
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- Health Topics
- < Back To How the Heart Works
- How Blood Flows through the Heart
- What the Heart Looks Like
- How the Heart Beats
MORE INFORMATION

How the Heart Works How Blood Flows through the Heart
Language switcher.
Arteries and veins link your heart to the rest of the circulatory system. Veins bring blood to your heart. Arteries take blood away from your heart. Your heart valves help control the direction the blood flows.
Heart valves
Heart valves control the flow of blood so that it moves in the right direction. The valves prevent blood from flowing backward.
The heart has four valves.
- The tricuspid valve separates the right atrium and right ventricle.
- The mitral valve separates the left atrium and left ventricle.
- The pulmonary valve separates the right ventricle and the pulmonary artery.
- The aortic valve separates the left ventricle and aorta.
The valves open and shut in time with the pumping action of your heart's chambers. The opening and closing involve a set of flaps called cusps or leaflets. The cusps open to allow blood to flow out of a chamber and close to allow the chamber to refill with blood. Heart valve diseases can cause backflow or slow the flow of blood through the heart.
Learn about what the valves of the heart look like and do. Medical Animation Copyright © 2022 Nucleus Medical Media, All rights reserved .
Adding oxygen to blood
Oxygen-poor blood from the body enters your heart through two large veins called the superior and inferior vena cava. The blood enters the heart's right atrium and is pumped to your right ventricle, which in turn pumps the blood to your lungs.
The pulmonary artery then carries the oxygen-poor blood from your heart to the lungs. Your lungs add oxygen to your blood. The oxygen-rich blood returns to your heart through the pulmonary veins. Visit our How the Lungs Work page to learn more about what happens to the blood in the lungs.
The oxygen-rich blood from the lungs then enters the left atrium and is pumped to the left ventricle. The left ventricle generates the high pressure needed to pump the blood to your whole body through your blood vessels.
When blood leaves the heart to go to the rest of the body, it travels through a large artery called the aorta. A balloon-like bulge, called an aortic aneurysm , can sometimes occur in the aorta.
Learn about how your heart circulates blood to your lungs and throughout your body. Medical Animation Copyright © 2022 Nucleus Medical Media, All rights reserved .
Supplying oxygen to the heart’s muscle
Like other muscles in the body, your heart needs blood to get oxygen and nutrients. Your coronary arteries supply blood to your heart. These arteries branch off from the aorta so that oxygen-rich blood is delivered to your heart as well as the rest of your body.
- The left coronary artery delivers blood to the left side of your heart, including your left atrium and ventricle and the septum between the ventricles.
- The circumflex artery branches off from the left coronary artery to supply blood to part of the left ventricle.
- The left anterior descending artery also branches from the left coronary artery and provides blood to parts of both the right and left ventricles.
- The right coronary artery provides blood to the right atrium and parts of both ventricles.
- The marginal arteries branch from the right coronary artery and provide blood to the surface of the right atrium.
- The posterior descending artery also branches from the right coronary artery and provides blood to the bottom of both ventricles.
Your coronary arteries supply oxygen to your body. Medical Animation Copyright © 2022 Nucleus Medical Media, All rights reserved .
Some conditions can affect normal blood flow through these heart arteries. Examples include:
- Heart attack
- Coronary heart disease
The coronary veins return oxygen-low blood from the heart's muscles back to the right atrium so it can be pumped to the lungs. They include:
- The anterior cardiac veins
- The great cardiac vein
- The middle cardiac vein
- The small cardiac vein
Global Health and Education

Circulatory System: Blood Flow Pathway Through the Heart
Pathway of blood through the heart.
In this educational lesson, we learn about the blood flow order through the human heart in 14 easy steps , from the superior and inferior vena cava to the atria and ventricles. Come also learn with us the heart’s anatomy, including where deoxygenated and oxygenated blood flow, in the superior vena cava, inferior vena cava, atrium, ventricle, aorta, pulmonary arteries, pulmonary veins, and coronary arteries.

Quick & Easy Video on Blood Flow Pathway Through the Heart
Blood flow order: step by step animation tutorial.
To gain a visual step-by-step understanding, check out our quick and easy video on the blood flow pathway through the heart in less than 90 seconds. Please notice that blue represents deoxygenated blood , and red represents oxygenated blood .
14 Steps of Blood Flow Through the Heart
In summary from the video, in 14 steps, blood flows through the heart in the following order: 1) body –> 2) inferior/superior vena cava –> 3) right atrium –> 4) tricuspid valve –> 5) right ventricle –> 6) pulmonary arteries –> 7) lu ngs –> 8) pulmonary veins –> 9) left atrium –> 10) mitral or bicuspid valve –> 11) left ventricle –> 12) aortic valve –> 13) aorta –> 14) body .

Superior Vena Cava & Inferior Vena Cava
The vena cava is the largest vein in the body that delivers oxygen-poor or deoxygenated blood to the right atrium of the heart. The superior vena cava comes from the upper part of the body, including the brain and arms, while the inferior vena cava comes from the abdominal area and legs.
Left Atrium & Right Atrium
The atria are the top two chambers of the heart that receive incoming blood from the body. The right atrium receives deoxygenated blood through the superior and inferior vena cavas from the body and pumps it to the right ventricle through the tricuspid valve, which opens to allow the blood flow through and closes to prevent blood backing up the atrium. The left atrium receives oxygenated blood through the pulmonary veins from the lungs. It pumps the blood through the mitral valve to the left ventricle. Attached to the atria are the pouches called auricles that expand to allow the atria to include more blood volume. For fetal circulation , there is a special hole shunt between the left atrium and right atrium called the foramen ovale that diverts blood away from the lungs and goes directly to the rest of the fetus’s body.

Left Ventricle & Right Ventricle
The ventricles are the two lower chambers of the heart. The right ventricle receives oxygen-poor blood from the right atrium and pumps it through the pulmonic semilunar valve to the pulmonary artery and into the lungs to be filled with oxygen. On the other hand, the left ventricle receives oxygen-rich blood from the left atrium and pumps it through the aortic semilunar valve to the aorta to deliver the oxygen to the rest of the body.

Pulmonary Arteries & Pulmonary Veins
The pulmonary arteries deliver oxygen-poor blood from the right ventricle of the heart to the lungs, while the pulmonary veins deliver oxygen-rich blood from the lungs to the left atrium of the heart. For fetal circulation , there is a special hole shunt called the ductus arteriosus that is between the pulmonary arteries and aorta to divert blood away from the fetus’s lungs. Learn more about how the ductus arteriosus works here, and why it’s there for fetuses .
Aorta & Coronary Arteries
The aorta is the largest artery in the body that leads from the left ventricle of the heart to the rest of the body. It carries oxygen-rich blood to deliver to the body’s cells. As an artery, it contains thicker walls than veins because it has to withstand the tough pumping blood pressure of the heart.

The coronary arteries are a set of arteries that branch off the aorta and are located on the heart. They carry oxygenated blood and nutrients to nourish the heart tissue cells. When the coronary arteries are clogged by excessive fatty tissue in cholesterol, it can lead to a lack of nutrients and oxygen for the heart, whose cells begin to perish, and this leads to a heart attack.
Final Test Your Knowledge! 😀
Summary: what are the 14 steps of blood flow through the heart.
Blood flows through the heart in the following order: 1) body –> 2) inferior/superior vena cava –> 3) right atrium –> 4) tricuspid valve –> 5) right ventricle –> 6) pulmonary arteries –> 7) lu ngs –> 8) pulmonary veins –> 9) left atrium –> 10) mitral or bicuspid valve –> 11) left ventricle –> 12) aortic valve –> 13) aorta –> 14) body .
Big thank you to our kind supporters! Please Like and Subscribe to our Email List at moosmosis.org , Facebook , Twitter , Youtube to support our open-access youth education initiatives! 🙂
Copyright © 2022 Moosmosis Organization: All Rights Reserved
All rights reserved. This essay or any portion thereof may not be reproduced or used in any manner whatsoever without the express written permission of the publisher.

Please Like and Subscribe to our Email List at moosmosis.org , Facebook , Twitter , Youtube to support our open-access youth education initiatives! 🙂
*This article has been accepted into Moosmosis’s Journal of Global Health and Education . Accepted 2020. Published July 2020.
Works cited.
- Tubbs RS. The heart is simply a muscle. Clin Anat . 2016;29(3):267-268. doi:10.1002/ca.22704
- Miao JH, Makaryus AN. Anatomy, Thorax, Heart Veins. In: StatPearls . Treasure Island (FL): StatPearls Publishing; 2020.
- Anderson RH, Wilcox BR. Understanding cardiac anatomy: the prerequisite for optimal cardiac surgery. Ann Thorac Surg . 1995;59(6):1366-1375. doi:10.1016/0003-4975(95)00195-q
- Courchaine K, Rykiel G, Rugonyi S. Influence of blood flow on cardiac development. Prog Biophys Mol Biol . 2018;137:95-110. doi:10.1016/j.pbiomolbio.2018.05.005
- Efimov IR. Innovation in optical imaging: looking inside the heart. Heart Rhythm . 2007;4(7):925-926. doi:10.1016/j.hrthm.2007.04.006
Do you “LUB” our hearty content? Please share, subscribe, & like for more! 😀
Share this:.

