Advances in Breast Cancer Research
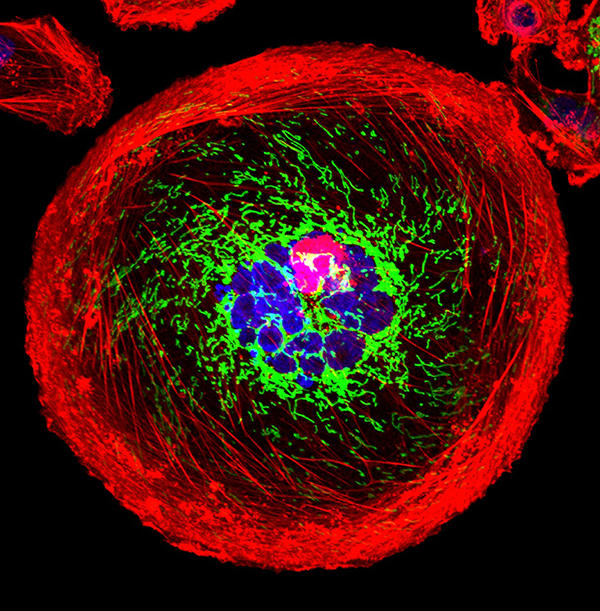
A polyploid giant cancer cell (PGCC) from triple-negative breast cancer.
NCI-funded researchers are working to advance our understanding of how to prevent, detect, and treat breast cancer. They are also looking at how to address disparities and improve quality of life for survivors of the disease.
This page highlights some of what's new in the latest research for breast cancer, including new clinical advances that may soon translate into improved care, NCI-supported programs that are fueling progress, and research findings from recent studies.

Early Detection of Breast Cancer
Breast cancer is one of a few cancers for which an effective screening test, mammography , is available. MRI ( magnetic resonance imaging ) and ultrasound are also used to detect breast cancer, but not as routine screening tools for people with average risk.
Ongoing studies are looking at ways to enhance current breast cancer screening options. Technological advances in imaging are creating new opportunities for improvements in both screening and early detection.
One technology advance is 3-D mammography , also called breast tomosynthesis . This procedure takes images from different angles around the breast and builds them into a 3-D-like image. Although this technology is increasingly available in the clinic, it isn’t known whether it is better than standard 2-D mammography , for detecting cancer at a less advanced stage.
NCI is funding a large-scale randomized breast screening trial, the Tomosynthesis Mammographic Imaging Screening Trial (TMIST) , to compare the number of advanced cancers detected in women screened for 5 years with 3-D mammography with the number detected in women screened with 2-D mammography.
Two concerns in breast cancer screening, as in all cancer screening, are:
- the potential for diagnosing tumors that would not have become life-threatening ( overdiagnosis )
- the possibility of receiving false-positive test results, and the anxiety that comes with follow-up tests or procedures
As cancer treatment is becoming more individualized, researchers are looking at ways to personalize breast cancer screening. They are studying screening methods that are appropriate for each woman’s level of risk and limit the possibility of overdiagnosis.
For example, the Women Informed to Screen Depending on Measures of Risk (WISDOM) study aims to determine if risk-based screening—that is, screening at intervals that are based on each woman’s risk as determined by her genetic makeup, family history , and other risk factors—is as safe, effective, and accepted as standard annual screening mammography.
WISDOM is also making a focused effort to enroll Black women in the trial. Past studies tended to contain a majority of White women and therefore, there is less data on how screening can benefit Black women. Researchers are taking a number of steps to include as many Black women as possible in the study while also increasing the diversity of all women enrolled.
Breast Cancer Treatment
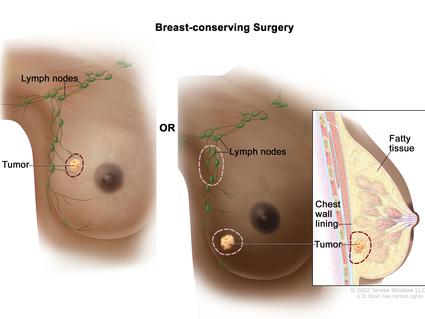
The mainstays of breast cancer treatment are surgery , radiation , chemotherapy , hormone therapy , and targeted therapy . But scientists continue to study novel treatments and drugs, along with new combinations of existing treatments.
It is now known that breast cancer can be divided into subtypes based on whether they:
- are hormone receptor (HR) positive which means they express estrogen and/or progesterone receptors ( ER , PR )
Shortening Radiation Therapy for Some with Early Breast Cancer
A condensed course was as effective and safe as the standard course for women with higher-risk early-stage breast cancer who had a lumpectomy.
As we learn more about the subtypes of breast cancer and their behavior, we can use this information to guide treatment decisions. For example:
- The NCI-sponsored TAILORx clinical trial. The study, which included patients with ER-positive, lymph node-negative breast cancer, found that a test that looks at the expression of certain genes can predict which women can safely avoid chemotherapy.
- The RxPONDER trial found that the same gene expression test can also be used to determine treatment options in women with more advanced breast cancer. The study found that some postmenopausal women with HR positive, HER-2 negative breast cancer that has spread to several lymph nodes and has a low risk of recurrence do not benefit from chemotherapy when added to their hormone therapy.
- The OFSET trial is comparing the addition of chemotherapy to usual treatment ( ovarian function suppression plus hormone therapy) to usual treatment alone in treating premenopausal estrogen receptor (ER)-positive/HER2-negative breast cancer patients who are at high risk of their cancer returning. This will help determine whether or not adding chemotherapy helps prevent the cancer from returning.
