- Search Menu
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Papyrology
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Evolution
- Language Reference
- Language Acquisition
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Media
- Music and Religion
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Science
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Lifestyle, Home, and Garden
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Clinical Neuroscience
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Ethics
- Business Strategy
- Business History
- Business and Technology
- Business and Government
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic History
- Economic Systems
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Behaviour
- Political Economy
- Political Institutions
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Theory
- Politics and Law
- Public Policy
- Public Administration
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter
- Next chapter >


5 Psychiatric Treatment of Bipolar Disorder: The Case of Janice
- Published: February 2013
- Cite Icon Cite
- Permissions Icon Permissions
Chapter 5 covers the psychiatric treatment of bipolar disorder, including a case history, key principles, assessment strategy, differential diagnosis, case formulation, treatment planning, nonspecific factors in treatment, potential treatment obstacles, ethical considerations, common mistakes to avoid in treatment, and relapse prevention.
Signed in as
Institutional accounts.
- GoogleCrawler [DO NOT DELETE]
- Google Scholar Indexing
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
Institutional access
- Sign in with a library card Sign in with username/password Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Sign in through your institution
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Sign in with a library card
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

Real Life Bipolar Disorder: A Case Study of Susan
Bipolar disorder is a complex and often misunderstood mental health condition that affects millions of individuals worldwide. For those living with bipolar disorder, the highs and lows of life can be dizzying, as they navigate through periods of intense mania and debilitating depression. To truly grasp the impact of this disorder, it’s crucial to explore real-life experiences and the stories of those who have dealt firsthand with its challenges.
In this article, we delve into the fascinating case study of Susan, a woman whose life has been profoundly shaped by her bipolar disorder diagnosis. By examining Susan’s journey, we aim to shed light on the realities of living with this condition and the strategies employed to manage and treat it effectively.
But before we plunge deeper into Susan’s story, let’s first gain a comprehensive understanding of bipolar disorder itself. We’ll explore the formal definition, the prevalence of the condition, and its impact on both individuals and society as a whole. This groundwork will set the stage for a more insightful exploration of Susan’s experience and provide valuable context for the subsequent sections of this article.
Bipolar disorder is more than just mood swings; it is a condition that can significantly disrupt an individual’s life, relationships, and overall well-being. By studying a real-life case like Susan’s, we can gain a personal insight into the multifaceted challenges faced by those with bipolar disorder and the importance of effective treatment and support systems. In doing so, we hope to foster empathy, inspire early diagnosis, and contribute to the advancement of knowledge about bipolar disorder’s complexities.
The Case of Susan: A Real Life Experience with Bipolar Disorder
Susan’s story provides a compelling illustration of the impact that bipolar disorder can have on an individual’s life. Understanding her background, symptoms, and the effects of the disorder on her daily life can provide valuable insights into the challenges faced by those with bipolar disorder.
Background Information on Susan
Susan, a thirty-eight-year-old woman, was diagnosed with bipolar disorder at the age of twenty-five. Her early experiences with the disorder were characterized by periods of extreme highs and lows, often resulting in strained relationships and an inability to maintain steady employment. Susan’s episodes of mania frequently led to impulsive decision-making, excessive spending sprees, and risky behaviors. On the other hand, her depressive episodes left her feeling hopeless, fatigued, and unmotivated.
Symptoms and Diagnosis of Bipolar Disorder in Susan
To receive an accurate diagnosis, Susan underwent a thorough examination by mental health professionals. The criteria for diagnosing bipolar disorder include significant and persistent mood swings, alternating between periods of mania and depression. Susan exhibited classic symptoms of bipolar disorder, such as elevated mood, increased energy, racing thoughts, decreased need for sleep, and reckless behavior during her manic episodes. These episodes were interspersed with periods of deep sadness, loss of interest in activities, and changes in appetite and sleep patterns during depressive phases.
Effects of Bipolar Disorder on Susan’s Daily Life
Living with bipolar disorder presents unique challenges for Susan. The unpredictable shifts in her mood and energy levels significantly impact her ability to function in both personal and professional spheres. During manic phases, Susan experiences heightened productivity, creativity, and confidence, often leading her to take on excessive responsibilities and projects. However, these periods are eventually followed by crashes into depressive episodes, leaving her unable to complete tasks, maintain relationships, or even perform routine self-care. The constant fluctuations in her emotional state make it difficult for Susan to establish a sense of stability and predictability in her life.
Susan’s struggle with bipolar disorder is not uncommon. Many individuals with this condition face similar obstacles in their daily lives, attempting to manage the debilitating highs and lows while striving for a sense of normalcy. By understanding the real-life implications of bipolar disorder, we can more effectively tailor our support systems and treatment options to address the needs of individuals like Susan. In the next section, we will explore the various approaches to treating and managing bipolar disorder, providing potential strategies for improving the quality of life for those living with this condition.
Treatment and Management of Bipolar Disorder in Susan
Managing bipolar disorder requires a multifaceted approach that combines psychopharmacological interventions, psychotherapy, counseling, and lifestyle modifications. Susan’s journey towards finding effective treatment and management strategies highlights the importance of a comprehensive and tailored approach.
Psychopharmacological Interventions
Pharmacological interventions play a crucial role in stabilizing mood and managing symptoms associated with bipolar disorder. Susan’s treatment plan involved medications such as mood stabilizers, antipsychotics, and antidepressants. These medications aim to regulate the neurotransmitters in the brain associated with mood regulation. Susan and her healthcare provider closely monitored her medication regimen and made adjustments as needed to achieve symptom control.
Psychotherapy and Counseling
Psychotherapy and counseling provide individuals with bipolar disorder a safe space to explore their thoughts, emotions, and behaviors. Susan engaged in cognitive-behavioral therapy (CBT), which helped her identify and challenge negative thought patterns and develop healthy coping mechanisms. Additionally, psychoeducation in the form of group therapy or support groups allowed Susan to connect with others facing similar challenges, fostering a sense of community and reducing feelings of isolation.
Lifestyle Modifications and Self-Care Strategies
In addition to medical interventions and therapy, lifestyle modifications and self-care strategies play a vital role in managing bipolar disorder. Susan found that maintaining a stable routine, including regular sleep patterns, exercise, and a balanced diet, helped regulate her mood. Avoiding excessive stressors and implementing stress management techniques, such as mindfulness meditation or relaxation exercises, also supported her overall well-being. Engaging in activities she enjoyed, nurturing her social connections, and setting realistic goals further enhanced her quality of life.
Striving for stability and managing bipolar disorder is an ongoing process. What works for one individual may not be effective for another. It is crucial for individuals with bipolar disorder to work closely with their healthcare providers and engage in open communication about treatment options and progress. Fine-tuning the combination of psychopharmacological interventions, therapy, and self-care strategies is essential to optimize symptom control and maintain stability.
Understanding the complexity of treatment and management helps foster empathy for individuals like Susan, who face the daily challenges associated with bipolar disorder. It underscores the importance of early diagnosis, accessible mental health care, and ongoing support systems to enhance the lives of individuals living with this condition. In the following section, we will explore the various support systems available to individuals with bipolar disorder, including family support, peer support groups, and the professional resources that contribute to their well-being.
Support Systems for Individuals with Bipolar Disorder
Navigating the challenges of bipolar disorder requires a strong support system that encompasses various sources of assistance. From family support to peer support groups and professional resources, these networks play a significant role in helping individuals manage their condition effectively.
Family Support
Family support is vital for individuals with bipolar disorder. Understanding and empathetic family members can provide emotional support, monitor medication adherence, and help identify potential triggers or warning signs of relapse. In Susan’s case, her family played a crucial role in her recovery journey, providing a stable and nurturing environment. Education about bipolar disorder within the family helps foster empathy, reduces stigma, and promotes open communication.
Peer Support Groups
Peer support groups provide individuals with bipolar disorder an opportunity to connect with others who share similar experiences. Sharing personal stories, strategies for coping, and offering mutual support can be empowering and validating. In these groups, individuals like Susan can find solace in knowing that they are not alone in their struggles. Peer support groups may meet in-person or virtually, allowing for easier access to support regardless of physical proximity.
Professional Support and Resources
Professional support is crucial in the management of bipolar disorder. Mental health professionals, such as psychiatrists, psychologists, and therapists, provide expertise and guidance in developing comprehensive treatment plans. Regular therapy sessions allow individuals like Susan to explore emotional challenges and develop healthy coping mechanisms. Psychiatrists closely monitor medication effectiveness and make necessary adjustments. Additionally, case managers or social workers can assist with navigating the healthcare system, accessing resources, and connect individuals with other community services.
Beyond direct professional support, there are resources and organizations dedicated to bipolar disorder education, advocacy, and support. Online forums, websites, and helplines provide information, guidance, and a sense of community. These platforms allow individuals to access information at any time and connect with others who understand their unique experiences.
Support systems for bipolar disorder are crucial in empowering individuals and enabling them to lead fulfilling lives. They contribute to reducing stigma, providing emotional support, and ensuring access to resources and education. Through these support systems, individuals with bipolar disorder can gain self-confidence, develop effective coping strategies, and improve their overall well-being.
In the next section, we explore the significance of case studies in understanding bipolar disorder and how they contribute to advancing research and knowledge in the field. Specifically, we will examine how Susan’s case study serves as a valuable contribution to furthering our understanding of this complex disorder.
The Importance of Case Studies in Understanding Bipolar Disorder
Case studies play a vital role in advancing our understanding of bipolar disorder and its complexities. They offer valuable insights into individual experiences, treatment outcomes, and the overall impact of the condition on individuals and society. Susan’s case study, in particular, provides a unique perspective that contributes to broader research and knowledge in the field.
How Case Studies Contribute to Research
Case studies provide an in-depth examination of specific individuals and their experiences with bipolar disorder. They allow researchers and healthcare professionals to observe patterns, identify commonalities, and gain valuable insights into the factors that influence symptom presentation, treatment response, and prognosis. By analyzing various case studies, researchers can generate hypotheses and refine treatment approaches to optimize outcomes for individuals with bipolar disorder.
Case studies are particularly helpful in documenting rare or atypical presentations of bipolar disorder. They shed light on lesser-known subtypes, such as rapid-cycling bipolar disorder or mixed episodes, contributing to a more comprehensive understanding of the condition. Case studies also provide opportunities for clinicians and researchers to discuss unique challenges and discover innovative interventions to improve treatment outcomes.
Susan’s Case Study in the Context of ATI Bipolar Disorder
Susan’s case study is an example of how individual experiences can inform the development of Assessment Technologies Institute (ATI) for bipolar disorder. By examining her journey, researchers can analyze treatment approaches, evaluate the effectiveness of various interventions, and develop evidence-based guidelines for managing bipolar disorder.
Susan’s case study provides rich information about the impact of medication, psychotherapy, and lifestyle modifications on symptom control and overall well-being. It offers valuable insights into the benefits and limitations of specific interventions, highlighting the importance of personalized treatment plans tailored to individual needs. Additionally, Susan’s case study can contribute to ongoing discussions about the role of support systems and the integration of peer support groups in managing and enhancing the lives of individuals with bipolar disorder.
The detailed documentation of Susan’s experiences serves as a powerful tool for healthcare providers, researchers, and individuals living with bipolar disorder. It highlights the complexities and challenges associated with the condition while fostering empathy and understanding among various stakeholders.
Case studies, such as Susan’s, play a crucial role in enhancing our understanding of bipolar disorder. They provide insights into individual experiences, treatment approaches, and the impact of the condition on individuals and society. Through these case studies, we can cultivate empathy for individuals with bipolar disorder, advocate for early diagnosis and effective treatment, and contribute to advancements in research and knowledge.
By illuminating the realities of living with bipolar disorder, we acknowledge the need for accessible mental health care, support systems, and evidence-based interventions. Susan’s case study exemplifies the importance of a comprehensive approach to managing bipolar disorder, integrating psychopharmacological interventions, psychotherapy, counseling, and lifestyle modifications.
Moving forward, it is essential to continue studying cases like Susan’s and explore the diverse experiences within the bipolar disorder population. By doing so, we can foster empathy, encourage early intervention and personalized treatment, and contribute to advancements in understanding bipolar disorder, ultimately improving the lives of individuals affected by this complex condition.
Empathy and Understanding for Individuals with Bipolar Disorder
Developing empathy and understanding for individuals with bipolar disorder is crucial in fostering a supportive and inclusive society. By recognizing the unique challenges they face and the complexity of their experiences, we can better advocate for their needs and provide the necessary resources and support.
It is important to understand that bipolar disorder is not simply a matter of mood swings or being “moody.” It is a chronic and often debilitating mental health condition that affects individuals in profound ways. The extreme highs of mania and the lows of depression can disrupt relationships, employment, and overall quality of life. Developing empathy means acknowledging that these struggles are real and offering support and understanding to those navigating them.
Encouraging Early Diagnosis and Effective Treatment
Early diagnosis and effective treatment are key factors in managing bipolar disorder and reducing the impact of its symptoms. Encouraging individuals to seek help and reducing the stigma associated with mental illness are crucial steps toward achieving early diagnosis. Increased awareness campaigns and education can empower individuals to recognize the signs and symptoms of bipolar disorder in themselves or their loved ones, facilitating timely intervention.
Once diagnosed, providing access to quality mental health care and ensuring individuals receive appropriate treatment is essential. Bipolar disorder often requires a combination of pharmacological interventions, psychotherapy, and lifestyle modifications. By advocating for comprehensive treatment plans and promoting ongoing care, we can help individuals with bipolar disorder achieve symptom control and improve their overall well-being.
The Role of Case Studies in Advancing Knowledge about Bipolar Disorder
Case studies, like Susan’s, play a significant role in advancing knowledge about bipolar disorder. They provide unique insights into individual experiences, treatment outcomes, and the wider impact of the condition. Researchers and healthcare providers can learn from these individual cases, developing evidence-based guidelines and refining treatment approaches.
Additionally, case studies contribute to reducing stigma by providing personal narratives that humanize the disorder. They showcase the challenges faced by individuals with bipolar disorder and highlight the importance of support systems, empathy, and understanding. By sharing these stories, we can help dispel misconceptions and promote a more compassionate approach toward mental health as a whole.
In conclusion, developing empathy and understanding for individuals with bipolar disorder is essential. By recognizing the complexity of their experiences, advocating for early diagnosis and effective treatment, and valuing the insights provided by case studies, we can create a society that supports and uplifts those with bipolar disorder. It is through empathy and education that we can reduce stigma, promote accessible mental health care, and improve the lives of those affected by this condition.In conclusion, gaining a comprehensive understanding of bipolar disorder is crucial in order to support individuals affected by this complex mental health condition. Through the real-life case study of Susan, we have explored the numerous facets of bipolar disorder, including its background, symptoms, and effects on daily life. Susan’s journey serves as a powerful reminder of the challenges individuals face in managing the highs and lows of bipolar disorder and emphasizes the importance of effective treatment and support systems.
We have examined the various approaches to treating and managing bipolar disorder, including psychopharmacological interventions, psychotherapy, and lifestyle modifications. Understanding the role of these treatments and the need for personalized care can significantly improve the quality of life for individuals like Susan.
Support systems also play a crucial role in helping those with bipolar disorder navigate the complexities of the condition. From family support to peer support groups and access to professional resources, fostering a strong network of assistance can provide the necessary emotional support, education, and guidance needed for individuals to effectively manage their symptoms.
Furthermore, case studies, such as Susan’s, contribute to advancing our knowledge about bipolar disorder. By delving into individual experiences, researchers gain valuable insights into treatment outcomes, prognosis, and the impact of the condition on individuals and society as a whole. These case studies foster empathy, reduce stigma, and contribute to the development of evidence-based guidelines and interventions that can improve the lives of individuals with bipolar disorder.
In fostering empathy and promoting early diagnosis, effective treatment, and ongoing support, we create a society that actively embraces and supports individuals with bipolar disorder. By encouraging understanding, reducing stigma, and prioritizing mental health care, we can ensure that those affected by bipolar disorder receive the support and resources necessary to lead fulfilling and meaningful lives. Through empathy, education, and continued research, we can work towards a future where individuals with bipolar disorder are understood, valued, and empowered to thrive.
Similar Posts

Understanding and Managing Bipolar Anger Towards Parents
Have you ever felt a surge of anger towards your parents that seems to come out of nowhere? Or maybe you’ve witnessed your child’s intense outbursts and wondered what could be causing such extreme emotions. It’s…

3 Symptoms or Conditions That Could be Mistaken for Dementia
Did you know that not every case of forgetfulness or cognitive decline is due to dementia? In fact, there are several other conditions and symptoms that mimic the signs of this debilitating disease, often leading to…

The Importance of Mental Health and Depression Counseling in Brandon
Mental health is an integral part of our overall well-being, yet it often remains misunderstood and overlooked. As we go about our daily lives, we rarely stop to consider the state of our mental health or…