- Share on Tumblr
Categories: Biology , stem
Tagged as: anatomy , Biology , blood flow , cardiovascular system , circulatory system , college , education , Feature , featured , heart , Journal of Global Health and Education , life , medicine , physiology , school , science , university
Published by Moosmosis
Passionate about lifelong learning, global health, and education! Check out our Moosmosis team's award-winning youth education site and articles @moosmosis.org Recognized by United Nations Academic Impact. View all posts by Moosmosis
249 replies »
- Pingback: Medical School: Learning Pain Management for Medical Students – Moosmosis
Good and Simple learning
Like Liked by 1 person
Thank you Vivek! Happy learning! 🙂
- Pingback: Epidural Hematoma vs Subdural Hematoma vs Subarachnoid Hemorrhage: Symptoms, Diagnosis, Treatment, and Prognosis – Moosmosis
- Pingback: Heart Block: First Degree vs Second Degree (Type I and Type 2) vs Third Degree – ECG Findings, Symptoms, Diagnosis, Treatment, and Prognosis [MCAT, USMLE, Biology, Medicine] – Moosmosis
- Pingback: Aortic Stenosis vs Aortic Regurgitation: Symptoms, Diagnosis, Treatment, and Prognosis [MCAT, USMLE, Biology, Medicine] – Moosmosis
Wonderful diagrams and article on heart blood flow! Wholesome and helpful ❤️
Thank you so much Kay! Have a wonderful day ❤️
Good job done keep it up✌🏻
Thank you so much!!!
Thanks a lot of 👍
Like Liked by 2 people
- Pingback: Systolic Heart Failure vs Diastolic Heart Failure: Symptoms, Diagnosis, Treatment, and Prognosis [MCAT, USMLE, Biology, Medicine] – Moosmosis
- Pingback: Stanford Type A vs Stanford Type B Aortic Dissection: Anatomy, Symptoms, Diagnosis, Treatment, and Prognosis [MCAT, USMLE, Biology, Medicine] – Moosmosis
- Pingback: Heart Attack versus Heart Failure: Anatomy, Symptoms, Diagnosis, Treatment, and Prognosis [MCAT, USMLE, Biology, Medicine] – Moosmosis
- Pingback: Sleeve Gastrectomy vs Roux-en-Y Gastric Bypass vs Adjustable Gastric Banding: Anatomy, Mechanisms, Treatment, and Prognosis – Moosmosis
Excellent and extremely helpful! I was super confused about the order, this helped me understand the heart blood flow steps so much better, thanks!!
Thank you so much Jackie! Happy to help!
- Pingback: Comparing and Contrasting Acute Cholecystitis vs. Acute Cholangitis: Symptoms, Causes, Treatments, and Prognosis – Moosmosis
- Pingback: Biology Major vs Chemistry Major vs Biochemistry Major in College – Moosmosis
Very high level and comprehensive post! Thanks for visiting my blog. I can’t use the “like” buttons on your blog.
Thank you so much! You have a great blog too! Have a nice day!
- Pingback: The Modified Barium Swallow Study: Exploring Anatomy, Procedure, Diagnoses, and Medical Findings – Moosmosis
- Pingback: Top 70 Medical Abbreviations in Medical Record Notes and Sample History & Physical Exam Note – Moosmosis
- Pingback: Inflammatory Bowel Diseases – Crohn’s Disease vs. Ulcerative Colitis: Symptoms, Diagnosis, Treatments, and Prognosis – Moosmosis
Wonderful article on heart blood flow!
Thank you so much for your kind words, Susie!
- Pingback: Urinary Tract Infections (UTI) – Cystitis vs Pyelonephritis: Symptoms, Diagnosis, Treatments, and Prognosis – Moosmosis
This is so helpful! Made heart blood flow steps easy to understand, thanks!
You’re very welcome! So glad you found it helpful
- Pingback: Types of Femoral Fractures: Femoral Head, Neck, Shaft, and Distal Femoral Fractures -Anatomy, Mechanisms, Treatment, and Prognosis – Moosmosis
- Pingback: Happy New Year and New Year Resolutions: 25 Health and Wellness Tips for a Healthier and Happier New Year – Moosmosis
Amazing! Excellent article on heart blood flow steps.
Thank you so much! Have an excellent day!! 😄
Excellent! So helpful
Thank you so much! We’re happy you found it helpful! ❤️❤️❤️
Thank you!! We love you too dear reader!! ❤️❤️❤️
Thanks for signing on to my blog – as an instructor in anatomy and physiology for medical students I think this blog is very helpful!
Thank you so much!!! ❤️ Your blog is very helpful and wonderful too! We hope you have a great day!
- Pingback: Circulatory System 101: Advantages and Disadvantages of Cardiac MRI versus Cardiac CT [MCAT, USMLE, Biology, Medicine] – Moosmosis
- Pingback: Types of Stroke – Ischemic Stroke vs Hemorrhagic Stroke: Symptoms, Diagnosis, Treatment, and Prognosis – Moosmosis
- Pingback: NBME Internal Medicine Form 6: Notes and Explanations for the Answers – Moosmosis
- Pingback: Top 25 Nutritious Foods to Eat for Health, Energy, and Wellness – Moosmosis
- Pingback: NBME Internal Medicine Form 4: Notes and Explanations for the Answers – Moosmosis
- Pingback: Top 20 Super Foods to Eat for a Healthy Long Life – Moosmosis
- Pingback: Top 20 Health and Wellness Tips for Successful Weight Loss and a Healthy Lifestyle – Moosmosis
- Pingback: NBME Internal Medicine Form 5: Notes and Explanations for the Answers – Moosmosis
- Pingback: Fueling Vitality: Top 25 Foods for Energy, Mood Boosting, and Happiness – Moosmosis
Leave a comment Cancel reply
Thank you for visiting.
- 2,652,732 Lifelong Learners!
Join Moosmosis and our wonderful lifelong learning community today! Free lessons and student opportunities
Email Address:
Subscribe for Free!
Today’s Top Posts
Our Community
Choose a Language
Please Like to Support!
- Already have a WordPress.com account? Log in now.
- Subscribe Subscribed
- Copy shortlink
- Report this content
- View post in Reader
- Manage subscriptions
- Collapse this bar
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
The Heart: Anatomy, Function, and Conditions
Four chambers and four valves in your heart pump blood through your body
Associated Conditions
The heart—the primary organ of the cardiovascular system—is a muscle that contracts regularly, via a natural pacemaker that produces electrical impulses . The heartbeat drives the transport of blood throughout the body, which provides oxygen and nutrients to all the body’s cells, tissues, and organs. Although the heart is a complicated organ, in essence, it is a pump that continuously works to circulate blood throughout the body.
PIXOLOGICSTUDIO / Getty Images
The heart is an organ that weighs approximately 350 grams (less than one pound). It’s nearly the size of an adult’s clenched fist.
It's located in the thorax (chest)—between the lungs —and extends downward between the second and fifth intercostal (between the ribs). It is fairly protected from many types of trauma because it is surrounded by the rib cage.
Together, the heart and the circulatory system comprise the cardiovascular system. The blood vessels carry the blood through a network of arteries , arterioles, and capillaries . Once the oxygen is absorbed by the tissues, blood is then returned to the heart via the veins .
Interestingly, if all of the blood vessels in the cardiovascular system were laid in a straight line—end-to-end—the total distance they would cover would be over 60,000 miles.
Blood Flow Through the Heart
The human heart is primarily comprised of four chambers. The two upper chambers are called the atria, the remaining two lower chambers are the ventricles.
The right and left sides of the heart are separated by a muscle called the “septum.” Both sides work together to efficiently circulate the blood.
Each chamber has its unique job in blood circulation:
- The right atrium: Receives oxygen-poor blood from the body, then pumps it to the right ventricle.
- Right ventricle: Pumps the deoxygenated blood to the lungs to receive oxygen.
- The left atrium: Receives the oxygenated blood from the lungs (via the pulmonary vein) and pumps it to the left ventricle.
- Left ventricle: The largest and most powerful of all the heart’s chambers pumps the oxygen-rich blood through the aorta (the largest artery in the body) to be circulated through the body’s arteries, arterioles, and capillaries to deliver oxygen to all the cells, tissues and organs throughout the body. Even though the walls of the left ventricle are only around a half-inch in thickness, the left ventricle has enough muscle power to push the blood out of the heart, through the aortic valve, and onto the rest of your body.
How Much Blood Is in the Average Adult’s Body?
An adult has approximately 1.2-1.5 gallons (or 10 units) of blood in their body. Blood is approximately 10% of an adult's weight.
The Heart Valves
Heart valves help control blood flow and direction.
Picture blood flowing from the atria to the ventricles. Once the ventricles are full, the mitral and tricuspid valves must close before the powerful contraction pumps out the blood. If the valves stay open, blood will be forced back up into the atria, instead of being sent out of the heart to circulate throughout the body.
Four heart valves function to regulate blood flow through the heart, these include:
- The tricuspid valve: Regulates the flow of blood between the right atrium and the right ventricle.
- The pulmonary valve: Controls the flow of blood from the right ventricle into the pulmonary arteries .
- The mitral valve: Regulates the flow of oxygenated blood from the left atrium into the left ventricle.
- The aortic valve: Allows oxygenated blood to flow from the left ventricle into the aorta to be circulated out of the body to all the tissues.
The heart is comprised of layers, including:
- The myocardium: The layer made up of cardiac muscle cell.
- The endocardium : The inner lining.
The heart is encased in a membrane called the pericardium. The pericardium’s job is to anchor the heart and keep it from overexpanding.
The heart’s location is in the middle of the thorax (chest), slightly to the left, and behind the sternum (breastbone). The space that houses the heart is called the mediastinum . Inside of the mediastinum, the heart is separated from other structures by the pericardium.
The backside of the heart is positioned near the vertebrae, the front side sits behind the sternum (breastbone). Attached to the superior (upper) portion of the heart are the great veins (the superior vena cava and the inferior vena cava) and the great arteries (the aorta and pulmonary trunk).
Anatomical Variations
There are many genetic and congenital defects that can affect the heart.
Examples of anomalies in adults include:
- Familial [hereditary] dilated cardiomyopathy: An inherited condition that causes the heart muscle to weaken and become thin. Familial dilated cardiomyopathy can lead to heart failure (HF), which is a condition in which the heart cannot effectively pump blood.
- Familial Hypercholesterolemia: An inherited disease that causes hypercholesterolemia (high blood cholesterol). This inherited condition can lead to coronary heart disease.
- Familial hypertrophic cardiomyopathy: A hereditary heart disorder involving thickening of part or all of the heart muscle, which can raise the pressure inside the heart’s chamber and interfere with normal blood flow from the heart. This makes the heart work harder to circulate the blood. In severe instances, hypertrophic cardiomyopathy can cause death.
The average heart rate is around 75 beats (contractions) per minute. The heart beats nearly:
- 108,000 times each day
- 37 million times per year
- 3 billion times in an average lifetime
There are many medical conditions that affect the heart.
Atherosclerosis is perhaps the most common condition that impacts the heart. Coronary artery disease (CAD) is atherosclerosis of the arteries that supply oxygen to the heart muscle. It is the leading cause of death and illnesses across the globe.
Cardiac arrhythmias are conditions in which the normal rate or rhythm of the heartbeat is disrupted.
Heart Failure (HF)
Heart failure (HF) is a commonly misunderstood term. Unlike the name suggests, the heart does not completely stop beating when a person has heart failure. Rather, it is not able to efficiently pump the blood to supply adequate oxygen and nutrients to the body’s cells, tissues, and organs.
Heart failure is not a single disorder—it's a continuum of signs and symptoms that can develop quickly, or can be chronic.
Endocarditis
Endocarditis is an infection or inflammation of the inner surface of the heart; this type of infection involves the heart valves. The infections can be hard to clear and continually seed the bacteria in the blood, leading to a serious, uncontrolled systemic infection.
The infections can permanently damage valves and can lead to heart failure.
Pericarditis
Pericarditis is inflammation of the pericardium (the membranous sac that encases the heart). Pericarditis can be caused by an infection, but not all pericarditis is infection-related. It can cause excess fluid accumulation, called pericardial effusion.
Pericarditis can impact a person at any age, but it is more common in men aged 16 to 65.
Verywell / Emily Roberts
Tests commonly ordered to diagnose cardiac and vascular disease include:
Physical Examination
Before your physical examination, your healthcare provider will take a thorough history to assess symptoms of heart disease.
The healthcare provider may ask about symptoms such as:
- Trouble breathing
- Exercise intolerance
- Any type of chest pain, such as angina
- Pain, numbness, or weakness in the arms or other extremities
- Fluttering in the chest
- Fainting or dizziness
- Severe fatigue
- Weight loss
A physical examination can detect signs and symptoms of cardiovascular disease.
Physical examination abnormalities that can indicate heart disease include:
- Poor circulation in the extremities
- An irregular heartbeat
- Changes in heart or lung sounds
- High or low blood pressure
Blood Tests
Blood tests can help diagnose some of the problems that can lead to heart disease.
Examples of blood tests you may have during an evaluation for heart disease include:
- A lipid profile
- Blood glucose levels
- A complete blood count
Non-Invasive Imaging Tests
Non-invasive imaging tests can include:
- Echocardiogram : Sometimes referred to as an “echo,” is an ultrasound of the heart.
- Doppler ultrasound: A specific type of ultrasound that uses a special device to look at the arteries or the veins and the velocity of blood flowing through the imaged vessel.
- Electrocardiogram (EKG or ECG) : A common test performed to evaluate the rhythm, rate, and activity of the heart.
- Stress EKG (exercise or treadmill test) : A test utilized to evaluate the blood supply in the coronary arteries when the heart is working (due to physical activity).
Emily Roberts / Verywell
Invasive Tests
An invasive test is one that is usually performed during a surgical procedure. This includes a cardiac catheterization, which is when a thin, hollow tube—called a catheter—is inserted into a large blood vessel that leads to the heart. A contrast dye is injected through the catheter, which serves to illuminate the area so that X-rays can be taken. Taking images of the blood vessels during cardiac catheterization is referred to as an angiography (picture of a blood vessel).
Texas Heart Institute. Heart anatomy .
Jarvis S, Saman S. Cardiac system 1: Anatomy and physiology . Nursing Times [online]. 2018;114(2):34-37.
American Red Cross. Whole blood and what it contains .
University of Rochester Medical Center. Anatomy and function of the heart valves .
OpenStax. Anatomy and physiology 19.1 heart anatomy .
Penn Medicine. All in the family: 3 common inherited heart diseases .
Ellulu MS, Patimah I, Khaza’ai H, Rahmat A, Abed Y, Ali F. Atherosclerotic cardiovascular disease: a review of initiators and protective factors. Inflammopharmacol. 2016;24(1):1-10. doi:10.1007/s10787-015-0255-y
American Heart Association. Types of heart failure .
Cleveland Clinic. Pericarditis .
UCSF Health. Diagnosing heart disease.
American Heart Association. What is cardiac catheterization .
By Sherry Christiansen Christiansen is a medical writer with a healthcare background. She has worked in the hospital setting and collaborated on Alzheimer's research.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Physiology, cardiovascular hemodynamics.
Joshua D. Pollock ; Ian V. Murray ; Stephen J. Bordes ; Amgad N. Makaryus .
Affiliations
Last Update: March 13, 2023 .
- Introduction
Hemodynamics ultimately begins with the heart which supplies the driving force for all blood flow in the body. Cardiac output propels blood through the arteries and veins as a function of ventricular contraction. Ventricular motion results from the shortening of cardiac myocytes concentrically. This squeezing motion is translated into the cardiac output, which is a function of both heart rate and ejection fraction (the starting volume after diastolic filling minus the final ventricular volume after systole). Hemodynamics represents the governing principles of this blood flow and its behavior in the blood vessels.
When considering physiologic blood flow, it is simplest to think of the blood flowing through pipes or cylinders, and from that basic understanding add in the complexities. Normal blood flow can be thought of as simple laminar flow in most instances (for exceptions, see pathology). A visualization of laminar flow can be seen in the figure below. Laminar flow is characterized by a gradient of flow lines representing different blood velocities at different locations in the tube. The reason for these differences in blood flow velocity is wall stress (a type of shear stress). When a fluid, in this case, blood, flows through a pipe, friction exists between the fluid and the wall of the tube. This friction decreases the velocity of the blood closest to the wall (hence the shorter lines on the diagram closer to the tube wall). Another factor within the realm of laminar flow is the Reynolds number. The Reynolds number is a value for a given fluid to model the conditions at which that fluid will remain in laminar flow. A variable affecting the Re number of a fluid, in this case, blood viscosity. In the case of blood, it is a product of its constituents: cells and protein. The Reynolds number considers the velocity of flow and external factors that might contribute to turbulent flow. [1] [2] [3]
The following is the equation for the Reynolds number, (where Re is the Reynolds number, ρ is the density, V is velocity, D is the diameter of the cylinder, and μ is the viscosity:
- Re= ρVD/μ
Turbulence is more likely to develop at a high Re number.
One of the most significant wrinkles in this simplified model is the principle of blood vessel compliance. Compliance is the amount of distention for a given amount of pressure. As such, when blood is pumped from the heart, the blood vessels do not act as complete rigid tubes. They expand and contract with the pressure changes due to their elastic nature.
Compliance can be modeled with the following equation, where C is the compliance, V is volume, and P is pressure:
- C = ΔV/ΔP
Essentially, the greater the change in volume for a given pressure change, the greater the compliance. Physiologically, veins have greater compliance than arteries under normal conditions. This is because arteries are thicker and more muscular than veins (less distensible). The result is a high-pressure system within the arteries and a lower resistance (low-pressure system) in the veins.
Pressure differences in the form of cardiac output and vessel compliance create blood flow.
This governing principle is quantified by Ohm’s law of fluid flow which states the following where flow (Q) is equal to the pressure gradient (ΔP) divided by resistance (R):
- Q = ΔP/R
Physiologically, this means that blood flow is equal to the change in pressure divided by systemic resistance. In other words, to increase blood flow, one could either increase the pressure difference (e.g., increased cardiac force) or decrease the systemic vascular resistance (e.g., dilate blood vessels). Blood vessel resistance can be thought of as how difficult it is to pass blood through a given set of vessels. Intuitively, the size and shape of the blood vessel can alter the ease of blood flow. A helpful analogy for blood flow resistance is motor vehicle traffic. The cars represent the ease of blood flowing through a blood vessel. If we made the road narrower or add a toll booth, fewer cars can pass a given point for a set amount of time. This is analogous to making the blood vessel narrower (blood vessel diameter is a factor for resistance) which increases resistance. The total resistance for a continuous blood vessel or group of vessels in series (one after another) is simply represented by the following, where R1 represents a section of a blood vessel with a given resistance:
- Rtot (total resistance) = R1 + R2 + R3 (and so on for increasing number of vessels)
However, when blood vessels diverge and create multiple paths with a common destination, we say these blood vessels are in parallel and resistance takes on the equation 1/Rtot = 1/R1 + 1/R2 + 1/R3 and so on. Testing this equation with some sample values will result in a total resistance less than the sum of its parts. Here again, the car analogy is helpful. Where adding blood vessels in series increasing the resistance (i.e., adding toll booths one after another on the road), adding blood vessels in parallel becomes analogous to opening multiple lanes. Within the analogy, it is easier to drive when there are several toll booths open (in parallel). A physiologic example of this phenomenon can be observed in capillary beds, where although blood vessels are very small, they are arranged in parallel and offer comparatively low resistance to flow.
- Pathophysiology
One can argue that virtually every cardiovascular pathology augments normal hemodynamics in some form or another. However, some examples very clearly illustrate the physiologic principles explained above. One such example is age-related vascular disease. While researchers still debate the exact mechanism for this disease, the result is a loss of normal endothelial compliance in the blood vessels. This change causes blood vessels to act stiffer and less distensible with the pressures of systole (where the heart pushes the blood into the blood vessels creating pressure). The main result of this seemingly minor change is an increase in blood pressure. By increasing the blood pressure, more load is placed on the heart, predisposing it to further compromise in the form of hypertrophy (i.e., the heart gets thicker in an attempted push against this greater vascular resistance) or direct vascular damage from the increased pressure (e.g., hemorrhagic stroke). [1] [2] [3]
While age is one common cause of hypertension, several others bear mentioning. Many endogenous substances act as vasoconstrictors and exert their effects to modify blood pressure. Angiotensin (I and II) and aldosterone are such components. Along with renin, these form the primary constituents of the renin-angiotensin-aldosterone system (RAAS). Aberrations in this pathway lead to elevated levels of these substances, especially angiotensin II and aldosterone, in the blood, which raises the blood pressure through increased vascular resistance (i.e., blood vessel constriction). Aldosterone is the end effector of this pathway, and in addition to vasoconstriction, causes reabsorption of sodium in the distal tubule of the kidney, which increases blood volume and blood pressure. This system exists to maintain normal pressure in times of fluid loss or hemorrhage, but pathological alterations are possible. Renal artery stenosis is one such case. Stenosis results in decreased blood flow to the kidney, subsequently increasing renin release. Increased renin leads to a cascade, resulting in elevated aldosterone (and angiotensin II). The vasoconstriction and salt retention that follows result in hypertension, which is resistant to typical modes of treatment.
Stress and anxiety also can contribute to elevated blood pressure. This effect takes place in the form of excess catecholamines (e.g., norepinephrine and epinephrine), which increase cardiac contractility, which increases flow and selectively constricts blood vessels, which increases vascular resistance. Essential hypertension is one example where hypertension seems to exist without any easily identifiable cause. These patients may have a family history of similar early elevations in blood pressure, but ultimately, this is a diagnosis of exclusion after ruling out other causes.
Regardless of the source, hypertension has important consequences for the body. In addition to cardiac remodeling, there are reflex changes to the blood vessels from the greater pressure. The arterioles, which are the smallest arterial blood vessels before the capillary beds, reflexively constrict to protect the relatively delicate capillary beds from these damaging forces. This reflex constriction increases resistance, which spares the capillaries, but also further increases pressure (remembering that P = RQ, so an increase in resistance will increase pressure for a given flow).
Another example of aberrant hemodynamics is pulmonary hypertension. [4] Pulmonary hypertension results from one or a combination of abnormal flow, pulmonary blood vessel constriction, or hypoxia. These mechanisms are further delineated by the classes of pulmonary hypertension outlined below:
- Class 1 - Idiopathic/heritable
- Class 2 - Secondary to left heart failure
- Class 3 - Secondary to lung disease and hypoxia
- Class 4 - Thromboembolic (pulmonary embolisms)
- Class 5 - Unclear etiology
The first four classes each illustrate a significant mechanism for increased resistance of a vascular system and an especially dangerous one in this particular pathology. The idiopathic or heritable disease can result in fibrosis or constriction of the blood vessels, but this category is very broad and includes toxins or defects in the body's ability to produce vasodilatory substances. These factors can result in the narrowing of the blood vessels and increased vascular resistance. Left heart failure results in a decrease in the forward blood flow and marked vascular congestion. Intuitively, this increases resistance in a similar way a large blockage in a blood vessel might. Lung disease and hypoxia illustrate an important physiologic point; the pulmonary arterioles are responsive to oxygen (resulting in vasodilation). Without oxygen, there is marked vasoconstriction, which increases vascular resistance and increases pressure (velocity increases to maintain net flow). The thromboembolic disease results in decreased pathways for pulmonary blood flow. As a result, the net resistance of the system increases. Recall that as parallel pathways are created, the net resistance becomes reduced (the emboli act in opposition to this). The increased pressure from the alveolar damage, among other mechanisms, results in significant morbidity and mortality for patients without a reversible cause of this condition. [5]
- Clinical Significance
A common application of these principles is the measurement of blood pressure. While automated machines are quickly replacing manual blood pressure readings as a rapid clinical tool, manual blood pressure is widely considered to be more reliable. Taking a manual blood pressure involves filling an inflatable cuff that is fastened above the systolic blood pressure to constrict the patient’s arm and slowly releasing the pressure while auscultating the main artery constricted. The practitioner is taking advantage of two key points to gauge the systolic and diastolic blood pressures. The first is when the sound of turbulent flow begins (Korsakoff sounds), and this audible heartbeat represents the first time blood flow overcomes the pressure of the cuff (the practitioner has been slowly lowering the cuff pressure while the blood pressure is relatively constant for a given beat). This blood flow is heard as a rushing noise because the increased velocity leads to non-laminar (turbulent) flow. The turbulent flow and audible beats continue to the next critical point, where the blood returns to laminar flow and the audible turbulent flow cases. The pressure at which this takes place represents the diastolic blood pressure. [6] [7]
Cardiac auscultation takes advantage of similar principles as the blood pressure measurement previously described. The foundation of both is the principle that turbulent flow may be auscultated, and laminar flow is essentially silent for our purposes. When auscultating a healthy heart, two beats are heard representing the closure of the mitral and tricuspid valve (S1) and then the aortic and pulmonic valves (S2). Under physiologic conditions, those are the only sounds heard, but pathologic valves or defects in the cardiac muscle can create extra noises. These noises are a result of the blood flow being disturbed, and as already mentioned while discussing blood pressure measurement, this can result in an audible rush of turbulent flow. Auscultated turbulent flow in cardiac examination represents murmurs and can help diagnose cardiac pathology.
Cardiovascular pharmacology is a massive topic, but a few principles are helpful when beginning to understand hemodynamics in a clinical context. One case is clinical blood pressure management. When treating blood pressure that is not related to an underlying condition (such as renal artery occlusion or pheochromocytoma), the primary goal is to decrease blood pressure to less than 130/80 in most of the population. These goals are achievable through medications that augment the variables previously discussed, namely systemic vascular resistance and cardiac contractility. While it is possible for certain drugs such as beta-blockers and non-dihydropyridine calcium channel blockers (verapamil and diltiazem) to decrease cardiac contractility, the majority of blood pressure medications target systemic vascular resistance. By decreasing systemic vascular resistance for a given cardiac output, the pressure decreases [remembering Q = ΔP/R, for flow (Q) to remain constant as resistance (R )goes down so must the pressure gradient (ΔP)]. Drugs such as ACE inhibitors and dihydropyridine calcium channel blockers (e.g., amlodipine) ultimately result in vasodilation and decreased systemic vascular resistance. Vasodilation also can be induced by nitrates to reduce cardiac preload in the case of angina.
Systemic vascular resistance also can be reversed by agents collectively referred to as vasopressors. This constricting of the blood vessels and the subsequent increase in resistance is valuable when the blood pressure drops to dangerous levels. A clinical example of this phenomenon may present in anaphylactic shock, where vasodilation decreases blood pressure to dangerous levels. Epinephrine can reverse this effect by increasing systemic vascular resistance.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
A depiction of laminar flow in a cross section of a blood vessel. The red arrows represent blood flow velocity and the black lines represent blood vessel walls. Adapted from hyperphysics.edu
Disclosure: Joshua Pollock declares no relevant financial relationships with ineligible companies.
Disclosure: Ian Murray declares no relevant financial relationships with ineligible companies.
Disclosure: Stephen Bordes declares no relevant financial relationships with ineligible companies.
Disclosure: Amgad Makaryus declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Pollock JD, Murray IV, Bordes SJ, et al. Physiology, Cardiovascular Hemodynamics. [Updated 2023 Mar 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Myocardial and ventricular function. Part II: Intact heart. [Herz. 1981] Myocardial and ventricular function. Part II: Intact heart. Strobeck JE, Sonnenblick EH. Herz. 1981 Oct; 6(5):275-87.
- Reduced First-Phase Ejection Fraction and Sustained Myocardial Wall Stress in Hypertensive Patients With Diastolic Dysfunction: A Manifestation of Impaired Shortening Deactivation That Links Systolic to Diastolic Dysfunction and Preserves Systolic Ejection Fraction. [Hypertension. 2017] Reduced First-Phase Ejection Fraction and Sustained Myocardial Wall Stress in Hypertensive Patients With Diastolic Dysfunction: A Manifestation of Impaired Shortening Deactivation That Links Systolic to Diastolic Dysfunction and Preserves Systolic Ejection Fraction. Gu H, Li Y, Fok H, Simpson J, Kentish JC, Shah AM, Chowienczyk PJ. Hypertension. 2017 Apr; 69(4):633-640. Epub 2017 Feb 21.
- Review [Hemodynamic guidelines in the treatment of acute myocardial infarction by means of vasodilators]. [Acta Med Austriaca Suppl. 1979] Review [Hemodynamic guidelines in the treatment of acute myocardial infarction by means of vasodilators]. Zilcher H. Acta Med Austriaca Suppl. 1979; 15:1-34.
- Determinants of exercise capacity in patients with coronary artery disease and mild to moderate systolic dysfunction. Role of heart rate and diastolic filling abnormalities. [Eur Heart J. 1996] Determinants of exercise capacity in patients with coronary artery disease and mild to moderate systolic dysfunction. Role of heart rate and diastolic filling abnormalities. Lele SS, Macfarlane D, Morrison S, Thomson H, Khafagi F, Frenneaux M. Eur Heart J. 1996 Feb; 17(2):204-12.
- Review Haemodynamic basis for the development of left ventricular failure in systolic hypertension and for its logical therapy. [J Hypertens. 1995] Review Haemodynamic basis for the development of left ventricular failure in systolic hypertension and for its logical therapy. Westerhof N, O'Rourke MF. J Hypertens. 1995 Sep; 13(9):943-52.
Recent Activity
- Physiology, Cardiovascular Hemodynamics - StatPearls Physiology, Cardiovascular Hemodynamics - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
19.1 Heart Anatomy
Learning objectives.
By the end of this section, you will be able to:
- Describe the location and position of the heart within the body cavity
- Describe the internal and external anatomy of the heart
- Identify the tissue layers of the heart
- Relate the structure of the heart to its function as a pump
- Compare systemic circulation to pulmonary circulation
- Identify the veins and arteries of the coronary circulation system
- Trace the pathway of oxygenated and deoxygenated blood thorough the chambers of the heart
The vital importance of the heart is obvious. If one assumes an average rate of contraction of 75 contractions per minute, a human heart would contract approximately 108,000 times in one day, more than 39 million times in one year, and nearly 3 billion times during a 75-year lifespan. Each of the major pumping chambers of the heart ejects approximately 70 mL blood per contraction in a resting adult. This would be equal to 5.25 liters of fluid per minute and approximately 14,000 liters per day. Over one year, that would equal 10,000,000 liters or 2.6 million gallons of blood sent through roughly 60,000 miles of vessels. In order to understand how that happens, it is necessary to understand the anatomy and physiology of the heart.
Location of the Heart
The human heart is located within the thoracic cavity, medially between the lungs in the space known as the mediastinum. Figure 19.2 shows the position of the heart within the thoracic cavity. Within the mediastinum, the heart is separated from the other mediastinal structures by a tough membrane known as the pericardium, or pericardial sac, and sits in its own space called the pericardial cavity . The dorsal surface of the heart lies near the bodies of the vertebrae, and its anterior surface sits deep to the sternum and costal cartilages. The great veins, the superior and inferior venae cavae, and the great arteries, the aorta and pulmonary trunk, are attached to the superior surface of the heart, called the base. The base of the heart is located at the level of the third costal cartilage, as seen in Figure 19.2 . The inferior tip of the heart, the apex, lies just to the left of the sternum between the junction of the fourth and fifth ribs near their articulation with the costal cartilages. The right side of the heart is deflected anteriorly, and the left side is deflected posteriorly. It is important to remember the position and orientation of the heart when placing a stethoscope on the chest of a patient and listening for heart sounds, and also when looking at images taken from a midsagittal perspective. The slight deviation of the apex to the left is reflected in a depression in the medial surface of the inferior lobe of the left lung, called the cardiac notch .
Everyday Connection
The position of the heart in the torso between the vertebrae and sternum (see Figure 19.2 for the position of the heart within the thorax) allows for individuals to apply an emergency technique known as cardiopulmonary resuscitation (CPR) if the heart of a patient should stop. By applying pressure with the flat portion of one hand on the sternum in the area between the line at T4 and T9 ( Figure 19.3 ), it is possible to manually compress the blood within the heart enough to push some of the blood within it into the pulmonary and systemic circuits. This is particularly critical for the brain, as irreversible damage and death of neurons occur within minutes of loss of blood flow. Current standards call for compression of the chest at least 5 cm deep and at a rate of 100 compressions per minute, a rate equal to the beat in “Staying Alive,” recorded in 1977 by the Bee Gees. If you are unfamiliar with this song, a version is available on www.youtube.com. At this stage, the emphasis is on performing high-quality chest compressions, rather than providing artificial respiration. CPR is generally performed until the patient regains spontaneous contraction or is declared dead by an experienced healthcare professional.
When performed by untrained or overzealous individuals, CPR can result in broken ribs or a broken sternum, and can inflict additional severe damage on the patient. It is also possible, if the hands are placed too low on the sternum, to manually drive the xiphoid process into the liver, a consequence that may prove fatal for the patient. Proper training is essential. This proven life-sustaining technique is so valuable that virtually all medical personnel as well as concerned members of the public should be certified and routinely recertified in its application. CPR courses are offered at a variety of locations, including colleges, hospitals, the American Red Cross, and some commercial companies. They normally include practice of the compression technique on a mannequin.
Interactive Link
Visit the American Heart Association website to help locate a course near your home in the United States. There are also many other national and regional heart associations that offer the same service, depending upon the location.
Shape and Size of the Heart
The shape of the heart is similar to a pinecone, rather broad at the superior surface and tapering to the apex (see Figure 19.2 ). A typical heart is approximately the size of your fist: 12 cm (5 in) in length, 8 cm (3.5 in) wide, and 6 cm (2.5 in) in thickness. Given the size difference between most members of the sexes, the weight of a female heart is approximately 250–300 grams (9 to 11 ounces), and the weight of a male heart is approximately 300–350 grams (11 to 12 ounces). The heart of a well-trained athlete, especially one specializing in aerobic sports, can be considerably larger than this. Cardiac muscle responds to exercise in a manner similar to that of skeletal muscle. That is, exercise results in the addition of protein myofilaments that increase the size of the individual cells without increasing their numbers, a concept called hypertrophy. Hearts of athletes can pump blood more effectively at lower rates than those of nonathletes. Enlarged hearts are not always a result of exercise; they can result from pathologies, such as hypertrophic cardiomyopathy . The cause of an abnormally enlarged heart muscle is unknown, but the condition is often undiagnosed and can cause sudden death in apparently otherwise healthy young people.
Chambers and Circulation through the Heart
The human heart consists of four chambers: The left side and the right side each have one atrium and one ventricle . Each of the upper chambers, the right atrium (plural = atria) and the left atrium, acts as a receiving chamber and contracts to push blood into the lower chambers, the right ventricle and the left ventricle. The ventricles serve as the primary pumping chambers of the heart, propelling blood to the lungs or to the rest of the body.
There are two distinct but linked circuits in the human circulation called the pulmonary and systemic circuits. Although both circuits transport blood and everything it carries, we can initially view the circuits from the point of view of gases. The pulmonary circuit transports blood to and from the lungs, where it picks up oxygen and delivers carbon dioxide for exhalation. The systemic circuit transports oxygenated blood to virtually all of the tissues of the body and returns relatively deoxygenated blood and carbon dioxide to the heart to be sent back to the pulmonary circulation.
The right ventricle pumps deoxygenated blood into the pulmonary trunk , which leads toward the lungs and bifurcates into the left and right pulmonary arteries . These vessels in turn branch many times before reaching the pulmonary capillaries , where gas exchange occurs: Carbon dioxide exits the blood and oxygen enters. The pulmonary trunk arteries and their branches are the only arteries in the post-natal body that carry relatively deoxygenated blood. Highly oxygenated blood returning from the pulmonary capillaries in the lungs passes through a series of vessels that join together to form the pulmonary veins —the only post-natal veins in the body that carry highly oxygenated blood. The pulmonary veins conduct blood into the left atrium, which pumps the blood into the left ventricle, which in turn pumps oxygenated blood into the aorta and on to the many branches of the systemic circuit. Eventually, these vessels will lead to the systemic capillaries, where exchange with the tissue fluid and cells of the body occurs. In this case, oxygen and nutrients exit the systemic capillaries to be used by the cells in their metabolic processes, and carbon dioxide and waste products will enter the blood.
The blood exiting the systemic capillaries is lower in oxygen concentration than when it entered. The capillaries will ultimately unite to form venules, joining to form ever-larger veins, eventually flowing into the two major systemic veins, the superior vena cava and the inferior vena cava , which return blood to the right atrium. The blood in the superior and inferior venae cavae flows into the right atrium, which pumps blood into the right ventricle. This process of blood circulation continues as long as the individual remains alive. Understanding the flow of blood through the pulmonary and systemic circuits is critical to all health professions ( Figure 19.4 ).
Membranes, Surface Features, and Layers
Our exploration of more in-depth heart structures begins by examining the membrane that surrounds the heart, the prominent surface features of the heart, and the layers that form the wall of the heart. Each of these components plays its own unique role in terms of function.
The membrane that directly surrounds the heart and defines the pericardial cavity is called the pericardium or pericardial sac . It also surrounds the “roots” of the major vessels, or the areas of closest proximity to the heart. The pericardium, which literally translates as “around the heart,” consists of two distinct sublayers: the sturdy outer fibrous pericardium and the inner serous pericardium. The fibrous pericardium is made of tough, dense connective tissue that protects the heart and maintains its position in the thorax. The more delicate serous pericardium consists of two layers: the parietal pericardium, which is fused to the fibrous pericardium, and an inner visceral pericardium, or epicardium , which is fused to the heart and is part of the heart wall. The pericardial cavity, filled with lubricating serous fluid, lies between the epicardium and the pericardium.
In most organs within the body, visceral serous membranes such as the epicardium are microscopic. However, in the case of the heart, it is not a microscopic layer but rather a macroscopic layer, consisting of a simple squamous epithelium called a mesothelium , reinforced with loose, irregular, or areolar connective tissue that attaches to the pericardium. This mesothelium secretes the lubricating serous fluid that fills the pericardial cavity and reduces friction as the heart contracts. Figure 19.5 illustrates the pericardial membrane and the layers of the heart.
Disorders of the...
Heart: cardiac tamponade.
If excess fluid builds within the pericardial space, it can lead to a condition called cardiac tamponade, or pericardial tamponade. With each contraction of the heart, more fluid—in most instances, blood—accumulates within the pericardial cavity. In order to fill with blood for the next contraction, the heart must relax. However, the excess fluid in the pericardial cavity puts pressure on the heart and prevents full relaxation, so the chambers within the heart contain slightly less blood as they begin each heart cycle. Over time, less and less blood is ejected from the heart. If the fluid builds up slowly, as in hypothyroidism, the pericardial cavity may be able to expand gradually to accommodate this extra volume. Some cases of fluid in excess of one liter within the pericardial cavity have been reported. Rapid accumulation of as little as 100 mL of fluid following trauma may trigger cardiac tamponade. Other common causes include myocardial rupture, pericarditis, cancer, or even cardiac surgery. Removal of this excess fluid requires insertion of drainage tubes into the pericardial cavity. Premature removal of these drainage tubes, for example, following cardiac surgery, or clot formation within these tubes are causes of this condition. Untreated, cardiac tamponade can lead to death.
Surface Features of the Heart
Inside the pericardium, the surface features of the heart are visible, including the four chambers. There is a superficial leaf-like extension of the atria near the superior surface of the heart, one on each side, called an auricle —a name that means “ear like”—because its shape resembles the external ear of a human ( Figure 19.6 ). Auricles are relatively thin-walled structures that can fill with blood and empty into the atria or upper chambers of the heart. You may also hear them referred to as atrial appendages. Also prominent is a series of fat-filled grooves, each of which is known as a sulcus (plural = sulci), along the superior surfaces of the heart. Major coronary blood vessels are located in these sulci. The deep coronary sulcus is located between the atria and ventricles. Located between the left and right ventricles are two additional sulci that are not as deep as the coronary sulcus. The anterior interventricular sulcus is visible on the anterior surface of the heart, whereas the posterior interventricular sulcus is visible on the posterior surface of the heart. Figure 19.6 illustrates anterior and posterior views of the surface of the heart.
The wall of the heart is composed of three layers of unequal thickness. From superficial to deep, these are the epicardium, the myocardium, and the endocardium (see Figure 19.5 ). The outermost layer of the wall of the heart is also the innermost layer of the pericardium, the epicardium, or the visceral pericardium discussed earlier.
The middle and thickest layer is the myocardium , made largely of cardiac muscle cells. It is built upon a framework of collagenous fibers, plus the blood vessels that supply the myocardium and the nerve fibers that help regulate the heart. It is the contraction of the myocardium that pumps blood through the heart and into the major arteries. The muscle pattern is elegant and complex, as the muscle cells swirl and spiral around the chambers of the heart. They form a figure 8 pattern around the atria and around the bases of the great vessels. Deeper ventricular muscles also form a figure 8 around the two ventricles and proceed toward the apex. More superficial layers of ventricular muscle wrap around both ventricles. This complex swirling pattern allows the heart to pump blood more effectively than a simple linear pattern would. Figure 19.7 illustrates the arrangement of muscle cells.
Although the ventricles on the right and left sides pump the same amount of blood per contraction, the muscle of the left ventricle is much thicker and better developed than that of the right ventricle. In order to overcome the high resistance required to pump blood into the long systemic circuit, the left ventricle must generate a great amount of pressure. The right ventricle does not need to generate as much pressure, since the pulmonary circuit is shorter and provides less resistance. Figure 19.8 illustrates the differences in muscular thickness needed for each of the ventricles.
The innermost layer of the heart wall, the endocardium , is joined to the myocardium with a thin layer of connective tissue. The endocardium lines the chambers where the blood circulates and covers the heart valves. It is made of simple squamous epithelium called endothelium , which is continuous with the endothelial lining of the blood vessels (see Figure 19.5 ).
Once regarded as a simple lining layer, recent evidence indicates that the endothelium of the endocardium and the coronary capillaries may play active roles in regulating the contraction of the muscle within the myocardium. The endothelium may also regulate the growth patterns of the cardiac muscle cells throughout life, and the endothelins it secretes create an environment in the surrounding tissue fluids that regulates ionic concentrations and states of contractility. Endothelins are potent vasoconstrictors and, in a normal individual, establish a homeostatic balance with other vasoconstrictors and vasodilators.
Internal Structure of the Heart
Recall that the heart’s contraction cycle follows a dual pattern of circulation—the pulmonary and systemic circuits—because of the pairs of chambers that pump blood into the circulation. In order to develop a more precise understanding of cardiac function, it is first necessary to explore the internal anatomical structures in more detail.
Septa of the Heart
The word septum is derived from the Latin for “something that encloses;” in this case, a septum (plural = septa) refers to a wall or partition that divides the heart into chambers. The septa are physical extensions of the myocardium lined with endocardium. Located between the two atria is the interatrial septum . Normally in an adult heart, the interatrial septum bears an oval-shaped depression known as the fossa ovalis , a remnant of an opening in the fetal heart known as the foramen ovale . The foramen ovale allowed blood in the fetal heart to pass directly from the right atrium to the left atrium, allowing some blood to bypass the pulmonary circuit. Within seconds after birth, a flap of tissue known as the septum primum that previously acted as a valve closes the foramen ovale and establishes the typical cardiac circulation pattern.
Between the two ventricles is a second septum known as the interventricular septum . Unlike the interatrial septum, the interventricular septum is normally intact after its formation during fetal development. It is substantially thicker than the interatrial septum, since the ventricles generate far greater pressure when they contract.
The septum between the atria and ventricles is known as the atrioventricular septum . It is marked by the presence of four openings that allow blood to move from the atria into the ventricles and from the ventricles into the pulmonary trunk and aorta. Located in each of these openings between the atria and ventricles is a valve , a specialized structure that ensures one-way flow of blood. The valves between the atria and ventricles are known generically as atrioventricular valves . The valves at the openings that lead to the pulmonary trunk and aorta are known generically as semilunar valves . The interventricular septum is visible in Figure 19.9 . In this figure, the atrioventricular septum has been removed to better show the bicuspid and tricuspid valves; the interatrial septum is not visible, since its location is covered by the aorta and pulmonary trunk. Since these openings and valves structurally weaken the atrioventricular septum, the remaining tissue is heavily reinforced with dense connective tissue called the cardiac skeleton , or skeleton of the heart. It includes four rings that surround the openings between the atria and ventricles, and the openings to the pulmonary trunk and aorta, and serve as the point of attachment for the heart valves. The cardiac skeleton also provides an important boundary in the heart electrical conduction system.
Heart: Heart Defects
One very common form of interatrial septum pathology is patent foramen ovale, which occurs when the septum primum does not close at birth, and the fossa ovalis is unable to fuse. The word patent is from the Latin root patens for “open.” It may be benign or asymptomatic, perhaps never being diagnosed, or in extreme cases, it may require surgical repair to close the opening permanently. As much as 20–25 percent of the general population may have a patent foramen ovale, but fortunately, most have the benign, asymptomatic version. Patent foramen ovale is normally detected by auscultation of a heart murmur (an abnormal heart sound) and confirmed by imaging with an echocardiogram. Despite its prevalence in the general population, the causes of patent ovale are unknown, and there are no known risk factors. In nonlife-threatening cases, it is better to monitor the condition than to risk heart surgery to repair and seal the opening.
Coarctation of the aorta is a congenital abnormal narrowing of the aorta that is normally located at the insertion of the ligamentum arteriosum, the remnant of the fetal shunt called the ductus arteriosus. If severe, this condition drastically restricts blood flow through the primary systemic artery, which is life threatening. In some individuals, the condition may be fairly benign and not detected until later in life. Detectable symptoms in an infant include difficulty breathing, poor appetite, trouble feeding, or failure to thrive. In older individuals, symptoms include dizziness, fainting, shortness of breath, chest pain, fatigue, headache, and nosebleeds. Treatment involves surgery to resect (remove) the affected region or angioplasty to open the abnormally narrow passageway. Studies have shown that the earlier the surgery is performed, the better the chance of survival.
A patent ductus arteriosus is a congenital condition in which the ductus arteriosus fails to close. The condition may range from severe to benign. Failure of the ductus arteriosus to close results in blood flowing from the higher pressure aorta into the lower pressure pulmonary trunk. This additional fluid moving toward the lungs increases pulmonary pressure and makes respiration difficult. Symptoms include shortness of breath (dyspnea), tachycardia, enlarged heart, a widened pulse pressure, and poor weight gain in infants. Treatments include surgical closure (ligation), manual closure using platinum coils or specialized mesh inserted via the femoral artery or vein, or nonsteroidal anti-inflammatory drugs to block the synthesis of prostaglandin E2, which maintains the vessel in an open position. If untreated, the condition can result in congestive heart failure.
Septal defects are not uncommon in individuals and may be congenital or caused by various disease processes. Tetralogy of Fallot is a congenital condition that may also occur from exposure to unknown environmental factors; it occurs when there is an opening in the interventricular septum caused by blockage of the pulmonary trunk, normally at the pulmonary semilunar valve. This allows blood that is relatively low in oxygen from the right ventricle to flow into the left ventricle and mix with the blood that is relatively high in oxygen. Symptoms include a distinct heart murmur, low blood oxygen percent saturation, dyspnea or difficulty in breathing, polycythemia, broadening (clubbing) of the fingers and toes, and in children, difficulty in feeding or failure to grow and develop. It is the most common cause of cyanosis following birth. The term “tetralogy” is derived from the four components of the condition, although only three may be present in an individual patient: pulmonary infundibular stenosis (rigidity of the pulmonary valve), overriding aorta (the aorta is shifted above both ventricles), ventricular septal defect (opening), and right ventricular hypertrophy (enlargement of the right ventricle). Other heart defects may also accompany this condition, which is typically confirmed by echocardiography imaging. Tetralogy of Fallot occurs in approximately 400 out of one million live births. Normal treatment involves extensive surgical repair, including the use of stents to redirect blood flow and replacement of valves and patches to repair the septal defect, but the condition has a relatively high mortality. Survival rates are currently 75 percent during the first year of life; 60 percent by 4 years of age; 30 percent by 10 years; and 5 percent by 40 years.
In the case of severe septal defects, including both tetralogy of Fallot and patent foramen ovale, failure of the heart to develop properly can lead to a condition commonly known as a “blue baby.” Regardless of normal skin pigmentation, individuals with this condition have an insufficient supply of oxygenated blood, which leads to cyanosis, a blue or purple coloration of the skin, especially when active.
Septal defects are commonly first detected through auscultation, listening to the chest using a stethoscope. In this case, instead of hearing normal heart sounds attributed to the flow of blood and closing of heart valves, unusual heart sounds may be detected. This is often followed by medical imaging to confirm or rule out a diagnosis. In many cases, treatment may not be needed. Some common congenital heart defects are illustrated in Figure 19.10 .
Right Atrium
The right atrium serves as the receiving chamber for blood returning to the heart from the systemic circulation. The two major systemic veins, the superior and inferior venae cavae, and the large coronary vein called the coronary sinus that drains the heart myocardium empty into the right atrium. The superior vena cava drains blood from regions superior to the diaphragm: the head, neck, upper limbs, and the thoracic region. It empties into the superior and posterior portions of the right atrium. The inferior vena cava drains blood from areas inferior to the diaphragm: the lower limbs and abdominopelvic region of the body. It, too, empties into the posterior portion of the atria, but inferior to the opening of the superior vena cava. Immediately superior and slightly medial to the opening of the inferior vena cava on the posterior surface of the atrium is the opening of the coronary sinus. This thin-walled vessel drains most of the coronary veins that return systemic blood from the heart. The majority of the internal heart structures discussed in this and subsequent sections are illustrated in Figure 19.9 .
While the bulk of the internal surface of the right atrium is smooth, the depression of the fossa ovalis is medial, and the anterior surface demonstrates prominent ridges of muscle called the pectinate muscles . The right auricle also has pectinate muscles. The left atrium does not have pectinate muscles except in the auricle.
The atria receive venous blood on a nearly continuous basis, preventing venous flow from stopping while the ventricles are contracting. While most ventricular filling occurs while the atria are relaxed, they do demonstrate a contractile phase and actively pump blood into the ventricles just prior to ventricular contraction. The opening between the atrium and ventricle is guarded by the tricuspid valve.