Genomic analyses, such as those carried out through The Cancer Genome Atlas (TCGA) , have provided more insights into the molecular diversity of breast cancer and eventually could help identify even more breast cancer subtypes. That knowledge, in turn, may lead to the development of therapies that target the genetic alterations that drive those cancer subtypes.
HR-Positive Breast Cancer Treatment
Hormone therapies have been a mainstay of treatment for HR-positive cancer. However, there is a new focus on adding targeted therapies to hormone therapy for advanced or metastatic HR-positive cancers. These treatments could prolong the time until chemotherapy is needed and ideally, extend survival. Approved drugs include:

Drug Combo Effective for Metastatic Breast Cancer in Younger Women
Ribociclib plus hormone therapy were superior to standard chemotherapy combos in a recent trial.
- Palbociclib (Ibrance) , ribociclib (Kisqali) , and everolimus (Afinitor) have all been approved by the FDA for use with hormone therapy for treatment of advanced or metastatic breast cancer. Ribociclib has been shown to increase the survival of patients with metastatic breast cancer . It has also shown to slow the growth of metastatic cancer in younger women when combined with hormone therapy.
- Elacestrant (Orserdu) is approved for HR-positive and HER2-negative breast cancer that has a mutation in the ESR1 gene, and has spread. It is used in postmenopausal women and in men whose cancer has gotten worse after at least one type of hormone therapy.
- Abemaciclib (Verzenio) can be used with or after hormone therapy to treat advanced or metastatic HR-positive, HER2-negative breast cancer. In October 2021, the Food and Drug Administration ( FDA ) approved abemaciclib in combination with hormone therapy to treat some people who have had surgery for early-stage HR-positive, HER2-negative breast cancer.
- Alpelisib (Piqray) is approved to be used in combination with hormone therapy to treat advanced or metastatic HR-positive, HER2-negative breast cancers that have a mutation in the PIK3CA gene .
- Sacituzumab govitecan-hziy (Trodelvy) is used for HR-positive and HER2-negative breast cancer that has spread or can't be removed with surgery. It is used in those who have received hormone therapy and at least two previous treatments. It has shown to extend the amount of time that the disease doesn't get worse ( progression-free survival ) and also shown to improve overall survival .
HER2-Positive Breast Cancer Treatment
The FDA has approved a number of targeted therapies to treat HER2-positive breast cancer , including:
- Trastuzumab (Herceptin) has been approved to be used to prevent a relapse in patients with early-stage HER2-positive breast cancer.
- Pertuzumab (Perjeta) is used to treat metastatic HER2-positive breast cancer, and also both before surgery ( neoadjuvant ) and after surgery ( adjuvant therapy ).
- Trastuzumab and pertuzumab together can be used in combination with chemotherapy to prevent relapse in people with early-stage HER2-positive breast cancer. Both are also used together in metastatic disease, where they delay progression and improve overall survival.
- Trastuzumab deruxtecan (Enhertu) is approved for patients with advanced or metastatic HER2-positive breast cancer who have previously received a HER2-targeted treatment. A 2021 clinical trial showed that the drug lengthened the time that people with metastatic HER2-positive breast cancer lived without their cancer progressing. The trial also showed that it was better at shrinking tumors than another targeted drug, trastuzumab emtansine (Kadcyla).
- Tucatinib (Tukysa) is approved to be used in combination with trastuzumab and capecitabine (Xeloda) for HER2-positive breast cancer that cannot be removed with surgery or is metastatic. Tucatinib is able to cross the blood–brain barrier, which makes it especially useful for HER2-positive metastatic breast cancer, which tends to spread to the brain.
- Lapatinib (Tykerb) has been approved for treatment of some patients with HER2-positive advanced or metastatic breast cancer, together with capecitabine or letrozole.
- Neratinib Maleate (Nerlynx) can be used in patients with early-stage HER2-positive breast cancer and can also be used together with capecitabine (Xeloda) in some patients with advanced or metastatic disease.
- Ado-trastuzumab emtansine (Kadcyla) is approved to treat patients with metastatic HER2-positive breast cancer who have previously received trastuzumab and a taxane . It's also used in some patients with early-stage HER2-positive breast cancer who have completed therapy before surgery ( neoadjuvant ) and have residual disease at the time of surgery.
HER2-Low Breast Cancer
A newly defined subtype, HER2-low, accounts for more than half of all metastatic breast cancers. HER2-low tumors are defined as those whose cells contain lower levels of the HER2 protein on their surface. Such tumors have traditionally been classified as HER2-negative because they did not respond to drugs that target HER2.
However, in a clinical trial, trastuzumab deruxtecan (Enhertu) improved the survival of patients with HER2-low breast cancer compared with chemotherapy , and the drug is approved for use in such patients.
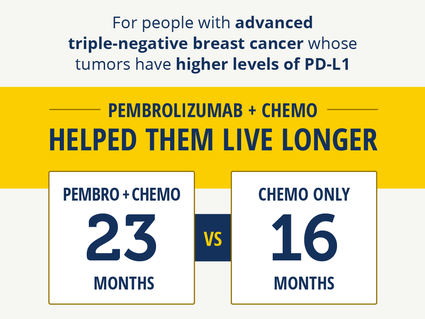
Immunotherapy Improves Survival in Triple-Negative Breast Cancer
For patients whose tumors had high PD-L1 levels, pembrolizumab with chemo helped them live longer.