Understanding VA Bipolar Secondary to PTSD: Causes, Symptoms, and Treatment Options
The experience of war leaves an indelible mark on those who serve in the military. Some veterans return home carrying not only the physical wounds of combat but also the unseen burden of psychological trauma. Post-Traumatic…
Anxiety Disorders and Symptoms: Understanding Different Types and Common Behaviors
Imagine constantly feeling on edge, as if danger is lurking around every corner. Your heart races, your palms sweat, and your mind is plagued with worry. Anxiety disorders can be debilitating, affecting millions of people around…
Living with Bipolar Disorder: Coping Strategies for Those Unable to Work
Imagine waking up every morning, your emotions swinging from intense feelings of euphoria and boundless energy to deep pits of despair and hopelessness. Imagine the constant battle within your mind, making it almost impossible to maintain…
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- Winter 2024 | VOL. 22, NO. 1 Reproductive Psychiatry: Postpartum Depression is Only the Tip of the Iceberg CURRENT ISSUE pp.1-142
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Ethics Commentary: Ethical Issues in Bipolar Disorder: Three Case Studies
- Laura Weiss Roberts , M.D., M.A.
Search for more papers by this author
Sound ethical decision making is essential to astute and compassionate clinical care. Wise practitioners readily identify and reflect on the ethical aspects of their work. They engage, often intuitively and without much fuss, in careful habits—in maintaining therapeutic boundaries, in seeking consultation from experts when caring for difficult or especially complex patients, in safeguarding against danger in high-risk situations, and in endeavoring to understand more about mental illnesses and their expression in the lives of patients of all ages, in all places, and from all walks of life. These habits of thought and behavior are signs of professionalism and help ensure ethical rigor in clinical practice.
Psychiatry is a specialty of medicine that, by its nature, touches on big moral questions. The conditions we treat often threaten the qualities that define human beings as individual, as autonomous, as responsible, as developing, and as fulfilled. The conditions we treat often are characterized by great suffering, disability, and stigma, and yet individuals with these conditions demonstrate such tremendous adaptation and strength as well. If all work by physicians is ethically important, then our work is especially so.
As a service to FOCUS readers, in this column we endeavor to provide ethics commentary on topics in clinical psychiatry. We also proffer clinical ethics questions and expert answers in order to sharpen readers’ decision-making skills and advance astute and compassionate clinical care in our field.
Ms. Genera is a 36-year-old woman with bipolar II disorder, first diagnosed in college, who is brought to the psychiatric emergency room by her boyfriend of 5 years. He is hoping that she will be admitted to the hospital “before she goes all-the-way manic.” He reports that she “almost lost her job last time!”
Over the past 6 weeks, he reports that Ms. Genera has needed “less and less” sleep, has been cleaning the house “around the clock,” and has “wanted a lot of sex even though she is really pissed off all of the time.” The patient states that she is “fine, more than fine, in fact.” She says that she has not been able to sleep “because of the neighbors.” She says that they talk loudly at night and that she and the baby will “fix that” because babies are “noisy at night too!” Her boyfriend is confused by this comment, saying that they have no children—“I don’t know why she says stuff like that. I know it’s the manic-depressive, but it is pretty crazy.” Ms. Genera states that her thoughts are like “O’Hare airport!” and that she has “no problem keeping up” with the different “planes coming and going.” The patient says that she stopped taking all of her medications about 3 months ago—“That lithium is really hard on me. I don’t like to take it unless I have to.” She has no history of alcohol or other substance use, no history of suicide attempts, and no history of dangerousness toward others.
On mental status exam, Ms. Genera is a neatly dressed, mildly overweight woman who appears slightly older than her stated age. She is cooperative with the clinical interview and asks that her boyfriend step out of the room when she is talking with the doctor. She is speaking quickly and loudly, with appropriate affect. Her thought form is linear. She denies hallucinations and reports no thoughts of self-harm.
Ms. Genera says that she has “Bipolar II, not Bipolar I—I don’t have it that bad. Never have. Yessirree, I am really good right now.” She does not want to be admitted to the hospital, despite her boyfriend’s request, but volunteers that she will go to an ambulatory care appointment with her psychiatrist on the next day.
——1.3 The psychiatrist arranges to speak with Ms. Genera alone during the clinical interview.
——1.4 The psychiatrist respects the patient’s preference not to be admitted to the hospital.
——1.5 The psychiatrist recommends diagnostic tests to occur at the time of the emergency evaluation.
——1.6 The psychiatrist sits with the patient’s boyfriend to offer emotional support and “a listening ear” after the clinical interview with the patient is completed.
——1.7 The psychiatrist documents accurately in the electronic medical record the full set of concerns raised by the patient and her boyfriend.
A resident in internal medicine with a well-established diagnosis of bipolar I disorder volunteers for a clinical trial that will test a new combination of medications and also involve two neuroimaging studies. The resident discusses the trial with his psychiatrist, who discourages the idea, stating that he has been concerned about the resident-patient, given the stresses of training and the severity of his illness. The resident responds, “Hey, Doc—get real! How often can you get $500—plus a brain scan, let alone TWO—free of charge?!” He decides to undergo screening for the clinical trial because he thinks he might benefit medically from an imaging test.
The resident knows that the trial will involve a washout period, so he decides to taper his medications in advance of the “official” enrollment date, 3 weeks away, which coincides with a planned vacation. Without medication, the resident becomes increasingly symptomatic. He has difficulty concentrating, becomes easily upset with team members, and develops progressively more erratic sleep. He was seen standing on the roof of the academic hospital and confided in a roommate that he was “tired of it all.”
Although he originally met criteria for the project, by the time of enrollment he had become too ill to enter the study. The psychiatrist-investigator permitted him to have the baseline neuroimaging study but did not allow the resident to progress to the full clinical trial. The resident returned to his apartment for his weeklong vacation. On the day he was scheduled to return to his training program, he did not turn up.
An 18-year-old male previously diagnosed with bipolar disorder is brought by his best friend to the emergency department of a rural hospital located near a ski area. The best friend reports that the patient “is completely wild—he just won’t stop—he’s going to kill himself on the slopes!”
The patient was first diagnosed when he experienced a “flat out manic” episode at age 13 years; he has been stable and doing well on lithium. He has a psychiatrist and therapist “back home,” although he will not provide their names.
The patient confided to his best friend that he “secretly” stopped his lithium recently, and the best friend states that the patient has been using alcohol. (“He says, ‘I like to get high while I’m high.’ ”) The patient is on vacation with his grandparents, two younger siblings, and the best friend.
The patient shows evidence of intoxication and is irritable but cooperative during the initial interview in the emergency department. His vitals are within normal limits and are stable. No abnormalities are found on physical examination.
While waiting to be seen, the patient appears to “sober up.” He is calm, pleasant, and respectful and thanks his friend and the emergency staff for helping him. He appears embarrassed. No abnormalities are found on mental status examination. The patient refuses a drug or urine test, and he refuses to allow the emergency physician to contact his grandparents or parents. The emergency physician calls a psychiatrist for consultation, which the patient declines.
Laura Weiss Roberts, M.D., M.A., Professor, Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine, Stanford, CA
Dr. Roberts reports: Owner, Investigator: Terra Nova Learning Systems
Srivastava S : Ethical considerations in the treatment of bipolar disorder . Focus ( Fall ); 9(4):461–464. Link , Google Scholar
Roberts LW, Hoop JG : Professionalism and Ethics: Q & A Self-Study Guide for Mental Health Professionals . Washington, DC, American Psychiatric Publishing, 2008 . Google Scholar
Roberts LW, Dyer A : A Concise Guide to Ethics in Mental Health Care . Washington, DC, American Psychiatric Publishing, 2004 . Google Scholar
- Cited by None

A Closer Look: Case Study on Bipolar Mood Disorder
In the days of Hippocrates, you'd likely attribute the erratic behaviors associated with bipolar mood disorder to an imbalance of bodily humors, but today, you know it's far more complex than that.
As you peruse the pages of this case study, you'll join the intricate journey through the life of a patient with bipolar disorder, whose story might resonate more deeply than you'd expect. You'll witness the oscillation between the highs of mania and the lows of depression, and understand why recognizing the nuances of this condition is pivotal.
The chronicle ahead lays bare the challenges of diagnosis, the trials of treatment, and the reality of living with a mood disorder that's as unpredictable as the weather in April.
Consider for a moment the impact of a single misstep in the delicate dance of managing bipolar disorder—you'll soon see why this case demands your attention, and perhaps, why it might change the way you view mental health care forever.
Key Takeaways
- Bipolar disorder is a complex mental health condition characterized by significant mood swings.
- Family support is critical in managing mental health challenges.
- Understanding the rhythm of mood fluctuations is crucial for managing bipolar disorder.
- Creating a consistent routine and having a strong support system are key to managing daily life with bipolar disorder.
Understanding Bipolar Disorder
Bipolar disorder is a complex mental health condition characterized by significant mood swings that can impact a person's thoughts, feelings, and behaviors. If you're grappling with this, you're not alone; it's a challenge faced by many.
Understanding bipolar mood disorders involves recognizing the pendulum-like shift between manic and depressive episodes. You may wonder if your intense high energy levels or periods of depression are signs of this condition. The diagnosis of bipolar is a critical step and involves a thorough assessment by a healthcare professional. They'll look at your symptoms, how long they last, and how they're affecting your life. It's not just about feeling up and down; it's a pattern that can wreak havoc if not properly managed.
To keep these fluctuations in check, a mood stabilizer is often prescribed. These medications help balance your moods and prevent the extreme highs and lows associated with bipolar disorder. It's essential to adhere to the treatment plan and communicate openly with your healthcare provider about how you're feeling.
Patient Background Profile
Understanding the nuances of bipolar disorder sets the stage for exploring the personal journey of Gary, a 19-year-old whose life was upended by this mental health challenge. Diagnosed with bipolar disorder, Gary's world shifted dramatically during his college years. His manic episode led to a sudden withdrawal from college and an unexpected switch from engineering to philosophy. This was a significant departure from his usual behavior, marked by reduced sleep, engaging in long, intense conversations, and exhibiting grandiose beliefs.
Gary's adolescent years were peppered with warning signs, including periods of withdrawal and depression, which may have hinted at his underlying condition. A family history of mental health issues can often be a precursor to such diagnoses, though Gary's case doesn't explicitly mention this. However, it's known that family support can be critical, and Gary's parents are no exception; they're eager to be involved in his treatment, recognizing early signs of anxiety and depression in his past.
The disruption in Gary's academic performance and personal relationships necessitated a robust treatment plan. Placed on a mood stabilizer and antipsychotic medication, Gary was also recommended adjunctive psychotherapy to help manage his condition and work towards stable behavior and improved functioning.
Episode Chronology
Mapping out the episode chronology in Gary's journey with bipolar disorder reveals the patterns and frequency of his mood swings, providing invaluable insights for managing his care. You'll notice that his major depressive disorder phases often follow intense hypomanic episodes, suggesting a cycle that dictates the rhythm of his life.
Understanding Gary's episode chronology, you'll see that the periods between his mood swings aren't just random; they're clues to what triggers his episodes. Maybe it's stress, lack of sleep, or even changes in the seasons. By keeping track of these patterns, you've got a better shot at predicting and heading off future episodes.
Treatment Approaches
Having explored the rhythm of Gary's mood fluctuations, it's crucial now to focus on how best to manage his bipolar disorder through effective treatment approaches. Treating bipolar can be complex, and it requires a tailored plan that takes into account his unique needs. Here's what you need to keep in mind:
- Medication Management
- Mood stabilizers are often the first line of defense; valproic acid, for instance, can be effective in controlling mood swings.
- Antipsychotics may be added for additional symptom control.
- Regular monitoring for side effects is key to maintaining overall health.
- Psychoeducation
- Understanding bipolar disorder and its management is empowering for you and your family.
- Knowledge about triggers and symptoms aids in early intervention.
- Collaborative Care
- Psychiatrists, therapists, and primary care providers should all be in sync when managing bipolar disorder.
- Communication between healthcare professionals ensures a cohesive and comprehensive approach.
Managing Daily Life
You'll find that creating a consistent routine is key to managing your daily life with bipolar mood disorder.
It's also vital to have a strong support system in place, as the people around you can provide essential help and understanding.
These strategies will help you maintain stability and manage the ups and downs that come with your condition.
Routine Structuring Strategies
Implementing a structured daily routine can significantly ease the management of bipolar disorder symptoms, offering stability and predictability in your life. Here's how you can tailor your daily routine to manage mood dysregulation effectively:
- Set regular times for:
- *Sleep:* Consistent sleep patterns stabilize your mood.
- *Meals:* Regular meals help maintain energy levels.
- *Exercise:* Physical activity is key in managing stress.
Prioritizing these aspects of your routine can lead to better adherence to adequate treatment and improve your overall well-being.
Support System Importance
Leaning on a robust support system, you can navigate the complexities of daily life with bipolar disorder more effectively, ensuring a network of care that promotes stability and well-being. Your support system's importance can't be overstated—it's the foundation that holds you steady amidst the shifting sands of emotions and challenges.
Here's a snapshot of how a strong support network can help you manage essential aspects of your life:
Reflecting on Progress
Reflecting on your progress with bipolar mood disorder, it's essential to evaluate how diagnosis and treatment have influenced your daily life and mental health. You've likely noticed changes in your clinical presentations, and it's crucial to track these shifts. Consider the following:
- Patient Reported Outcomes
- *Symptom Management*: Have you experienced a reduction in the frequency or severity of mood episodes?
- *Quality of Life*: Are you finding more stability and enjoyment in your daily activities?
- *Self-Awareness*: Have you become more attuned to your triggers and early warning signs?
Adherence to your treatment plan plays a pivotal role in your journey. Engaging with your healthcare provider allows for necessary adjustments and ensures that your mental health remains a priority. Comorbid conditions and lifestyle factors also significantly impact your treatment response, necessitating a holistic approach to your well-being.
Regular monitoring is key to managing side effects and maintaining overall stability. By collaborating with your care team and being proactive about your health, you're laying the groundwork for continued progress and a more balanced life.
Frequently Asked Questions What Are Some Interesting Research Topics on Bipolar Disorder?
You might explore the genetic basis of bipolar disorder, the effectiveness of psychotherapy combined with medication, or the impact of lifestyle factors on symptom management in your research.
What Is the Average Age of Death for a Person With Bipolar Disorder?
You've asked about the average age of death for someone with bipolar disorder. It's sadly shorter, typically 9 to 20 years less than the general population, ranging from 47 to 61 years old.
What Is the Leading Cause of Death in Bipolar People?
You should know that the leading cause of death in bipolar people is suicide, a tragic consequence that underscores the importance of vigilant care and support for those managing this condition.
How Does Bipolar Disorder Affect Someone's Everyday Life?
Bipolar disorder is like an unpredictable storm, disrupting your daily life with extreme mood swings that can hinder your work, strain relationships, and make sticking to routines feel nearly impossible.
You've journeyed through the labyrinth of bipolar disorder, navigating its highs and lows alongside our patient. From the chaos of misdiagnosis to the anchor of tailored therapy, you've seen the transformation. Like a time traveler who's witnessed history's pivotal turn, you understand now how crucial timely intervention is.
Let's celebrate the milestones, recognizing that with acceptance and consistent care, managing bipolar disorder isn't just a possibility—it's a reality etched in the annals of personal triumph.

Daniel Logan is a renowned author and mental health expert who specializes in psychology and mental health topics. Daniel holds a degree in psychology from the University of California, Los Angeles (UCLA). With years of experience in the field, he has become a trusted voice in the industry, sharing insights and knowledge on a variety of mental health issues.
Top Mood Disorder Treatment Centers: A Comparative Review
Creating an Effective Disruptive Mood Dysregulation Disorder Treatment Plan: A PDF Guide
Best Weed Strains for Anxiety: A Comprehensive Guide
Can You Get SSI for Borderline Personality Disorder? A Comprehensive Guide
Disruptive Mood Dysregulation Disorder Vs Intermittent Explosive Disorder: a…
Comprendiendo Los Trastornos Del Estado De Ánimo: Una Guía Completa En…
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.