Right Ventricle
The right ventricle receives blood from the right atrium through the tricuspid valve. Each flap of the valve is attached to strong strands of connective tissue, the chordae tendineae , literally “tendinous cords,” or sometimes more poetically referred to as “heart strings.” There are several chordae tendineae associated with each of the flaps. They are composed of approximately 80 percent collagenous fibers with the remainder consisting of elastic fibers and endothelium. They connect each of the flaps to a papillary muscle that extends from the inferior ventricular surface. There are three papillary muscles in the right ventricle, called the anterior, posterior, and septal muscles, which correspond to the three sections of the valves.
When the myocardium of the ventricle contracts, pressure within the ventricular chamber rises. Blood, like any fluid, flows from higher pressure to lower pressure areas, in this case, toward the pulmonary trunk and the atrium. To prevent any potential backflow, the papillary muscles also contract, generating tension on the chordae tendineae. This prevents the flaps of the valves from being forced into the atria and regurgitation of the blood back into the atria during ventricular contraction. Figure 19.11 shows papillary muscles and chordae tendineae attached to the tricuspid valve.
The walls of the ventricle are lined with trabeculae carneae , ridges of cardiac muscle covered by endocardium. In addition to these muscular ridges, a band of cardiac muscle, also covered by endocardium, known as the moderator band (see Figure 19.9 ) reinforces the thin walls of the right ventricle and plays a crucial role in cardiac conduction. It arises from the inferior portion of the interventricular septum and crosses the interior space of the right ventricle to connect with the inferior papillary muscle.
When the right ventricle contracts, it ejects blood into the pulmonary trunk, which branches into the left and right pulmonary arteries that carry it to each lung. The superior surface of the right ventricle begins to taper as it approaches the pulmonary trunk. At the base of the pulmonary trunk is the pulmonary semilunar valve that prevents backflow from the pulmonary trunk.
Left Atrium
After exchange of gases in the pulmonary capillaries, blood returns to the left atrium high in oxygen via one of the four pulmonary veins. While the left atrium does not contain pectinate muscles, it does have an auricle that includes these pectinate ridges. Blood flows nearly continuously from the pulmonary veins back into the atrium, which acts as the receiving chamber, and from here through an opening into the left ventricle. Most blood flows passively into the heart while both the atria and ventricles are relaxed, but toward the end of the ventricular relaxation period, the left atrium will contract, pumping blood into the ventricle. This atrial contraction accounts for approximately 20 percent of ventricular filling. The opening between the left atrium and ventricle is guarded by the mitral valve.
Left Ventricle
Recall that, although both sides of the heart will pump the same amount of blood, the muscular layer is much thicker in the left ventricle compared to the right (see Figure 19.8 ). Like the right ventricle, the left also has trabeculae carneae, but there is no moderator band. The mitral valve is connected to papillary muscles via chordae tendineae. There are two papillary muscles on the left—the anterior and posterior—as opposed to three on the right.
The left ventricle is the major pumping chamber for the systemic circuit; it ejects blood into the aorta through the aortic semilunar valve.
Heart Valve Structure and Function
A transverse section through the heart slightly above the level of the atrioventricular septum reveals all four heart valves along the same plane ( Figure 19.12 ). The valves ensure unidirectional blood flow through the heart. Between the right atrium and the right ventricle is the right atrioventricular valve , or tricuspid valve . It typically consists of three flaps, or leaflets, made of endocardium reinforced with additional connective tissue. The flaps are connected by chordae tendineae to the papillary muscles, which control the opening and closing of the valves.
Emerging from the right ventricle at the base of the pulmonary trunk is the pulmonary semilunar valve, or the pulmonary valve ; it is also known as the pulmonic valve or the right semilunar valve. The pulmonary valve is comprised of three small flaps of endothelium reinforced with connective tissue. When the ventricle relaxes, the pressure differential causes blood to flow back into the ventricle from the pulmonary trunk. This flow of blood fills the pocket-like flaps of the pulmonary valve, causing the valve to close and producing an audible sound. Unlike the atrioventricular valves, there are no papillary muscles or chordae tendineae associated with the pulmonary valve.
Located at the opening between the left atrium and left ventricle is the mitral valve , also called the bicuspid valve or the left atrioventricular valve . Structurally, this valve consists of two cusps, compared to the three cusps of the tricuspid valve. In a clinical setting, the valve is referred to as the mitral valve, rather than the bicuspid valve. The two cusps of the mitral valve are attached by chordae tendineae to two papillary muscles that project from the wall of the ventricle.
At the base of the aorta is the aortic semilunar valve, or the aortic valve , which prevents backflow from the aorta. It normally is composed of three flaps. When the ventricle relaxes and blood attempts to flow back into the ventricle from the aorta, blood will fill the cusps of the valve, causing it to close and producing an audible sound.
In Figure 19.13 a , the two atrioventricular valves are open and the two semilunar valves are closed. This occurs when both atria and ventricles are relaxed and when the atria contract to pump blood into the ventricles. Figure 19.13 b shows a frontal view. Although only the left side of the heart is illustrated, the process is virtually identical on the right.
Figure 19.14 a shows the atrioventricular valves closed while the two semilunar valves are open. This occurs when the ventricles contract to eject blood into the pulmonary trunk and aorta. Closure of the two atrioventricular valves prevents blood from being forced back into the atria. This stage can be seen from a frontal view in Figure 19.14 b .
When the ventricles begin to contract, pressure within the ventricles rises and blood flows toward the area of lowest pressure, which is initially in the atria. This backflow causes the cusps of the tricuspid and mitral (bicuspid) valves to close. These valves are tied down to the papillary muscles by chordae tendineae. During the relaxation phase of the cardiac cycle, the papillary muscles are also relaxed and the tension on the chordae tendineae is slight (see Figure 19.13 b ). However, as the myocardium of the ventricle contracts, so do the papillary muscles. This creates tension on the chordae tendineae (see Figure 19.14 b ), helping to hold the cusps of the atrioventricular valves in place and preventing them from being blown back into the atria.
The aortic and pulmonary semilunar valves lack the chordae tendineae and papillary muscles associated with the atrioventricular valves. Instead, they consist of pocket-like folds of endocardium reinforced with additional connective tissue. When the ventricles relax and the change in pressure forces the blood toward the ventricles, the blood presses against these cusps and seals the openings.
Visit this site to observe an echocardiogram of actual heart valves opening and closing. Although much of the heart has been “removed” from this gif loop so the chordae tendineae are not visible, why is their presence more critical for the atrioventricular valves (tricuspid and mitral) than the semilunar (aortic and pulmonary) valves?
Heart Valves
When heart valves do not function properly, they are often described as incompetent and result in valvular heart disease, which can range from benign to lethal. Some of these conditions are congenital, that is, the individual was born with the defect, whereas others may be attributed to disease processes or trauma. Some malfunctions are treated with medications, others require surgery, and still others may be mild enough that the condition is merely monitored since treatment might trigger more serious consequences.
Valvular disorders are often caused by carditis, or inflammation of the heart. One common trigger for this inflammation is rheumatic fever, or scarlet fever, an autoimmune response to the presence of a bacterium, Streptococcus pyogenes , normally a disease of childhood.
While any of the heart valves may be involved in valve disorders, mitral regurgitation is the most common, detected in approximately 2 percent of the population, and the pulmonary semilunar valve is the least frequently involved. When a valve malfunctions, the flow of blood to a region will often be disrupted. The resulting inadequate flow of blood to this region will be described in general terms as an insufficiency. The specific type of insufficiency is named for the valve involved: aortic insufficiency, mitral insufficiency, tricuspid insufficiency, or pulmonary insufficiency.
If one of the cusps of the valve is forced backward by the force of the blood, the condition is referred to as a prolapsed valve. Prolapse may occur if the chordae tendineae are damaged or broken, causing the closure mechanism to fail. The failure of the valve to close properly disrupts the normal one-way flow of blood and results in regurgitation, when the blood flows backward from its normal path. Using a stethoscope, the disruption to the normal flow of blood produces a heart murmur.
Stenosis is a condition in which the heart valves become rigid and may calcify over time. The loss of flexibility of the valve interferes with normal function and may cause the heart to work harder to propel blood through the valve, which eventually weakens the heart. Aortic stenosis affects approximately 2 percent of the population over 65 years of age, and the percentage increases to approximately 4 percent in individuals over 85 years. Occasionally, one or more of the chordae tendineae will tear or the papillary muscle itself may die as a component of a myocardial infarction (heart attack). In this case, the patient’s condition will deteriorate dramatically and rapidly, and immediate surgical intervention may be required.
Auscultation, or listening to a patient’s heart sounds, is one of the most useful diagnostic tools, since it is proven, safe, and inexpensive. The term auscultation is derived from the Latin for “to listen,” and the technique has been used for diagnostic purposes as far back as the ancient Egyptians. Valve and septal disorders will trigger abnormal heart sounds. If a valvular disorder is detected or suspected, a test called an echocardiogram, or simply an “echo,” may be ordered. Echocardiograms are sonograms of the heart and can help in the diagnosis of valve disorders as well as a wide variety of heart pathologies.
Visit this site for a free download, including excellent animations and audio of heart sounds.
Career Connection
Cardiologist.
Cardiologists are medical doctors that specialize in the diagnosis and treatment of diseases of the heart. After completing 4 years of medical school, cardiologists complete a three-year residency in internal medicine followed by an additional three or more years in cardiology. Following this 10-year period of medical training and clinical experience, they qualify for a rigorous two-day examination administered by the Board of Internal Medicine that tests their academic training and clinical abilities, including diagnostics and treatment. After successful completion of this examination, a physician becomes a board-certified cardiologist. Some board-certified cardiologists may be invited to become a Fellow of the American College of Cardiology (FACC). This professional recognition is awarded to outstanding physicians based upon merit, including outstanding credentials, achievements, and community contributions to cardiovascular medicine.
Visit this site to learn more about cardiologists.
Cardiovascular Technologist/Technician
Cardiovascular technologists/technicians are trained professionals who perform a variety of imaging techniques, such as sonograms or echocardiograms, used by physicians to diagnose and treat diseases of the heart. Nearly all of these positions require an associate degree, and these technicians earn a median salary of $49,410 as of May 2010, according to the U.S. Bureau of Labor Statistics. Growth within the field is fast, projected at 29 percent from 2010 to 2020.
There is a considerable overlap and complementary skills between cardiac technicians and vascular technicians, and so the term cardiovascular technician is often used. Special certifications within the field require documenting appropriate experience and completing additional and often expensive certification examinations. These subspecialties include Certified Rhythm Analysis Technician (CRAT), Certified Cardiographic Technician (CCT), Registered Congenital Cardiac Sonographer (RCCS), Registered Cardiac Electrophysiology Specialist (RCES), Registered Cardiovascular Invasive Specialist (RCIS), Registered Cardiac Sonographer (RCS), Registered Vascular Specialist (RVS), and Registered Phlebology Sonographer (RPhS).
Visit this site for more information on cardiovascular technologists/technicians.
Coronary Circulation
You will recall that the heart is a remarkable pump composed largely of cardiac muscle cells that are incredibly active throughout life. Like all other cells, a cardiomyocyte requires a reliable supply of oxygen and nutrients, and a way to remove wastes, so it needs a dedicated, complex, and extensive coronary circulation. And because of the critical and nearly ceaseless activity of the heart throughout life, this need for a blood supply is even greater than for a typical cell. However, coronary circulation is not continuous; rather, it cycles, reaching a peak when the heart muscle is relaxed and nearly ceasing while it is contracting.
Coronary Arteries
Coronary arteries supply blood to the myocardium and other components of the heart. The first portion of the aorta after it arises from the left ventricle gives rise to the coronary arteries. There are three dilations in the wall of the aorta just superior to the aortic semilunar valve. Two of these, the left posterior aortic sinus and anterior aortic sinus, give rise to the left and right coronary arteries, respectively. The third sinus, the right posterior aortic sinus, typically does not give rise to a vessel. Coronary vessel branches that remain on the surface of the artery and follow the sulci are called epicardial coronary arteries .
The left coronary artery distributes blood to the left side of the heart, the left atrium and ventricle, and the interventricular septum. The circumflex artery arises from the left coronary artery and follows the coronary sulcus to the left. Eventually, it will fuse with the small branches of the right coronary artery. The larger anterior interventricular artery , also known as the left anterior descending artery (LAD), is the second major branch arising from the left coronary artery. It follows the anterior interventricular sulcus around the pulmonary trunk. Along the way it gives rise to numerous smaller branches that interconnect with the branches of the posterior interventricular artery, forming anastomoses. An anastomosis is an area where vessels unite to form interconnections that normally allow blood to circulate to a region even if there may be partial blockage in another branch. The anastomoses in the heart are very small. Therefore, this ability is somewhat restricted in the heart so a coronary artery blockage often results in death of the cells (myocardial infarction) supplied by the particular vessel.
The right coronary artery proceeds along the coronary sulcus and distributes blood to the right atrium, portions of both ventricles, and the heart conduction system. Normally, one or more marginal arteries arise from the right coronary artery inferior to the right atrium. The marginal arteries supply blood to the superficial portions of the right ventricle. On the posterior surface of the heart, the right coronary artery gives rise to the posterior interventricular artery , also known as the posterior descending artery. It runs along the posterior portion of the interventricular sulcus toward the apex of the heart, giving rise to branches that supply the interventricular septum and portions of both ventricles. Figure 19.15 presents views of the coronary circulation from both the anterior and posterior views.
Diseases of the...
Diseases of the….
Heart: Myocardial Infarction Myocardial infarction (MI) is the formal term for what is commonly referred to as a heart attack. It normally results from a lack of blood flow (ischemia) and oxygen (hypoxia) to a region of the heart, resulting in death of the cardiac muscle cells. An MI often occurs when a coronary artery is blocked by the buildup of atherosclerotic plaque consisting of lipids, cholesterol and fatty acids, and white blood cells, primarily macrophages. It can also occur when a portion of an unstable atherosclerotic plaque travels through the coronary arterial system and lodges in one of the smaller vessels. The resulting blockage restricts the flow of blood and oxygen to the myocardium and causes death of the tissue. MIs may be triggered by excessive exercise, in which the partially occluded artery is no longer able to pump sufficient quantities of blood, or severe stress, which may induce spasm of the smooth muscle in the walls of the vessel.
In the case of acute MI, there is often sudden pain beneath the sternum (retrosternal pain) called angina pectoris, often radiating down the left arm in males but not in female patients. Until this anomaly between the sexes was discovered, many female patients suffering MIs were misdiagnosed and sent home. In addition, patients typically present with difficulty breathing and shortness of breath (dyspnea), irregular heartbeat (palpations), nausea and vomiting, sweating (diaphoresis), anxiety, and fainting (syncope), although not all of these symptoms may be present. Many of the symptoms are shared with other medical conditions, including anxiety attacks and simple indigestion, so differential diagnosis is critical. It is estimated that between 22 and 64 percent of MIs present without any symptoms.
An MI can be confirmed by examining the patient’s ECG, which frequently reveals alterations in the ST and Q components. Some classification schemes of MI are referred to as ST-elevated MI (STEMI) and non-elevated MI (non-STEMI). In addition, echocardiography or cardiac magnetic resonance imaging may be employed. Common blood tests indicating an MI include elevated levels of creatine kinase MB (an enzyme that catalyzes the conversion of creatine to phosphocreatine, consuming ATP) and cardiac troponin (the regulatory protein for muscle contraction), both of which are released by damaged cardiac muscle cells.
Immediate treatments for MI are essential and include administering supplemental oxygen, aspirin that helps to break up clots, and nitroglycerine administered sublingually (under the tongue) to facilitate its absorption. Despite its unquestioned success in treatments and use since the 1880s, the mechanism of nitroglycerine is still incompletely understood but is believed to involve the release of nitric oxide, a known vasodilator, and endothelium-derived releasing factor, which also relaxes the smooth muscle in the tunica media of coronary vessels. Longer-term treatments include injections of thrombolytic agents such as streptokinase that dissolve the clot, the anticoagulant heparin, balloon angioplasty and stents to open blocked vessels, and bypass surgery to allow blood to pass around the site of blockage. If the damage is extensive, coronary replacement with a donor heart or coronary assist device, a sophisticated mechanical device that supplements the pumping activity of the heart, may be employed. Despite the attention, development of artificial hearts to augment the severely limited supply of heart donors has proven less than satisfactory but will likely improve in the future.
MIs may trigger cardiac arrest, but the two are not synonymous. Important risk factors for MI include cardiovascular disease, age, smoking, high blood levels of the low-density lipoprotein (LDL, often referred to as “bad” cholesterol), low levels of high-density lipoprotein (HDL, or “good” cholesterol), hypertension, diabetes mellitus, obesity, lack of physical exercise, chronic kidney disease, excessive alcohol consumption, and use of illegal drugs.
Coronary Veins
Coronary veins drain the heart and generally parallel the large surface arteries (see Figure 19.15 ). The great cardiac vein can be seen initially on the surface of the heart following the interventricular sulcus, but it eventually flows along the coronary sulcus into the coronary sinus on the posterior surface. The great cardiac vein initially parallels the anterior interventricular artery and drains the areas supplied by this vessel. It receives several major branches, including the posterior cardiac vein, the middle cardiac vein, and the small cardiac vein. The posterior cardiac vein parallels and drains the areas supplied by the marginal artery branch of the circumflex artery. The middle cardiac vein parallels and drains the areas supplied by the posterior interventricular artery. The small cardiac vein parallels the right coronary artery and drains the blood from the posterior surfaces of the right atrium and ventricle. The coronary sinus is a large, thin-walled vein on the posterior surface of the heart lying within the atrioventricular sulcus and emptying directly into the right atrium. The anterior cardiac veins parallel the small cardiac arteries and drain the anterior surface of the right ventricle. Unlike these other cardiac veins, it bypasses the coronary sinus and drains directly into the right atrium.
Heart: Coronary Artery Disease
Coronary artery disease is the leading cause of death worldwide. It occurs when the buildup of plaque—a fatty material including cholesterol, connective tissue, white blood cells, and some smooth muscle cells—within the walls of the arteries obstructs the flow of blood and decreases the flexibility or compliance of the vessels. This condition is called atherosclerosis, a hardening of the arteries that involves the accumulation of plaque. As the coronary blood vessels become occluded, the flow of blood to the tissues will be restricted, a condition called ischemia that causes the cells to receive insufficient amounts of oxygen, called hypoxia. Figure 19.16 shows the blockage of coronary arteries highlighted by the injection of dye. Some individuals with coronary artery disease report pain radiating from the chest called angina pectoris, but others remain asymptomatic. If untreated, coronary artery disease can lead to MI or a heart attack.
The disease progresses slowly and often begins in children and can be seen as fatty “streaks” in the vessels. It then gradually progresses throughout life. Well-documented risk factors include smoking, family history, hypertension, obesity, diabetes, high alcohol consumption, lack of exercise, stress, and hyperlipidemia or high circulating levels of lipids in the blood. Treatments may include medication, changes to diet and exercise, angioplasty with a balloon catheter, insertion of a stent, or coronary bypass procedure.
Angioplasty is a procedure in which the occlusion is mechanically widened with a balloon. A specialized catheter with an expandable tip is inserted into a superficial vessel, normally in the leg, and then directed to the site of the occlusion. At this point, the balloon is inflated to compress the plaque material and to open the vessel to increase blood flow. Then, the balloon is deflated and retracted. A stent consisting of a specialized mesh is typically inserted at the site of occlusion to reinforce the weakened and damaged walls. Stent insertions have been routine in cardiology for more than 40 years.
Coronary bypass surgery may also be performed. This surgical procedure grafts a replacement vessel obtained from another, less vital portion of the body to bypass the occluded area. This procedure is clearly effective in treating patients experiencing a MI, but overall does not increase longevity. Nor does it seem advisable in patients with stable although diminished cardiac capacity since frequently loss of mental acuity occurs following the procedure. Long-term changes to behavior, emphasizing diet and exercise plus a medicine regime tailored to lower blood pressure, lower cholesterol and lipids, and reduce clotting are equally as effective.
As an Amazon Associate we earn from qualifying purchases.
This book may not be used in the training of large language models or otherwise be ingested into large language models or generative AI offerings without OpenStax's permission.
Want to cite, share, or modify this book? This book uses the Creative Commons Attribution License and you must attribute OpenStax.
Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction
- Authors: J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble, Peter DeSaix
- Publisher/website: OpenStax
- Book title: Anatomy and Physiology
- Publication date: Apr 25, 2013
- Location: Houston, Texas
- Book URL: https://openstax.org/books/anatomy-and-physiology/pages/1-introduction
- Section URL: https://openstax.org/books/anatomy-and-physiology/pages/19-1-heart-anatomy
© Jan 27, 2022 OpenStax. Textbook content produced by OpenStax is licensed under a Creative Commons Attribution License . The OpenStax name, OpenStax logo, OpenStax book covers, OpenStax CNX name, and OpenStax CNX logo are not subject to the Creative Commons license and may not be reproduced without the prior and express written consent of Rice University.
BLOOD FLOW through the HEART
Mar 25, 2019
600 likes | 869 Views
BLOOD FLOW through the HEART. Biology Version:. The right and left sides of the heart work together Right Side Blood enters the heart through two large veins, the inferior and superior vena cava, emptying oxygen-poor blood from the body into the right atrium. Left Side
Share Presentation
- tricuspid valve
- aortic valve
- pulmonic valve
- tricuspid valve shuts
- emptying oxygen poor blood