Triple-Negative Breast Cancer Treatment
Triple-negative breast cancers (TNBC) are the hardest to treat because they lack both hormone receptors and HER2 overexpression , so they do not respond to therapies directed at these targets. Therefore, chemotherapy is the mainstay for treatment of TNBC. However, new treatments are starting to become available. These include:
- Sacituzumab govitecan-hziy (Trodelvy) is approved to treat patients with TNBC that has spread to other parts of the body . Patients must have received at least two prior therapies before receiving the drug.
- Pembrolizumab (Keytruda) is an immunotherapy drug that is approved to be used in combination with chemotherapy for patients with locally advanced or metastatic TNBC that has the PD-L1 protein. It may also be used before surgery (called neoadjuvant ) for patients with early-stage TNBC, regardless of their PD-L1 status.
- PARP inhibitors, which include olaparib (Lynparza) and talazoparib (Talzenna) , are approved to treat metastatic HER2-negative or triple-negative breast cancers in patients who have inherited a harmful BRCA gene mutation. Olaparib is also approved for use in certain patients with early-stage HER2-negative or triple-negative breast cancer.
- Drugs that block the androgen receptors or prevent androgen production are being tested in a subset of TNBC that express the androgen receptor.
For a complete list of drugs for breast cancer, see Drugs Approved for Breast Cancer .
NCI-Supported Breast Cancer Research Programs
Many NCI-funded researchers working at the NIH campus, as well as across the United States and world, are seeking ways to address breast cancer more effectively. Some research is basic, exploring questions as diverse as the biological underpinnings of cancer and the social factors that affect cancer risk. And some are more clinical, seeking to translate this basic information into improving patient outcomes. The programs listed below are a small sampling of NCI’s research efforts in breast cancer.
TMIST is a randomized breast screening trial that compares two Food and Drug Administration (FDA)-approved types of digital mammography, standard digital mammography (2-D) with a newer technology called tomosynthesis mammography (3-D).
The Breast Specialized Programs of Research Excellence (Breast SPOREs) are designed to quickly move basic scientific findings into clinical settings. The Breast SPOREs support the development of new therapies and technologies, and studies to better understand tumor resistance, diagnosis, prognosis, screening, prevention, and treatment of breast cancer.
The NCI Cancer Intervention and Surveillance Modeling Network (CISNET) focuses on using modeling to improve our understanding of how prevention, early detection, screening, and treatment affect breast cancer outcomes.
The Confluence Project , from NCI's Division of Cancer Epidemiology and Genetics (DCEG) , is developing a research resource that includes data from thousands of breast cancer patients and controls of different races and ethnicities. This resource will be used to identify genes that are associated with breast cancer risk, prognosis, subtypes, response to treatment, and second breast cancers. (DCEG conducts other breast cancer research as well.)
The Black Women’s Health Study (BWHS) Breast Cancer Risk Calculator allows health professionals to estimate a woman’s risk of developing invasive breast cancer over the next 5 years. With the NCI-funded effort, researchers developed a tool to estimate the risk of breast cancer in US Black women. The team that developed the tool hopes it will help guide more personalized decisions on when Black women—especially younger women—should begin breast cancer screening.
The goal of the Breast Cancer Surveillance Consortium (BCSC) , an NCI-funded program launched in 1994, is to enhance the understanding of breast cancer screening practices in the United States and their impact on the breast cancer's stage at diagnosis, survival rates, and mortality.
There are ongoing programs at NCI that support prevention and early detection research in different cancers, including breast cancer. Examples include:
- The Cancer Biomarkers Research Group , which promotes research in cancer biomarkers and manages the Early Detection Research Network (EDRN) . EDRN is a network of NCI-funded institutions that are collaborating to discover and validate early detection biomarkers. Within the EDRN, the Breast and Gynecologic Cancers Collaborative Group conducts research on breast and ovarian cancers.
- NCI's Division of Cancer Prevention houses the Breast and Gynecologic Cancer Research Group which conducts and fosters the development of research on the prevention and early detection of breast and gynecologic cancers.
Breast Cancer Survivorship Research
NCI’s Office of Cancer Survivorship, part of the Division of Cancer Control and Population Sciences (DCCPS), supports research projects throughout the country that study many issues related to breast cancer survivorship. Examples of studies funded include the impact of cancer and its treatment on physical functioning, emotional well-being, cognitive impairment , sleep disturbances, and cardiovascular health. Other studies focus on financial impacts, the effects on caregivers, models of care for survivors, and issues such as racial disparities and communication.
Breast Cancer Clinical Trials
NCI funds and oversees both early- and late-phase clinical trials to develop new treatments and improve patient care. Trials are available for breast cancer prevention , screening , and treatment .
Breast Cancer Research Results
The following are some of our latest news articles on breast cancer research and study updates:
- Can Some People with Breast Cancer Safely Skip Lymph Node Radiation?
- Study Adds to Debate about Mammography in Older Women
- Pausing Long-Term Breast Cancer Therapy to Become Pregnant Appears to Be Safe
- A Safer, Better Treatment Option for Some Younger Women with Breast Cancer
- Shorter Course of Radiation Is Effective, Safe for Some with Early-Stage Breast Cancer
- Pembrolizumab Improves Survival in Advanced Triple-Negative Breast Cancer
View the full list of Breast Cancer Research Results and Study Updates .
- Search by keyword
- Search by citation
Page 1 of 104
Outcomes of sentinel node biopsy according to MRI response in an association with the subtypes in cN1–3 breast cancer after neoadjuvant systemic therapy, multicenter cohort study
This study investigated the feasibility of sentinel lymph node biopsy (SLNB) after neoadjuvant systemic therapy (NAST) in patients with initially high nodal burden.