No thanks, I’m not interested!
Puer Aeternus: The Eternal Child Archetype
Dark Psychology & Manipulation: Types, Symptoms, Overcoming
Nurturing Minds: True Life Care Mental Health in Morris Plains, New Jersey
Nurturing Mental Health Treatment in New Jersey: A Comprehensive Approach to True…
- Clinical Depression
- Anxiety Disorders
- Dissociative Disorder
- Motor Disorders
- Attention Deficit Hyperactive Disorder
- Discrete Trial Training
- Montessori and ABA
- Rational Emotive Behavior Therapy – REBT
- Cognitive Behavior Therapy
Self Improvement Through Hypnosis, Hypnotherapy and Raikov Effect
5 Freelancers Side Projects to Make Extra & Depression Free Earning
- Privacy Policy
Welcome, Login to your account.
Recover your password.
A password will be e-mailed to you.
Globalize your Research
A Case Study on Bipolar Affective Disorder Current Episode Manic Without Psychotic Symptoms
- International Journal of Clinical Case Reports and Reviews
Introduction
Method and research design:, result and discussion:, conclusion:, quick links.
- Aims and scope
- Article processing charges
- Editorial board
- Editorial Workflow
Case Report | DOI: https://doi.org/10.31579/2690-4861/290
- Bhadra Sharma E 1
- Sannet Thomas 2*
1 MSc. Psychology Student, Parumala Mar Gregorios College, Valanjavattom, Tiruvalla, Kerala, India.
2 Doctoral Research Scholar, Department of Applied Psychology, Veer Bahadur Singh Purvanchal University, Jaunpur, Uttar Pradesh, India.
*Corresponding Author: Sannet Thomas, Doctoral Research Scholar, Department of Applied Psychology, Veer Bahadur Singh Purvanchal University, Jaunpur, Uttar Pradesh, India.
Citation: Bhadra Sharma E., Thomas S., (2023), A Case Study on Bipolar Affective Disorder Current Episode Manic Without Psychotic Symptoms, International Journal of Clinical Case Reports and Reviews. 13(1); DOI: 10.31579/2690-4861/290
Copyright: © 2023 Sannet Thomas, This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 16 January 2023 | Accepted: 19 January 2023 | Published: 30 January 2023
Keywords: mood disorders; bipolar affective disorder; mania; depression
Mood disorders are the second most common condition and can repeat for a variety of reasons. Bipolar mood disorders can cause severe manic and depressed episodes that, if not adequately treated, can result in substantial social and personal problems. This study used a single case study approach and was qualitative in nature. A patient with bipolar affective disorder without psychotic symptoms participated in the trial. A case history form and a mental state assessment instrument were used to gather the data, which was then analysed using the content analysis approach. A 27-year-old lady who has been diagnosed with bipolar affective disorder and is now experiencing a manic episode without psychotic symptoms served as the study's sample. The patient was a resident of a private mental health facility in Kerala. This study discovered that pharmacotherapy, family therapy, in-patient rehabilitation, out-patient rehabilitation, and cognitive behavioural therapy can all help manage bipolar affective disorder, current episode manic without psychotic symptoms. The outcome of the current study comprises a thorough analysis of the sample's history and present conditions, along with interventions and management techniques.
A mood disorder, formerly known as an affective disorder, is an emotional condition that primarily affects our state of mind. A clinically significant disturbance in how a person feels in connection to their surroundings, which results in unhelpful behavior, characterizes a set of mental illnesses known as mood disorders. (Claudio & Andrea, 2022). The primary issue with these diseases is a shift in mood or affect, typically toward melancholy or elation. (ICD-10). Seasonal affective disorder (SAD), major depressive disorder (MDD), and bipolar disorder (BD) are a few examples of mood disorders. These conditions can also be further classified according to the severity, timing, or suspected cause of the illness. (APA, 2013). Patients with mood disorders have bodily and cognitive abnormalities that impair their ability to function. One such change is the disruption of the sleep–wake cycle, which shows up both physiologically and behaviourally. (Claudio & Andrea, 2022).
Mood disorder patients exhibit two key moods: mania and depression. The extreme sorrow and hopelessness that characterize depression (Hooley et al., 2016). People during depressive episodes will have a persistent depressed mood and may lose interest in previously pleasurable activities along with significant changes in sleep pattern and appetite for at least two weeks. According to the diagnostic criteria of DSM-5, symptoms of a depressive episode include depressed mood, significant changes in sleep patterns and appetite, psychomotor agitation or retardation, diminished ability to think and concentrate, and recurrent thoughts of death. 60percentage to 90percentage of major depressive disorder patients experience sleep difficulties, with insomnia and hypersomnia being the most prevalent disorders. This varies depending on how severe the depression is. (Abad & Guilleminault, 2005).
Mania is the other major mood. The extreme and irrational enthusiasm and exhilaration that characterizes mania. When experiencing a manic episode, a person's mood is noticeably heightened and expansive, perhaps being interrupted by intensely irritable outbursts. (Hooley et al., 2016). For a precise diagnosis, these significant mood swings must last for at least a week. The existence of an abnormally high, expansive, and irritable mood for at least four weeks is the hallmark of the milder variant known as a hypomanic episode. Considering its difficult clinical presentations and long-term view, a patient with mania must be provided with a personalized treatment for functional recovery. Psychoeducational strategies are also used for the maintenance of treatment results (Pacchiarotti et al., 2020).
There are two main classifications of mood disorders. Both unipolar and bipolar mood disorders exist. Unipolar mood disorders are characterized by the recurrent occurrence of full-blown depressive episodes. For a clear diagnosis, the person must show the symptoms of a depressive episode for longer than two weeks. If a person suffers from the occurrence of depressive episodes for about two years, then the person can be diagnosed as having persistent depressive disorder (PDD) or formerly known dysthymia. Here the symptoms are commonly found as half-blown (Hooley et al., 2016).
Bipolar mood disorders are characterized by the presence of both key moods, that is, Depression and mania. A person with bipolar disorder may alternatively experience both depressive and manic episodes (Hooley et al., 2016). Bipolar I disorder and bipolar II disorder are subtypes of bipolar disorders. Among these, the occurrence of mixed episodes—which are characterized by symptoms of both full-blown manic and severe depressive episodes lasting at least one week—signals the existence of bipolar I disorder. When a person has significant depressive periods and hypomanic episodes, bipolar II disorder is identified. When a full-blown manic episode is lacking in a patient with bipolar II disorder, this condition is known as cyclothymia. When someone exhibits half-blown bipolar mood disorder symptoms for at least two years, it is diagnosed. (World Health Organization, 1992).
Suicide and mood problems are related. Compared to the non-clinical population, the clinical group has a much greater prevalence of suicidal conduct. (Shah et al., 2022). Mood disorders can occur with or without psychotic symptoms and they can be seen as associated with somatic symptoms (World Health Organization, 1992). It was shown that kids with social anxiety disorder were more likely to also have a mood problem. It was discovered that those kids had more significant anxiety issues prior to therapy. Recent research says that the treatment of mood disorders was related to anxiety reduction (Baartmans et al., 2022).
Causal factors of mood disorders focus on biological, psychological, and socio-cultural factors. Family studies and twin studies have indicated that the prevalence of mood disorders is around two to three times greater among blood relatives due to biological variables. (Akdemir&Gokler, 2008). This shows the genetic influence in increasing the vulnerability towards the development of unipolar mood disorders. Neurochemical factors and hormonal regulatory and immune system abnormalities can also contribute to mood disorder development. psychological root causes Consider stressful life situations as key causative variables. Numerous studies have demonstrated that extremely stressful life situations might serve as precursors for mood disorders. Numerous studies have shown that this illness has an impact on patients' whole families and may reduce their fortitude and adaptability.
Treatment and management of mood disorders include pharmacotherapy, psychotherapy, and alternative biological treatments. Pharmacological methods cannot be avoided in the treatment of mood disorders. Anti-depressants, anti-psychotics, and mood-stabilizing drugs are found to be commonly used in treating mood disorders. Monoamine oxidase inhibitors (MAOs) and selective serotonin reuptake inhibitors are examples of antidepressants (SSRIs). Patients with mood disorders are treated with lithium as a mood stabilizer. Several forms of psychotherapy are used widely for treating mood disturbances [Datta et al., 2021].
It is common to employ therapies including behavior activation therapy, family and marital therapy, interpersonal therapy, and cognitive behavioral therapy (CBT). In addition to these pharmacological methods and psychotherapies, several biological approaches include electroconvulsive therapy (ECT), bright light therapy, and deep brain stimulation.
When a person has bipolar affective disorder, the present episode is manic without psychotic symptoms (ICD F30.1) and they have previously experienced at least one prior affective episode (hypomanic, manic, depressed, or mixed). (ICD 10) Mania is defined by an elevated mood that is discordant with the patient's condition and lacks psychotic symptoms. It can range from thoughtless merriment to practically uncontrollable excitement. Increased energy that comes with elation causes overactivity, pressure in speaking, and a reduced desire for sleep. There is a lack of continuous attention, and distractions are frequently obvious. Overconfidence and lofty ideals can inflate one's sense of self-worth. Loss of typical social inhibitions can lead to actions that are careless, foolish, or out of character for the situation. (ICD 10).
Relevance Of the Study:
Mood disorders are the second most prevalent type of disorder in psychopathology. Mood disorders are commonly seen with relapses and recurrences. So, a continuation of medication and follow-up sessions are necessary. However, at least half of the people are never receiving adequate treatment. So, this particular study can help in reducing stigma and human rights violations towards the affected people. And, through this particular study, people can have more awareness about mood disorders, Specifically the bipolar affective disorder, current episode manic without psychotic symptoms.
Review Of Literature:
Shah, K., Trivedi, C., Kamrai, D., Srinivas, S., & Mansuri, Z. (2022) conducted a study on suicide in adolescents with mood disorders. The study's goals were to examine the relationship between youth suicide and mood disorders as well as the influence of comorbid conditions in disruptive mood dysregulation disorder on adolescent suicidal thoughts. The National Inpatient Sample dataset was utilized in the study to select individuals with mood disorders, and the Chi-square test was employed to compare groups. According to the study, teenagers with mood disorders who do not have disruptive mood dysregulation disorder had approximately double the chance of having suicidal thoughts or actually attempting suicide.
Baartmans, J. M. D., van Steensel, F. J. A., Klein, A. M., & Bögels, S. M. (2022) conducted a study on The Role of Comorbid Mood Disorders in Cognitive Behavioral Therapy for Childhood Social Anxiety. The study aimed to determine the degree of occurrence of mood disorders as the result of cognitive behavioral therapies in children with social anxiety. The sample of the study consisted of 152 children who were clinically diagnosed as having social anxiety or any other anxiety disorder. The findings imply that children with social anxiety are more likely than those with other anxiety disorders to also have comorbidity with a mood condition.
Rashid, M. H., Ahmed, A. U., & Khan, M. Z. R. (2019) conducted a study on substance abuse among bipolar mood disorder patients. Determine the prevalence of drug use among patients with bipolar mood disorder was the goal of this descriptive cross-sectional investigation. 115 bipolar patients made up the sample; both males and females, inpatients and outpatients, were taken into account. Data collection was done using a standardized questionnaire. According to the survey, 23.8percentage of the respondents engaged in drug misuse.
Deepika, K. (2019). conducted a study on a case report on bipolar affective disorder: Mania with psychotic symptoms. The study adopted the method of a case study which aims to find the key characteristics and implications of mania with psychotic symptoms.
Akdemir, D., & Gokler, B. (2017) conducted a study on psychopathology in the children of parents with a bipolar mood disorder. The purpose of the study was to determine how frequently offspring of parents with bipolar mood disorder experience mental illnesses. 33 children of 28 control parents and 36 children of 28 parents with bipolar I illness made up the sample. The SADS-L (Schedule for Affective Disorders and Schizophrenia-Lifetime Version) and the SADS-L for School-Aged Children (Present and Lifetime Version) are screening tools (K-SADS-L). According to the study, children of parents with bipolar illness had a greater prevalence of psychopathology than children of the control group.
A case study can be defined as a record of research that consists of information about the development of a particular individual, group, or situation over time. It is a systematic investigation of a single individual or group of individuals which uses several statistical and psychological tools (McCombes, 2022)
The present study adopted the case study method. It is consisted with combined form of exploratory, cumulative and critical instance case studies. As a case study is an in-depth investigation of a person, a group of individuals, or a unit with the intention of generalizing it on several occasions. it allows us to explore the characteristics, meanings, and implications of the particular case. Exploratory case study involves detailed research of the subject aimed at providing an in-depth understanding of the study. Cumulative case study involves generalizing a phenomenon after collecting information from different sources. Critical instance case study aims in determining the cause and consequences of an event.
In this case study, case history and mental status examination have been taken from the client and informants. Information collected was cross-checked and reversed twice, and reliability and adequacy were also assured.
Sample Description:
A 27-year-old female inpatient with the bipolar affective disorder, current episode manic without psychotic symptoms. The patient was a married woman from a middle-class family who has been taking treatment for the past 10 years. The case was taken from one of the private mental health establishments in Kerala to which the patient was admitted. The patient was admitted to the hospital for 20 days, from there the data were collected by the researcher.
The present study uses Mental Status Examination (MSE) and case history. An MSE is an inevitable part of the clinical assessment which helps find the current state of the client, under the domains of general appearance, mood, affect, speech, thought process, perception, cognition, insight, and judgment.
A case history includes an in-depth analysis of a person or group. It mainly has detailed information relating to the patient’s psychological and medical conditions. A case history is used to get a client’s test results, and professional, sociological, occupational, and educational data. The data collected in a case history includes socio-demographic data, presenting complaints and their duration, nature of the illness, history of present illness, negative history, treatment history, family history, personal history, and pre-morbid personality.
Data Analysis:
The Present study uses the tool content analysis for analyzing data. Content analysis is a research tool that helps analyze the presence, meaning, and relationship of certain words or concepts. Content analysis is also helpful in quantifying the collected information.
Ethical Concerns:
Full consent from the participant was obtained. The confidentiality of the data collected from the participant was ensured. The participant is not harmed in any way. The anonymity of individuals and the privacy of the participant is ensured.
Case History:
Socio-demographic data: The patient named J.O.V., is a 27-year-old female, hailing from a middle-class family who has been educated up to plus two and is presently unemployed. She was a married woman and mother of a 2-year-old child. The informants were the patient, her husband, and her sibling. The collected information was adequate and reliable.
Presenting complaints and their duration: Reported by the patient- The patient has reported that she was suffering from a decreased need for sleep and tended to throw objects when got angry, for the last seven months. For the past four months, she an increased craving for food and a feeling that people are avoiding her complained and also complains that her family is cursing that she is not attending to her child properly.
Reported by the informant: The informant has complained of lack of sleep (not sleeping for about 48 hours), not giving proper attention to the child, suicidal tendency, increased talk, getting raised easily, and throwing objects when got raised for the past seven months. They also complained about spending a lot of money on buying mobile phones, ornaments, and gadgets, and, overuse of mobile phones for the past four months.
Nature of illness: The onset of illness was found to be gradual. The course was episodic and stable progress has been identified. Precipitating factors were not elicited.
History of present illness: The patient was maintaining normal till seven months back. Then she started getting raised quickly without any reason and experienced a decreased need for sleep. She felt that everyone around her is trying to avoid her. When having such feelings, she preferred to be alone and isolated herself. At times she lost her interest in everything, so she will not do anything and simply sit alone without doing anything. After that, the patient started spending a lot of money buying ornaments, mobile phones, and gadgets. She experienced an increased craving for food. She had the wish to eat all time a day. Before four months her mood suddenly changed to an extraordinary sadness and continued lack of sleep. Then she started to elicit highly irritable behavior with increased talk. Her symptoms caused impairments in her personal and social life, as she became more irritable with decreased sleep and a situation of missing from the house. As she began not to attend even her child properly, her family brought the patient to one of the private hospitals in Kerala for treatment and getting In-patient care.
Negative history: The patient has no history of head injury, trauma, epilepsy, headache, and vomiting. There is no history of psychoactive substance use. The patient shows no history of seeing or hearing things that others cannot see or hear. There is no history of the patient having repeated ideas, thoughts, or images coming to her mind. The patient has no history of irrational fear towards objects, events, or situations.
Treatment history: The patient had taken treatment with in-patient care previously from another private hospital in Kerala. Then she took treatment from one of the Government medical colleges, Kerala In-Patient care for 20 days. In 2017, treatment was taken from another private hospital, in Kerala for 20 days. Then she took treatment from another Government medical college, several times.
History: When the patient was 17 years old, the family identified behavioral changes such as increased talk, decreased need for sleep, and irritability. The patient was complaining that these changes occurred as a result of losing her friendship and love. But the family is not giving assurance for her complaint. Then she was taken to a private mental health centre, in Kerala for treatment and In-Patient care. There found an improvement with the treatment. She got married at the age of 21 years. After marriage, she started to show her symptoms including irritable behavior and increased talk. Due to this, the relationship got divorced 3 months after the marriage. After the divorce, she attempted suicide by jumping into a well. So, she was taken to one among the Government medical college hospital in Kerala, and was admitted for about 20 days (2015). The patient showed improvement with the treatment. Approximately 1 year later her symptoms started to reappear, and she went to another hospital alone for gaining treatment (according to the client). But the family brought her back and took treatment at a private mental health centre as in-patient for 20 days (2017). She showed improvement with the treatment. After that the client showed similar symptoms and has been getting medical care as in-patient several times from Government medical college, Kerala. 4 years later, she got married again. The relationship happily continued and she gave birth to a child. 7 months back she got hit by the current episode.
Family history: Consanguinity is absent. The patient belongs to a middle-class family, where her husband and brother are the earning members. The patient’s father is the family decision-maker. The patient maintained a good relationship with the family. General interaction within the family is good. There is a history of the psychiatric problem in her family. There found a history of wandering and missing out(grandfather). In the mother’s family, there is a history of suicide(grandfather) and mental illness(grandmother). The information about the illness is not known adequately. Her mother shows a history of bipolar affective disorder and her elder sister has a history of suicidal attempts and thyroid. There is no history of substance abuse in the family. The family is aware of the patient’s illness. Several members of the patient’s family show mental and behavioral dysfunctions and there are interpersonal conflicts in the family. So, family dynamics are dysfunctional.
Personal history: The birth and development of the patient were appropriate. There are no complications during delivery. The delivery was full-term and normal at the hospital. There are no significant abnormalities in the pre-natal and post-natal development. The development milestones were age appropriate. The patient was brought up by their mother. There is no maternal deprivation observed. There is no history of neurotic traits such as nail biting, body rocking, night terrors, phobias, and stammering. Education history started education at 5 years. She belongs to an average student. The medium was Malayalam. She had many friends but the relationships were not well maintained. She discontinued her degree (BA Literature) during her first year due to illness. Relationships with teachers were not good. Occupation history: The patient started an occupational career at the age of 25. She worked as a sales girl in a gold shop for about 2 months and left the job due to the pandemic situation.
Marital history: The patient got married at 21. The marriage was an arranged one with the consent of the family but got divorced after a relationship of only 3 months. Her disorder was the primary reason for the divorce. After 4 years, when she was 25 years old, she married again. The marriage was also an arranged one with the consent of the family. The husband is supportive. Currently, the client and her husband are satisfied with the relationship. Sexual history: the mode of gaining sexual knowledge is from friends. No history of sexual abuse is found. Marital sexual life is also satisfied. Menstrual history: menstrual cycle(menarche) begins at the age of 14 years. There are no significant abnormalities in the response to menarche noted. Then after the menstruation is regular till now. There were no mood swings during the menstrual cycle, but the client complained about back pain during menstruation. Substance use history, the patient has no history of any psychoactive substance use.
Pre-morbid personality: Attitude towards self, she was a confident personality but was not able to make decisions. And she maintains an average level of self-esteem. Attitude towards others: she was an extrovert who quickly feels empathetic towards others. She doesn’t have many intimate friends. She always kept a good relationship with her family. She was not much talkative in the family except with her mother. The predominant mood was happy. Moral standards, she is a religious person who keeps religious rituals always. Stress reaction, she was able to tolerate and deal effectively with stress. Habit, the sleep pattern was normal, and had no habit of doing exercises. Fantasy life, dream with the content of ‘falling into the water. Other personality traits, there is no presence of personality traits such as OCD, ADHD, ODD, emotionally unstable personality, impulsivity, and narcissistic personality
Mental status examination (MSE)
General appearance and behavior: The patient was alert, attentive, and conscious during the session. The patient’s dressing was appropriate. Eye contact was established and maintained. A good rapport was made. The patient’s attitude toward the examiner was cooperative. Reality contact was present. Tics/mannerisms and catatonic phenomena were absent.
Psychomotor activity: Increased psychomotor activity by walking during the session and drinking a lot of water.
Speech: The speech was relevant and coherent. Reaction time was normal. Volume and tone were normal and she maintained the prosody of speech.
Mood and affect: The mood were sad and her affect was shallow which was inappropriate to the situation and congruent to the thought content.
Thought: The patient doesn’t show any abnormalities in the stream, form, possession, and content of thought. That is., there is no presence of flight of ideas, circumstantiality, tangentiality, obsessions, compulsions, etc.
Perception: There is no presence of hallucinations and illusions. Other psychotic phenomena such as somatic passivity and made phenomena are absent. Other phenomena like depersonalization and derealization are also found to be absent.
Cognitive functions: Attention and concentration, the digit span test, and serial subtraction were given. In forward, the digit span is 4 and in backward the digit span is 3. In the serial subtraction test, the patient completed the task in 115 seconds. This shows that the patient’s attention was aroused and maintained. Orientation, the client was asked questions of time, place, and person, and found that the patient’s orientations were intact. Memory, the patient’s immediate memory was tested by conducting a recall test. The patient was able to recall what the examiner has said. The recent memory of the patient was tested by asking her questions regarding the past 24 hours and it is found that the patient’s recent memory was intact. Remote memory was tested by asking questions about personal details such as to say her date of birth. From this, it can be concluded that the patient’s memory was intact.
Intelligence: General information, the patient was asked questions for testing general knowledge. The responses of the patient indicate that general information is adequate. Comprehension, the patient’s comprehension is assessed by asking some situational questions and is found adequate. Arithmetic ability, after comprehension, the arithmetic ability of the patient is assessed by asking some simple arithmetic questions and is found adequate. Abstract ability, the patient’s abstract ability is assessed by giving tests to find similarities and dissimilarities of objects the examiner is saying. Proverbs are given to the patient and asked to explain them. The assessments of general information, comprehension, arithmetic ability, and abstract ability indicate that the patient has an average intellectual capacity.
Judgment: The patient's personal, social, and test judgment is found to be intact.
Insight: The patient has a level five insight. Since she is accepting all her minor and major symptoms and is also aware of the need for treatment.
Provisional diagnosis: F31.1 (ICD-10 CLASSIFICATION) Bipolar affective disorder, current episode manic without psychotic symptoms.
Diagnostic guidelines: For a definite diagnosis
- The present episode has to meet the requirements for mania without psychotic symptoms. and
- There must have been at least one prior affective episode in the past, whether it was mixed, hypomanic, manic, or depressed.
Diagnostic criteria for mania: The episode must last at least a week and be severe enough to substantially interfere with daily tasks and social interactions. Energy levels should rise along with a few of the symptoms listed below when the mood changes.
- Decreased need for sleep
- Grandiosity
- Excessive optimism
- Particularly pressure of speech
The patient has had such emotional episodes in the past and has recently had greater energy, decreased sleepiness, and excessive optimism. Given that this fits the aforementioned requirements, we can provisory classify the patient's present manic episode as having bipolar affective disorder.
Interventions And Management Plan:
A medical doctor or trained clinical psychologist determines an intervention and management plan for any mental disturbance. Since Bipolar affective disorder is a long-term condition, continuous and prolonged treatment is needed. Professionals suggest several management strategies for bipolar affective disorder treatment. This often includes:
Hospitalization- Doctors often prefer hospitalization if the patient seems to be more dangerous and has suicidal ideas. Psychiatric hospital care helps stabilize the patient’s mood, and, maintains a safe and calm atmosphere.
Medications - Several medications are used in treating bipolar disorders. Taking medication helps balance your moods in the right way. The types and doses of medicines are determined by the doctor. Commonly prescribed medications in the treatment of bipolar affective disorder include:
- Mood stabilizers- This includes lithium, valproic acid, equator, etc.
- Antipsychotics- Olanzapine, risperidone, aripiprazole. This comprises commonly prescribed antipsychotics.
- Antidepressants- Antidepressants are given to manage depression. But these are prescribed along with mood stabilizers or antipsychotics since antidepressants trigger mania.
- Anti-anxiety medications- This has benzodiazepine in it. This provides better sleep and also helps with dealing with anxiety.
Psychotherapy- bipolar disorder treatment includes psychotherapy on a regular basis. Numerous therapies may be beneficial. A family, a group, or an individual may get therapy.
Treatments provided include:
- Cognitive Behaviour Therapy (CBT)- The goal of this treatment is to discover unhealthy ideas and behaviors and replace them with constructive ones.
- Psychoeducation- Learning about bipolar illness can help patients better comprehend their current situation, prevent relapses, and adhere to therapy.
- Family-focused therapy- Family therapy helps make the family of the patient aware of the disorder and warning signs of bipolar episodes.
If the patient doesn't improve with antidepressants, further therapeutic options include electroconvulsive therapy (ECT) and occasionally transcranial magnetic stimulation.
This study discusses a case of bipolar affective disorder, current episode manic without psychotic symptoms. Here the study concentrates on the characteristics, symptoms and features of bipolar affective disorder, current episode manic without psychotic symptoms and also the interventions used for this case. For those who suffer from bipolar affective disorder, the present episode is manic without psychotic symptoms, and the patient has previously had at least one prior affective episode (hypomanic, manic, depressed, or mixed). (ICD 10) Mania is defined by an elevated mood that is out of proportion to the patient's circumstances and can vary from casual merriment to almost uncontrollable excitement. Mania is characterized by the absence of psychotic symptoms. Overactivity, difficulty speaking, and a diminished need for sleep are all symptoms of the increased energy that comes with joy. Continuous concentration is lacking, and distractions are usually evident. An exaggerated feeling of self-worth can result from overconfidence and ambitious ambitions. Losing one's normal social inhibitions might cause one to act carelessly, foolishly, or inappropriately given the circumstances.
Limitations:
The study adopted a single case study method, the result cannot be generalized to larger populations.
Declarations:
This article's completion was not supported by any money.
Conflicts of interest/Competing interests
The authors have no financial or non-financial interests to report.
Data Availability Statement
Only datasets produced during and/or analyzed during the current investigation are available upon reasonable request from the corresponding author.
Authors' contributions
the two writers have each made a meaningful contribution and agree that they should both be given authorship credit.
Ethics approval
The Departmental Research Committee granted ethical approval.
Consent to participate
Informed consent was taken from the informant and also from the institution
Consent for publication
All authors of this research Study consent to the work being used for publication.
Acknowledgments
The article, A case study on bipolar affective disorder, current episode without psychotic symptoms (ICD F 31.1), is a record of original research effort, we therefore declare. We attest to the work's originality and the absence of any instances of plagiarism across the whole manuscript.
- Abad, V. C., & Guilleminault, C. (2005). Sleep and psychiatry. Dialogues in Clinical Neuroscience, 7(4), 291–303. View at Publisher | View at Google Scholar
- Ahuja, N. (2017b). A short textbook of psychiatry. Jaypee publications. View at Publisher | View at Google Scholar
- Akdemir, D., &Gokler, B. (2008). Psychopathology in the children of parents with a bipolar mood disorder, Article 18561045. View at Publisher | View at Google Scholar
- Baartmans, J. M. D., van Steensel, F. J. A., Klein, A. M., & Bögels, S. M. (2022). The Role of Comorbid Mood Disorders in Cognitive Behavioral Therapy for Childhood Social Anxiety. Cognitive Therapy and Research, 46(5), 983–991. View at Publisher | View at Google Scholar
- (2021). Bipolar disorder - Diagnosis and treatment - Mayo Clinic. View at Publisher | View at Google Scholar
- Claudio, A., & Andrea, F. (2022). Circadian neuro markers of mood disorders. Journal of Affective Disorders Reports, 10, 100384. View at Publisher | View at Google Scholar
- Datta, S., Suryadevara, U., & Cheong, J. (2021). Mood Disorders. CONTINUUM: Lifelong Learning in Neurology, 27(6), 1712–1737. View at Publisher | View at Google Scholar
- Deepika, K. (2019). case report on bipolar affective disorder: Mania with psychotic symptoms. Pondicherry Journal of Nursing. 12(02);51. View at Publisher | View at Google Scholar
- Hooley, J. M., Butcher, J. N., Nock, M. K., & Mineka, S. M. (2016). Abnormal Psychology (17th Edition) (17th ed.). Pearson. View at Publisher | View at Google Scholar
- McCombes, S. (2022). What Is a Case Study? | Definition, Examples & Methods. Scribbr. View at Publisher | View at Google Scholar
- Pacchiarotti, I., Anmella, G., Colomer, L., & Vieta, E. (2020). How to treat mania. Acta Psychiatrica Scandinavica, 142(3), 173–192. View at Publisher | View at Google Scholar
- Pinto, J. V., Ziak, M. L., Schaffer, A., & Yatham, L. N. (2022). Cannabidiol in the Treatment of Mood Disorders. Current Treatment Options in Psychiatry, 9(3), 140–150. View at Publisher | View at Google Scholar
- Rashid, M. H., Ahmed, A. U., & Khan, M. Z. R. (2019). Substance Abuse among Bipolar Mood Disorder Patients. Delta Medical College Journal, 7(1), 31–34. View at Publisher | View at Google Scholar
- Sadock, B. J., Sadock, V. A., & Md, R. P. (2014). Kaplan and Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry (Eleventh). LWW. View at Publisher | View at Google Scholar
- Shah, K., Trivedi, C., Kamrai, D., Srinivas, S., & Mansuri, Z. (2022). Suicide in Adolescents with Mood Disorders. European Psychiatry, 65(S1), S141–S141. View at Publisher | View at Google Scholar
- (2022). 6 Types of Case Study - Definition and Examples. (n.d.). View at Publisher | View at Google Scholar
- World Health Organization. (1992). The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. View at Publisher | View at Google Scholar
- (2022). What is an Exploratory Case Study? View at Publisher | View at Google Scholar
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Virginia E. Koenig
Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Delcio G Silva Junior
Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Ziemlé Clément Méda
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

Mina Sherif Soliman Georgy
We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

Layla Shojaie
The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Sing-yung Wu
Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Orlando Villarreal
Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.