Presentation Transcript
Biology Version: The right and left sides of the heart work together Right Side Blood enters the heart through two large veins, the inferior and superior vena cava, emptying oxygen-poor blood from the body into the right atrium. Left Side The pulmonary vein empties oxygen-rich blood, from the lungs into the left atrium.
Atrial contraction Right Side Blood flows from your right atrium into your right ventricle through the open tricuspid valve. When the ventricles are full, the tricuspid valve shuts. This prevents blood from flowing backward into the atria while the ventricles contract (squeeze). Left Side Blood flows from your left atrium into your left ventricle through the open mitral valve. When the ventricles are full, the mitral valve shuts. This prevents blood from flowing backward into the atria while the ventricles contract (squeeze).
Ventricular contraction Oxygen and carbon dioxide travels to and from tiny air sacs in the lungs, through the walls of the capillaries, into the blood. Right Side Blood leaves the heart through the pulmonic valve, into the pulmonary artery and to the lungs. Left Side Blood leaves the heart through the aortic valve, into the aorta and to the body. This pattern is repeated, causing blood to flow continuously to the heart, lungs and body.
Anatomy Version
Superior Vena Cava
Superior Vena Cava Inferior Vena Cava
Superior Vena Cava Right Atrium Inferior Vena Cava
Superior Vena Cava Right Atrium Tricuspid Valve Inferior Vena Cava
Superior Vena Cava Right Atrium Inferior Vena Cava Tricuspid Valve
Superior Vena Cava Right Atrium Inferior Vena Cava Tricuspid Valve Right Ventricle
Superior Vena Cava Right Atrium Pulmonary Semilunar Valve Inferior Vena Cava Tricuspid Valve Right Ventricle
Superior Vena Cava Pulmonary Trunk Right Atrium Pulmonary Semilunar Valve Inferior Vena Cava Tricuspid Valve Right Ventricle
Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Right Atrium Pulmonary Semilunar Valve Inferior Vena Cava Tricuspid Valve Right Ventricle
Lungs Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Right Atrium Pulmonary Semilunar Valve Inferior Vena Cava Tricuspid Valve Right Ventricle
Lungs Pulmonary Veins Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Right Atrium Pulmonary Semilunar Valve Inferior Vena Cava Tricuspid Valve Right Ventricle
Lungs Pulmonary Veins Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Left Atrium Right Atrium Pulmonary Semilunar Valve Inferior Vena Cava Tricuspid Valve Right Ventricle
Lungs Pulmonary Veins Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Right Atrium Left Atrium Pulmonary Semilunar Valve Inferior Vena Cava Tricuspid Valve Right Ventricle
Pulmonary Loop Lungs Pulmonary Veins Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Right Atrium Left Atrium Pulmonary Semilunar Valve Inferior Vena Cava Tricuspid Valve Right Ventricle
Pulmonary Loop Lungs Pulmonary Veins Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Right Atrium Left Atrium Bicuspid Valve Pulmonary Semilunar Valve Inferior Vena Cava Tricuspid Valve Right Ventricle
Pulmonary Loop Lungs Pulmonary Veins Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Right Atrium Left Atrium Pulmonary Semilunar Valve Inferior Vena Cava Bicuspid Valve Tricuspid Valve Right Ventricle
Pulmonary Loop Lungs Pulmonary Veins Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Right Atrium Left Atrium Pulmonary Semilunar Valve Inferior Vena Cava Bicuspid Valve Tricuspid Valve Left Ventricle Right Ventricle
Pulmonary Loop Lungs Pulmonary Veins Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Right Atrium Left Atrium Pulmonary Semilunar Valve Inferior Vena Cava Bicuspid Valve Tricuspid Valve Right Ventricle Left Ventricle
Pulmonary Loop Lungs Pulmonary Veins Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Right Atrium Left Atrium Pulmonary Semilunar Valve Inferior Vena Cava Bicuspid Valve Tricuspid Valve Intraventricular Septum Right Ventricle Left Ventricle
Pulmonary Loop Lungs Pulmonary Veins Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Right Atrium Left Atrium Aortic Semilunar Valve Pulmonary Semilunar Valve Inferior Vena Cava Bicuspid Valve Tricuspid Valve Intraventricular Septum Right Ventricle Left Ventricle
Pulmonary Loop Lungs Pulmonary Veins Pulmonary Arteries Superior Vena Cava Aortic Trunk Pulmonary Trunk Right Atrium Left Atrium Aortic Semilunar Valve Pulmonary Semilunar Valve Inferior Vena Cava Bicuspid Valve Tricuspid Valve Intraventricular Septum Right Ventricle Left Ventricle
Pulmonary Loop Lungs Pulmonary Veins Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Aortic Trunk Right Atrium Left Atrium Aortic Semilunar Valve Pulmonary Semilunar Valve Inferior Vena Cava Bicuspid Valve Tricuspid Valve Intraventricular Septum Right Ventricle Left Ventricle
Pulmonary Loop Lungs Brachiocephalic Artery Pulmonary Veins Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Aortic Trunk Right Atrium Left Atrium Aortic Semilunar Valve Pulmonary Semilunar Valve Inferior Vena Cava Bicuspid Valve Tricuspid Valve Intraventricular Septum Right Ventricle Left Ventricle
Pulmonary Loop Left Common Corotid Artery Lungs Brachiocephalic Artery Pulmonary Veins Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Aortic Trunk Right Atrium Left Atrium Aortic Semilunar Valve Pulmonary Semilunar Valve Inferior Vena Cava Bicuspid Valve Tricuspid Valve Intraventricular Septum Right Ventricle Left Ventricle
Pulmonary Loop Left Subclavian Artery Left Common Corotid Artery Lungs Brachiocephalic Artery Pulmonary Veins Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Aortic Trunk Right Atrium Left Atrium Aortic Semilunar Valve Pulmonary Semilunar Valve Inferior Vena Cava Bicuspid Valve Tricuspid Valve Intraventricular Septum Right Ventricle Left Ventricle
Pulmonary Loop Left Common Corotid Artery Lungs Left Subclavian Artery Brachiocephalic Artery Pulmonary Veins Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Aortic Trunk Right Atrium Left Atrium Aortic Semilunar Valve Pulmonary Semilunar Valve Inferior Vena Cava Bicuspid Valve Tricuspid Valve Intraventricular Septum Right Ventricle Left Ventricle
Pulmonary Loop Left Common Corotid Artery Lungs Left Subclavian Artery Brachiocephalic Artery Aorta Pulmonary Veins Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Aortic Trunk Right Atrium Left Atrium Aortic Semilunar Valve Pulmonary Semilunar Valve Inferior Vena Cava Bicuspid Valve Tricuspid Valve Intraventricular Septum Right Ventricle Left Ventricle
Pulmonary Loop Left Common Corotid Artery Lungs Left Subclavian Artery Brachiocephalic Artery Pulmonary Veins Aorta Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Aortic Trunk Right Atrium Left Atrium Aortic Semilunar Valve Pulmonary Semilunar Valve Inferior Vena Cava Bicuspid Valve Tricuspid Valve Intraventricular Septum Right Ventricle Left Ventricle
Pulmonary Loop Left Common Corotid Artery Lungs Left Subclavian Artery Brachiocephalic Artery Pulmonary Veins Aorta Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Aortic Trunk Right Atrium Left Atrium Arteries Aortic Semilunar Valve Pulmonary Semilunar Valve Inferior Vena Cava Bicuspid Valve Tricuspid Valve Intraventricular Septum Right Ventricle Left Ventricle
Pulmonary Loop Left Common Corotid Artery Lungs Left Subclavian Artery Brachiocephalic Artery Pulmonary Veins Aorta Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Aortic Trunk Right Atrium Left Atrium Aortic Semilunar Valve Pulmonary Semilunar Valve Inferior Vena Cava Arteries Bicuspid Valve Tricuspid Valve Intraventricular Septum Right Ventricle Left Ventricle
Pulmonary Loop Left Common Corotid Artery Lungs Left Subclavian Artery Brachiocephalic Artery Pulmonary Veins Aorta Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Aortic Trunk Right Atrium Left Atrium Aortic Semilunar Valve Pulmonary Semilunar Valve Inferior Vena Cava Arteries Bicuspid Valve Tricuspid Valve Intraventricular Septum Right Ventricle Left Ventricle Body
Pulmonary Loop Left Common Corotid Artery Lungs Left Subclavian Artery Brachiocephalic Artery Pulmonary Veins Aorta Pulmonary Arteries Superior Vena Cava Pulmonary Trunk Aortic Trunk Right Atrium Left Atrium Aortic Semilunar Valve Pulmonary Semilunar Valve Inferior Vena Cava Arteries Bicuspid Valve Tricuspid Valve Intraventricular Septum Right Ventricle Left Ventricle Body Tissues
- More by User
Empty Heart Blood Flow Anatomy
... the blood flow can not be understood until the anatomy is learned. ... When you feel comfortable with the anatomy you can click the link to the Blood ...
1.3k views • 62 slides
BLOOD FLOW. Barbara Grobelnik Advisor: dr. Igor Serša. The study of blood flow behavior: Improving the design of implants (heart valves, artificial heart) and extra-corporeal flow devices (blood oxygenators, dialysis machines)
893 views • 18 slides
Path of Blood Through The Heart
Path of Blood Through The Heart. Heart Chambers and Valves. Atria or Atrium Auricles Ventricles Interatrial Septum Interventricular septum Atrioventricular Orifice. Heart Chambers and Valves. Atrioventricular Valve (A-V valve) Sulci Atrioventricular (coronary) Sulcus
387 views • 15 slides
Blood Vessels and Flow Through the circulatory system
Blood Vessels and Flow Through the circulatory system. Heart pumps blood by increasing local pressure As blood travels through circulatory system, it encounters friction. Physics of Blood Flow. Physics of Blood Flow. What sets the resistance of a tube?. Think of drinking through a straw
714 views • 33 slides
The Path of Blood Through the Heart
The Path of Blood Through the Heart. Part I All the blood from the body travels through veins back to the heart. The blood from the head and neck enter the heart through the superior vena cava . Most of the blood from the rest of body enters the heart through the inferior vena cava .
525 views • 5 slides
UNDERSTANDING THE BLOOD FLOW OF THE HEART
UNDERSTANDING THE BLOOD FLOW OF THE HEART. Rheede Hopgood . Blood enters the heart through two large veins, the inferior and superior vena cava, emptying oxygen-poor blood from the body into the right atrium.
293 views • 8 slides
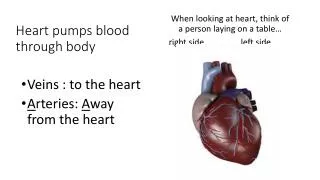
Heart pumps blood through body
Heart pumps blood through body. When looking at heart, think of a person laying on a table… r ight side left side. Veins : to the heart A rteries: A way from the heart. Heart is a PumP. 4 chambers Heart beat you hear is open/closing of valve noise Deoxygenated blood right side
298 views • 7 slides
Blood Flow. The purpose of cardiovascular regulation is to maintain adequate blood flow through the capillaries to the tissues Actual volume of blood flowing through a vessel, an organ, or the entire circulation in a given period: Is measured in ml/min .
949 views • 45 slides
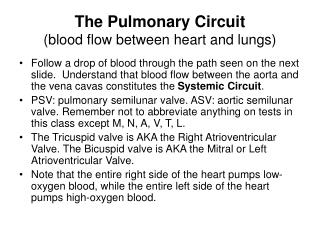
The Pulmonary Circuit (blood flow between heart and lungs)
The Pulmonary Circuit (blood flow between heart and lungs). Follow a drop of blood through the path seen on the next slide. Understand that blood flow between the aorta and the vena cavas constitutes the Systemic Circuit .
488 views • 12 slides