- View Full Text
Meeting Abstracts from the British Society of Breast Radiology annual scientific meeting 2023
This article is part of a Supplement: Volume 26 Supplement 1
Selective omission of sentinel lymph node biopsy in mastectomy for ductal carcinoma in situ: identifying eligible candidates
Sentinel lymph node biopsy (SLNB) is recommended for patients with ductal carcinoma in situ (DCIS) undergoing mastectomy, given the concerns regarding upstaging and technical difficulties of post-mastectomy SL...
Metabolomics assisted by transcriptomics analysis to reveal metabolic characteristics and potential biomarkers associated with treatment response of neoadjuvant therapy with TCbHP regimen in HER2 + breast cancer
This study aimed to explore potential indicators associated with the neoadjuvant efficacy of TCbHP regimen (taxane, carboplatin, trastuzumab, and pertuzumab) in HER2 + breast cancer (BrCa) patients.
Chitin-mediated blockade of chitinase-like proteins reduces tumor immunosuppression, inhibits lymphatic metastasis and enhances anti-PD-1 efficacy in complementary TNBC models
Chitinase-like proteins (CLPs) play a key role in immunosuppression under inflammatory conditions such as cancer. CLPs are enzymatically inactive and become neutralized upon binding of their natural ligand chi...
Serum protein profiling reveals an inflammation signature as a predictor of early breast cancer survival
Breast cancers exhibit considerable heterogeneity in their biology, immunology, and prognosis. Currently, no validated, serum protein-based tools are available to evaluate the prognosis of patients with early ...
U2AF2-SNORA68 promotes triple-negative breast cancer stemness through the translocation of RPL23 from nucleoplasm to nucleolus and c-Myc expression
Small nucleolar RNAs (snoRNAs) play key roles in ribosome biosynthesis. However, the mechanism by which snoRNAs regulate cancer stemness remains to be fully elucidated.
Clinical factors associated with patterns of endocrine therapy adherence in premenopausal breast cancer patients
Patients with hormone receptor positive breast cancer are recommended at least five years of adjuvant endocrine therapy, but adherence to this treatment is often suboptimal. We investigated longitudinal trends...
Correction: Mcl-1 confers protection of Her2-positive breast cancer cells to hypoxia: therapeutic implications
The original article was published in Breast Cancer Research 2016 18 :26
Exploring the dynamic interplay between exosomes and the immune tumor microenvironment: implications for breast cancer progression and therapeutic strategies
Breast cancer continues to pose a substantial worldwide health concern, demanding a thorough comprehension of the complex interaction between cancerous cells and the immune system. Recent studies have shown th...
Establishing conditions for the generation and maintenance of estrogen receptor-positive organoid models of breast cancer
Patient-derived organoid models of estrogen receptor-positive (ER+) breast cancer would provide a much-needed tool to understand drug resistance and disease progression better. However, the establishment and l...
Factors associated with overall survival in breast cancer patients with leptomeningeal disease (LMD): a single institutional retrospective review
Breast cancer-related leptomeningeal disease (BC-LMD) is a dire diagnosis for 5–8% of patients with breast cancer (BC). We conducted a retrospective review of BC-LMD patients diagnosed at Moffitt Cancer Center...
Paradoxical cancer cell proliferation after FGFR inhibition through decreased p21 signaling in FGFR1-amplified breast cancer cells
Fibroblast growth factors (FGFs) control various cellular functions through fibroblast growth factor receptor (FGFR) activation, including proliferation, differentiation, migration, and survival. FGFR amplific...
Correction: The novel phosphatase NUDT5 is a critical regulator of triple-negative breast cancer growth
The original article was published in Breast Cancer Research 2024 26 :23
Temporal changes in mammographic breast density and breast cancer risk among women with benign breast disease
Benign breast disease (BBD) and high mammographic breast density (MBD) are prevalent and independent risk factors for invasive breast cancer. It has been suggested that temporal changes in MBD may impact futur...
Expression- and splicing-based multi-tissue transcriptome-wide association studies identified multiple genes for breast cancer by estrogen-receptor status
Although several transcriptome-wide association studies (TWASs) have been performed to identify genes associated with overall breast cancer (BC) risk, only a few TWAS have explored the differences in estrogen ...
BIRC5 expression by race, age and clinical factors in breast cancer patients
Survivin/BIRC5 is a proliferation marker that is associated with poor prognosis in breast cancer and an attractive therapeutic target. However, BIRC5 has not been well studied among racially diverse population...
Factors associated with engraftment success of patient-derived xenografts of breast cancer
Patient-derived xenograft (PDX) models serve as a valuable tool for the preclinical evaluation of novel therapies. They closely replicate the genetic, phenotypic, and histopathological characteristics of prima...
TMEM120B strengthens breast cancer cell stemness and accelerates chemotherapy resistance via β1-integrin/FAK-TAZ-mTOR signaling axis by binding to MYH9
Breast cancer stem cell (CSC) expansion results in tumor progression and chemoresistance; however, the modulation of CSC pluripotency remains unexplored. Transmembrane protein 120B (TMEM120B) is a newly discov...
Breast cancer survivors suffering from lymphedema: What really do affect to corporeality/body image? A qualitative study
Breast cancer-related lymphedema is currently one of the most serious complications that most affect the quality of life of women undergoing breast cancer. The aim of this study was to explore in-depth the exp...