Katarzyna Byczkowska
Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Anthony Kodzo-Grey Venyo
Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Pedro Marques Gomes
Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.


Bernard Terkimbi Utoo
This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Prof Sherif W Mansour
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dr Shiming Tang
Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

Raed Mualem
International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Andreas Filippaios
Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dr Suramya Dhamija
Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

Bruno Chauffert
I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!

Baheci Selen
"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

Jesus Simal-Gandara
I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

Douglas Miyazaki
We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

Dr Griffith
I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

Dr Tong Ming Liu
I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

Husain Taha Radhi
I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

Tania Munoz
“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.

George Varvatsoulias
Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.

Our Collaborations
Lorem ipsum dolor sit amet, consectetur adipisicing elit. Culpa, repudiandae, suscipit repellat minus molestiae ea.

ORIGINAL RESEARCH article
Significant improvements in the olfactory sensitivity of bipolar i disorder patients during euthymia versus manic episodes: a longitudinal study.

- Department of Psychiatry, Shunde WuZhongpei Memorial Hospital, Foshan, Guangdong, China
Introduction: Research has indicated that individuals diagnosed with bipolar disorder (BD) might experience alterations in their olfaction or levels of serum tumor necrosis factor-α (TNF-α), but no studies have investigated olfactory function and serum TNF-α in BD patients simultaneously. Moreover, there is a lack of existing research that compares the longitudinal olfactory function between individuals with manic and euthymic BD I.
Methods: Patients with manic BD I (BDM, n=44) and healthy controls (HCs, n=32) were evaluated symptoms (measured via the Young Manic Rating Scale, YRMS), social function (measured via the Global Assessment Function, GAF), serum TNF-α, and olfactory function (via the Sniffin’ Sticks test) including olfactory sensitivity (OS) and olfactory identification (OI). The BDM patients were followed up to the remission period and re-evaluated again. We compared OS, OI and serum TNF-α in manic and euthymic patients with BD I and HCs. We examined the correlation between olfactory function and symptoms, social function, and serum TNF-α in patients with BD I.
Results: The BDM patients exhibited significantly lower OS and OI compared to the HCs (Z = −2.235, P = 0.025; t = −6.005, P < 0.001), while a positive correlation was observed between OS and GAF score (r = 0.313, P = 0.039). The OS in the BD I remission group (n=25) exhibited significantly superior performance compared to the BDM group (t = −4.056, P < 0.001), and the same as that in the HCs (P = 0.503). The change in OS showed a positive correlation with the decrease in YMRS score (r = 0.445, P = 0.026), and a negative correlation with the course of disease (r = -0.594, P = 0.002). The TNF-α in BD I patients was significantly lower compared to HCs (P < 0.001), and not significantly correlated with olfactory function (all P > 0.05).
Conclusion: The findings suggest that OS and OI are impaired in BDM patients, and the impaired OS in those patients can be recovered in the remission stage. OI may serve as a potential characteristic marker of BD. OS might be useful as an index for BDM treatment efficacy and prognosis.
1 Introduction
Bipolar disorder (BD) is primarily characterized by the occurrence of recurring and alternating episodes of mania or hypomania, as well as depression. According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) , BD can be classified as bipolar I disorder (BD I) and bipolar II disorder (BD II). Compared with patients with BD II, who experience hypomania and depression, patients with BD I also experience manic episodes ( 1 ). However, there are no specific biological markers to inform psychiatric diagnoses of BD. Instead, the diagnostic criteria are defined by clinical history and psychiatric examination, so individuals with BD are often misdiagnosed with other conditions. Individuals with different mental disorders, and even different subtypes of BD, often need to be treated differently. For instance, the improper administration of antidepressant treatments to patients with depressive BD can induce mania ( 2 ). Therefore, identifying the biomarkers of BD holds significant importance in enhancing the precision and effectiveness of individual diagnosis and treatment approaches within the realm of clinical psychiatry.
Numerous research studies have provided evidence supporting the close association between emotion and the limbic system, comprising of the cingulate cortex, hippocampus, amygdala, and orbitofrontal cortex ( 3 ). Functional and anatomical irregularities within the limbic system have been detected through imaging examinations in individuals diagnosed with bipolar disorder ( 4 – 7 ). The limbic system also plays an important role in olfactory processing and the piriform cortex provides projections to the amygdala, hippocampus, and orbitofrontal cortex, serving as a crucial secondary olfactory region ( 8 , 9 ). Accordingly, scholars have suggested that olfactory function might be implicated in BD ( 10 , 11 ). Imaging studies exhibit noticeably reduced depth in their bilateral olfactory sulci compared to the healthy people ( 12 ). Sancaktar et al. ( 13 ) reported that compared with that in healthy controls (HCs), glucose metabolism in the olfactory bulb and amygdala was more active in patients with euthymic BD. This supports the hypothesis that emotional processing is primarily influenced by the olfactory bulb, and indicates that the olfactory bulb and amygdala are closely related to the pathogenesis of BD.
There is limited knowledge regarding the olfactory function in individuals diagnosed with BD, as the available information is scarce and inconsistent. Thus, the controversy surrounding the potential use of olfactory disorder as a biological marker for BD remains unresolved ( 14 ). Li et al. ( 15 ) reported that olfactory sensitivity (OS) in patients with BD was impaired only during the acute phase, and there was a negative association between OS impairment and the severity of clinical symptoms. In contrast, olfactory identification (OI) was impaired in patients in both the acute and euthymic phases of BD, so Li et al. proposed that OS might be a state indicator for BD, while OI could serve as a trait indicator of BD. However, Kazour et al. ( 16 ) carried out a cross-sectional study involving 33 patients with depressive BD, 30 patients with euthymic BD after depression, and 49 HCs. The results of their study indicated that there were no significant differences in the OS and OI between patients with depressive BD or euthymic BD, and HCs.
Inflammation is hypothesized to be a potential pathophysiological mechanism underlying BD ( 17 ), with cytokines playing a significant role in this process ( 18 ). As one of the pro-inflammatory cytokines, tumor necrosis factor-α (TNF-α) is generally associated with killing and inhibiting the activity of tumor cells. It also induces the production of other cytokines ( 19 , 20 ). These cytokines, including TNF-α, are considered to be important factors related to the pathogenesis of BD, and may be appropriate targets for BD treatment ( 21 ). There is evidence that the pathophysiological mechanism underlying BD is associated with the modulation of neural plasticity and apoptosis, and that cytokines like TNF-α exert a significant influence on the pathogenesis of BD by influencing these processes ( 22 ).
Studies have indicated an elevation in peripheral blood TNF-α among BD patients. Van den Ameele et al. ( 23 ) revealed that in individuals diagnosed with BD, plasma TNF-α was increased in the acute phase and decreased in remission stage, such that it was consistent with that of HCs. Studies conducted by Munkholm et al. ( 24 ) and Modabbernia et al. ( 25 ) also reported a significant elevation in the concentration of TNF-α among BD patients when compared to HCs. However, a few studies suggested that TNF-α among BD patients did not increase ( 19 , 20 ) or even decrease ( 26 ) in the acute phase.
In recent years, scholars have attempted to identify biomarkers to assist in the diagnosis of BD. Many cytokines, including TNF-α, have received increasing attention from researchers. These studies have indicated that TNF-α could potentially serve as a valuable biomarker for assisting in the diagnosis of BD. Research have indicated that patients with BD may exhibit abnormal olfactory function. Although there are inconsistent results, olfactory impairment has the potential to be a biological marker of bipolar disorder. In view of the fact that the sensitivity and specificity of olfactory function or peripheral TNF-α are not high enough when used alone for early diagnosis or efficacy evaluation of BD. This study simultaneously observed the changes of these two indicators in the acute phase and remission phase of BDM patients, and accumulated clinical reference data for future exploration of the adjuvant effect of TNF-α combined with olfactory function in the diagnosis and treatment of BD. A review published in 2023 suggested that inflammation may be involved in the pathophysiological mechanism of olfactory dysfunction in some psychiatric disorders ( 27 ). It can be inferred that cytokines, including TNF-α, may be associated with olfactory function in psychiatric disorders. Given that both impaired olfactory function and elevated peripheral TNF-α in BD may occur during the acute stage, but neither may show abnormal changes during the remission stage. It can be hypothesized that the pathophysiological mechanisms underlying these two phenomena are related to each other, resulting in the changes of olfactory function and peripheral TNF-α levels in BD patients.
Although previous studies basically grouped BDM patients with depressive BD and euthymic BD patients, limited studies have specifically examined the olfactory function of BDM individuals alone. A study by Kazour et al. ( 28 ) appears to be the first report on olfactory function in patients with BDM, but it was a cross-sectional comparison of participants in different groups instead of a longitudinal comparison of patients in the same group.
In summary, few studies have investigated olfactory function in patients with BDM alone. Furthermore, no studies have compared olfactory function longitudinally between individuals with manic and euthymic BD I, or analyzed the relationship between serum TNF-α level and olfactory dysfunction among patients with BD. The objective of this study was to provide a new index to facilitate the early detection of BD I or to assess treatment outcomes, and to provide new clinical evidence regarding the pathophysiological mechanisms of BD.
We postulated that patients with manic BD I (BDM) may exhibit impaired olfactory function and elevated serum TNF-α, but that these changes would return to normal levels during the remission period. Furthermore, we hypothesized that there might be a potential association between olfactory function and serum TNF-α levels among these individuals.
2.1 Participants
The study involved individuals diagnosed with BDM who were hospitalized at Shunde WuZhongpei Memorial Hospital, Foshan City, Guangdong, China, from July 2022 to December 2022. The patients were followed up and evaluated during hospitalization or as outpatients when they were in the remission period. At the same time, HCs were recruited from the healthy hospital staff who had matched social and demographic characteristics as the case group. The patients in the BDM group were diagnosed with BDM according to the DSM-5 , had no other mental disorders, and received a Young Mania Rating Scale (YMRS) score ≥20 and a Hamilton Rating Scale for Depression (HAMD) score <12. The BD I remission (BDR) group were the same BDM patients, assessed during the follow-up period. They were re-evaluated when there had been no obvious clinical symptoms for at least one month, and received a YMRS score ≤7 and HAMD score ≤8. The HCs also had no mental illness, and had a YMRS score ≤7 and HAMD score ≤8.
All participants were of Chinese Han nationality, aged 18–60 years, and had attended primary school education or above. They had no history of head or neck trauma, nasal surgery, neurological diseases (epilepsy, stroke), intellectual disability, or any diseases that could impact olfactory function (like nasal polyps, common colds, or allergies). Individuals with a prior record of alcohol or substance abuse or dependence within the last year, as well as those unable to complete the olfactory examination or scale evaluation, were not included in the study.
The experimental flow and study steps are shown in Figure 1 .
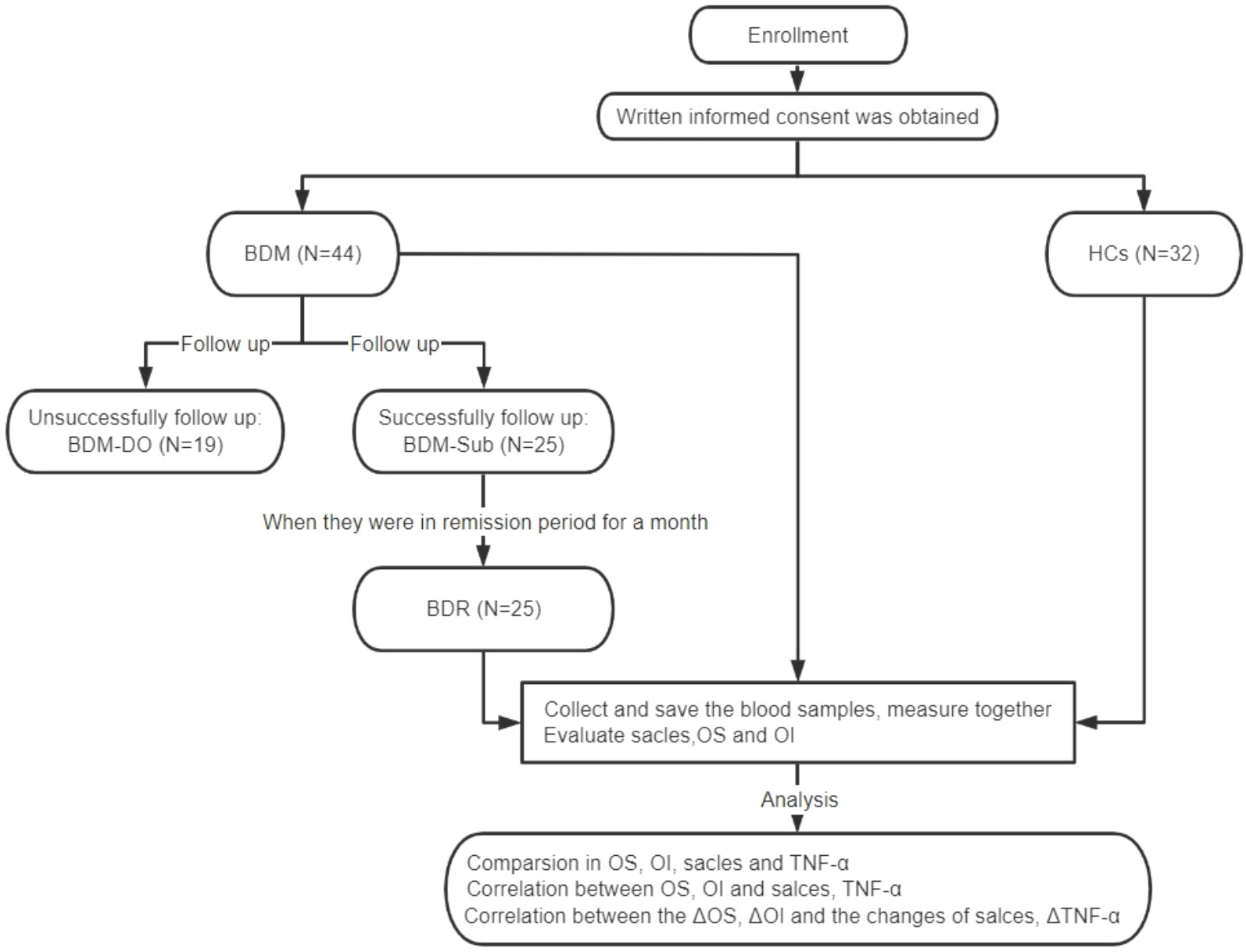
Figure 1 CONSORT diagram for assessments of olfactory function and serum TNF-α levels. BDM, patients with manic BD I; HCs, healthy controls; BDM-DO, patients with manic BD I who dropped out during the follow-up; BDM-Sub, sub group of BDM, patients with manic BD I who could be followed up to the remission period; BDR, patients with manic BD I who were followed up to the remission period; OS, olfactory sensitivity; OI, olfactory identification; TNF-α, tumor necrosis factor-α; ΔOS, change in olfactory sensitivity; ΔOI, change in olfactory identification; ΔTNF-α, change in tumor necrosis factor-α levels.