Renal Blood Flow
Renal Blood Flow. Total renal blood flow: TRBF ~ 1270 ml/min ~ 20-25% of CO (5000 ml/min) ~ 90% to cortex Total renal plasma flow: TRPF ~ 700 ml/min (Hct ~ 0.45) Filtration fraction ~ 20% (GFR = 125 / 700 ml/min) The low medullary flow is due to high resistance of the vasa recta.
893 views • 17 slides
Real-time visualization of blood flow through the brain
Real-time visualization of blood flow through the brain. Steven Manos, Marco Mazzeo , Peter Coveney, University College London (UCL) The GENIUS project (Grid Enabled Neurosurgical Imaging Using Simulation) to study blood flow around the brain prior to surgery greatly increasing the
160 views • 1 slides
Objective: You will be able to trace the flow of blood through the heart.
Objective: You will be able to trace the flow of blood through the heart. Do Now: Read all of p. 945 What is the function of the valves in the heart?. Transport. Transport involves absorbing substances in the blood and circulating it through the body
588 views • 47 slides

Blood Flow. Heart ïƒ Lungs ïƒ Heart ïƒ Body. Vena Cava - vein. AORTA - artery. Atria. Ventricles. UNoxygenated blood enters the atrium on the right side of the heart. Unoxygenated blood comes in from the top of the body through the superior vena cava .
447 views • 18 slides
Blood supply of the Heart
Blood supply of the Heart. Dr. Sama ul Haque Dr Rania Gabr. Objectives. Enlist the arteries and veins supplying heart. Describe the origin and branches of the right and left coronary arteries. Define coronary artery anastomosis.
3.72k views • 27 slides

Blood/Heart
Blood/Heart. Heart Facts. The heart you see drawn on the average Valentine is only a rough representation Of the actual structure of the heart. Your heart is actually shaped more like an Upside down pear. Crazy Fact.
529 views • 18 slides
Blood flow through the human circulatory system
Blood flow through the human circulatory system. God is Life. Throughout the Old Testament God has used the symbol of blood to identify life. Leviticus 17:11 – For the life of the flesh is in the blood
269 views • 16 slides
BLOOD SUPPLY OF THE HEART
BLOOD SUPPLY OF THE HEART. Dr Jamila EL medany. &. Dr Essam Salama. Objectives. At the end of the lecture the student should be able to know about; The arterial supply of the cardiac muscle regarding (origin, course, distribution and branches). The coronary anastmosis .
405 views • 18 slides
Blood Flow in Heart
Blood Flow in Heart. Blood Returns from the Body Right Atrium ________________________ Valve Right ________________________ ________________________ Semilunar Valve ________________________ Trunk Right and Left ________________________ ________________________
241 views • 13 slides
Aim : How does blood travel through the human heart?
Aim : How does blood travel through the human heart?. Do Now : Circulatory System Questions. HW : Page 967 Question #11-16. What happened in this clip? What did you hear coming from the heart? What do you think was causing this sound?
204 views • 9 slides

The Human Heart and Blood Flow
The Human Heart and Blood Flow. The Human Heart. http://www.nlm.nih.gov/medlineplus/ency/presentations/100147_1.htm. Located in the Thoracic Cavity, between the two lungs and slightly to the left About the size of a clenched fist. Weighs around a ½ pound.
318 views • 7 slides
Blood brings nutrients to each bodyu2019s organ, including the brain. When nutrients are restricted from getting where they are needed, your body canu2019t function at its best. Thatu2019s why itu2019s so important to consume foods that increase blood flow.
150 views • 8 slides
Pulmonary Blood Flow
Pulmonary Blood Flow. Lectures on respiratory physiology. Pulmonary and systemic circulations. Alveoli with capillaries. Compression of capillaries. P ulmonary capillary has a very thin wall. Small pulmonary vein. Alveolar and extra-alveolar vessels.
376 views • 32 slides

- Upload Ppt Presentation
- Upload Pdf Presentation
- Upload Infographics
- User Presentation
- Related Presentations

Benefits of Physiotherapy
By: drdwayn Views: 971

Food hygiene
By: drdwayn Views: 1791

Top 8 Considerable Benefits of Physiotherapy
By: drdwayn Views: 1273

Acute Sinusitis - Diagnosis Management and Complications
By: drdwayn Views: 1781

Classification and Components of Removable Partial Dentures
By: drdwayn Views: 1266
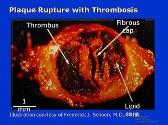
Pathogenesis of Acute Coronary Syndromes
By: JenniferDwayne Views: 1269

Cardiac Assist Devices
By: drdwayn Views: 1063

Blood coagulation and fibrinolysis
By: JenniferDwayne Views: 1586

How does blood flow inform us about brain function
By: JenniferDwayne Views: 640

The Cardiovascular System
By: KhushbuSG Views: 583

- About : I am Dr. Dwayne Faulk
- Occupation : Medical Professional
- Specialty : Other Health Professionals
- Country : United States of America
HEALTH A TO Z
- Eye Disease
- Heart Attack
- Medications
Cardiovascular System Anatomy and Physiology