Correction: a phase 1b study of zilovertamab in combination with paclitaxel for locally advanced/unresectable or metastatic HER2-negative breast cancer
The original article was published in Breast Cancer Research 2024 26 :32
Breast composition during and after puberty: the Chilean Growth and Obesity Cohort Study
Breast density (BD) is a strong risk factor for breast cancer. Little is known about how BD develops during puberty. Understanding BD trajectories during puberty and its determinants could be crucial for promo...
UCHL1 contributes to insensitivity to endocrine therapy in triple-negative breast cancer by deubiquitinating and stabilizing KLF5
Ubiquitin carboxyl-terminal hydrolase L1 (UCHL1) is a deubiquitinating enzyme that regulates ERα expression in triple-negative cancer (TNBC). This study aimed to explore the deubiquitination substrates of UCHL...
Cell morphology best predicts tumorigenicity and metastasis in vivo across multiple TNBC cell lines of different metastatic potential
Metastasis is the leading cause of death in breast cancer patients. For metastasis to occur, tumor cells must invade locally, intravasate, and colonize distant tissues and organs, all steps that require tumor ...
The role of surgical tissue injury and intraoperative sympathetic activation in postoperative immunosuppression after breast-conserving surgery versus mastectomy: a prospective observational study
Breast cancer is the second most common cause of death from cancer in women worldwide. Counterintuitively, large population-based retrospective trials report better survival after breast-conserving surgery (BC...
HER2-low and tumor infiltrating lymphocytes in triple-negative breast cancer: Are they connected?
Most patients with triple-negative breast cancer (TNBC) are not candidates for targeted therapy, leaving chemotherapy as the primary treatment option. Recently, immunotherapy has demonstrated promising results...
Detection of HER2 expression using 99m Tc-NM-02 nanobody in patients with breast cancer: a non-randomized, non-blinded clinical trial
99m Tc radiolabeled nanobody NM-02 ( 99m Tc-NM-02) is a novel single photon emission computed tomography (SPECT) probe with a high affinity and specificity for human epidermal growth factor receptor 2 (HER2). In thi...
How does weight gain since the age of 18 years affect breast cancer risk in later life? A meta-analysis
Early life factors are important risk factors for breast cancer. The association between weight gain after age 18 and breast cancer risk is inconsistent across previous epidemiologic studies. To evaluate this ...
Clinically relevant gene signatures provide independent prognostic information in older breast cancer patients
The clinical utility of gene signatures in older breast cancer patients remains unclear. We aimed to determine signature prognostic capacity in this patient subgroup.
The FBXW7-binding sites on FAM83D are potential targets for cancer therapy
Increasing evidence shows the oncogenic function of FAM83D in human cancer, but how FAM83D exerts its oncogenic function remains largely unclear. Here, we investigated the importance of FAM83D/FBXW7 interactio...
A risk analysis of alpelisib-induced hyperglycemia in patients with advanced solid tumors and breast cancer
Hyperglycemia is an on-target effect of PI3Kα inhibitors. Early identification and intervention of treatment-induced hyperglycemia is important for improving management of patients receiving a PI3Kα inhibitor ...
Overcoming doxorubicin resistance in triple-negative breast cancer using the class I-targeting HDAC inhibitor bocodepsin/OKI-179 to promote apoptosis
Triple-negative breast cancer (TNBC) is an aggressive breast cancer subtype with a poor prognosis. Doxorubicin is part of standard curative therapy for TNBC, but chemotherapy resistance remains an important cl...
PTHrP intracrine actions divergently influence breast cancer growth through p27 and LIFR
The role of parathyroid hormone (PTH)-related protein (PTHrP) in breast cancer remains controversial, with reports of PTHrP inhibiting or promoting primary tumor growth in preclinical studies. Here, we provide...
Small molecule inhibitor targeting the Hsp70-Bim protein–protein interaction in estrogen receptor-positive breast cancer overcomes tamoxifen resistance
Estrogen receptor (ER) positive patients compromise about 70% of breast cancers. Tamoxifen, an antagonist of ERα66 (the classic ER), is the most effective and the standard first-line drug. However, its efficac...
A phase 1b study of zilovertamab in combination with paclitaxel for locally advanced/unresectable or metastatic HER2-negative breast cancer
Zilovertamab is a humanized monoclonal antibody targeting ROR1, an onco-embryonic antigen expressed by malignant cells of a variety of solid tumors, including breast cancer. A prior phase 1 study showed that z...
The Correction to this article has been published in Breast Cancer Research 2024 26 :46
Augmented interpretation of HER2, ER, and PR in breast cancer by artificial intelligence analyzer: enhancing interobserver agreement through a reader study of 201 cases
Accurate classification of breast cancer molecular subtypes is crucial in determining treatment strategies and predicting clinical outcomes. This classification largely depends on the assessment of human epide...
The prostate-specific membrane antigen holds potential as a vascular target for endogenous radiotherapy with [ 177 Lu]Lu-PSMA-I&T for triple-negative breast cancer
Overexpression of prostate-specific membrane antigen (PSMA) on the vasculature of triple-negative breast cancer (TNBC) presents a promising avenue for targeted endogenous radiotherapy with [ 177 Lu]Lu-PSMA-I&T. Thi...

Metabolic adaptation towards glycolysis supports resistance to neoadjuvant chemotherapy in early triple negative breast cancers
Neoadjuvant chemotherapy (NAC) is the standard of care for patients with early-stage triple negative breast cancers (TNBC). However, more than half of TNBC patients do not achieve a pathological complete respo...
