune .
Dr. David Reuben, director of the Multicampus Program in Geriatrics Medicine and Contrology at the UCLA David Geffen School of Medicine, agrees. He equates aging, a normal biological phenomenon, to a “computer processor up in your brain that doesn’t work quite as quickly.” An example: When a word or phrase is “on the tip of your tongue,” and you find yourself saying, “give me a couple of minutes and it will pop back in.” Such retrieval deficits are “very common with aging,” he says.
Dementia is an umbrella term for a wide range of disorders involving a progressive or persistent loss of intellectual functioning, from mild to severe, with Alzhermier’s being the most common. While some cognitive “slowing” can occur as a part of the normal aging process, symptoms of dementia are distinct and are signs of disease, experts say.
According to the National Institute on Aging, signs that you or a loved one may be experiencing dementia—and not just normal aging—include:
- Asking the same question repeatedly
- Having trouble following directions like recipes
- Getting lost in a place you know well
- Becoming increasingly more confused about time, places, and people
- Not taking care of yourself, including eating poorly, forgetting to bathe or shower, or acting in an unsafe manner
Making a bad decision, missing a monthly payment, or losing something from time to time is normal, according to the agency. But making poor decisions much of the time, having trouble taking care of your monthly bills, and misplacing things often (and being unable to find them) is not.
What to do if you’re concerned about dementia
Those with dementia symptoms should contact their doctor, who will ask questions like when the symptoms began, if they’ve been getting worse, and to what extent, if any, they’re interfering with daily activities. A doctor may choose to refer a patient for a neuropsychological exam, which could shed further light on the situation or simply provide a record of baseline cognitive functioning, experts tell Fortune.
“Everyone has a slip once in a while,” Schumann says, citing the example of a lone incident of misplaced keys.
But symptoms like trouble balancing a checkbook and remembering how to dress and groom oneself are often signs of dementia, he cautions. The good news: If mood changes or sleep disturbances aren’t present, dementia is unlikely.
While the thought of a dementia diagnosis can be frightening, many are pushing for an early diagnosis, Reuben says. That’s for several reasons. It allows one to get their affairs in order. And it also provides a ray of hope, since there “may be drugs on the horizon” that can help those with earlier stage dementia.
This story was originally featured on Fortune.com
- 5 side hustles where you may earn over $20,000 per year—all while working from home
- Looking to make extra cash? This CD has a 5.15% APY right now
- Buying a house? Here's how much to save
- This is how much money you need to earn annually to comfortably buy a $600,000 home

Finish Your Essay Today! EssayBot Suggests Best Contents and Helps You Write. No Plagiarism!
Customer Reviews
What Can You Help Me With?
No matter what assignment you need to get done, let it be math or English language, our essay writing service covers them all. Assignments take time, patience, and thorough in-depth knowledge. Are you worried you don't have everything it takes? Our writers will help with any kind of subject after receiving the requirements. One of the tasks we can take care of is research papers. They can take days if not weeks to complete. If you don't have the time for endless reading then contact our essay writing help online service. With EssayService stress-free academic success is a hand away. Another assignment we can take care of is a case study. Acing it requires good analytical skills. You'll need to hand pick specific information which in most cases isn't easy to find. Why waste your energy on this when they're so many exciting activities out there? Our writing help can also do your critical thinking essays. They aren't the easiest task to complete, but they're the perfect occasion to show your deep understanding of the subject through a lens of critical analysis. Hire our writer services to ace your review. Are you struggling with understanding your professors' directions when it comes to homework assignments? Hire professional writers with years of experience to earn a better grade and impress your parents. Send us the instructions, and your deadline, and you're good to go.
Niamh Chamberlain


IMAGES
VIDEO
COMMENTS
Early onset Alzheimer disease (EOAD) is a neurodegenerative dementing disorder that is relatively rare (<1% of all Alzheimer cases). Various genetic mutations of the presenilin 1 (PSEN1) and presenilin 2 (PSEN2) as well as the amyloid precursor protein (APP) gene have been implicated.Mutations of PSEN1 and PSEN2 alter γ-secretase enzyme that cleaves APP resulting in increase in the relative ...
These three case studies help you to consider different situations that people with dementia face. They are: Raj, a 52 year old with a job and family, who has early onset dementia. Bob and Edith, an older married couple who both have dementia and are struggling to cope, along with their family. Joan, an older woman, who lives alone and has just ...
Case 24 Tremor, Hallucinations, and Cognitive Decline; Case 25 Dementia Following Stroke; Case 26 Vascular Cognitive Impairment; Case 27 Rapidly Progressive Behavioral Changes and Cognitive Symptoms in a 29-Year-Old Woman; Case 28 Young Woman Feeling Sick and Confused; Case 29 A Man with Urinary Incontinence and Trouble Walking; Case 30 ...
One study adopted 18F-florbetaben PET imaging in Down syndrome patients, suggesting potential role of amyloid imaging in identifying population at risk of dementia. 17 Similar study was conducted on patients with Down syndrome, but with 18F-florbetapir tracer. 18 An attempt to differentiate Down Syndrome pathology from AD has also been made ...
Rasin and Kautz (2007) carried out a study that focused on caregivers in assisted living facilities. The National Centre for Assisted Living (NCAL) estimates that "42% to 50% of residents in assisted living facilities have dementia and 34% of them exhibit behavioural symptoms of dementia at least once a week.".