This study was approved by the Medical Ethics Committee of Shunde WuZhongpei Memorial Hospital, Foshan City, Guangdong, China, and conducted in accordance with the principles outlined in the Declaration of Helsinki. Participants or their family members were duly informed and consented in writing. Our study strictly adhered to the principle of voluntary participation, allowing participants to withdraw at any given time.
2.2 Measures
The YMRS: This is primarily employed for the assessment of manic symptoms; the score range is 0–60. Generally, YMRS scores of 0–5 suggest the absence of evident manic symptoms, scores ranging from 6 to 10 indicate the presence of manic symptoms, and score more than 22 indicates severe manic symptoms.
HMAD: This is one of the most frequently utilized scales employed to assess depression in clinical practice. In our study, we used the 24-item version of the HAMD (HAMD-24). A total HAMD-24 score >20 reflects mild or moderate depressive symptoms, while HAMD-24 <8 indicates no depressive symptoms.
Global Assessment Function (GAF): This is employed for the assessment of the psychological, social, and professional functions of the participants. GAF has only one statistic, that is, the total score (1–100 points). A higher score indicates a milder disease state. For each participant, we evaluated GAF, HAMD and YMRS in person, with two psychiatrists who were trained in the use of the scales as evaluators.
Sniffin’ Sticks test (SST): The SST serves as a tool for measuring quantitative olfactory abilities that can test OS and OI respectively. The OS test comprised a total of 16 n-butanol olfactory felt-tip pens and corresponding blank pens. The pen exhibited a 4% concentration of n-butanol, which was the highest among all the pens, and the other pens contained varying concentrations, corresponding to concentration levels 1–16, respectively. Before the OS test, the No. 1 n-butanol pen was given to the subject to familiarize them with the test odor. Each group was tested with one n-butanol olfactory pen and two blank pens. The determination of OS was achieved through the utilization of a single staircase method. The triplets were presented to the subject successively, until they accurately identified the scent in two consecutive trials, leading to a reversal of the staircase. The threshold estimate was determined by calculating the geometric mean of the last four points where reversals occurred out of a total of seven reversals. A higher OS score corresponded with greater OS. The OI examination comprised a collection of 16 distinct olfactory sticks. The participants were requested to recognize the 16 odors and choose the correct answer for each stick from four options provided. Each accurate response was recorded as 1 point, while an inaccurate response received no points. The cumulative score amounted to 16 points. A higher OI score corresponded with greater OI ( 29 ).
Serum TNF-α: The TNF-α ELISA kit (Shanghai Renjie Biotechnology Co., Ltd.) was used to detect sample concentrations via a double-antibody sandwich ELISA. A fasting venous blood sample of 5ml was collected from the subjects in the morning and centrifuged after natural coagulation at room temperature. The centrifugation process lasted approximately 20 minutes at a speed of 2000-3000 revolutions per minute. Carefully collect the supernatant and store it in the refrigerator at -40°C for measurement. Two dedicated technicians belonging to our team members carried out the experiment in the laboratory of Shunde WuZhongpei Memorial Hospital, Foshan City, Guangdong, China, according to the manufacturer’s instructions of the TNF-α ELISA kit.
2.3 Statistics
SPSS 25.0 software (SPSS Inc, Chicago, IL, USA) was utilized for conducting statistical analyses. The number of cases and constituent ratios were used to present the qualitative data, while the chi-square test was employed for analysis. The normality of the quantitative data was tested, and the measurement data that followed a normal distribution are presented as the mean ± standard deviation. Otherwise, they are shown as the median values (25th percentile, 75th percentile) [M (P 25 , P 75 )]. Considering the sample size of our study, we used the Shapiro-Wilk test to determine normality. A comparison between the two groups of data with a normal distribution was conducted using either an independent sample t-test or paired sample t-test. For non-normally distributed data, the comparison was performed using either the Mann-Whitney U test or Wilcoxon signed rank sum test. The relationships were analyzed via Pearson’s correlation or Spearman’s correlation. The significance level for the tests was set at α = 0.05, and both two-tailed tests were performed.
3.1 Comparison between the BDM and HC groups
A total of 44 patients with BDM and 32 HCs were included in the study. There was no notable distinctions in age, gender, smoking habits, or education background between the two groups (all P > 0.05). The OS and OI in the two groups were compared via the Mann-Whitney U test and independent sample t-test respectively, and we found significant differences in both OS and OI between the two groups (Z = −2.235, P = 0.025 and t = −6.005, P < 0.001, respectively). As shown in Table 1 , which includes a box chart showing the OS and OI, the BDM group exhibited poorer performance in both the OS and OI compared to the HCs (see Figures 2A, B ). We observed a significant difference in serum TNF-α levels between the two groups (Z = −4.650, P < 0.001), suggesting that the BDM group exhibited reduced serum TNF- α compared to the HCs.
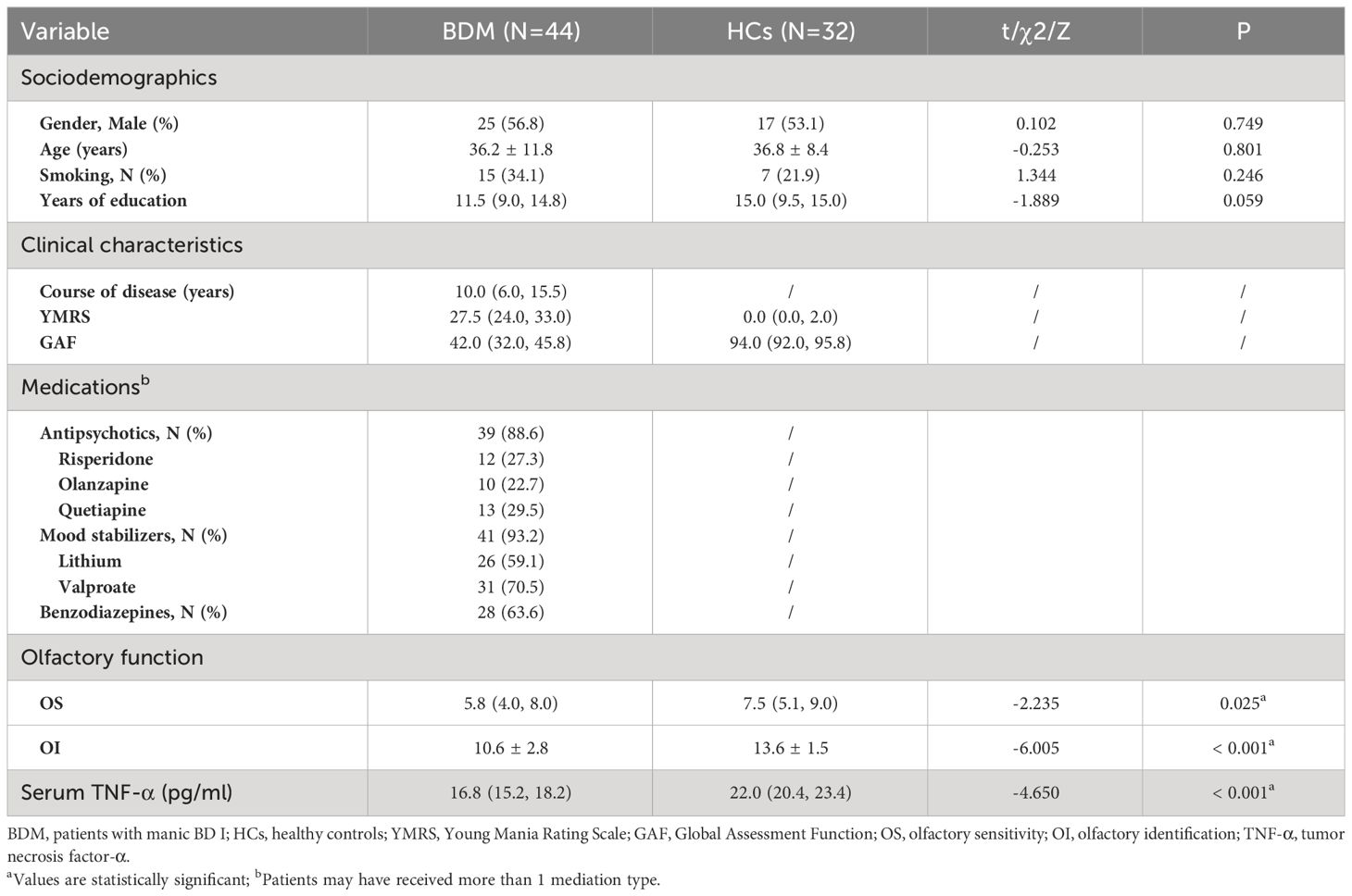
Table 1 Sociodemographics, clinical characteristics, olfactory function, and TNF-α levels in individuals with BDM and HCs.
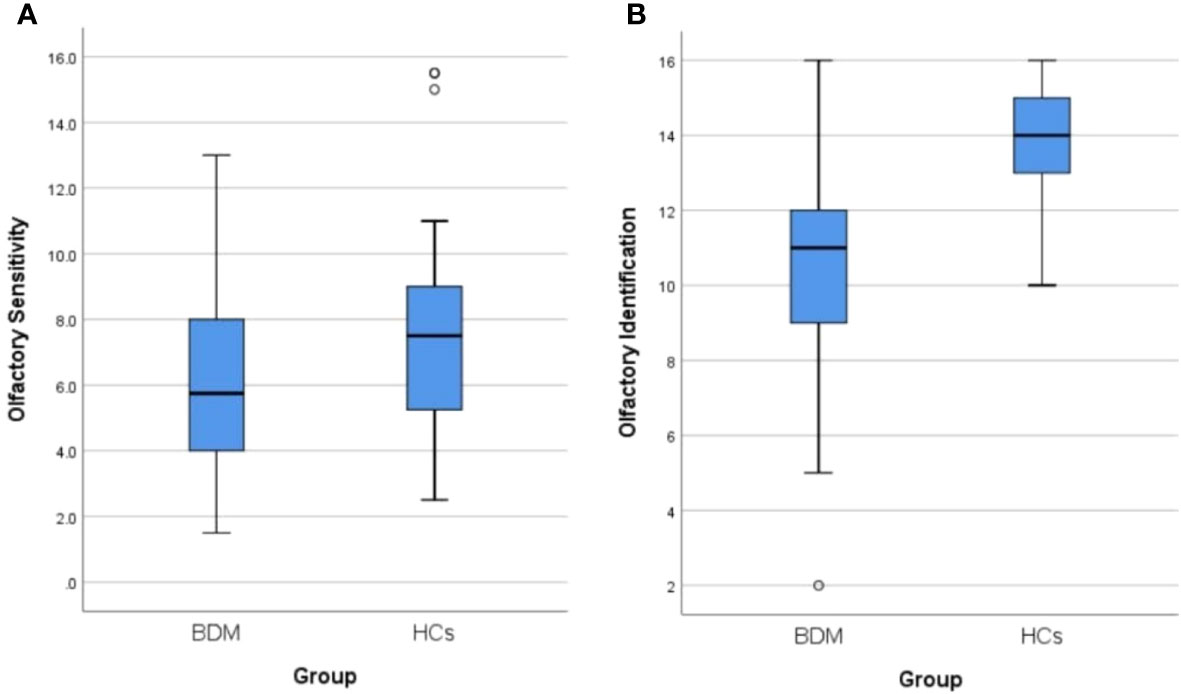
Figure 2 (A) Comparison of olfactory sensitivity between BDM and HCs. (B) Comparison of olfactory identification between BDM and HCs. BDM, patients with manic BD I; HCs, healthy controls.
3.2 Comparison between the euthymic BD and HC groups
The BD symptoms, olfactory function, and TNF-α were followed up in the BDM group. At the end of the study in December 2022, a total of 25 patients were in remission and had successfully completed the follow-up. The follow-up completion rate was 56.82% (before completion of the follow-up, the subgroup was called the “BDM subgroup (BDM-sub)”; after completion of the follow-up, the group was called the “BD I remission group (BDR)”). There were no notable disparities in age, gender, smoking habits, or education background between these 25 patients and the 32 HCs (all P > 0.05). In the BDR patients, the OI was worse than that in the HCs (Z = −4.039, P < 0.001), but there were no notable disparities in OS between the two groups (Z = −0.669, P = 0.503). Serum TNF-α levels in the BDR patients were found to be significantly decreased compared to those observed in the HCs (Z = −4.535, P < 0.001). See Table 2 .
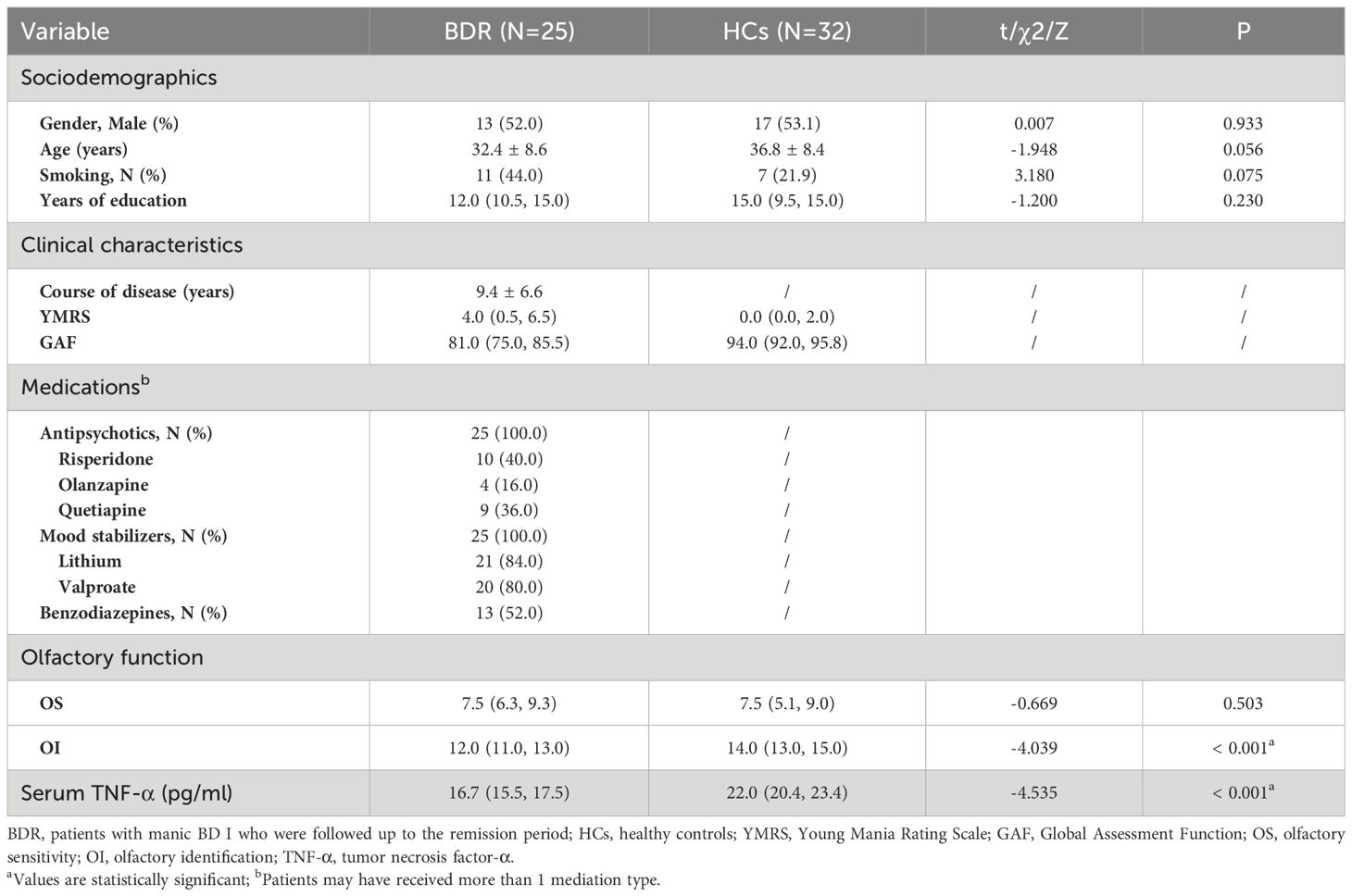
Table 2 Sociodemographics, clinical characteristics, olfactory function, and TNF-α levels in BDR patients and HCs.
3.3 Comparison between the BDM and euthymic BD groups
3.3.1 comparison between the bdm subgroup and the bdm drop-out subgroup.
There were 19 patients who failed to complete the follow-up assessment at the end of the study (called the “BDM drop-out subgroup (BDM-DO)”), of which 5 patients were still in the manic state at the end of the follow-up period. Another 14 patients were discharged after hospitalization, but they were not evaluated again after discharge because of personal reasons. There were significant differences in age, YMRS score, GAF score, and medication type between the two subgroups, but no significant differences in the other items (P > 0.05). This suggests that clinical symptoms and impaired social function in the BDM-DO may have been more serious than those in BDM-sub, which may be related to the fact that some patients in the BDM-DO did not achieve remission at the follow-up endpoint. Although there were differences in age, clinical symptoms, and social function between the BDM-sub and BDM-DO, there were no disparities in gender, smoking, education, or course of disease, and there were no disparities in OS, OI, or serum TNF-α at the time of inclusion between the two subgroups. See Table 3 .
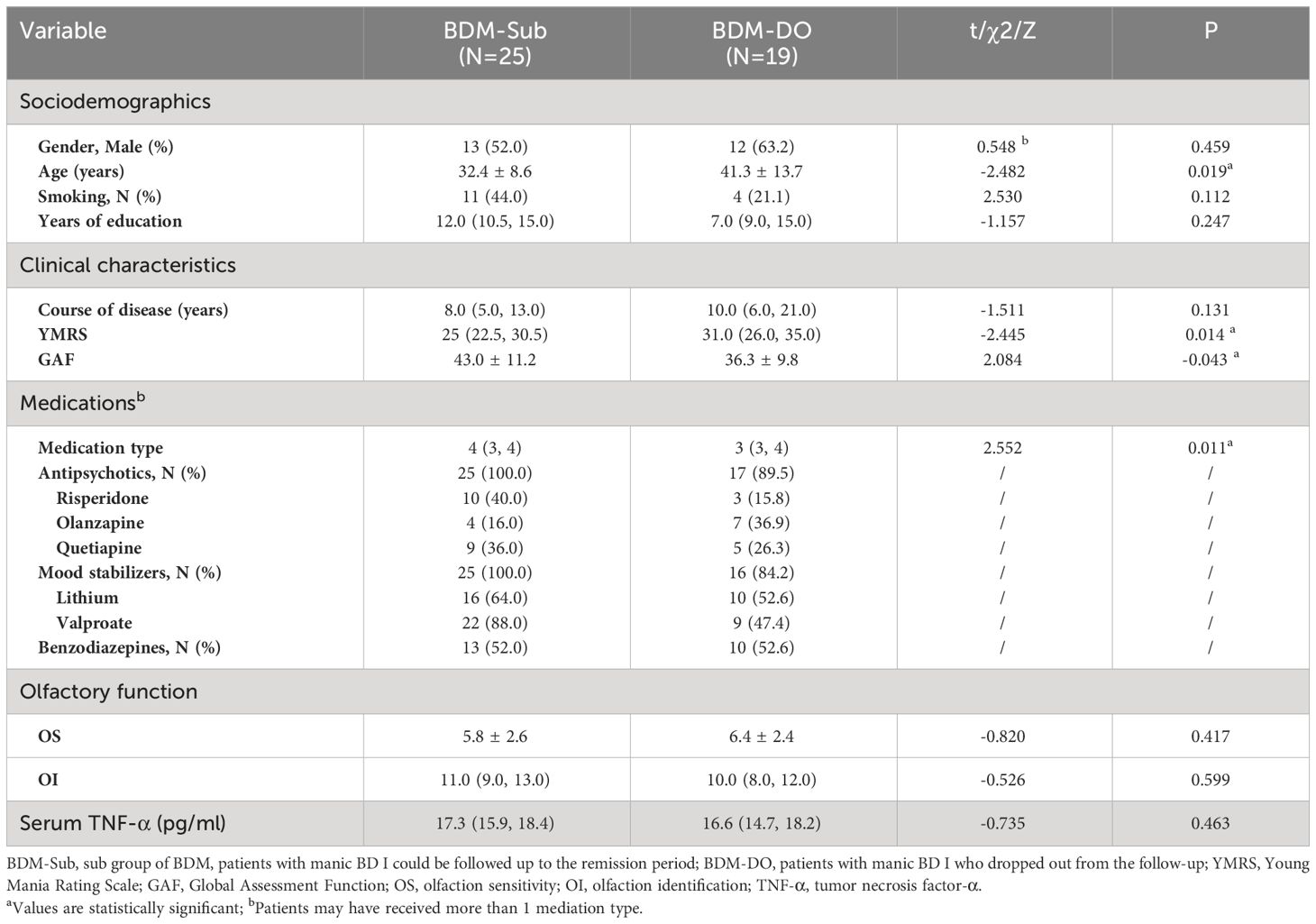
Table 3 Sociodemographics, clinical characteristics, medications, olfactory function, and TNF-α levels in the BDM-Sub versus BDM-DO.
3.3.2 Changes in olfactory function and TNF-α in the BDM subgroup versus euthymic BD group
According to a paired sample t-test, the impaired OS in patients with BDM-sub was significantly improved during remission (t = −4.056, P < 0.001). However, there was no notable disparities in OI or serum TNF-α between the two groups, as determined by the Wilcoxon symbolic rank sum test. See Table 4 .
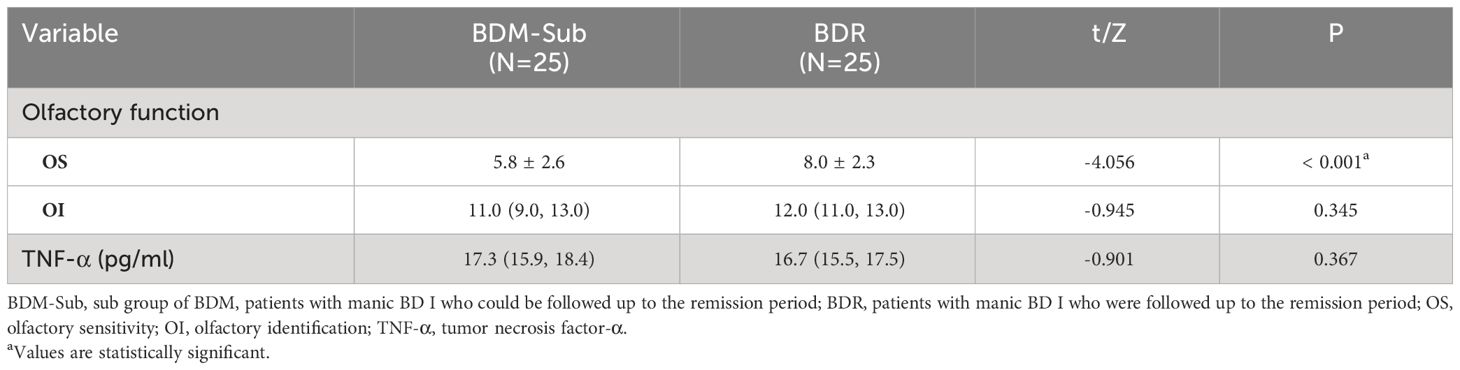
Table 4 Olfactory function and TNF-α levels in the BDM-Sub and BDR groups.
3.4 Correlation analysis in the BDM and euthymic BD groups
The correlation analysis (Pearson/Spearman) between the OS or OI and age, course of disease, years of education, YMRS score, GAF score, and serum TNF-α in the BDM group showed a positive correlation between the OS and GAF score in the BDM group (r = 0.313, P = 0.039). Furthermore, the analysis of Pearson’s correlation revealed a positive association between OS and OI in the BDM group (r = 0.380, P = 0.011), indicating that the OS and OI were impaired synchronously in patients with BDM. However, there was no significant correlation found between age, course of disease, years of education, YMRS score, GAF score, or TNF-α levels with either the OS or OI in the BDR group (all P > 0.05).
Correlations (Pearson/Spearman) were analyzed respectively between the changes in OS or OI (ΔOS or ΔOI, respectively) in BDR patients and other indexes, including age, course of disease, years of education, decrease in YMRS score (ΔYMRS, reflecting the recovery of manic symptoms), change in GAF score (ΔGAF, reflecting the recovery of manic symptoms), and change in TNF-α levels (ΔTNF-α). The results showed that ΔOS in BDR patients was negatively correlated with the course of the disease (r = -0.594, P = 0.002) and positively correlated with the decrease in YMRS score (r = 0.445, P = 0.026). See Table 5 .
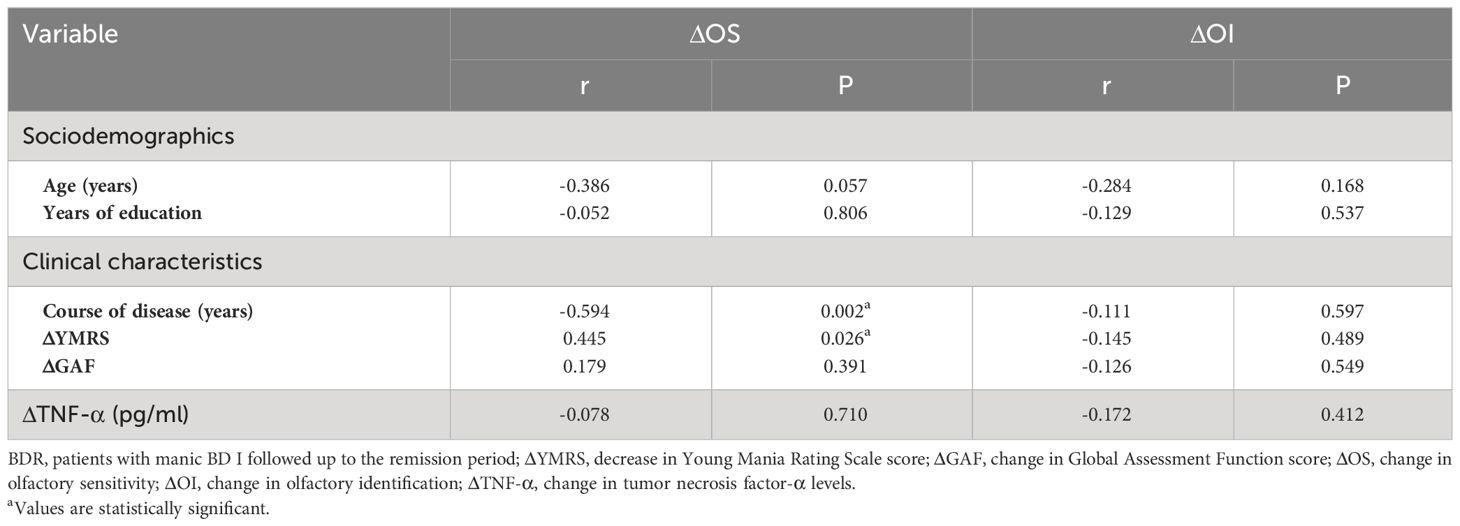
Table 5 Relationships between change in olfactory function and other indexes in BDR patients.
4 Discussion
4.1 olfactory sensitivity.
In this study, we observed that the OS of BDM individuals was significantly lower compared to that of the HCs, and that impaired OS could be recovered in the remission phase. No notable distinction was observed between individuals with euthymic BD and HCs. With regard to OS, the results of Kazour et al. ( 28 ) and Li et al. ( 15 ) were not consistent. Li et al. ( 15 ) revealed that the OS in patients with BDM was comparatively reduced compared to the HCs, which is aligning with our study. Kazour et al. ( 28 ) showed that the OS in patients with BDM was comparable to that of HCs, which contradicts the findings of our own research. A potential explanation could be the disparity in gender distribution within the patient group: in Kazour ’ s study, there were fewer men (44.4%), while in Li ’ s study and our study, the proportion of men with bipolar mania was higher, 58.6% and 56.8%, respectively. Kamath et al. ( 30 ) pointed out that in a test of OS in patients with acute mood disorder, olfactory function may be different in patients with acute mood disorder because of gender-bcased differences.
Li et al. ( 15 ) and Kazour et al. ( 16 , 28 ) similarly reported that there was no significant disparity in OS among euthymic BD patients compared to HCs. The results of our study align well with these previous investigations. In addition, Hardy et al. ( 10 ) found that there was no obvious difference in OS between 20 patients with stable BD and 44 HCs, which seems to support the results of this study. However, the result of Hardy’s study should be interpreted carefully because of different definitions and criteria for the stable condition or remission among different studies. In addition to the potential influence of gender differences, Kazour et al. ( 28 ) pointed out in the summary of their report that the results of longitudinal studies on olfactory function in the same group of patients should be more accurate than that of cross-sectional studies.
4.2 Olfactory identification
In our study, OI was obviously impaired in BDM patients when compared to that observed in HCs, and this impairment was present in euthymic patients. Kazour et al. ( 28 ) and Li et al. ( 15 ) revealed that OI was impaired in patients with BDM, which is in line with our findings.
During the remission stage, Lahera et al. ( 11 ) found that 39 individuals with euthymic BD had impaired OI compared with HCs. The results reported by Kazour et al. ( 28 ) and Li et al. ( 15 ) are similar to those of Lahera et al., and all are consistent with the results of the current study. Furthermore, a research conducted by Kazour et al. ( 16 ) demonstrated that 33 patients with euthymic BD had poorer OI for pleasant odors compared with HCs, although no overall impairment in OI was found when comparing these patients with 49 HCs. Kamath et al. ( 31 ) conducted a study that included 43 BD I patients (of which 13 with psychotic symptoms) and 72 HCs, and showed that BD I patients had impaired OI in comparison to HCs. Although their study did not specify the disease status of their patients, the results were consistent with our study.
4.3 Correlation between olfactory function and various indexes (except TNF-α)
We examined the association between olfactory function, manic symptoms, and social function among BDM patients, and discovered a positive correlation between OS and social function. A lower OS was associated with poorer social function. A change in OS demonstrated a positive association with a reduction in YMRS score (reflecting the improvement in manic symptoms) and exhibited a negative association with the course of disease, indicating that the better the recovery of manic symptoms, the better the recovery of impaired OS, and the longer the course of disease, the worse the recovery of impaired OS.