Identification of CD160-TM as a tumor target on triple negative breast cancers: possible therapeutic applications
Despite major therapeutic advances, triple-negative breast cancer (TNBC) still presents a worth prognosis than hormone receptors-positive breast cancers. One major issue relies in the molecular and mutational ...
Contrast-enhanced ultrasound to predict malignant upgrading of atypical ductal hyperplasia
A malignancy might be found at surgery in cases of atypical ductal hyperplasia (ADH) diagnosed via US-guided core needle biopsy (CNB). The objective of this study was to investigate the diagnostic performance ...
MRI-based tumor shrinkage patterns after early neoadjuvant therapy in breast cancer: correlation with molecular subtypes and pathological response after therapy
MRI-based tumor shrinkage patterns (TSP) after neoadjuvant therapy (NAT) have been associated with pathological response. However, the understanding of TSP after early NAT remains limited. We aimed to analyze ...
Are better AI algorithms for breast cancer detection also better at predicting risk? A paired case–control study
There is increasing evidence that artificial intelligence (AI) breast cancer risk evaluation tools using digital mammograms are highly informative for 1–6 years following a negative screening examination. We h...
Prognostic impact of HER2 biomarker levels in trastuzumab-treated early HER2-positive breast cancer
Overexpression of human epidermal growth factor receptor 2 (HER2) caused by HER2 gene amplification is a driver in breast cancer tumorigenesis. We aimed to investigate the prognostic significance of manual sco...
The novel phosphatase NUDT5 is a critical regulator of triple-negative breast cancer growth
The most aggressive form of breast cancer is triple-negative breast cancer (TNBC), which lacks expression of the estrogen receptor (ER) and progesterone receptor (PR), and does not have overexpression of the h...
The Correction to this article has been published in Breast Cancer Research 2024 26 :53
Low-dose acetylsalicylic acid reduces local inflammation and tissue perfusion in dense breast tissue in postmenopausal women
One major risk factor for breast cancer is high mammographic density. It has been estimated that dense breast tissue contributes to ~ 30% of all breast cancer. Prevention targeting dense breast tissue has the ...
Improving lesion detection in mammograms by leveraging a Cycle-GAN-based lesion remover
The wide heterogeneity in the appearance of breast lesions and normal breast structures can confuse computerized detection algorithms. Our purpose was therefore to develop a Lesion Highlighter (LH) that can impro...
TBCRC 039: a phase II study of preoperative ruxolitinib with or without paclitaxel for triple-negative inflammatory breast cancer
Patients with inflammatory breast cancer (IBC) have overall poor clinical outcomes, with triple-negative IBC (TN-IBC) being associated with the worst survival, warranting the investigation of novel therapies. ...
ADAMTS18 deficiency associates extracellular matrix dysfunction with a higher risk of HER2-positive mammary tumorigenesis and metastasis
Human epidermal growth factor receptor 2 (HER2)-positive breast cancer accounts for about 20% of all breast cancer cases and is correlated with a high relapse rate and poor prognosis. ADAMTS18 is proposed as an i...
Development of a machine learning-based radiomics signature for estimating breast cancer TME phenotypes and predicting anti-PD-1/PD-L1 immunotherapy response
Since breast cancer patients respond diversely to immunotherapy, there is an urgent need to explore novel biomarkers to precisely predict clinical responses and enhance therapeutic efficacy. The purpose of our...
Development and prognostic validation of a three-level NHG-like deep learning-based model for histological grading of breast cancer
Histological grade is a well-known prognostic factor that is routinely assessed in breast tumours. However, manual assessment of Nottingham Histological Grade (NHG) has high inter-assessor and inter-laboratory...
- Editorial Board
- Manuscript editing services
- Instructions for Editors
- Sign up for article alerts and news from this journal
- Collections
- Follow us on Twitter
Annual Journal Metrics
2022 Citation Impact 7.4 - 2-year Impact Factor 7.4 - 5-year Impact Factor 1.764 - SNIP (Source Normalized Impact per Paper) 2.408 - SJR (SCImago Journal Rank)
2023 Speed 20 days submission to first editorial decision for all manuscripts (Median) 129 days submission to accept (Median)
2023 Usage 2,432,781 downloads 1,561 Altmetric mentions
- More about our metrics
Breast Cancer Research
ISSN: 1465-542X
- Submission enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 27 May 2023
Global trends and forecasts of breast cancer incidence and deaths
- Yuyan Xu 1 na1 ,
- Maoyuan Gong 1 na1 ,
- Yue Wang 2 ,
- Yang Yang 1 ,
- Shu Liu 2 &
- Qibing Zeng ORCID: orcid.org/0000-0002-6694-1503 1
Scientific Data volume 10 , Article number: 334 ( 2023 ) Cite this article
10k Accesses
25 Citations
10 Altmetric
Metrics details
- Cancer epidemiology
- Risk factors
Breast cancer (BC) is one of the major public health challenges worldwide. Studies that address the new evidence on trends of BC are of great importance for preventing and controlling the occurrence and development of diseases and improving health. The aim of this study was to analyze the outcomes for the global burden of disease (GBD), incidence, deaths, and risk factors for BC from 1990 to 2019, and predict the GBD of BC until 2050 to inform global BC control planning efforts. In this study, the results show that the regions with low levels of socio-demographic index (SDI) will have the largest disease burden of BC in the future. The leading global risk factor for death attributable to BC in 2019 was metabolic risks, followed by behavioral risks. This study supports the worldwide urgent need for comprehensive cancer prevention and control strategies to reduce exposure, early screening, and improve treatment to effectively reduce the GBD of BC.