This paper will discuss a case study of Loretta, a 72-year-old Australian diagnosed with dementia, describing a woman's clinical condition by using ICF terminology and structure and outlining the measures which need to be imposed for providing her with effective interventions and enhancing the professionalism of the involved exercise physician.
Check out Smart'n, the exclusive platform for nursing students, for more case study types. It offers over 2,500 NCLEX practice questionsand 60+ hours of NGN-NCLEX-style nursing case studies, helping you track progress and become a more confident registered nurse. Start your journey to NCLEX success with Smart'n. Understanding dementia.
Dementia is a dreaded neurodegenerative disorder that causes progressive decline in cognitive or mental functions. Alzheimer's disease is the most common type of dementia and the two terms are often used interchangeably. Dementia is an impairment that gets worse over time, and cannot be reversed by medication or surgery (Levine 2006, p 12).
Dementia Case Study Review: A basis for interpersonal Practice Communication is the process of conveying opinions and exchanging ideas in a way which enhances the interpersonal relationship between individuals. It is a skill that enables us to share ideas and solve the problems that people encounter in their everyday life to live meaningfully.
Case Study. Download the Full Case Study for Bob and Edith PDF file (64KB) Vignette - Bob. Download the Vignette for Bob PDF file (56KB) Name: Robert (Bob) Woodgate. ... Edith was diagnosed with vascular dementia a few months ago when Gary became concerned about her mixing up household tasks, for example putting shopping in the oven. ...
Disability: dementia with Lewy Bodies. First language: English. Family: estranged and in Ireland. Location: village in South West. Joan lives in a house in a small village. She has lived there for 28 years. She has two dogs and 11 chickens. Joan has always been quite private but is well known in her village. She goes to the nearby town on the ...
Donepezil hydrochloride/Aricept 10 mg once daily at bedtime: is a reversible inhibitor of acetylcholinesterase.They are for the adjunctive treatment of moderate Alzheimer's disease. Like all other medication donepezil has its side effects which are nausea,vomiting,anorexia,diarrhoea,insomnia,dizziness and agitation just to mention a few.
Case Analysis And Problems With Dementia Nursing Essay. Dementia is a progressive and irreversible decline in mental function1. Lewy Body Dementia (DLB) is a form of degenerative dementia characterised by the presence of "Lewy Bodies" which are clumps of alpha-synuclein and ubiquitin protein in neurons2. These are only detectable in post ...
Dementia Case Study Essay. Decent Essays. 501 Words; 3 Pages; Open Document. After reading the case study about John and Lydia, it appears that the individual's heath is declining. Lydia and John home seems to be showing early signs of dementia, due to their memory declining. According to Broderick and Blewitt (2015) said that "Dementia is ...
Dementia Case Study Essay. 950 Words 4 Pages. As of 2010, an estimated 5.1 million Americans were affected by Alzheimer's Dementia and related Dementias (Hebert et al., 2003). Dementia is a syndrome that results in decline of memory and at least one other cognitive ability, significant enough to interfere with daily life activities (American ...
The End- of- Life Decision Making case study presents a problem where a public guardian has been appointed for Ms. Long, and is seeing her for the first time to compose an assessment, and make several determinations. One of those determinations is whether Ms. Long is terminally ill. Upon seeing her, the guardian takes note of the facts.
Essay for assignment case study: my patient mrs. diagnosed with dementia has an advance directive of do not resuscitate (dnr). dnr is type of legal order from. ... Dementia case study - Essay for assignment. University: Northern Virginia Community College. Course: Bio ethics (227) 5 Documents. Students shared 5 documents in this course.
Alzheimer's Case Studies. The Alzheimer's Association reports that by the year 2025, 7. 1 million people 65 and older will be suffering from Alzheimer's disease. Alzheimer's is a form of dementia and its devastating that there will be roughly 7. 1 million diagnosed with one specific form of dementia. With this skyrocketing increase will ...
Dementia Case Study Essay. Decent Essays. 1406 Words; 6 Pages; Open Document. The first questions will be to develop a history for information to understand what is wrong. There are several situations that might precipitate dementia-like symptoms. They will include questions on whether or not the person is on drugs. There are medicines that ...
The aim of the nurse is to have a person-centred dementia care, a holistic approach on caring for someone as a whole person and endeavouring to meet all their needs instead of focusing only on the physical aspect (Newton, 1991). The nurse should involve the patient and family on making a plan of care, as this preserve the dignity and respect of ...
Dementia Case Study. 1586 Words7 Pages. Care of a Confused Client. Introduction. Dementia is the umbrella term given to the various disorders that cause damage to the brain. Alzheimer's disease is the main type of dementia and accounts for more than 50% of all cases. The other main types of dementia are Vascular dementia, Lewy Body dementia ...
Case Analysis And Problems With Dementia Nursing Essay. Dementia is a progressive and irreversible decline in mental function1. Lewy Body Dementia (DLB) is a form of degenerative dementia characterised by the presence of "Lewy Bodies" which are clumps of alpha-synuclein and ubiquitin protein in neurons2. These are only detectable in post ...
Case in point: Legendary actor Bruce Willis. In a May 31 essay in Vogue, daughter Tallulah Willis opened up about her dad's 2022 diagnosis with aphasia, which impairs the ability to speak ...
Hire a Writer. (415) 520-5258. Level: College, High School, University, Undergraduate, Master's. The first step in making your write my essay request is filling out a 10-minute order form. Submit the instructions, desired sources, and deadline. If you want us to mimic your writing style, feel free to send us your works. In case you need ...