Journey to the heart of our being with the cardiovascular system study guide . Aspiring nurses, chart the pulsating rivers of life as you discover the anatomy and dynamics of the body’s powerful pump and intricate vessel networks.
Table of Contents
Functions of the heart, heart structure and functions, layers of the heart, chambers of the heart, associated great vessels, heart valves, cardiac circulation vessels, blood vessels, major arteries of the systemic circulation, major veins of the systemic circulation, intrinsic conduction system of the heart, the pathway of the conduction system, cardiac cycle and heart sounds, cardiac output, physiology of circulation, cardiovascular vital signs, blood circulation through the heart, capillary exchange of gases and nutrients, age-related physiological changes in the cardiovascular system.
The functions of the heart are as follows:
- Managing blood supply. Variations in the rate and force of heart contraction match blood flow to the changing metabolic needs of the tissues during rest, exercise, and changes in body position.
- Producing blood pressure. Contractions of the heart produce blood pressure, which is needed for blood flow through the blood vessels.
- Securing one-way blood flow. The valves of the heart secure a one-way blood flow through the heart and blood vessels.
- Transmitting blood. The heart separates the pulmonary and systemic circulations, which ensures the flow of oxygenated blood to tissues.
Anatomy of the Heart
The cardiovascular system can be compared to a muscular pump equipped with one-way valves and a system of large and small plumbing tubes within which the blood travels.
The modest size and weight of the heart give few hints of its incredible strength.
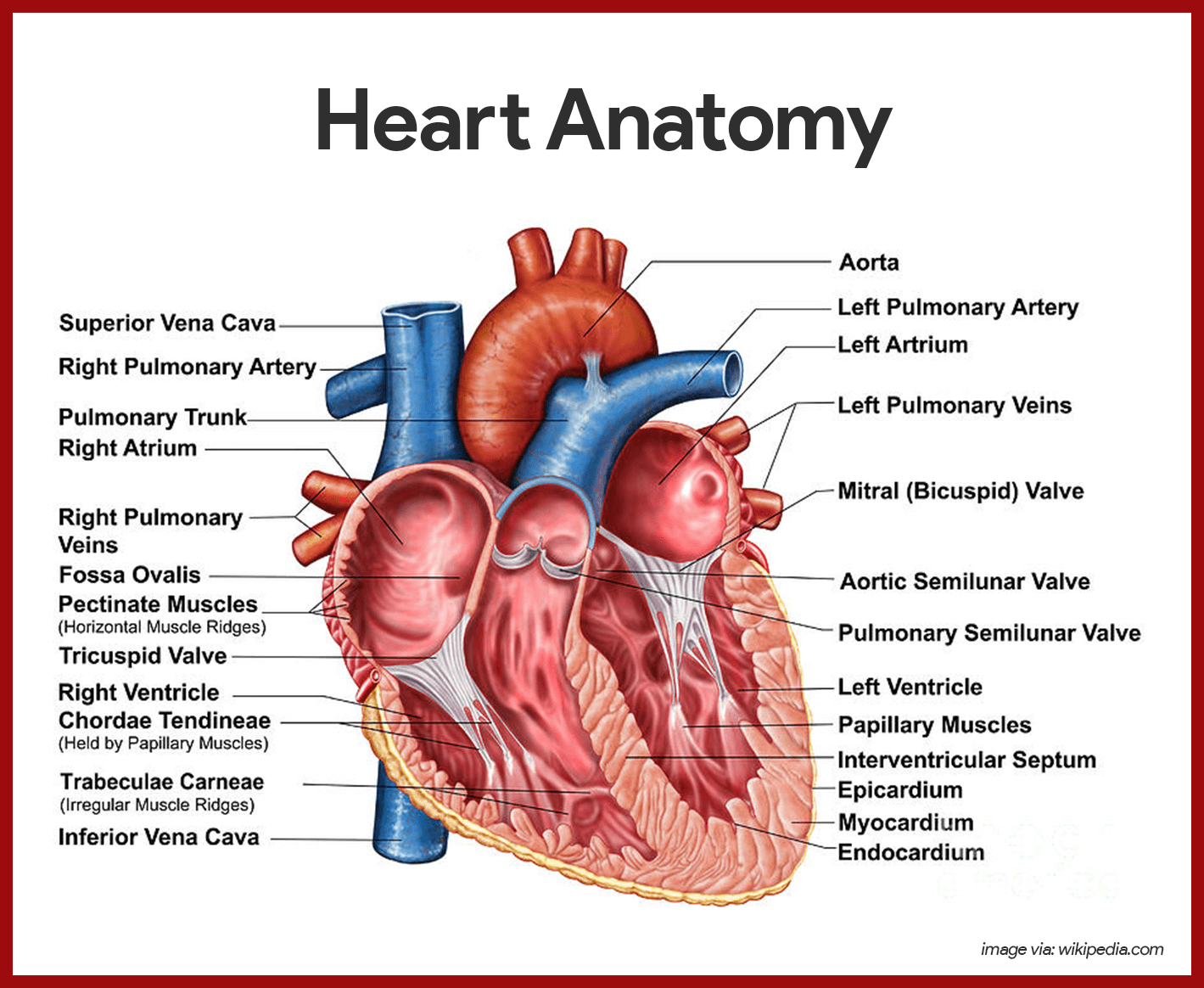
- Weight. Approximately the size of a person’s fist, the hollow , cone-shaped heart weighs less than a pound .
- Mediastinum. Snugly enclosed within the inferior mediastinum, the medial cavity of the thorax, the heart is flanked on each side by the lungs.
- Apex. Its more pointed apex is directed toward the left hip and rests on the diaphragm, approximately at the level of the fifth intercostal space.
- Base. Its broad posterosuperior aspect, or base , from which the great vessels of the body emerge, points toward the right shoulder and lies beneath the second rib.
- Pericardium. The heart is enclosed in a double-walled sac called the pericardium which is the outermost layer of the heart.
- Fibrous pericardium. The loosely fitting superficial part of this sac is referred to as the fibrous pericardium, which helps protect the heart and anchors it to surrounding structures such as the diaphragm and sternum .
- Serous pericardium. Deep to the fibrous pericardium is the slippery, two-layer serous pericardium, where its parietal layer lines the interior of the fibrous pericardium.
The heart muscle has three layers and they are as follows:
- Epicardium. The epicardium or the visceral and outermost layer is actually a part of the heart wall.
- Myocardium. The myocardium consists of thick bundles of cardiac muscle twisted and whirled into ringlike arrangements and it is the layer that actually contracts.
- Endocardium. The endocardium is the innermost layer of the heart and is a thin, glistening sheet of endothelium hat lines the heart chambers.
The heart has four hollow chambers, or cavities: two atria and two ventricles.
- Receiving chambers. The two superior atria are primarily the receiving chambers, they play a lighter role in the pumping activity of the heart.
- Discharging chambers. The two inferior, thick-walled ventricles are the discharging chambers, or actual pumps of the heart wherein when they contract, blood is propelled out of the heart and into circulation.
- Septum. The septum that divides the heart longitudinally is referred to as either the interventricular septum or the interatrial septum, depending on which chamber it separates.
The great blood vessels provide a pathway for the entire cardiac circulation to proceed.
- Superior and inferior vena cava. The heart receives relatively oxygen-poor blood from the veins of the body through the large superior and inferior vena cava and pumps it through the pulmonary trunk .
- Pulmonary arteries. The pulmonary trunk splits into the right and left pulmonary arteries, which carry blood to the lungs, where oxygen is picked up and carbon dioxide is unloaded.
- Pulmonary veins. Oxygen-rich blood drains from the lungs and is returned to the left side of the heart through the four pulmonary veins.
- Aorta. Blood returned to the left side of the heart is pumped out of the heart into the aorta from which the systemic arteries branch to supply essentially all body tissues.
The heart is equipped with four valves, which allow blood to flow in only one direction through the heart chambers.
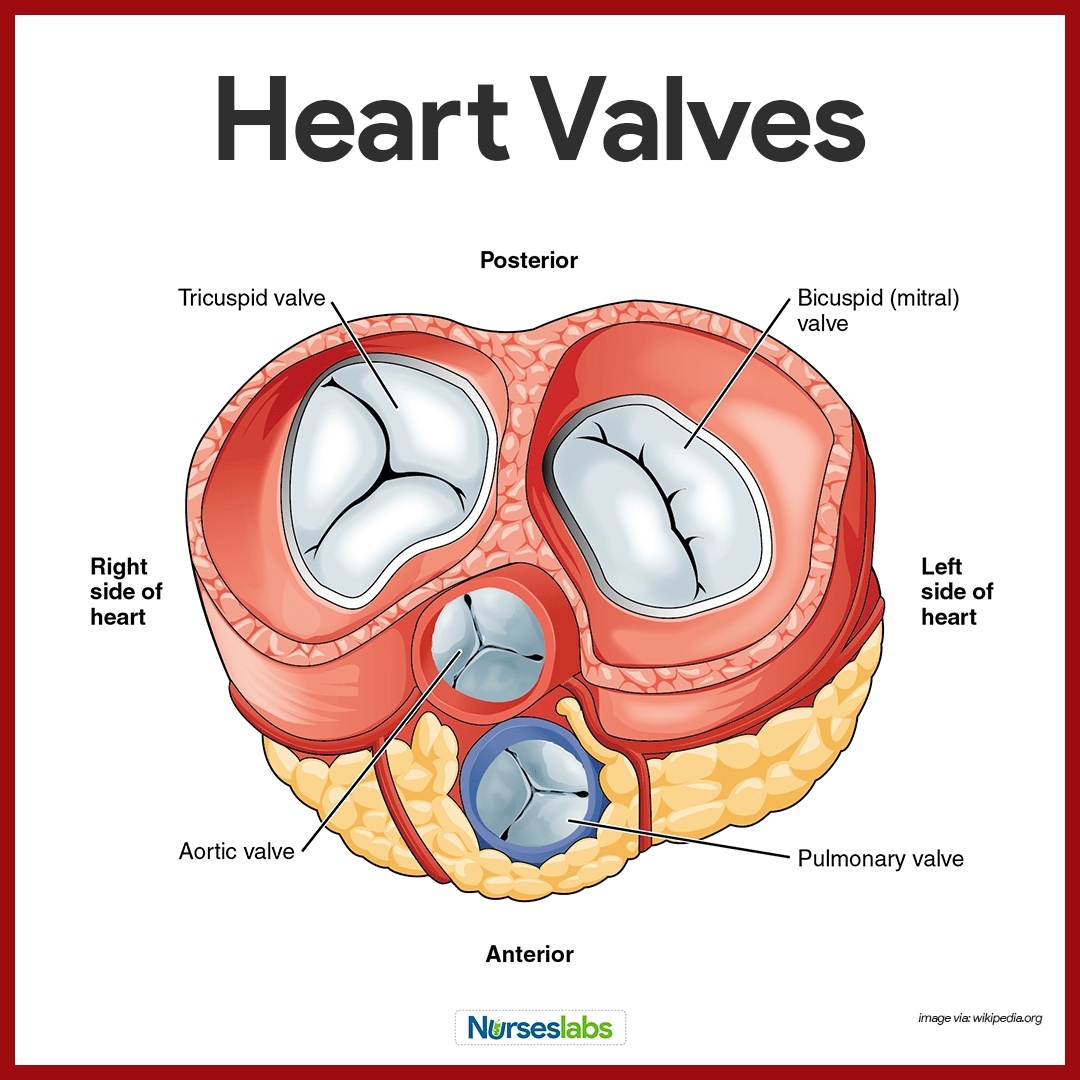
- Atrioventricular valves. Atrioventricular or AV valves are located between the atrial and ventricular chambers on each side, and they prevent backflow into the atria when the ventricles contract.
- Bicuspid valves. The left AV valve- the bicuspid or mitral valve, consists of two flaps, or cusps, of the endocardium.
- Tricuspid valve. The right AV valve, the tricuspid valve, has three flaps.
- Semilunar valve. The second set of valves, the semilunar valves, guards the bases of the two large arteries leaving the ventricular chambers, thus they are known as the pulmonary and aortic semilunar valves.
Although the heart chambers are bathed with blood almost continuously, the blood contained in the heart does not nourish the myocardium.
- Coronary arteries. The coronary arteries branch from the base of the aorta and encircle the heart in the coronary sulcus (atrioventricular groove) at the junction of the atria and ventricles, and these arteries are compressed when the ventricles are contract and fill when the heart is relaxed.
- Cardiac veins. The myocardium is drained by several cardiac veins, which empty into an enlarged vessel on the posterior of the heart called the coronary sinus .
Blood circulates inside the blood vessels, which form a closed transport system, the so-called vascular system.
- Arteries. As the heart beats, blood is propelled into large arteries leaving the heart.
- Arterioles. It then moves into successively smaller and smaller arteries and then into arterioles, which feed the capillary beds in the tissues.
- Veins. Capillary beds are drained by venules , which in turn empty into veins that finally empty into the great veins entering the heart.
Except for the microscopic capillaries, the walls of the blood vessels have three coats or tunics.
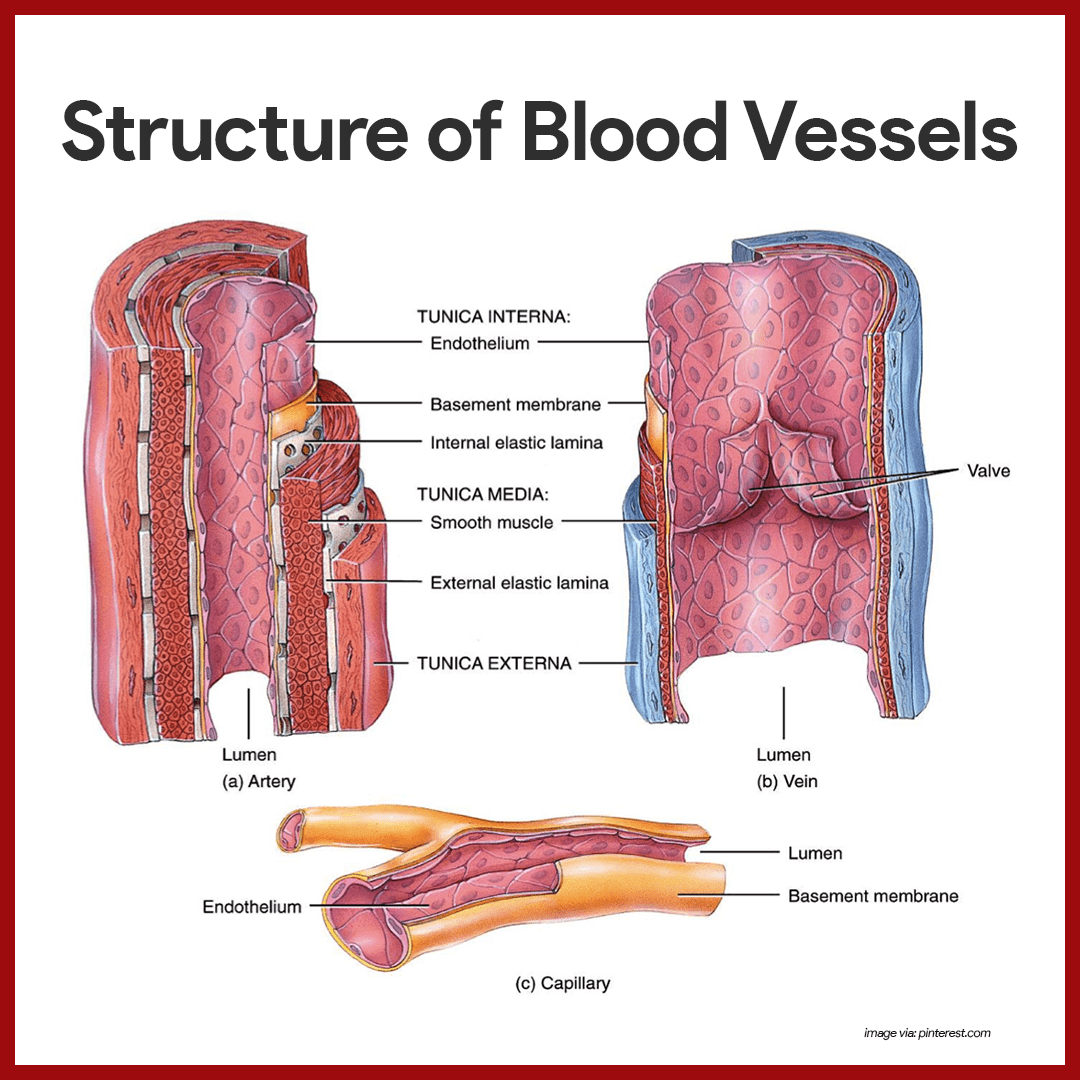
- Tunica intima. The tunica intima, which lines the lumen, or interior, of the vessels, is a thin layer of endothelium resting on a basement membrane and decreases friction as blood flows through the vessel lumen.
- Tunica media. The tunica media is the bulky middle coat which mostly consists of smooth muscle and elastic fibers that constrict or dilate, making the blood pressure increase or decrease.
- Tunica externa. The tunica externa is the outermost tunic composed largely of fibrous connective tissue, and its function is basically to support and protect the vessels.
The major branches of the aorta and the organs they serve are listed next in the sequence from the heart.
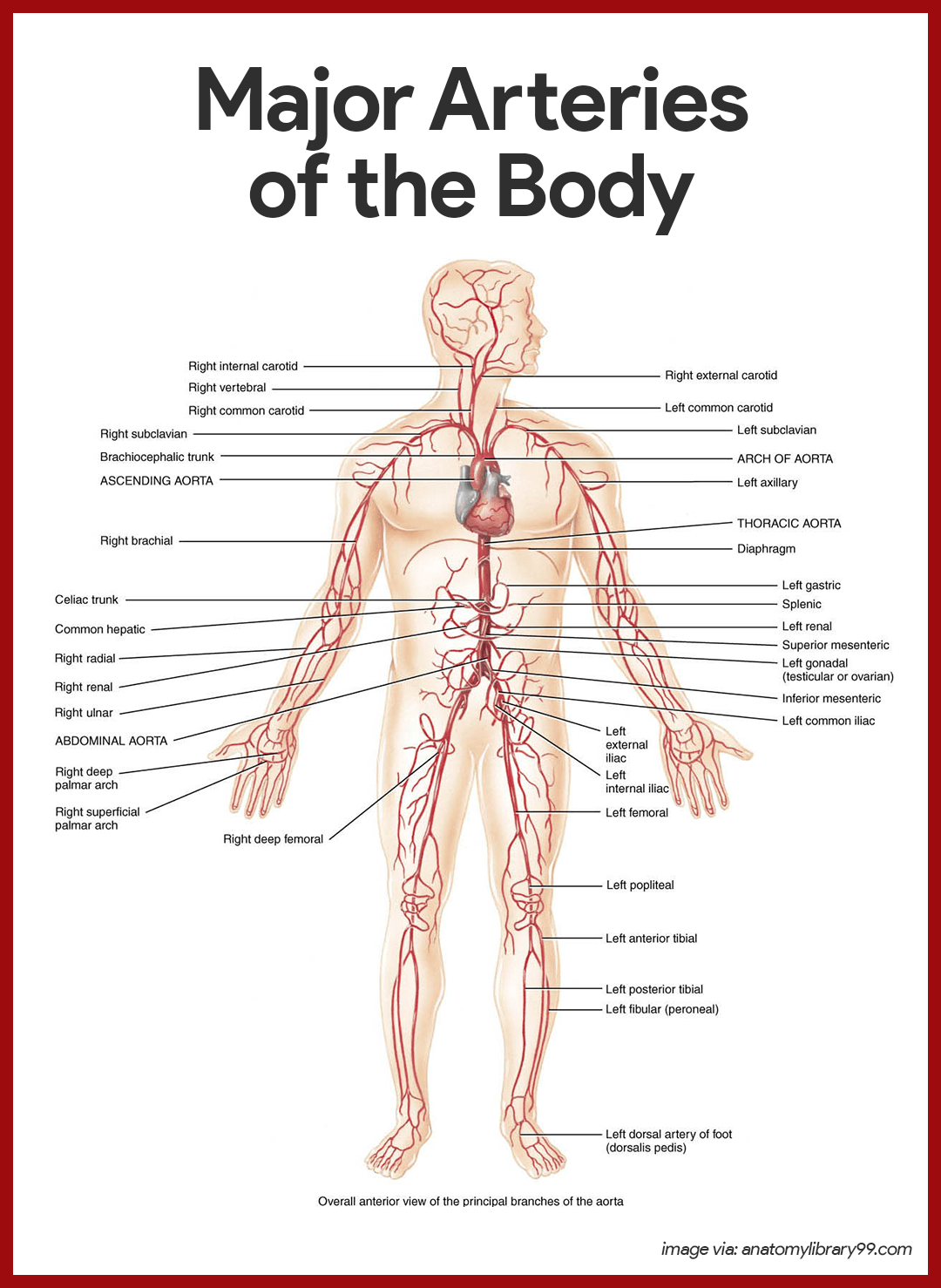
Arterial Branches of the Ascending Aorta
The aorta springs upward from the left ventricle of the heart as the ascending aorta.
- Coronary arteries. The only branches of the ascending aorta are the right and left coronary arteries, which serve the heart.
Arterial Branches of the Aortic Arch
The aorta arches to the left as the aortic arch.
- Brachiocephalic trunk. The brachiocephalic trunk, the first branch off the aortic arch, splits into the right common carotid artery and right subclavian artery .
- Left common carotid artery. The left common carotid artery is the second branch of the aortic arch and it divides, forming the left internal carotid , which serves the brain, and the l eft external carotid , which serves the skin and muscles of the head and neck.
- Left subclavian artery. The third branch of the aortic arch, the left subclavian artery , gives off an important branch- the vertebral artery , which serves as part of the brain.
- Axillary artery. In the axilla, the subclavian artery becomes the axillary artery.
- Brachial artery. the subclavian artery continues into the arm as the brachial artery, which supplies the arm.
- Radial and ulnar arteries. At the elbow, the brachial artery splits to form the radial and ulnar arteries, which serve the forearm.
Arterial Branches of the Thoracic Aorta
The aorta plunges downward through the thorax, following the spine as the thoracic aorta.
- Intercostal arteries. Ten pairs of intercostal arteries supply the muscles of the thorax wall.
Arterial Branches of the Abdominal Aorta
Finally, the aorta passes through the diaphragm into the abdominopelvic cavity, where it becomes the abdominal aorta.
- Celiac trunk. The celiac trunk is the first branch of the abdominal aorta and has three branches: the left gastric artery supplies the stomach ; the splenic artery supplies the spleen , and the common hepatic artery supplies the liver.
- Superior mesenteric artery. The unpaired superior mesenteric artery supplies most of the small intestine and the first half of the large intestine or colon .
- Renal arteries. The renal arteries serve the kidneys.
- Gonadal arteries. The gonadal arteries supply the gonads, and they are called ovarian arteries in females while in males they are testicular arteries .
- Lumbar arteries. The lumbar arteries are several pairs of arteries serving the heavy muscles of the abdomen and trunk walls.
- Inferior mesenteric artery. The inferior mesenteric artery is a small, unpaired artery supplying the second half of the large intestine.
- Common iliac arteries. The common iliac arteries are the final branches of the abdominal aorta.
Major veins converge on the venae cavae, which enter the right atrium of the heart.
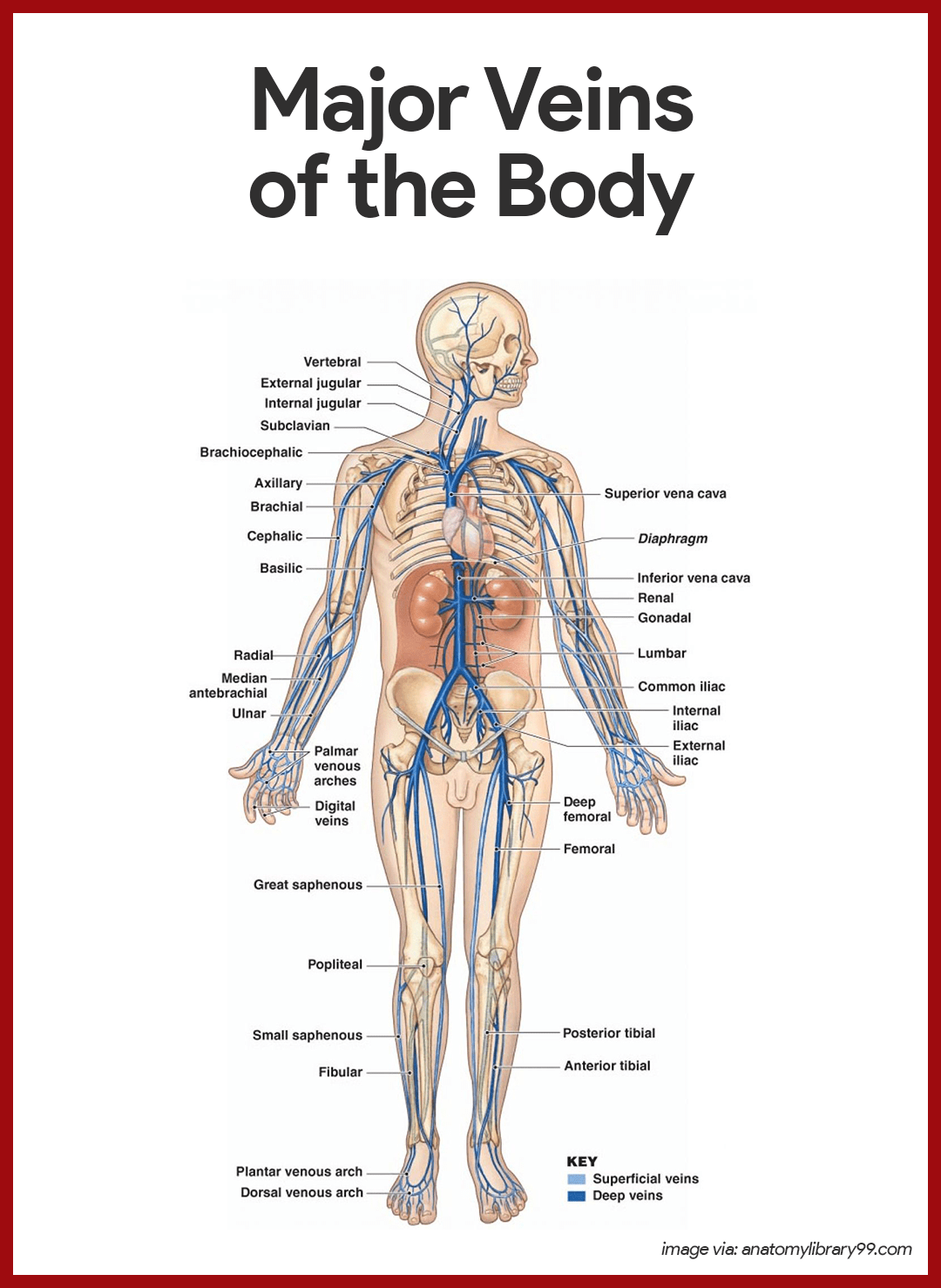
Veins Draining into the Superior Vena Cava
Veins draining into the superior vena cava are named in a distal-to-proximal direction; that is, in the same direction the blood flows into the superior vena cava.
- Radial and ulnar veins . The radial and ulnar veins are deep veins draining the forearm; they unite to form the deep brachial vein , which drains the arm and empties into the axillary vein in the axillary region.
- Cephalic vein. The cephalic vein provides for the superficial drainage of the lateral aspect of the arm and empties into the axillary vein.
- Basilic vein. The basilic vein is a superficial vein that drains the medial aspect of the arm and empties into the brachial vein proximally.
- Median cubital vein. The basilic and cephalic veins are joined at the anterior aspect of the elbow by the median cubital vein, often chosen as the site for blood removal for the purpose of blood testing.
- Subclavian vein. The subclavian vein receives venous blood from the arm through the axillary vein and from the skin and muscles of the head through the external jugular vein .
- Vertebral vein. The vertebral vein drains the posterior part of the head.
- Internal jugular vein. The internal jugular vein drains the dural sinuses of the brain.
- Brachiocephalic veins. The right and left brachiocephalic veins are large veins that receive venous drainage from the subclavian, vertebral, and internal jugular veins on their respective sides.
- Azygos vein. The azygos vein is a single vein that drains the thorax and enters the superior vena cava just before it joins the heart.
Veins Draining into the Inferior Vena Cava
The inferior vena cava, which is much longer than the superior vena cava, returns blood to the heart from all body regions below the diaphragm.
- Tibial veins. The anterior and posterior tibial veins and the fibular vein drain the leg; the posterior tibial veins become the popliteal vein at the knee and then the femoral vein in the thigh; the femoral vein becomes the external iliac vein as it enters the pelvis.
- Great saphenous veins. The great saphenous veins are the longest veins in the body; they begin at the dorsal venous arch in the foot and travel up the medial aspect of the leg to empty into the femoral vein in the thigh.
- Common iliac vein. Each common iliac vein is formed by the union of the external iliac vein and the internal iliac vein which drains the pelvis.
- Gonadal vein. The right gonadal vein drains the right ovary in females and the right testicles in males; the left gonadal vein empties into the left renal veins superiorly.
- Renal veins. The right and left renal veins drain the kidneys.
- Hepatic portal vein. The hepatic portal vein is a single vein that drains the digestive tract organs and carries this blood through the liver before it enters the systemic circulation.
- Hepatic veins. The hepatic veins drain the liver.
Physiology of the Heart
As the heart beats or contracts, the blood makes continuous round trips- into and out of the heart, through the rest of the body, and then back to the heart- only to be sent out again.
The spontaneous contractions of the cardiac muscle cells occurs in a regular and continuous way, giving rhythm to the heart.
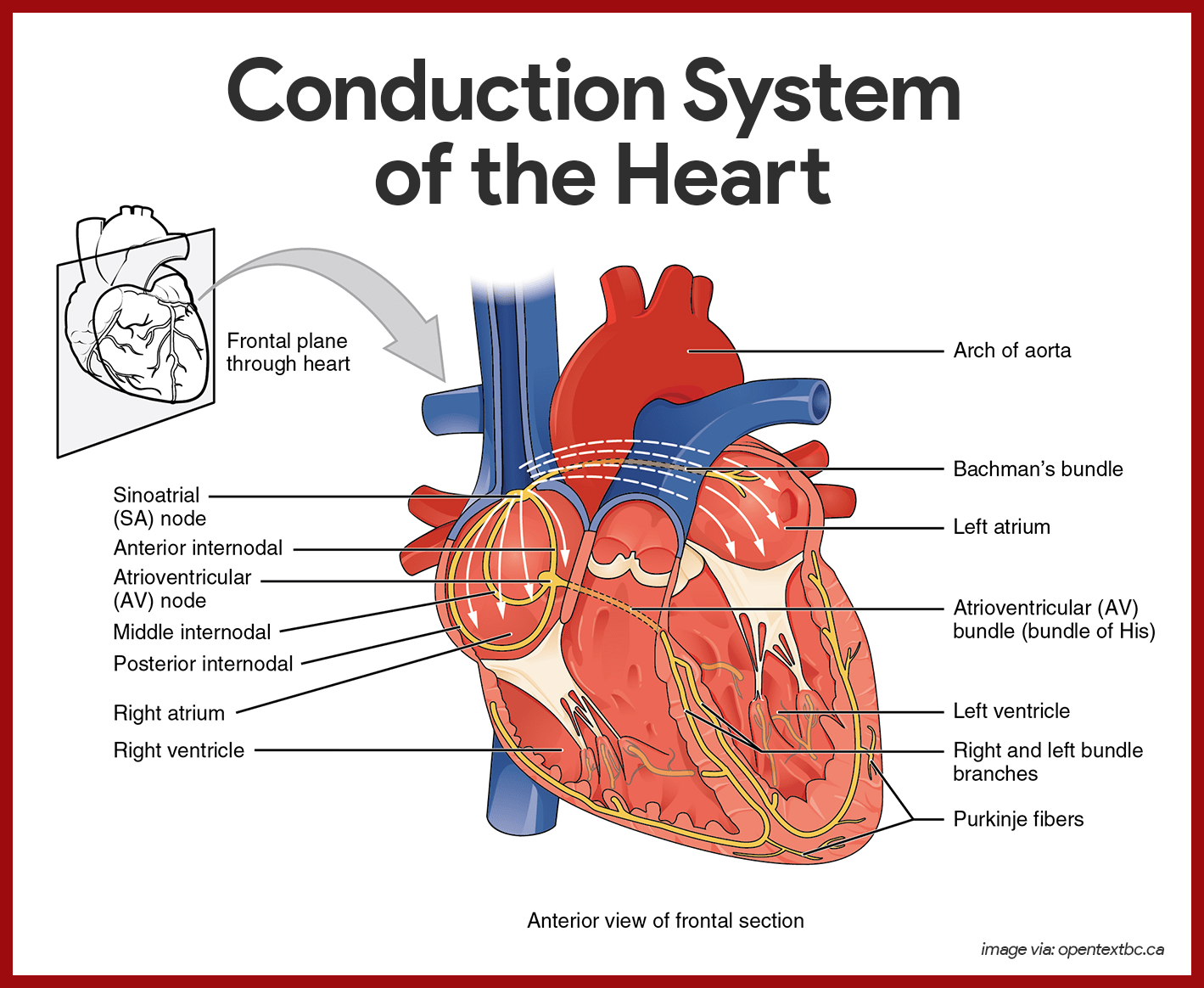
- Cardiac muscle cells. Cardiac muscle cells can and do contract spontaneously and independently, even if all nervous connections are severed.
- Rhythms. Although cardiac muscles can beat independently, the muscle cells in the different areas of the heart have different rhythms.
- Intrinsic conduction system. The intrinsic conduction system, or the nodal system , that is built into the heart tissue sets the basic rhythm.
- Composition. The intrinsic conduction system is composed of a special tissue found nowhere else in the body; it is much like a cross between a muscle and nervous tissue.
- Function. This system causes heart muscle depolarization in only one direction- from the atria to the ventricles; it enforces a contraction rate of approximately 75 beats per minute on the heart, thus the heart beats as a coordinated unit.
- Sinoatrial (SA) node. The SA node has the highest rate of depolarization in the whole system, so it can start the beat and set the pace for the whole heart; thus the term “ pacemaker “.
- Atrial contraction. From the SA node, the impulse spread through the atria to the AV node, and then the atria contract.
- Ventricular contraction. It then passes through the AV bundle, the bundle branches, and the Purkinje fibers, resulting in a “wringing” contraction of the ventricles that begins at the heart apex and moves toward the atria.
- Ejection. This contraction effectively ejects blood superiorly into the large arteries leaving the heart.
The conduction system occurs systematically through:
- SA node. The depolarization wave is initiated by the sinoatrial node.
- Atrial myocardium. The wave then successively passes through the atrial myocardium.
- Atrioventricular node. The depolarization wave then spreads to the AV node, and then the atria contract.
- AV bundle. It then passes rapidly through the AV bundle.
- Bundle branches and Purkinje fibers. The wave then continues on through the right and left bundle branches, and then to the Purkinje fibers in the ventricular walls, resulting in a contraction that ejects blood, leaving the heart.
In a healthy heart, the atria contract simultaneously, then, as they start to relax, contraction of the ventricles begins.
- Systole. Systole means heart contraction .
- Diastole. Diastole means heart relaxation .
- Cardiac cycle. The term cardiac cycle refers to the events of one complete heartbeat, during which both atria and ventricles contract and then relax.
- Length. The average heart beats approximately 75 times per minute, so the length of the cardiac cycle is normally about 0.8 seconds .
- Mid-to-late diastole. The cycle starts with the heart in complete relaxation ; the pressure in the heart is low, and blood is flowing passively into and through the atria into the ventricles from the pulmonary and systemic circulations; the semilunar valves are closed, and the AV valves are open; then the atria contract and force the blood remaining in their chambers into the ventricles.
- Ventricular systole. Shortly after, the ventricular contraction begins, and the pressure within the ventricles increases rapidly, closing the AV valves; when the intraventricular pressure is higher than the pressure in the large arteries leaving the heart, the semilunar valves are forced open, and blood rushes through them out of the ventricles; the atria are relaxed, and their chambers are again filling with blood.
- Early diastole. At the end of systole, the ventricles relax, the semilunar valves snap shut, and for a moment the ventricles are completely closed chambers; the intraventricular pressure drops and the AV valves are forced open; the ventricles again begin refilling rapidly with blood, completing the cycle.
- First heart sound. The first heart sound, “lub” , is caused by the closing of the AV valves.
- Second heart sound. The second heart sound, “dub” , occurs when the semilunar valves close at the end of systole.
Cardiac output is the amount of blood pumped out by each side of the heart in one minute. It is the product of the heart rate and the stroke volume .
- Stroke volume. Stroke volume is the volume of blood pumped out by a ventricle with each heartbeat.
- Regulation of stroke volume . According to Starling’s law of the heart , the critical factor controlling stroke volume is how much the cardiac muscle cells are stretched just before they contract; the more they are stretched , the stronger the contraction will be; and anything that increases the volume or speed of venous return also increases stroke volume and force of contraction.
- Factors modifying basic heart rate. The most important external influence on heart rate is the activity of the autonomic nervous system , as well as physical factors (age, gender, exercise, and body temperature).
A fairly good indication of the efficiency of a person’s circulatory system can be obtained by taking arterial blood and blood pressure measurements.
Arterial pulse pressure and blood pressure measurements, along with those of respiratory rate and body temperature, are referred to collectively as vital signs in clinical settings.
- Arterial pulse. The alternating expansion and recoil of an artery that occurs with each beat of the left ventricle create a pressure wave-a pulse- that travels through the entire arterial system.
- Normal pulse rate. Normally, the pulse rate (pressure surges per minute) equals the heart rate, so the pulse averages 70 to 76 beats per minute in a normal resting person.
- Pressure points. There are several clinically important arterial pulse points, and these are the same points that are compressed to stop blood flow into distal tissues during hemorrhage , referred to as pressure points.
- Blood pressure. Blood pressure is the pressure the blood exerts against the inner walls of the blood vessels, and it is the force that keeps blood circulating continuously even between heartbeats.
- Blood pressure gradient. The pressure is highest in the large arteries and continues to drop throughout the systemic and pulmonary pathways, reaching either zero or negative pressure at the venae cavae.
- Measuring blood pressure. Because the heart alternately contracts and relaxes, the off-and-on flow of the blood into the arteries causes the blood pressure to rise and fall during each beat, thus, two arterial blood pressure measurements are usually made: systolic pressure (the pressure in the arteries at the peak of ventricular contraction) and diastolic pressure (the pressure when the ventricles are relaxing).
- Peripheral resistance. Peripheral resistance is the amount of friction the blood encounters as it flows through the blood vessels.
- Neural factors. The parasympathetic division of the autonomic nervous system has little or no effect on blood pressure, but the sympathetic division has the major action of causing vasoconstriction or narrowing of the blood vessels, which increases blood pressure.
- Renal factors. The kidneys play a major role in regulating arterial blood pressure by altering blood volume, so when blood pressure increases beyond normal, the kidneys allow more water to leave the body in the urine , then blood volume decreases which in turn decreases blood pressure.
- Temperature. In general, cold has a vasoconstricting effect, while heat has a vasodilating effect.
- Chemicals. Epinephrine increases both heart rate and blood pressure; nicotine increases blood pressure by causing vasoconstriction; alcohol and histamine cause vasodilation and decreased blood pressure.
- Diet. Although medical opinions tend to change and are at odds from time to time, it is generally believed that a diet low in salt , saturated fats , and cholesterol help to prevent hypertension , or high blood pressure.
The right and left sides of the heart work together in achieving a smooth-flowing blood circulation .
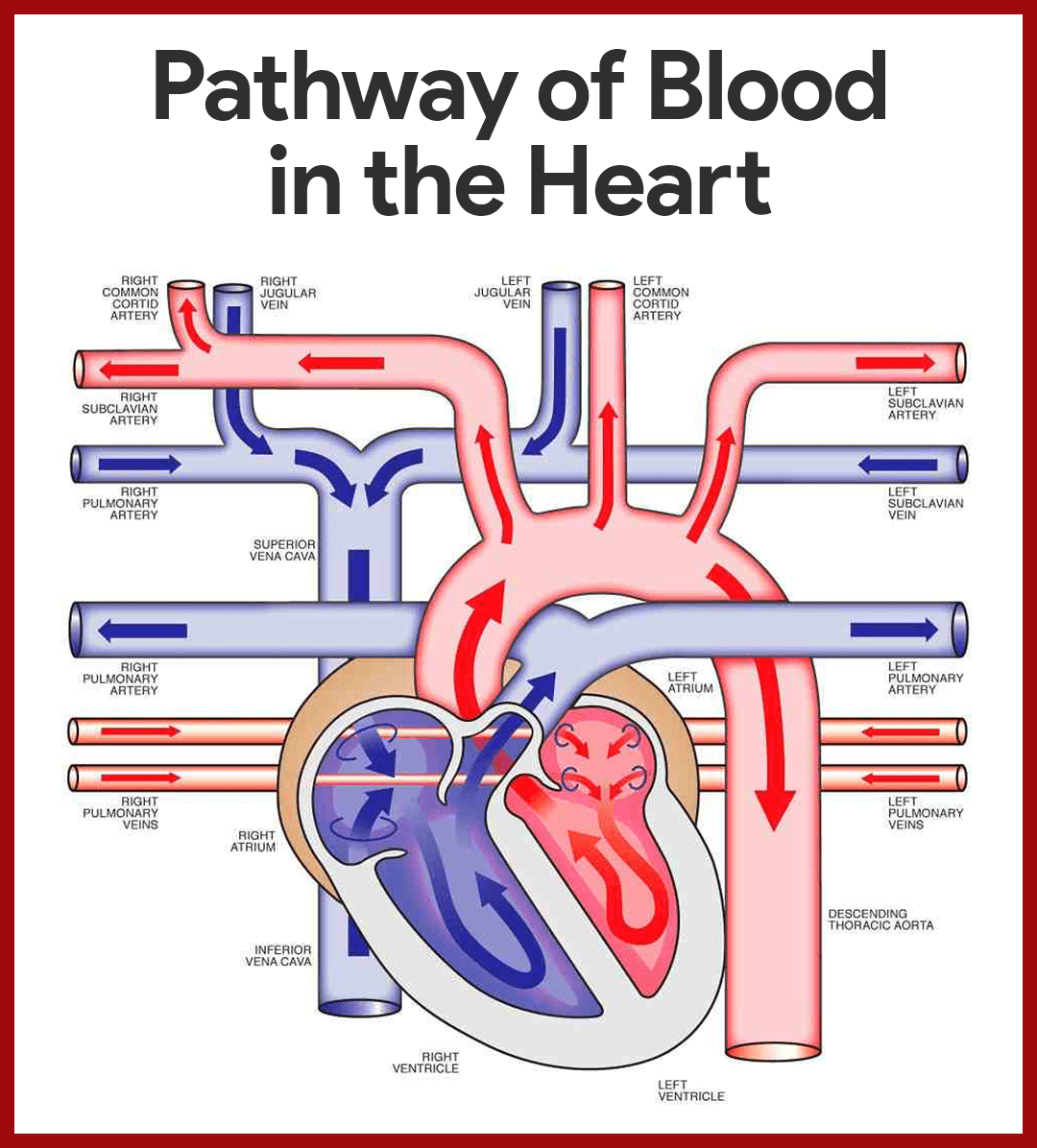
- Entrance to the heart. Blood enters the heart through two large veins, the inferior and superior vena cava, emptying oxygen-poor blood from the body into the right atrium of the heart.
- Atrial contraction. As the atrium contracts, blood flows from the right atrium to the right ventricle through the open tricuspid valve.
- Closure of the tricuspid valve. When the ventricle is full, the tricuspid valve shuts to prevent blood from flowing backward into the atria while the ventricle contracts.
- Ventricle contraction. As the ventricle contracts, blood leaves the heart through the pulmonic valve, into the pulmonary artery, and to the lungs where it is oxygenated.
- Oxygen-rich blood circulates. The pulmonary vein empties oxygen-rich blood from the lungs into the left atrium of the heart.
- Opening of the mitral valve. As the atrium contracts, blood flows from your left atrium into your left ventricle through the open mitral valve.
- Prevention of backflow. When the ventricle is full, the mitral valve shuts. This prevents blood from flowing backward into the atrium while the ventricle contracts.
- Blood flow to the systemic circulation. As the ventricle contracts, blood leaves the heart through the aortic valve, into the aorta, and to the body.
Substances tend to move to and from the body cells according to their concentration gradients.
- Capillary network. Capillaries form an intricate network among the body’s cells such that no substance has to diffuse very far to enter or leave a cell.
- Routes. Basically, substances leaving or entering the blood may take one of four routes across the plasma membranes of the single layer of endothelial cells forming the capillary wall.
- Lipid-soluble substances. As with all cells, substances can diffuse directly through their plasma membranes if the substances are lipid-soluble.
- Lipid-insoluble substances. Certain lipid-insoluble substances may enter or leave the blood and/or pass through the plasma membranes within vesicles, that is, by endocytosis or exocytosis .
- Intercellular clefts. Limited passage of fluid and small solutes is allowed by intercellular clefts (gaps or areas of plasma membrane not joined by tight junctions), so most of our capillaries have intercellular clefts.
- Fenestrated capillaries. Very free passage of small solutes and fluid is allowed by fenestrated capillaries, and these unique capillaries are found where absorption is a priority or where filtration occurs.
The capacity of the heart for work decreases with age. Older peoples’ rate is slower to respond to stress and slower to return to normal after periods of physical activity . Changes in arteries occur frequently which can negatively affect blood supply.
Health promotion teaching can include risk detection and reduction for cardiovascular diseases, blood pressure and cholesterol level monitoring, ideal weight maintenance, and a low- sodium diet.
Craving more insights? Dive into these related materials to enhance your study journey!
- Anatomy and Physiology Nursing Test Banks . This nursing test bank includes questions about Anatomy and Physiology and its related concepts such as: structure and functions of the human body, nursing care management of patients with conditions related to the different body systems.
12 thoughts on “Cardiovascular System Anatomy and Physiology”
very informative!
So great work that could help alot of nurses all over the world, I appreciate it so much.
Nurseslabs have done a very nice work. I wish them good health and strength to continue with the good work.
This excerpt was a magnificent essay of the “Heart Human”.My daughter Arlene Rivera is also an RN and this you wrote about all the heart makes me feel better to know about the knowledge you people possess.Thanks.
In the pathway above, the right subclavian vein is incorrectly labeled as the right pulmonary artery.
For the first time since i leave Nursing school I have now fully understood the cardiovascular system. Keep the good work Matt Vera, you are the best.
Hey Alex, Thank you so much for your kind words! I’m thrilled to hear that our explanations have helped you gain a better understanding of the cardiovascular system. It’s always wonderful to see the impact of educational resources on students and professionals alike.
If there are any more topics or concepts within nursing or healthcare that you’d like to explore or if you have any questions, please don’t hesitate to reach out. Your curiosity and dedication to learning are truly commendable! 🩺🫁📚✨
What is the reference?!
terimakasih atas dedikasinya. super
Enjoy your work, I saw an error in the last image. The right subclavian vein was given the wrong name.
I always found it difficult to find nursing resources since a lot of those that I have seen require payment (and pricey at that). I’m glad I found Nurseslabs. It helps me understand topics that confused me as a student and things I need to refresh since I have been in the profession for a while now.
Easily comprehensible, nice description.
Leave a Comment Cancel reply
FREE K-12 standards-aligned STEM
curriculum for educators everywhere!
Find more at TeachEngineering.org .
- TeachEngineering
- Heart to Heart
Lesson Heart to Heart
Grade Level: 11 (9-12)
(four 45-minutes periods or two 90-minute periods)
Lesson Dependency: None
Subject Areas: Biology
- Print lesson and its associated curriculum
Curriculum in this Unit Units serve as guides to a particular content or subject area. Nested under units are lessons (in purple) and hands-on activities (in blue). Note that not all lessons and activities will exist under a unit, and instead may exist as "standalone" curriculum.
- The Mighty Heart
- What's with All the Pressure?
- Model Heart Valves
TE Newsletter
Engineering connection, learning objectives, worksheets and attachments, more curriculum like this, introduction/motivation, associated activities, vocabulary/definitions, user comments & tips.