Hardy et al. ( 10 ) reported a positive association between the OS with social function in BD patients, which was in accordance with the findings of this study. Furthermore, the occurrence of anosmia was found to have an adverse effect on patient daily life, social relationships, and the ability to work ( 32 ). Although we did not observed significant association between OI and social function among BD patients in this investigation, Cumming et al. ( 33 ) previously reported that OI and social function were correlated in this patient group. This discrepancy may be related to the use of different tools in different studies. To evaluate social function, Cumming et al. used the Zigler Social Competence Scale, which considers education background, professional standing, work experience, and marital situation. In our study, we used the GAF to assess social function with a single subjective score, which may be less accurate.
As for the relationship between OS and manic symptoms, Hardy et al. ( 10 ) found that these variables were correlated, such that increased severity of manic symptoms was associated with decreased OS. Li et al. ( 15 ) also reported a negative association between the YMRS score and OS in patients with BD. The above results are similar to those of our study. Although we failed to establish a correlation between OS and manic symptoms during BDM or euthymic BD, we found that the degree of OS recovery after BDM remission was positively correlated with the degree of manic symptom recovery (the reduction in YMRS score). Future studies should expand the sample size to further clarify the correlation between olfactory dysfunction and manic symptoms in patients with BD.
In addition, we found that the recovery of OS after remission in patients with BDM exhibited a negative correlation with the course of the disease. A possible explanation is that most patients with BD have a chronic course of disease and tend to have recurrent episodes ( 34 ). The chronic nature of the disease leads to increased structural and functional abnormalities within the brain areas shared by BD and olfaction (e.g., orbitofrontal cortex and hippocampus), slowing the OS recovery process.
4.4 Relationship between TNF-α and olfactory function
In this study, it was observed that the levels of serum TNF-α were comparatively reduced in BD patients when compared to those in HCs during both the manic phase and the subsequent remission stage. Most prior investigations have indicated that peripheral TNF-α among BD patients is either elevated or comparable to those observed in HCs. Luo et al. ( 35 ) and Solmi et al. ( 36 ) found that the serum TNF-α levels were markedly elevated in individuals with BD during the acute phase compared to those in HCs. The latter study also revealed that there was no statistically significant difference in the TNF-α level between patients with euthymic BD and HCs. Studies of peripheral TNF-α have also shown elevated levels in BD I patients. Wang et al. ( 37 ) and Chen et al. ( 38 ) respectively observed that serum TNF-α among patients with BD I was significantly higher than that in HCs.
Pantović-Stefanović et al. ( 26 ) carried out a longitudinal follow-up study involving 83 patients with acute BD I, and showed that the levels of serum TNF-α in the patients who successfully achieved remission after 10 weeks of treatment were significantly lower compared to those of HCs in both the acute phase and remission stage. The findings of the present study are in line with these results, which may be attributed to the inherent characteristics of TNF-α. The pro-inflammatory cytokine TNF-α is implicated in the initial inflammatory process of BD, while also exhibiting anti-inflammatory properties and contributing to the subsequent anti-inflammatory response ( 39 ). Figiel ( 40 ) pointed out that TNF-α might have a protective effect on the brain. Therefore, the observed decrease in TNF-α levels among BD patients in current study might be explained by the relationship between the decline in TNF-α levels and the chronic course of BD. Although our study did not discover any association between serum TNF-α levels and the course of disease among BD patients in our study, Pantović-Stefanović et al. ( 26 ) observed a negative correlation between untreated course of disease and serum TNF-α levels in BD patients.
We observed olfactory dysfunction in patients with manic and euthymic BD, as well as reduced serum TNF-α levels, but no association between the olfactory dysfunction and serum TNF-α levels. At present, there is a lack of research indicating any connection between TNF-α and olfactory function in patients with BDM or euthymic BD. These two pathophysiological mechanisms of BD are relatively complex with many influencing factors, and may be independent from one another. Thus, it may not be possible to describe the relationship between them using a simple linear correlation.
5 Limitations
The study has several limitations that should be acknowledged. Firstly, the sample size was relatively small, and a large number of patients dropped out during the follow-up period. Secondly, the subjective nature of the olfactory function measurement method employed in this study could have potentially influenced the outcomes. In the future, we hope to combine objective olfactory detection methods. Thirdly, all the patients included in this study were under medication, which was not controlled. Thus, we could not exclude the influence of different therapeutic medications on olfactory function and serum TNF-α in patients with BD.
6 Conclusions
In patients with BDM, both OS and OI showed synchronous impairment when compared to those in the HCs, and OS was positively correlated with GAF score. Impaired OS in patients with BDM can be recovered in the remission stage, and the degree of recovery of OS exhibits a positive correlation with the degree of recovery of manic symptoms. We observed no statistically significant disparity in OS between patients with euthymic BD I and HCs, suggesting that OS could be a new marker for treatment efficacy and BDM prognosis. The OI in patients with BDM was still significantly impaired even when manic symptoms were recovered, suggesting that OI could potentially serve as a trait marker in bipolar manic patients. We observed no significant correlation between olfactory ability and peripheral TNF-α in BDM patients, suggesting that the pathophysiological mechanism of olfactory function and TNF-α in BD may be independent.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Ffurther inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Medical Ethics Committee of Shunde WuZhongpei Memorial Hospital, Foshan City, Guangdong, China. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
XL: Writing – original draft, Investigation, Formal analysis, Data curation, Methodology, Conceptualization. LS: Investigation, Data curation, Writing – original draft. YL: Investigation, Data curation, Writing – original draft. HY: Investigation, Data curation, Writing – original draft. AZ: Data curation, Writing – original draft. CY: Investigation, Data curation, Writing – original draft. CC: Writing – review & editing, Supervision. CL: Writing – review & editing, Supervision, Methodology, Conceptualization.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Medical Scientific Research Project of the Foshan Science and Technology Bureau (No.:1920001000420) and Shunde WuZhongpei Memorial Hospital (No.:202211), Foshan City, Guangdong, China.
Acknowledgments
We express our gratitude to Professor Laiquan Zou (affiliated with the Chemical Senses and Mental Health Lab, Department of Psychology, School of Public Health, Southern Medical University, Guangzhou, China) for his experimental guidance. This work was supported by the Clinical Departments of Shunde WuZhongpei Memorial Hospital, Foshan City. We also thank Sydney Koke, MFA, from Liwen Bianji (Edanz) ( www.liwenbianji.cn ) for editing a draft of this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Carvalho AF, Ropper AH, Firth J, Vieta E. Bipolar disorder. N Engl J Med . (2020) 383:58–66. doi: 10.1056/NEJMra1906193
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Chen CK, Wu LS, Huang MC, Kuo CJ, Cheng AT. Antidepressant treatment and manic switch in bipolar I disorder: A clinical and molecular genetic study. J personalized Med . (2022) 12. doi: 10.3390/jpm12040615
CrossRef Full Text | Google Scholar
3. Rolls ET. The cingulate cortex and limbic systems for emotion, action, and memory. Brain Struct Funct . (2019) 224:3001–18. doi: 10.1007/s00429-019-01945-2
4. Keener MT, Phillips ML. Neuroimaging in bipolar disorder: a critical review of current findings. Curr Psychiatry Rep . (2007) 9:512–20. doi: 10.1007/s11920-007-0070-2
5. Agarwal N, Port JD, Bazzocchi M, Renshaw PF. Update on the use of MR for assessment and diagnosis of psychiatric diseases. Radiology . (2010) 255:23–41. doi: 10.1148/radiol.09090339
6. Brambilla P, Hatch JP, Soares JC. Limbic changes identified by imaging in bipolar patients. Curr Psychiatry Rep . (2008) 10:505–9. doi: 10.1007/s11920-008-0080-8
7. Berk M, Malhi GS, Hallam K, Gama CS, Dodd S, Andreazza AC, et al. Early intervention in bipolar disorders: clinical, biochemical and neuroimaging imperatives. J Affect Disord . (2009) 114:1–13. doi: 10.1016/j.jad.2008.08.011
8. Kivity S, Ortega-Hernandez OD, Shoenfeld Y. Olfaction–a window to the mind. Isr Med Assoc J . (2009) 11:238–43.
PubMed Abstract | Google Scholar
9. Turetsky BI, Hahn CG, Borgmann-Winter K, Moberg PJ. Scents and nonsense: olfactory dysfunction in schizophrenia. Schizophr Bull . (2009) 35:1117–31. doi: 10.1093/schbul/sbp111
10. Hardy C, Rosedale M, Messinger JW, Kleinhaus K, Aujero N, Silva H, et al. Olfactory acuity is associated with mood and function in a pilot study of stable bipolar disorder patients. Bipolar Disord . (2012) 14:109–17. doi: 10.1111/j.1399-5618.2012.00986.x
11. Lahera G, Ruiz-Murugarren S, Fernandez-Liria A, Saiz-Ruiz J, Buck BE, Penn DL. Relationship between olfactory function and social cognition in euthymic bipolar patients. CNS Spectr . (2016) 21:53–9. doi: 10.1017/S1092852913000382
12. Takahashi T, Malhi GS, Nakamura Y, Suzuki M, Pantelis C. Olfactory sulcus morphology in established bipolar affective disorder. Psychiatry Res . (2014) 222:114–7. doi: 10.1016/j.pscychresns.2014.02.005
13. Sancaktar M, Kocamer Sahin S, Demir B, Elboga U, Elboga G, Altindag A. Is abnormal metabolism in the olfactory bulb and amygdala associated with bipolar disorder? J Neural Transm (Vienna) . (2023) 130:145–52. doi: 10.1007/s00702-023-02587-9
14. Henry C, Meyrel M, Bigot M, Alonso M, Lledo PM, Dargel AA. Can olfactory dysfunction be a marker of trait or states of bipolar disorders? A comprehensive review. J Affect Disord . (2020) 266:498–502. doi: 10.1016/j.jad.2020.01.081
15. Li SB, Li ZT, Lyu ZH, Zhang XY, Zou LQ. Odour identification impairment is a trait but not a disease-specific marker for bipolar disorders: Comparisons of bipolar disorder with different episodes, major depressive disorder and schizophrenia. Aust N Z J Psychiatry . (2022) 56:71–80. doi: 10.1177/0004867421998774
16. Kazour F, Richa S, Abi Char C, Surget A, Elhage W, Atanasova B. Olfactory markers for depression: Differences between bipolar and unipolar patients. PloS One . (2020) 15:e0237565. doi: 10.1371/journal.pone.0237565
17. Berk M, Kapczinski F, Andreazza AC, Dean OM, Giorlando F, Maes M, et al. Pathways underlying neuroprogression in bipolar disorder: focus on inflammation, oxidative stress and neurotrophic factors. Neurosci Biobehav Rev . (2011) 35:804–17. doi: 10.1016/j.neubiorev.2010.10.001
18. Wang AK, Miller BJ. Meta-analysis of cerebrospinal fluid cytokine and tryptophan catabolite alterations in psychiatric patients: comparisons between schizophrenia, bipolar disorder, and depression. Schizophr Bull . (2018) 44:75–83. doi: 10.1093/schbul/sbx035
19. Doganavsargil Baysal O, Erdogan A, Cinemre B, Akbas H, Sen Kaya S, Kus S. Levels of TNF alpha, Soluble TNF Receptors (sTNF-R1, sTNF-R2) in Bipolar Disorder. Noro Psikiyatr Ars . (2020) 57:136–40. doi: 10.29399/npa.24844
20. Jacoby AS, Munkholm K, Vinberg M, Pedersen BK, Kessing LV. Cytokines, brain-derived neurotrophic factor and C-reactive protein in bipolar I disorder - Results from a prospective study. J Affect Disord . (2016) 197:167–74. doi: 10.1016/j.jad.2016.03.040
21. Pereira AC, Oliveira J, Silva S, Madeira N, Pereira CMF, Cruz MT. Inflammation in Bipolar Disorder (BD): Identification of new therapeutic targets. Pharmacol Res . (2021) 163:105325. doi: 10.1016/j.phrs.2020.105325
22. Brietzke E, Kauer-Sant'Anna M, Teixeira AL, Kapczinski F. Abnormalities in serum chemokine levels in euthymic patients with bipolar disorder. Brain Behav Immun . (2009) 23:1079–82. doi: 10.1016/j.bbi.2009.04.008
23. van den Ameele S, Coppens V, Schuermans J, De Boer P, Timmers M, Fransen E, et al. Neurotrophic and inflammatory markers in bipolar disorder: A prospective study. Psychoneuroendocrinology . (2017) 84:143–50. doi: 10.1016/j.psyneuen.2017.07.003
24. Munkholm K, Brauner JV, Kessing LV, Vinberg M. Cytokines in bipolar disorder vs. healthy control subjects: a systematic review and meta-analysis. J Psychiatr Res . (2013) 47:1119–33. doi: 10.1016/j.jpsychires.2013.05.018
25. Modabbernia A, Taslimi S, Brietzke E, Ashrafi M. Cytokine alterations in bipolar disorder: a meta-analysis of 30 studies. Biol Psychiatry . (2013) 74:15–25. doi: 10.1016/j.biopsych.2013.01.007
26. Pantović-Stefanović M, Petronijević N, Dunjić-Kostić B, Velimirović M, Nikolić T, Jurišić V, et al. sVCAM-1, sICAM-1, TNF-α and IL-6 levels in bipolar disorder type I: Acute, longitudinal and therapeutic implications. World J Biol Psychiatry . (2016) 19:S41–51. doi: 10.1080/15622975.2016.1259498
27. Marin C, Alobid I, Fuentes M, López-Chacón M, Mullol J. Olfactory dysfunction in mental illness. Curr Allergy Asthma Rep . (2023) 23:153–64. doi: 10.1007/s11882-023-01068-z