Similar content being viewed by others
Forecast of a future leveling of the incidence trends of female breast cancer in Taiwan: an age-period-cohort analysis
Yi-Chu Chen, Shih-Yung Su, … Wen-Chung Lee
Trends in female breast cancer incidence, mortality, and survival in Austria, with focus on age, stage, and birth cohorts (1983–2017)
Lazo Ilic, Gerald Haidinger, … Kyriaki Papantoniou
A multilevel assessment of the social determinants associated with the late stage diagnosis of breast cancer
Nayara Priscila Dantas de Oliveira, Marianna de Camargo Cancela, … Dyego Leandro Bezerra de Souza
Introduction
Breast cancer (BC) is a most common malignant tumor, and its global burden of disease (GBD) has become one of the important factors that endanger the health of the world population, especially the health of women 1 . The global BC statistics report shows that in 2020, there will be 2.261 million new cases and 685,000 deaths worldwide, and BC has become the number one malignant tumor in the world 2 . Although some cancer cases cannot be prevented, governments can develop a range of health interventions to minimize exposure to known cancer risk factors, such as environmental factors, lifestyle behaviors, dietary habits, metabolic factors, etc 3 . Therefore, understanding the relative contributions of modifiable risk factors to the GBD of BC and their long-term trends is critical to inform local and global cancer control efforts.
Global Health Data Exchange provides two important research tools (GBD Comparison Tool and GBD Results Tool) that have been open sourced to quantify GBD, assessing GBD by age group, sex and time (1990 to 2019) in countries around the world), attributed to a wide range of modifiable risk factors 4 . GBD 2019 is the latest iteration of the GBD study, which provides an opportunity to assess the global cancer burden attributable to risk factors. Previous studies assessed the global, regional, and national burden of breast cancer until 2017 5 , 6 , 7 , 8 , 9 . A recent study 10 evaluated the GBD of female BC from 1990 to 2019 and predicted the GBD of female BC in 2035. However, these studies know little about the global cancer burden attributable to metabolic, behavioral, diet, physical activity factors and its more longer-term future forecasts to 2050.
In this study, we report for the first time the GBD for BC attributable to a comprehensive inventory of metabolism, behavior, diet, and physical activity from 1990 to 2019, using breast cancer incidence, deaths, and risk factor results. Furthermore, this study provides a new perspective on the attributable cancer burden by estimating the risk-attributable cancer burden at global levels using incidence and deaths.
Global burden of disease and temporal trends of breast cancer
To assess the global GBD and changing trends of BC, the incident cases, death cases and ASR of BC in 1990 and 2019 were calculated, and the estimated annual percentage change (EAPC) was used to demonstrate the temporal trends from 1990 to 2019. The global GBD and temporal trends of BC are presented in Supplementary Tables 1 and 2 . Globally, the incident cases of BC increased from 876,990 in 1990 to 2,002,350 in 2019, and the EAPC for incidence increased by an average 0.33% per year. Although the death cases of BC in 2019 is higher than in 1990 worldwide, the EAPC for deaths decreased by an average 0.56% per year. In terms of gender, the number of cases and ASR of women are higher than that of men, regardless of morbidity and death. However, it is worth noting that the EAPC for incidence in men increased by an average 0.91% per year, which is higher than the woman with 0.36%. And the EAPC for deaths in different gender population both gradually decreased. Compared with other SDI regions, the incident cases, death cases and ASR of BC in high SDI regions were at a higher level. However, it is exciting to note that the EAPC for incidence began to decline in high SDI regions, and the EAPC for deaths also decreased the most in this group. In the other hand, we also observed a fast increase in the EAPC for incidence in the middle SDI regions and the EAPC for deaths in the low SDI regions. Further observation of the GBD and temporal trends of 21 GBD regions found that the highest incident cases and ASR for incidence of BC is in East Asia region, and the largest decline for EAPC is in Central Asia region. Moreover, Western Sub-Saharan Africa is the only region where EAPC for incidence continues to grow. Western Europe, Oceania and High-income North America are the region with higher breast cancer deaths in 1990, but by 2019, only the Oceania region was found to still be at relatively high levels. The EAPC for deaths in the Western Sub-Saharan Africa region increased fast, but High-income North America, Australasia and Western Europe regions decreased more obviously.
Figures 1 and 2 show the GBD of BC incidence and mortality for 204 countries and territories. As shown, the countries with the highest incidence and deaths of ASR in 1990 were concentrated in high-income countries (Figs. 1a and 2a ). However, the top 2 countries with the highest incidence and deaths of ASR in 2019 are not high-income countries, such as Lebanon and Solomon Islands with the highest incidence (Fig. 1b ) and Pakistan and Solomon Islands with the highest death (Fig. 2b ). Subsequently, we further analyzed global changes in cancer case (Figs. 1c and 2c ) and EAPC (Figs. 1d and 2d ) to better indicate temporal trends in GBD. From the perspective of changes in cancer cases, only 2 countries have seen a decline in incidence, while 72 countries have seen a decline in deaths. Among them, 52 countries with an increase for incidence of more than 300%, but only 3 countries had an increase for deaths of more than 300%, and the largest increase was both in the Solomon Islands.