Engineers begin their work to design solutions to problems by first gathering information in the form of background information about the system they are working with, testing and analysis data that they collect from various sources, and information from experts on the subject matter.
After Part I of this lesson, students should be able to:
- Identify the parts of the heart (left and right ventricles, left and right atria, interventricular septum, mitral valve, tricuspid valve, pulmonary valve, aortic valve, pericardium, valve leaflets, aorta).
- Describe how blood flows through the heart in a specific path.
- Explain how problems with the heart may cause health concerns.
After Part II of this lesson, students should be able to:
- Identify the parts of the human heart on a diagram and with a biological specimen.
- Describe blood flow through the human heart, elaborating on what role each part of the heart plays in this process.
- Define terms associated with the heart and its function.
- Explain what blood pressure is, and take blood pressure using available tools.
Educational Standards Each TeachEngineering lesson or activity is correlated to one or more K-12 science, technology, engineering or math (STEM) educational standards. All 100,000+ K-12 STEM standards covered in TeachEngineering are collected, maintained and packaged by the Achievement Standards Network (ASN) , a project of D2L (www.achievementstandards.org). In the ASN, standards are hierarchically structured: first by source; e.g. , by state; within source by type; e.g. , science or mathematics; within type by subtype, then by grade, etc .
International technology and engineering educators association - technology.
View aligned curriculum
Do you agree with this alignment? Thanks for your feedback!
State Standards
Tennessee - science.
Your grandmother, who has been a non-smoker and relatively healthy throughout her life, has recently noticed that she is becoming increasingly short of breath as she does simple things, such as climbing the steps in her house. She has also noticed that her heart rate increases when she does mild exercise, such as walking to the mailbox or going upstairs. What could be causing this? Is it just due to her getting older? Is there reason to be concerned? What can be done to help her?
The human heart is vital in sustaining homeostasis —the stability or equilibrium in a biological system. In fact, the heart has a specific anatomy that aids in this function. The way the heart is designed determines the path that blood must take through it in order to be pumped around the body.
Lesson Background and Concepts for Teachers
Part I: Legacy Cycle
After presenting the "grandmother" challenge, hand out the Challenge Question Brainstorm Worksheet and ask students to brainstorm ideas about what could be causing the heart condition ( Legacy Cycle Step 2: Generate Ideas ). Hopefully, the challenge information provided will steer students towards a possible cardiac issue, but be prepared for other ideas (such as respiratory issues, infection, etc.). Record all ideas on the classroom board, and group them into student-generated categories. While there is no real lecture to this part of the lesson, it is important to that all students participate in the brainstorming portion of the lesson and record all ideas. In brainstorming, remind students that no ideas are silly, and that all ideas should be heard. Hopefully, students have some early ideas they can share about the heart, but it may be necessary to prompt them if not.
After students have completed brainstorming ideas, read to them (or have them read to themselves) the Cardiac Valve Research: Expert Interview ( Legacy Cycle Step 3: Multiple Perspectives ), which introduces ideas about how heart valves might contribute to health problems. This interview steers them more towards a cardiac issue and a solution. After reading the interview, begin a class discussion about heart defects. (Note: You may need to distinguish between congenital defects (present at birth) and those that develop later in life.)
A congenital heart defect is a condition that approximately 9 of every 1,000 people are born with and affects the structure of the heart and the large blood vessels that directly move blood to and from the heart (aorta, pulmonary arteries, superior and inferior vena cava). These defects can block blood flow or cause blood to flow in irregular patterns through the heart. In some cases, no action needs to be taken, but in other cases, medication or surgery is necessary.
While a congenital heart defect is a condition that some people are born with, many other heart diseases and defects develop through people's lives. These conditions, referred to as cardiovascular or heart disease, affect the heart's valves, muscles and blood vessels, including arteries, capillaries and veins. These diseases include coronary heart disease (which affects the coronary artery that supplies blood to the heart muscles, and can lead to heart attack)s, cardiomyophathy (a disease of the muscles in the heart), hypertensive heart disease (includes complications to the heart due to high blood pressure), valvular heart disease (diseases such as inflammation or stiffness to the heart valves that affects the movement of blood through the heart), and many others.
Part I of the lesson ends with students using the Internet to research possible heart problems by ( Legacy Cycle Step 4: Research and Revise ). They should research the diseases previously mentioned, as well as other heart diseases. Remind students that the goal is to search for information that might be useful in approaching the challenge question. (Note: If no time remains, assign completion of this research as homework.) Suggested search topics include heart valve disease, heart valve problems, cardiac regurgitation and heart function.
Part II: Heart Anatomy and Blood Flow
Part II of the lesson (Days 2-4) utilizes Legacy Cycle Step 4: Research and Revise in that students learn about the form and function of the heart, as well as about blood flow through the heart's chambers. This information is useful in later understanding the concept of blood pressure, as well as the stresses placed on heart valves and the problems caused by such stress. Students also research the anatomy of the heart by dissecting a sheep heart in the associated activity, The Mighty Heart .
On Day 2 of the lesson, provide a class lecture using The Human Heart and Blood Flow Presentation (a PowerPoint file) and the suggested script below, on heart anatomy and blood flow. The purpose of the lecture is to ensure students understand how the heart is structured and how it works; spending a quality amount of time on this background information ensures student mastery of heart form and function and lends clarity to the activities.
The information below is a suggested script for the PowerPoint presentation. While intended to map to the slides, it is also great resource information on its own, or in conjunction with detailed heart photographs or diagrams.
Slide 1: Title: The Human Heart and Blood Flow
Slide 2: The human heart is a muscular organ located in the thoracic cavity, nestled between the two lungs and very slightly to the left of center. For adult humans, it is about the size of their clenched fists; for children, it is about the size of their clenched fists, and grows as they grow. The heart weighs approximately ½ pound, but it is normal to vary in size, just as the overall size of people varies.
Slide 3: The heart, like many organs in the body, is covered by a protective membrane. This membrane is called the pericardium . The pericardium also holds fluid, which adds additional protection to the heart. This fluid is called pericardial fluid . The heart itself is composed of muscle tissue, and is subdivided into three layers:
- Epicardium — this is the outermost layer of the heart, and it helps to reduce friction by containing some fat amongst the coronary arteries.
- Myocardium — this thick layer of cardiac muscle is the part of the heart that contracts to create a pumping action. It is very thick around the left ventricle because of the amount of force needed to move the blood from the heart to the rest of the body.
- Endocardium — this is the innermost layer of the heart, and comes into physical contact with the blood. This layer lines the two atria and the ventricles.
Slide 4-5: The heart is a pump that is designed to move blood through the human body. It does this by contractions of the myocardium, thus causing the chambers of the heart to compress and push the blood within. Valves serve as one-way doors, separating the chambers of the heart and the vessels that lead out of the heart. These valves prevent blood from moving in the wrong direction as it moves through and out of the heart. Contractions occur at an average rate of 70 beats per minute (bpm), providing the movement of a continual flow of blood throughout the body.
Slides 6-7: Blood moving through the heart is cyclic, so we start with blood entering the heart after it has been through the rest of the body. We call this blood deoxygenated because the cells of the body have diffused the oxygen from the red blood cells for use in cellular respiration. Deoxygenated blood follows the following path:
- Superior and inferior vena cava — deoxygenated blood enters the heart from these two veins. The superior vena cava drains the upper portions of the body (head and arms), while the inferior vena cave drains the lower parts of the body. This blood enters the...
- Right atrium — deoxygenated blood enters the heart through this chamber. The coronary sinus is another smaller vein that drains the myocardium in to this chamber. When the atria contract, this pushes blood down through the...
- Tricuspid valve — a three-flap valve that opens whenever blood is pushed through it by the contractions of the atria. This valve also closes whenever the atria relax because of the change in pressure from the blood. To prevent the valves from folding back the incorrect way, they are held in place by long fibers called chordae tendineae.
- Right ventricle — this chamber receives deoxygenated blood from the right atrium, and contracts to push blood up to the lungs. This muscular chamber has thinner walls than the left ventricle simply because the distance the right ventricle has to pump blood is shorter. As it leaves the right ventricle, the blood passes through the...
- Pulmonary (semilunar) valve — this valve also has three leaflets (cusps) that close to prevent backflow (regurgitation) of blood. From here, blood travels into the...
- Pulmonary arteries — these arteries carry deoxygenated blood from the heart to the lungs. This is the only artery in the body to carry oxygen-poor blood, because it is on its way to the lungs to pick up more oxygen.
- Pulmonary veins — re-oxygenated blood reenters the heart via these veins, which are the only veins in the body to carry oxygen-rich blood. This blood reenters the heart through the...
- Left atrium — this chamber contracts with the right atrium, and pushes blood through the...
- Mitril (bicuspid) valve — this valve has two leaflets, and also has the chordae tendineae to reinforce them.
- Left ventricle — this chamber receives blood from the left ventricle, and is responsible for contracting to push blood out through the vessels of the body. Because of this task, the myocardium that makes up the walls of the left ventricle is much thicker. Also, the left and right ventricles are separated by a myocardial wall called the interventricular septum. Blood leaving this chamber moves through the...
- Aortic (semilunar) valve — this valve works much the same way as the pulmonary valve works.
- Aorta — this is the largest artery of the body, receiving oxygen-rich blood from the left ventricle and moving it through the rest of the body via other smaller arteries and veins.
Have students continue their research on congenital heart defects and the nature and side effects of valve disease for additional learning opportunities (or assign this work as homework). Many online resources are at students' disposal. A focused internet search using the keywords previously mentioned yields hundreds of content-rich documents.
Specifically, additional information on congenital heart defects can be found at: http://kidshealth.org/parent/medical/heart/congenital_heart_defects.html#
And, additional information on valve disease can be found at: http://www.medicinenet.com/heart_valve_disease/article.htm
- The Mighty Heart - Students experience firsthand the amazing heart by dissection of a sheep's heart. They identify all the structural components and draw their own labeled diagrams.
- What's with All the Pressure? - Measuring blood pressure is an excellent way to assess circulatory system and heart health. Students learn and practice measuring blood pressure using blood pressure cuffs and stethoscopes. They learn about blood pressure, how it is measured, and how it is related to the structure of the heart and its functioning.
aorta: The largest artery of the body; it takes blood from the left ventricle and moves it to the body.
atria: The two chambers of the heart that receive blood from the body.
congenital: Congenital defects are those present at birth and usually refer to a disorder. Congenital defects can negatively influence homeostasis if referring to a disease (vs. a defect).
endocardium: The inner most layer of the heart that touches blood that is flowing through the heart
epicardium: A tissue layer that covers the myocardium of the heart and makes up the outside borders of the heart.
myocardium: Thick muscle tissue that makes up the middle layer of the heart.
pericardium: A membrane that covers and protects the heart.
pulmonary circulation: The movement of blood between the heart and the lungs.
systemic circulation: The movement of blood between the heart and the body (excluding the lungs).
valve: A flap of tissue that acts as a one-way door to help blood flow in one direction in the heart.
ventricle: A heart chamber that receives blood from the atria and send blood to the body.
Pre-Lesson Assessment
Engineering and the Body Class Discussion: Ask students if they believe engineering has anything to do with the health of the human body. Begin a class discussion to assess how familiar students are with engineering's involvement in the medical industry by asking the following questions:
- Do you think engineers play any role in our health? (Answer: Yes)
- What is an example of an engineer whose work might affect our health? (Possible answers: Biomedical engineers work with doctors and surgeons to design medical technologies, tools, equipment and procedures, chemical engineers design medicines, and civil and environmental engineers create infrastructure that provides drinking water treatment, waste water treatment and air quality, which all have a direct influence on public health.)
- What type of engineer might work hand in hand with a doctor to help a patient with heart disease? (Answer: A biomedical engineer designs technologies that doctors can use, such as stents to open arteries clogged by plaque build-up, artificial heart valves to replace deteriorated or injured heart valves, and artificial hearts that pump blood through the body during surgeries and even after a person's biological heart fails.)
Post-Introduction Assessment
Brainstorming : Assess students' prior knowledge based on their brainstorming session feedback with the Challenge Question Brainstorm Worksheet . Gauge what they already know about the heart from their responses.
Lesson Summary Assessment
Heart Disease and Defects Research: Have students conduct Internet research to learn more about heart diseases as well as various defects. Require students to research at least 10 different types of heart diseases, including at least one disease of the heart valves, take notes, and write brief summaries (two paragraphs) about each disease to turn in for grading. Have them incorporate the vocabulary words—such as left and right atria, left and right ventricle, tricuspid valve, mitral valve, interventricular septum, aorta, aortic valve, superior and inferior vena cava, pulmonary arteries and pulmonary veins—in the summaries.