28. Kazour F, Atanasova B, Mourad M, El Hachem C, Desmidt T, Richa S, et al. Mania associated olfactory dysfunction: A comparison between bipolar subjects in mania and remission. J Psychiatr Res . (2022) 156:330–8. doi: 10.1016/j.jpsychires.2022.10.038
29. Hummel T, Sekinger B, Wolf SR, Pauli E, Kobal G. 'Sniffin' sticks': olfactory performance assessed by the combined testing of odor identification, odor discrimination and olfactory threshold. Chem Senses . (1997) 22:39–52. doi: 10.1093/chemse/22.1.39
30. Kamath V, Lasutschinkow P, Ishizuka K, Sawa A. Olfactory functioning in first-episode psychosis. Schizophr Bull . (2018) 44:672–80. doi: 10.1093/schbul/sbx107
31. Kamath V, Paksarian D, Cui L, Moberg PJ, Turetsky BI, Merikangas KR. Olfactory processing in bipolar disorder, major depression, and anxiety. Bipolar Disord . (2018) 20:547–55. doi: 10.1111/bdi.12625
32. Croy I, Nordin S, Hummel T. Olfactory disorders and quality of life–an updated review. Chem Senses . (2014) 39:185–94. doi: 10.1093/chemse/bjt072
33. Cumming AG, Matthews NL, Park S. Olfactory identification and preference in bipolar disorder and schizophrenia. Eur Arch Psychiatry Clin Neurosci . (2011) 261:251–9. doi: 10.1007/s00406-010-0145-7
34. Grande I, Berk M, Birmaher B, Vieta E. Bipolar disorder. Lancet . (2016) 387:1561–72. doi: 10.1016/s0140-6736(15)00241-x
35. Luo Y, He H, Zhang M, Huang X, Fan N. Altered serum levels of TNF-alpha, IL-6 and IL-18 in manic, depressive, mixed state of bipolar disorder patients. Psychiatry Res . (2016) 244:19–23. doi: 10.1016/j.psychres.2016.07.027
36. Solmi M, Suresh Sharma M, Osimo EF, Fornaro M, Bortolato B, Croatto G, et al. Peripheral levels of C-reactive protein, tumor necrosis factor-alpha, interleukin-6, and interleukin-1beta across the mood spectrum in bipolar disorder: A meta-analysis of mean differences and variability. Brain Behav Immun . (2021) 97:193–203. doi: 10.1016/j.bbi.2021.07.014
37. Wang TY, Lee SY, Chen SL, Chung YL, Li CL, Chang YH, et al. The differential levels of inflammatory cytokines and BDNF among bipolar spectrum disorders. Int J Neuropsychopharmacol . (2016) 19. doi: 10.1093/ijnp/pyw012
38. Chen MH, Hsu JW, Huang KL, Tsai SJ, Su TP, Li CT, et al. Role of obesity in systemic low-grade inflammation and cognitive function in patients with bipolar I disorder or major depressive disorder. CNS Spectr . (2021) 26:521–7. doi: 10.1017/S1092852920001534
39. Park SH, Park-Min KH, Chen J, Hu X, Ivashkiv LB. Tumor necrosis factor induces GSK3 kinase-mediated cross-tolerance to endotoxin in macrophages. Nat Immunol . (2011) 12:607–15. doi: 10.1038/ni.2043
40. Figiel I. Pro-inflammatory cytokine TNF-alpha as a neuroprotective agent in the brain. Acta Neurobiol Exp (Wars) . (2008) 68:526–34. doi: 10.55782/ane-2008-1720
Keywords: bipolar I disorder, manic, olfactory sensitivity, olfactory identification, tumor necrosis factor-α, longitudinal study
Citation: Liu X, Su L, Li Y, Yuan H, Zhao A, Yang C, Chen C and Li C (2024) Significant improvements in the olfactory sensitivity of bipolar I disorder patients during euthymia versus manic episodes: a longitudinal study. Front. Psychiatry 15:1348895. doi: 10.3389/fpsyt.2024.1348895
Received: 03 December 2023; Accepted: 25 March 2024; Published: 08 April 2024.
Reviewed by:
Copyright © 2024 Liu, Su, Li, Yuan, Zhao, Yang, Chen and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chunyang Li, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Shanghai Arch Psychiatry
- v.30(2); 2018 Apr 25
Language: English | Chinese
Analysis of Misdiagnosis of Bipolar Disorder in An Outpatient Setting
双相情感障碍在门诊的误诊情况分析.
Bipolar disorder is a mental illness with a high misdiagnosis rate and commonly misdiagnosed as other mental disorders including depression, schizophrenia, anxiety disorders, obsessive-compulsive disorders, and personality disorders, resulting in the mistreatment of clinical symptoms and increasing of recurrent episodes.
To understand the reasons for misdiagnosis of bipolar disorder in an outpatient setting in order to help clinicians more clearly identify the disease and avoid diagnostic errors.
Data from an outpatient clinic included two groups: those with a confirmed diagnosis of bipolar disorder (CD group) and those who were misdiagnosed (i.e. those who did in fact have bipolar disorder but received a different diagnoses and those without bipolar disorder who received a bipolar diagnosis [MD group]). Information between these two groups was compared.
There were a total of 177 cases that met the inclusion criteria for this study. Among them, 136 cases (76.8%) were in the MD group and 41 cases (23.2%) were in the CD group. Patents with depression had the most cases of misdiagnosis (70.6%). The first episode of the patients in the MD group was more likely to be a depressive episode (χ 2 =5.206, p =0.023) and these patients had a greater number of depressive episodes during the course of the disease ( Z =-2.268, p =0.023); the time from the onset of the disease to the first treatment was comparatively short ( Z =-2.612, p =0.009) in the group with misdiagnosis; the time from the onset of disease to a confirmed diagnosis was longer ( Z =-3.685, p <0.001); the overall course of disease was longer ( Z =-3.274, p =0.001); there were more inpatients for treatment (χ 2 =4.539, p =0.033); and hospitalization was more frequent ( Z =-2.164, p =0.031). The group with misdiagnosis had more psychotic symptoms (χ 2 =11.74, p = 0.001); particularly when depression occurred (χ 2 =7.63, p = 0.006), and the incidence of comorbidity was higher (χ 2 =5.23, p =0.022). The HCL-32 rating was lower in the misdiagnosis group ( t =-2.564, p =0.011). There were more patients diagnosed with bipolar and other related disorders in the misdiagnosis group than in the confirmed diagnosis group (11.0% v. 4.9%) and there were more patients in the MD group diagnosed with depressive episodes who had a recent episode (78.7% v. 65.9%).
Conclusions
The rate of misdiagnosis of patients with bipolar receiving outpatient treatment was quite high and they often received a misdiagnosis of depression. In the misdiagnosis group the first episode tended to manifest as a depressive episode. In this group there were also a greater number of depressive episodes over the course of illness, accompanied by more psychotic symptoms and a higher incidence of comorbidity. Moreover, these patients apparently lacked insight into their own mania and hypomania symptoms, resulting in difficulties in early diagnosis, longer time needed to confirm the diagnosis, higher rate of hospitalization, and greater number of hospitalizations.
背景
双相情感障碍是一种高误诊率的精神疾病,常被误诊为抑郁症、精神分裂症、焦虑症、强迫症和人格障碍等精神疾病,导致临床症状不能有效控制,病情呈反复发作趋势,故近年来双相情感障碍的误诊问题越来越引起精神科医生的重视。
目的
了解双相情感障碍在门诊的误诊情况,并分析其误诊原因,指导临床医师加强对双相情感障碍的识别,尽量避免或减少其误诊和漏诊。
方法
纳入专家门诊确诊为双相情感障碍的患者,了解其在门诊的就诊及误诊和漏诊情况,通过比较误诊组(包含漏诊者)和确诊组的临床资料进一步分析导致误诊和漏诊的可能原因。
结果
双相情感障碍在专家门诊就诊患者中占 31.5%。符合本研究入组标准的共有177 例,其中误诊组136 例(76.8%),确诊组41 例(23.2%),误诊为抑郁症者最多(70.6%)。误诊组患者首次发作更多的表现为抑郁发作( χ2 =5.206, p =0.023),并且病程中抑郁发作次数更多( Z =-2.268, p =0.023);误诊组起病至首次治疗的时间较短( Z =-2.612, p =0.009)、而起病至确诊时间更长 ( Z =-3.685, p <0.001),总病程更长( Z =-3.274, p =0.001),并且住院治疗的患者更多( χ2 =4.539, p =0.033),住院次数也更多( Z =-2.164, p =0.031);误诊组伴有精神病性症状更多( χ2 =11.74, p =0.001),尤其抑郁发作时( χ2 =7.63, p =0.006),共病的发生率更高( χ2 =5.23, p =0.022);误诊组HCL-32 评分更低( t =-2.564, p =0.011)。误诊组诊断为其他特定的双相及相关障碍的患者较确诊组多(11.0% v. 4.9%),并且误诊组最近发作情况表现为抑郁发作的 患者较多(78.7% v. 65.9%)。
结论
门诊双相情感障碍患者的误诊率高,常被误诊为抑郁症。误诊组患者首次发作更多的表现为抑郁发作,病程中抑郁发作次数更多,伴有精神病性症状更多,共病的发生率更高,并且患者对自身躁狂或轻躁狂发作情况明显认识不足,导致早期难以明确诊断,确诊所需时间更长,住院比率更高,住院次数更多。临床医生应提高对双相情感障碍的识别,避免或减少双相情感障碍的误诊和漏诊。
1. Background
Misdiagnosis is an incorrect diagnosis. The objectives of making a diagnosis are to determine the nature of a disease and to select targeted treatment so that the condition takes a favorable turn. Therefore, the incorrect, incomprehensive, or untimely diagnosis is considered to be a misdiagnosis. In clinical work, bipolar disorder is usually difficult to diagnose in its early stages, especially when it has an early onset. Hirschfeld and colleagues [ 1 ] reported that the misdiagnosis rate for bipolar disorder could reach as high as 69%. Only 20% of patients with bipolar disorder with a current depressive episode were given a confirmed diagnosis within the first year of treatment. A confirmed diagnosis was typically given 5 to 10 years after the first episode of the disease. [ 2 ] Generally, the disorder was misdiagnosed as major depressive disorder, schizophrenia, anxiety disorder, borderline personality disorder, or substance dependence. [ 3 ] It was most commonly misdiagnosed as major depressive disorder. [ 4 ] Because of psychotic symptoms, 31% of patients with bipolar I disorder were mistakenly diagnosed as having other disorders with obvious psychotic symptoms such as schizophrenia or substance use induced psychotic disorders. [ 5 ] The reason for this may be related to clinical practitioners who believe that Schneider’s first rank symptoms are specific symptoms of schizophrenia. [ 6 ] Patients with bipolar II disorder were usually misdiagnosed as having unipolar depression. [ 7 ] The reason might be related to the disease characteristics of bipolar disorder. When the clinical manifestation of the first episode was depression, the patient was often simply diagnosed as having depressive disorder. [ 6 ] Misdiagnosis also occurs when there are other comorbid disorders making affective symptoms, when there is not sufficient attention paid to medical history, or through overly restrictive use of the diagnostic criteria. Some studies showed that bipolar disorder has high comorbidity [ 8 , 9 ] often combined with alcohol and drug dependence, personality disorder, and all sorts of anxiety disorders. The clinical manifestations of comorbidity often masked or were confused with affective symptoms, thereby causing clinical misdiagnosis.
Currently, there is still a lack of systematic research regarding the identification rate and the diagnostic rate of bipolar disorder and clinicians understanding of bipolar disorder. Therefore, we followed up and analyzed data from patients seen in our psychiatric specialist clinic receving treatment for bipolar disorder in order to further understand the reasons for misdiagnosis.
2.1 Participants
The participants in this study were patients with bipolar disorder that had consecutive consultations in the specialist outpatient clinic of our hospital from March 1 st 2016 to August 31 st 2016. There were a total of 181 cases. After selection, 177 cases were enrolled, including 85 males and 92 females. Range of ages was from 18 to 64 years old. The mean(SD) age was 29.1 (11.5) years old. All participants were in line with the following: (a) meeting diagnostic criteria for bipolar disorder according to DSM-V; (b) at least 2 consultation visits after enrollment into this study; (c) aged 18 to 65 years; (d) did not have severe somatic diseases, mental retardation, mental disorders caused by organic diseases, psychoactive substance or alcohol abuse. We excluded pregnant and lactating women, holdouts and people with incomplete clinical data. The enrolled participants were divided into two groups. The participants who were diagnosed with bipolar disorder in the first visit were regarded as the confirmed diagnosis group. The participants who were not diagnosed with bipolar disorder in the first visit and yet received a bipolar diagnosis in the return visit were regarded as the misdiagnosis group (including patients with missed diagnosis: The diagnosis was depression when the participants only showed depressive episode in the first consultation and there was no confirmed mania or hypomania episodes. The diagnosis was bipolar disorder when mania and hypomania were present in the return visit). There were 41 participants (23.2%) in the confirmed diagnosis group and 136 persons (76.8%) in the misdiagnosis group.
2.2 Study methods
Cross-sectional and retrospective study methods were used. Information were collected by professional psychiatrists. The method of information gathering was a combination of checking medical history and interviews with the patient and at least one immediate family member. The relevant clinical data was recorded in detail. Demographic data and clinical data of all patients with bipolar disorder were collected using a self-compiled questionnaire. Clinical data included the age of first onset, the clinical manifestation of the first episode, the time from the onset to the first consultation, the course of disease, the time from the onset to the confirmed diagnosis, diagnosis and classification, the number of manic depressive episodes, whether there were mixed characteristics to these episodes, whether or not patient was hospitalized for treatment, current clinical manifestation and treatment, whether or not there is a family history of mental illness, history of suicide, psychotic symptoms, and whether the bipolar disorder is rapid cycling or comorbid with another illness. All the enrolled patients were assessed with PHQ-9 and HCL-32 self-rating scales. The demographic data and clinical data of the MD group and CD group were compared.
2.3 Statistical methods
All data were processed using SPSS 17.0 Methods used included t-test, Mann-Whitney test, and chi-square test. A p value of less than 0.05 was considered statistically significant and less than 0.01 was considered highly statistically significant.
3.1 Bipolar disorder consultation and misdiagnosis in an outpatient department
In this study, there were 574 cases of outpatients in the specialist clinic. Among these cases, there were 181 patients with bipolar disorder (31.5%). Of these, 177 cases that met the inclusion criteria. Among the cases, 136 cases had had misdiagnosis and the misdiagnosis rate reached 76.8% (see figure 2 ). The most common misdiagnosis was depression (96 cases, 70.6%) followed by schizophrenia (28 cases, 20.6%) and obsessive compulsive disorder (21 cases, 15.4%); also included were anxiety disorder (9 cases, 6.6%) and personality disorder (2 cases, 1.5%) (see figure 3 ). Among them, 16 patients were misdiagnosed with 2 disorders and 2 patients were misdiagnosed with 3 disorders.

Bipolar disorder consultation in the specialist outpatient clinic

Other diagnoses besides Bipolar given (MD group)
3.2 Comparison of the demographic data between the MD group and CD group (see table 1 )
Comparison of the demographic data between the bipolar disorder misdiagnosis group and confirmed diagnosis group
The difference between the demographic data of the two groups was not statistically significant in any category.
3.3 Comparison of the clinical characteristics between the bipolar disorder MD group and CD group
The age at first episode ( t =-0.059, p =0.953), total number of episodes ( Z = -1.019, p = 0.308), number of manic episodes ( Z = -1.373, p = 0.17), and the PHQ-9 score during depressive episode ( t =1.177, p =0.241) had no statistically significant differences. There was also no difference between the two groups in family history of bipolar disorder.
Patients in the MD group more commonly had depression during their first episode ( χ 2 = 5.206, p = 0.023) and the number of depressive episodes was significantly more during the course of illness ( Z = -2.268, p = 0.023). The time from the onset of illness to first treatment was significantly shorter ( Z =-2.612, p =0.009) in the MD group, the time from the onset of illness to the confirmed diagnosis was longer ( Z =-3.685, p <0.001), the overall course of disease was longer ( Z =-3.274, p =0.001), there were more cases receiving inpatient treatment ( χ 2 =4.539, p =0.033), and hospitalization was more frequent ( Z =-2.164, p =0.031). The MD group had more psychotic symptoms ( χ 2 =11.74, p = 0.001), particularly during depressive episodes ( χ 2 =7.63, p = 0.006), and the incidence of comorbidity was higher ( χ 2 =5.23, p =0.022). The HCL-32 rating was lower in the MD group ( t =-2.564, p =0.011). See table 2 .
Comparison of the clinical characteristics between the bipolar disorder misdiagnosis group and confirmed diagnosis group
3.4 Comparison of diagnosis and pharmacological treatment between the MD group and CD group
There was no statistically significant difference between the two groups in diagnostic classification ( χ 2 =1.417, p =504), but there were more patients diagnosed with other specific bipolar and related disorders in the MD group than in the CD group (11.0% v. 4.9%). In terms of recent episodes and clinical medication, the differences between the 2 groups were not statistically significant ( χ 2 =2.816, p =0.093). However, the patients in the misdiagnosis group that in recent mood episodes presented with depression were more (78.7% v. 65.9%). The ratio of rapid cycling episodes in the two groups ( χ 2 =0.012, p =0.914) and having episodes with mixed features ( χ 2 =0.086, p =0.770) were not statistically significant. See table 3
Comparison of the diagnosis and pharmacological treatment between the bipolar disorder misdiagnosis group and confirmed diagnosis group
* p <0.05
** p <0.01
3.5 Comparison of the number of manic and depressive episodes between the MD and CD groups
There were more depressive episodes than manic episodes reported in both groups. This difference in the MD had high statistical significance ( Z = -9.034, p = 0.001). This difference in the CD group also had statistical significance ( Z = -2.508, p = 0.012). See table 4
Comparison of the manic and depressive episodes between the bipolar disorder misdiagnosis group and confirmed diagnosis group
4. Discussion
4.1 main findings.
The results of this study show that the misdiagnosis rate of bipolar disorder was 76.8%. The misdiagnosis rate is slightly higher than the reported results in studies conducted outside of China. [ 1 ] This could be related to the source of our sample. All the patients selected for this study were from the specialist outpatient department, including a larger number of patients with refractory bipolar disorder and atypical symptoms. Of the 177 patients enrolled, 36 had mixed features, 53 had rapid cycling episodes, 51 had comorbidity with other disorders, and 17 were diagnosed with other specific bipolar and related disorders.
This study shows that bipolar disorder patients are most likely to be misdiagnosed with depression. The misdiagnosis rate is as high as 70.6%. The result shares similarity with other studies. [ 2 , 10 ] The reason may be related to the characteristics of the onset of bipolar disorder itself, especially when the episode of onset is depressive with no mania or hypomania. [ 2 , 11 ] In the entire course of bipolar disorder, there were apparently more depressive episodes than manic or hypomanic episodes. [ 12 ] In particular the patients with bipolar II disorder had a depressive presentation throughout most of their illness, [ 13 ] making the clinical diagnosis even more difficult. In the misdiagnosis group of this study, there were more patients having a depressive episode at onset and the frequency of depressive episodes was apparently higher than the manic episode, thereby prolonging the time for clinical diagnosis and increasing the misdiagnosis rate.
Patients with bipolar disorder are often misdiagnosed as having unipolar depression in many circumstances. The reason is related to clinicians or patients lacking knowledge about manic and hypomanic symptoms. Some research shows that the hypomanic state was often mistaken by clinicians or patients as the signs of improvement or remission of depression and they neglected the risk of the disorder further worsening, resulting in misdiagnosis. [ 14 , 15 ] The results of this study showed that the HCL-32 score of the patients in the MD group was lower, which also confirmed the above views.
The results of this study also showed that 20.6% of the patients with bipolar disorder were misdiagnosed as having schizophrenia. In addition, more than half of the 136 patients in the MD group had psychotic symptoms, so it was clear that the presence of psychotic symptoms increased the risk of being misdiagnosed as having schizophrenia especially during the onset of depression. In other studies, 61.5% of patients with bipolar disorder with psychotic symptoms were misdiagnosed as having other mental disorders at the time of first treatment. Moreover, 45% of the patients showed psychotic symptoms such as hallucinations or delusions during depressive episodes. [ 17 ] Some studies [ 18 ] showed that psychotic symptoms are one of the major risk factors for bipolar disorder in patients with depression. They can even be used as a predictor of whether patients with depression have bipolar disorder.
In this study, 15.4% of patients were misdiagnosed with obsessive-compulsive disorder, 6.6% of them were misdiagnosed with anxiety disorder, and 1.5% of them were misdiagnosed as having a personality disorder. The reason for misdiagnosis may be related to the comorbidity of bipolar disorder. Comorbidity was very common in bipolar disorder. This study showed that 1/3 of the patients in the MD group had comorbidity and it was more than in the CD group. It can be seen that the presence of comorbidity may mask emotional symptoms, leading to an increase in misdiagnosis rate. A meta-analysis [ 8 ] indicated that the incidence of comorbid anxiety disorders with bipolar disorder was 42.7% and comorbid obsessive-compulsive disorder was 10.7%. A systematic review of 64 related articles [ 9 ] indicated that the incidence of bipolar disorder comorbid with obsessive-compulsive disorder was between 11% and 21%. Comorbidity results in complex or atypical clinical symptoms, increases the rate of clinical misdiagnosis, and leads to treatment difficulties.
In terms of diagnosis classification, this study showed that there was no significant statistical difference between the two groups. However, the patients of the MD group diagnosed as other specific bipolar disorder and other related disorder were slightly more than the CD group. This could be one of the reasons for misdiagnosis. Many of the symptoms of the patients in this study were hypomanic or manic yet did not fit the time criteria for bipolar. For example hypomanic symptoms only lasted 2 to 3 days, or the time criteria for a hypomanic episode was met but the criteria for other symptoms were not met. These were harder to identify and diagnose at an early stage. However, this study was carried out in a clinic specializing in affective disorders therefore the staff in this setting may have a higher ability to diagnose this type of bipolar disorder.
4.2 Limitations
This study was a cross-sectional and retrospective study. The clinical data were collected mainly from checking past medical records and interviewing patients and at least one family member regarding history of illness. Although each patient had at least two follow-up visits and was asked carefully about the medical history in order to ensure the integrity of the medical history data, it is not guaranteed that the patients and their family members provided a complete medical history. Patients with a long medical history and recurrent episodes were especially unable to recall the timing and manifestation of each episdoe.
The sample for this study originated from a psychiatric clinic specializing in the diagnosis and treatment of affective disorders. The diagnosis and differential diagnosis in this clinic were more standardized; the compliance of the patients was good; the interruption rate of treatment was low; and the drop-out rate from follow-up visits was low. Therefore this sample should be somewhat conducive to follow-up and research development. However, the source of the sample was relatively narrow in this study as it did not include patients with other diagnoses or in other treatment settings. Moreover, the sample size was limited and the diagnosis and treatment situations of bipolar disorder in the general outpatient service were not covered. Therefore, a wider and larger sample study is needed to further explore the current status of bipolar disorder misdiagnosis in psychiatric outpatient clinics in China.
4.3 Implications
When bipolar disorder is misdiagnosed or missed altogether, symptoms cannot be effectively treated, episodes tend to be recurrent, and rapid cycling episodes are more commonly seen. [ 19 ] The risk of suicide increases, [ 20 ] which in turn increases the need for hospitalization and overall burden of the disease. [ 21 ] This can also explain why the patients in the MD group tended to have a higher rate of hospitalization. Therefore, early diagnosis is conducive to appropriate and timely treatment and is beneficial to the maximum recovery of the patients’ function. The earlier the correct diagnosis and treatment, the greater the chance that the patient will recover.
However, any doctor could make mistakes in cross-sectional diagnosis due to the complexity of the presentation of bipolar disorder. This study looked into the causes of bipolar disorder misdiagnosis and missed diagnosis in the outpatient service in hopes of improving guidance for clinical workers. In order to prevent the misdiagnosis of bipolar disorder, clinicians should conduct comprehensive and in-depth clinical examination, pay full attention to emotional symptoms, identify hypomanic symptoms carefully, search for diagnostic clues for bipolar disorder from the clinical symptoms of depression, ask about whether there were past episodes of hypomania or mania especially during medical history collection, and enhance the identification of bipolar disorder so as to avoid or reduce the misdiagnosis and missed diagnosis of bipolar disorder.
Subsequently, clinicians should try harder to identify psychiatric symptoms and affective symptoms and pay close attention to those depressive patients with psychotic symptoms. At the same time, they should consider that comorbidity with other disorders in bipolar is common. Clinicians should improve the identification of comorbidity and avoid or reduce the misdiagnosis and missed diagnosis of bipolar disorder so as to give timely and standardized treatment to patients with bipolar disorder and improve the short-term and long-term treatment effects and quality of life to the greatest extent.

Flowchart of the study
Hui Shen acquired her bachelor’s degree in clinical medicine at Shanghai Second Medical University in 2003. In the same year she began working at the Shanghai Mental Health Center. She has 13 years of clinical work experience in psychiatry. At present, she is the chief rehabilitation doctor at SMHC. Her research interests are the treatment of schizophrenia and bipolar disorder, as well as the cognitive function and rehabilitation therapy of psychiatric patients.
Funding statement
Shanghai Mental Health Center affiliated to the Shanghai Jiao Tong University project (project code: 2016-YJ-12);
Shanghai Mental Health Center affiliated to the Shanghai Jiao Tong University project (project code: 2014 - YL - 04);
National Key Technology Research and Development Program (project code:2012BAI01B04)
Conflicts of interest statement
The authors declare no conflict of interest related to this manuscript.
Informed consent
Written informed consent was provided by all participants.
Ethical approval
This study was approved by the ethics committee of the Shanghai Mental Health Center affiliated to Shanghai Jiao Tong University.
Copyright permission on work’s translation
I have authorized the article to Shanghai Archives of Psychiatry for translation from Chinese to English. I have confirmed all the information included in this article is correct.
Authors’ contributions
Hui Shen: research design, data analysis, and article writing
Li Zhang: medical history collection, scale evaluation
Chuchen Xu: medical history collection, scale evaluation, and literature review
Meijuan Chen: research guidance
Yiru Fang: research guidance

FDA Approves Fanapt for Mixed, Manic Episodes Associated With Bipolar I Disorder
The atypical antipsychotic was approved for the acute treatment of schizophrenia in 2009.

Argus_AdobeStock

The US Food and Drug Administration (FDA) has approved Fanapt® (iloperidone) tablets for the acute treatment of mixed or manic episodes connected to bipolar I disorder in adults. Fanapt is a second-generation antipsychotic that was FDA-approved for the acute treatment of schizophrenia in 2009. 1,2
“Manic or mixed episodes associated with bipolar I disorder are highly complex conditions, which require a host of trusted options to meet individual patient needs, said Mihael H. Polymeropoulos, MD, president, CEO, and chairman of the board at Fanapt developer Vanda Pharmaceuticals Inc, in a press release.
“With over 100,000 patient years of experience, Fanapt is a familiar therapeutic agent that offers flexible dosing with a well-known safety profile. This FDA approval gives patients and service providers a new treatment option for managing bipolar I disorder.”
The FDA based this decision on the results of a phase 3 clinical trial assessing the efficacy of Fanapt in managing acute manic and mixed episodes linked with bipolar I disorder in adults.1 The clinical study (VP-VYV-683-3201) involved around 400 participants who had been diagnosed with bipolar I disorder and were experiencing a current manic episode. These participants were randomly assigned to receive either Fanapt or a placebo at a 1:1 ratio across clinical sites in the United States, Bulgaria, and Poland. 3
The primary measurement at the end of week 4 was conducted using the Young Mania Rating Scale (YMRS), which evaluates the severity of manic symptoms. Results indicated that patients treated with Fanapt exhibited notably greater improvement compared with those receiving the placebo, with a highly statistically significant difference (p=0.000008) observed. 3
Throughout the 4-week study period, YMRS assessments were conducted weekly. Significant improvement in the Fanapt group over the placebo group was evident as early as week 2. Various secondary outcome measures, including the Clinician Global Impression of Severity (CGI-S) and the Clinician Global Impression of Change (CGI-C), also achieved statistical significance (p=0.0005 and p=0.0002, respectively). 3
Fanapt has also shown efficacy in reducing the symptoms of bipolar mania in a more recent study entitled, “Efficacy and safety of iloperidone in bipolar mania: a double-blind, placebo-controlled study,” 1 the results of which Vanda submitted to the FDA in January 2024. 4 This phase 3 study focused on patients who were exhibiting psychotic features, with half of the total 414 participants receiving a daily dose of 24 mg of Fanapt (206 participants) and the other half receiving a placebo (208 participants). 2
The study protocol consisted of a screening period lasting up to 7 days prior to randomization, followed by a 1-day baseline evaluation period and a subsequent 28-day treatment phase.
The primary objective of the study was to assess the change in symptoms of mania from baseline to week 4, as measured by the YMRS, in comparison with the placebo group. Secondary efficacy measures included changes in scores on the CGI-S and CGI-C scales from baseline. 2
Results indicated a notable improvement in mania symptoms among participants receiving Fanapt compared with those receiving the placebo at the 4-week mark. Specifically, Fanapt was associated with a mean reduction of -4.0 on the YMRS scale (P = .000008) and significant decreases in scores on the CGI-S (mean, -0.4; P = .0005) and CGI-C scales (mean, -0.5; P = .0002) when compared with the placebo group. Statistically significant differences favoring Fanapt were also observed as early as day 14 and continued through days 21 and 28 of the study. 2
“Many patients today are still unable to find suitable treatment options for effectively managing bipolar disorder,” said Stephen Stahl, MD, PhD, professor of psychiatry at the University of California San Diego, in a press release. “Tailoring the right treatment for the right patient is critical for effective care, and the approval of Fanapt represents an important milestone. Fanapt possesses a well-studied safety profile, and its approval will provide patients with a new and effective option for treating a highly complex disorder.”
Stay up-to-date on news related to research on promising new interventions and developments in the treatment of a wide variety of psychiatric disorders at psychiatrictimes.com .
Note: This article was prepared with the assistance of ChatGPT.
1. Vanda Pharmaceuticals’ Fanapt® (iloperidone) receives US FDA approval for the acute treatment of bipolar I disorder. PR Newswire. News release. April 2, 2024. Accessed April 2, 2024. https://www.prnewswire.com/news-releases/vanda-pharmaceuticals-fanapt-iloperidone-receives-us-fda-approval-for-the-acute-treatment-of-bipolar-i-disorder-302106405.html
2. Yasgur BS. Schizophrenia med safe, effective for bipolar mania: phase 3 data. MedScape. February 1, 2024. Accessed April 1, 2024. https://www.medscape.com/viewarticle/schizophrenia-med-safe-effective-bipolar-mania-phase-3-data-2024a100029i?form=fpf
3. Fanapt® shown to be effective in bipolar I disorder in phase III clinical study. Vanda Pharmaceuticals Inc. News release. December 19, 2022. Accessed April 2, 2024. https://vandapharmaceuticalsinc.gcs-web.com/node/15146/pdf
4. Vanda Pharmaceuticals announces the publication of Efficacy and Safety of Iloperidone in Bipolar Mania: A Double-Blind, Placebo-Controlled Study in the Journal of Clinical Psychiatry. PR Newswire. News release. January 17, 2024. Accessed April 1, 2024. https://www.prnewswire.com/news-releases/vanda-pharmaceuticals-announces-the-publication-of-efficacy-and-safety-of-iloperidone-in-bipolar-mania-a-double-blind-placebo-controlled-study-in-the-journal-of-clinical-psychiatry-302037494.html

The Week in Review: April 1-5

Here's to a Psychedelic Revolution
First Patient Dosed in Phase 2 Clinical Trial of NBI-1070770 for MDD

Blue Light, Depression, and Bipolar Disorder

An Update on Bipolar I Disorder

Psychiatry in the News: March 2024
2 Commerce Drive Cranbury, NJ 08512
609-716-7777


IMAGES
VIDEO
COMMENTS
We're going to go ahead to patient case No. 1. This is a 27-year-old woman who's presented for evaluation of a complex depressive syndrome. She has not benefitted from 2 recent trials of antidepressants—sertraline and escitalopram. This is her third lifetime depressive episode.
Sarah is a 42-year-old married woman who has a long history of both depressive and hypomanic episodes. She has been diagnosed with bipolar disorder based on her symptoms, such as alcohol use, hyper-sexuality, and mood cycles, and her previous diagnoses, such as borderline personality disorder and major depression. The web page provides details of her case study, diagnosis, and treatment options.
Gary is a 19-year-old who withdrew from college after a manic episode and was diagnosed with bipolar disorder. Learn about his symptoms, diagnosis, and treatment options from this case study by a clinical psychologist.
Gus Alva, MD, DFAPA: Psychiatric Times presents this roundtable on the management of bipolar disorder, a phenomenal dialogue allowing clinicals a perspective regarding current trends and where we may be headed in the future. This is an interesting case, as we take a look at this 23-year-old female who first comes in to see her psychiatrist with moderate depressive symptoms.
EP: 4. Takeaways for Bipolar Disorder Management. Nidal Moukaddam, MD, PhD: Today, we're going to talk about a new case. A 30-year-old man has taken short-term disability leave from work due to the progression of a depressive episode. He received a diagnosis of bipolar I disorder about 10 years ago. He had his first episode of mania at the ...
studies. Case reports and small observations studies or randomized controlled trials of fewer than 50 patients were excluded. Modern definitions of bipolar disorder In the 1970s, the International Classification of Diseases and the Diagnostic and Statistical Manual of Mental Disorders reflected the prototypes of mania
Presents a case report of a 30-year-old married Caucasian woman, presented to our university clinic seeking a new psychiatrist to manage her bipolar illness. She had moved to the Southeast due to her husband's job relocation three months ago, and had few social contacts in her new city. She reported emerging from the depths of a severe major depressive episode one year ago and since then had ...
The terms "soft bipolar" or "bipolar spectrum" were first proposed by Akiskal and Mallya ( 4) to describe psychopathological states that could not be easily diagnosed. It has been reported that soft bipolar cases may be prevalent up to 5.1%-23.7% ( 5 ). Cyclothymia and unspecified type of bipolar disorder are suggested to be present ...
Early-onset Bipolar Disorder. Studies have shown that bipolar disorder usually begins with an index episode of depression: positive family history (Pavuluri, Birmaher, & Naylor, 2005), clinical severity, psychotic symptoms, and psychomotor retardation are well documented predictors of bipolarity.Approximately 20% of youths with a first major depressive episode will develop a manic episode.
Chapter 5 covers the psychiatric treatment of bipolar disorder, including a case history, key principles, assessment strategy, differential diagnosis, case formulation, treatment planning, nonspecific factors in treatment, potential treatment obstacles, ethical considerations, common mistakes to avoid in treatment, and relapse prevention.
Introduction. Bipolar disorder is one of the common psychiatric disorders with an episodic instability in the mood, behavior, and insight ().It has a significant impact on individual performance, reduces the quality of life (), and amplifies suicide risk ().Fortunately, with advances in the treatment of psychiatric illnesses, including bipolar disorder, many of these patients are able to live ...
The current study is a case report involving three Japanese patients with bipolar II disorder, who started CBT during the depressive phase after a hypomanic episode was stabilized by pharmacotherapy. All patients experienced excessively positive thinking one week apart and were able to choose behaviors that would stabilize bipolar mood by ...
In the 1990s, bipolar disorder was seen as a severe, rare, incurable condition found only in adults. Medication, primarily lithium, was the sole treatment offered to most patients. Today, experts are learning that the disorder is more common—affecting about 4% of U.S. children and adults—and presents along a diverse continuum.
Susan's Case Study in the Context of ATI Bipolar Disorder. Susan's case study is an example of how individual experiences can inform the development of Assessment Technologies Institute (ATI) for bipolar disorder. By examining her journey, researchers can analyze treatment approaches, evaluate the effectiveness of various interventions, and ...
Case 1. Ms. Genera is a 36-year-old woman with bipolar II disorder, first diagnosed in college, who is brought to the psychiatric emergency room by her boyfriend of 5 years. He is hoping that she will be admitted to the hospital "before she goes all-the-way manic.". He reports that she "almost lost her job last time!".
In 2023, the Heinz C. Prechter Bipolar Research Program was named as one of six institutions that is part of the BD² Integrated Network with BD²: Breakthrough Discoveries for Thriving with Bipolar Disorder.. Along with Brigham and Women's Hospital-McLean Hospital, University of California Los Angeles, Johns Hopkins University, Mayo Clinic, UTHealth Houston, the Prechter Program at the ...
Case Studies in Communication Disorders - October 2016. ... Case study 48 - Woman aged 24 years with bipolar disorder. from Section F - Psychiatric disorders. Published online by Cambridge University Press: 09 November 2016 Louise Cummings. Show author details Louise Cummings
As you peruse the pages of this case study, you'll join the intricate journey through the life of a patient with bipolar disorder, whose story might resonate more deeply than you'd expect. You'll witness the oscillation between the highs of mania and the lows of depression, and understand why recognizing the nuances of this condition is pivotal.
Case Report on Bipolar Affective Disorder: Mania with Psychotic Symptoms Kounassegarane Deepika AbstrAct Bipolar affective disorder (BPAD) is a major psychiatric disorder all around the world, which is mainly characterized by frequent and recurrent episodes of mania, hypomania, and depression. A majority of complete etiology or pathogenesis of ...
Let's start by reviewing a couple of case scenarios and try to figure this out. The first one is a patient with bipolar 1 disorder who reports new onset of movements. This is a 54-year-old woman who received a diagnosis of bipolar 1 disorder at the age of 32, after requiring hospitalization for an acute manic episode.
Introduction. In the United States, the aggregate twelve-month prevalence rate of DSM-V bipolar I and. II disorders, along with bipolar disorder not otherwise specified, is 1.8%, and the ...
Introduction. Bipolar disorder (BD) is a chronic illness associated with severely debilitating symptoms that can have profound effects on both patients and their caregivers (Miller, 2006).BD typically begins in adolescence or early adulthood and can have life‐long adverse effects on the patient's mental and physical health, educational and occupational functioning, and interpersonal ...
The article, A case study on bipolar affective disorder, current episode without psychotic symptoms (ICD F 31.1), is a record of original research effort, we therefore declare. We attest to the work's originality and the absence of any instances of plagiarism across the whole manuscript. ...
Background: While numerous studies have compared symptoms of major depressive episodes (MDEs) associated with bipolar disorder (BD; i.e., bipolar depression) versus major depressive disorder (MDD; i.e., unipolar depression), little is known about this topic in youth. We compared MDE symptoms in youth with BD with youth with suspected BD who have similar clinical and familial characteristics ...
Introduction: Research has indicated that individuals diagnosed with bipolar disorder (BD) might experience alterations in their olfaction or levels of serum tumor necrosis factor-α (TNF-α), but no studies have investigated olfactory function and serum TNF-α in BD patients simultaneously. Moreover, there is a lack of existing research that ...
In this study, 15.4% of patients were misdiagnosed with obsessive-compulsive disorder, 6.6% of them were misdiagnosed with anxiety disorder, and 1.5% of them were misdiagnosed as having a personality disorder. The reason for misdiagnosis may be related to the comorbidity of bipolar disorder. Comorbidity was very common in bipolar disorder.
A case for early alternative treatments The study, which published Wednesday in the journal JAMA Psychiatry, analyzed national health insurance data for the entire population of Taiwan for a 15 ...
The FDA based this decision on the results of a phase 3 clinical trial assessing the efficacy of Fanapt in managing acute manic and mixed episodes linked with bipolar I disorder in adults.1 The clinical study (VP-VYV-683-3201) involved around 400 participants who had been diagnosed with bipolar I disorder and were experiencing a current manic ...