Students learn how healthy human heart valves function and the different diseases that can affect heart valves. They also learn about devices and procedures that biomedical engineers have designed to help people with damaged or diseased heart valves.

Students learn all about the body's essential mighty organ, the heart, as well as the powerful blood vascular system. This includes information on the many different sizes and pervasiveness of capillaries, veins and arteries, and how they affect blood flow through the system. Then students focus on ...

Students are presented with the unit's grand challenge problem: You are the lead engineer for a biomaterials company that has a cardiovascular systems client who wants you to develop a model that can be used to test the properties of heart valves without using real specimens.

This lesson describes how the circulatory system works, including the heart, blood vessels and blood. Students learn about the chambers and valves of the heart, the difference between veins and arteries, and the different components of blood.

Shier, D., Butler, J,. and Lewis, R. Hole's Human Anatomy & Physiology, Eleventh Edition. New York, NY: McGraw Hill Higher Education, 2007.
Contributors
Supporting program, acknowledgements.
The contents of this digital library curriculum were developed under National Science Foundation RET grant nos. 0338092 and 0742871. However, these contents do not necessarily represent the policies of the National Science Foundation, and you should not assume endorsement by the federal government.
Last modified: September 7, 2017

IMAGES
VIDEO
COMMENTS
Blood flows through your heart, lungs and body in a series of steps. After delivering oxygen and nutrients to all your organs and tissues, your blood enters your heart and flows to your lungs to gain oxygen and get rid of waste. It then flows back to your heart, which pumps the refreshed blood out through your aorta to nourish your body again.
An easy way to see the way blood flows through the heart. Healthcare. 1 of 7. Download Now. Download to read offline. Blood Flow Through the Heart - Download as a PDF or view online for free.
The valves open and shut in time with the pumping action of your heart's chambers. The opening and closing involve a set of flaps called cusps or leaflets. The cusps open to allow blood to flow out of a chamber and close to allow the chamber to refill with blood. Heart valve diseases can cause backflow or slow the flow of blood through the heart.
Anatomy of the heart made easy along with the blood flow through the cardiac structures, valves, atria, and ventricles. Cardiovascular system animation for U...
Pathway of Blood Through the Heart. In this educational lesson, we learn about the blood flow order through the human heart in 14 easy steps, from the superior and inferior vena cava to the atria and ventricles.Come also learn with us the heart's anatomy, including where deoxygenated and oxygenated blood flow, in the superior vena cava, inferior vena cava, atrium, ventricle, aorta, pulmonary ...
The heart is a hollow, muscular organ about the size of a fist. It is responsible for pumping blood through the blood vessels by repeated, rhythmic contractions. The heart is composed of cardiac muscle, an involuntary muscle tissue that is found only within this organ. The term "cardiac" (as in cardiology) means "related to the heart" and comes
The human circulatory system consists of several circuits: The pulmonary circuit provides blood flow between the heart and lungs. The systemic circuit allows blood to flow to and from the rest of the body. The coronary circuit strictly provides blood to the heart (not pictured in the figure below). Image credit: Blood flow from the heart by ...
The right side of the heart pumps blood out into the Pulmonary artery going away from the heart and towards the lungs, this blood still has not been oxygenated! 2. Next the blood enters the lungs and performs gas exchange, the blood now has high O2 and goes to the pulmonary vein back towards the heart. 3.
Oxygenated blood from the left side of the heart gets pumped out of the aorta. From there, blood flows through arteries, arterioles, and then capillaries (tiny blood vessels that transport blood, nutrients, and oxygen to cells). Deoxygenated blood from the capillaries then flows back to the heart through venules, veins, and ultimately through ...
Blood Flow Through the Heart . The human heart is primarily comprised of four chambers. The two upper chambers are called the atria, the remaining two lower chambers are the ventricles. The right and left sides of the heart are separated by a muscle called the "septum." Both sides work together to efficiently circulate the blood.
Overview of the main coronary arteries and cardiac veins. Coronary arteries and cardiac veins. The heart is a muscular, four-chambered organ that is responsible for distributing blood throughout the body. The continuous activity of the heart creates a large demand for nutrients to be delivered to cardiac tissue and for waste to be removed.
Meet the heart! The heart, nestled between the lungs and protected by the rib cage, serves as a powerful pump ensuring blood flow throughout the body. This systemic flow delivers oxygen and nutrients to cells and removes waste. Additionally, the heart manages pulmonary flow, sending blood to the lungs for oxygenation before distributing it to ...
The blood flow through the heart is quite logical. It happens with the heart cycle, which consists of the periodical contraction and relaxation of the atrial and ventricular myocardium (heart muscle tissue). Systole is the period of contraction of the ventricular walls, while the period of ventricular relaxation is known as diastole.
Circulatory system. The circulatory system, also called cardiovascular system, is a vital organ system that delivers essential substances to all cells for basic functions to occur. Also commonly known as the cardiovascular system, is a network composed of the heart as a centralised pump, blood vessels that distribute blood throughout the body, and the blood itself, for transportation of ...
Hemodynamics ultimately begins with the heart which supplies the driving force for all blood flow in the body. Cardiac output propels blood through the arteries and veins as a function of ventricular contraction. Ventricular motion results from the shortening of cardiac myocytes concentrically. This squeezing motion is translated into the cardiac output, which is a function of both heart rate ...
A transverse section through the heart slightly above the level of the atrioventricular septum reveals all four heart valves along the same plane (Figure 19.12). The valves ensure unidirectional blood flow through the heart. Between the right atrium and the right ventricle is the right atrioventricular valve, or tricuspid valve. It typically ...
Step 1 and 6 involve a blood vessel, which makes sense as this is how blood enters and exits that side of the heart. Steps 2-5 involve a chamber, valve, chamber, and valve. So if you remember this general pattern, it will help you recall the order in which blood flows through each side of the heart.
Presentation Transcript. BLOOD FLOW through the HEART. Biology Version: The right and left sides of the heart work together Right Side Blood enters the heart through two large veins, the inferior and superior vena cava, emptying oxygen-poor blood from the body into the right atrium. Left Side The pulmonary vein empties oxygen-rich blood, from ...
The Heart. Lecture Presentation by Lori Garrett, Parkland College. 20-1 Describe the anatomy of the heart, including vascular supply and pericardium structure, and trace the flow of blood through the heart, identifying the major blood vessels, chambers, and heart valves. 20-2 Explain the events of an action potential in cardiac muscle, indicate ...
Check out this medical presentation on Atrium, which is titled "The Cardiovascular System: The Heart", to know about the heart anatomy and the cardiovascular system. ... Chapter 18, Cardiovascular System 47 Cardiac Cycle Cardiac cycle refers to all events associated with blood flow through the heart Systole - contraction of heart muscle ...
Variations in the rate and force of heart contraction match blood flow to the changing metabolic needs of the tissues during rest, exercise, and changes in body position. Producing blood pressure. Contractions of the heart produce blood pressure, which is needed for blood flow through the blood vessels. Securing one-way blood flow.
If the pulmonary pressures rise enough, they may force blood into the systemic circuit through the ductus arteriosus. This condition—a patent ductus arteriosus— creates a "right-to-left shunt.". Because the circulating blood is not adequately oxygenated, it develops a deep red color.
Describe how blood flows through the heart in a specific path. Explain how problems with the heart may cause health concerns. ... On Day 2 of the lesson, provide a class lecture using The Human Heart and Blood Flow Presentation (a PowerPoint file) and the suggested script below, on heart anatomy and blood flow. The purpose of the lecture is to ...