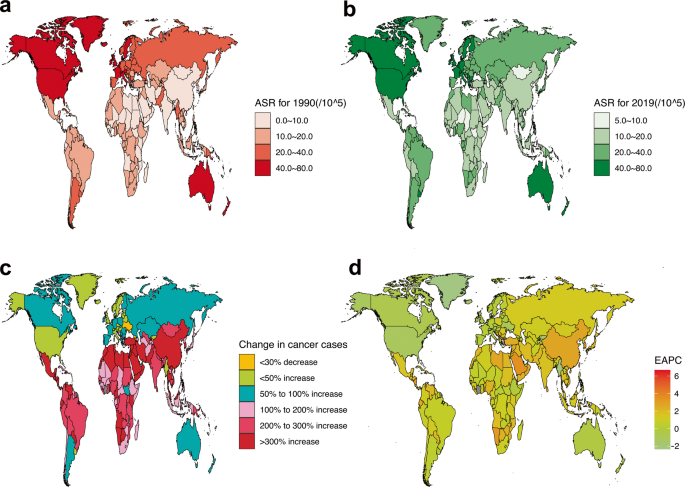
Global GBD and temporal trends of BC incidence in 204 countries or territories. ASR: age standardized rate; BC: breast cancer; EAPC: estimated annual percentage change; GBD: global burden of disease. ( a ) The ASR per 100,000 people in 1990; ( b ) The ASR per 100,000 people in 2019; ( c ) The change in cancer cases; ( d ) EAPC in different countries or territories.
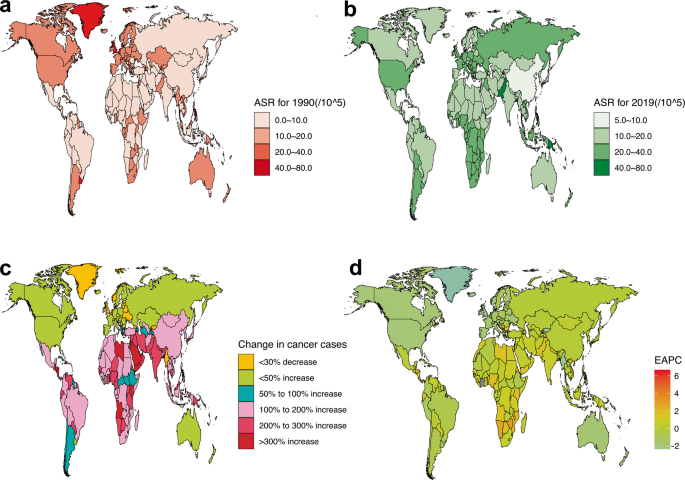
Global GBD and temporal trends of BC deaths in 204 countries or territories. ASR: age standardized rate; BC: breast cancer; EAPC: estimated annual percentage change; GBD: global burden of disease. ( a ) The ASR per 100,000 people in 1990; ( b ) The ASR per 100,000 people in 2019; ( c ) The change in cancer cases; ( d ) EAPC in different countries or territories.
Supplementary Fig. 1 combines EAPC for incidence and deaths data in a hierarchical cluster analysis to identify countries with similar annual growth rates in incidence and deaths. As shown in the multimedia appendices, 35 countries (or territories) were cluster into the significant increase group, including the Northern Mariana Islands, Taiwan (Province of China), Netherlands, Germany, Viet Nam, Gambia, etc . A total of 39 countries (or territories) were categorized into the minor increase group, including United States of America, United Kingdom, Pakistan, Canada, etc . Another 120 countries (or territories) were grouped into the remained stable or minor decrease group, including China, Japan, France, Mexico, and Solomon Islands. The remaining 10 countries (or territories) were categorized into the significant decrease group, including Turkmenistan, Uzbekistan, Puerto Rico, Kazakhstan, Bahrain, Colombia, Singapore, Maldives, Chile.
Global burden of disease of breast cancer attributable to risk factors
The results of GBD of BC attributable to the risk factors were shown in Fig. 3 and Supplementary Figs. 2 and 3 . As revealed in the Figure, the leading risk factor in terms of attributable BC deaths was metabolic risks worldwide, which accounted for 31.98% in 1990, and has a gradual increasing trend in 2019, accounting for 46.87%. Alcohol use, tobacco, dietary risks, and low physical activity were the next greatest risk factors. The percentage of BC deaths due to metabolic risks was significantly heterogeneous all over the world, with the highest percentage observed in Oceania region (55.48% in 1990 and 63.76% in 2019), followed by Southeast Asia region (47.34% in 1990 and 63.69% in 2019). The largest increase in the percentage for BC deaths due to the metabolic risks from 1990 to 2019 are Southern Sub-Saharan Africa (17.66%), South Asia (17.29%), Andean Latin America (16.59%), Southeast Asia (16.35%) regions. At the same time, we also observed a gradual decrease in the percentage of BC deaths due to behavioral risks such as such as alcohol use and tobacco. Dietary risks and low physical activity have remained relatively stable over the past 20 years. When we assessed the time trends of attributable risk factors at the SDI level, we found that the most increase in the percentage for BC deaths due to the metabolic risks from 1990 to 2019 are in the middle (14.42%), low-middle (14.41%) and middle-high (13.29%) SDI areas. Multimedia Appendix 2 shows the two metabolic risks attributable to breast cancer death. As shown in the figure, the global and low, middle-low and high SDI regions accounted for half and half percentage of BC deaths due to high fasting plasma glucose and high body mass index, but the fasting plasma glucose in the middle, middle-high SDI region was very high, accounting for 70.10%~ 84.62%. Furthermore, the proportion of low, low-middle, and middle SDI areas attributed to the high body mass index is increasing, especially in the low-middle SDI areas, from 42.65% in 1990 to 54.70% in 2019.
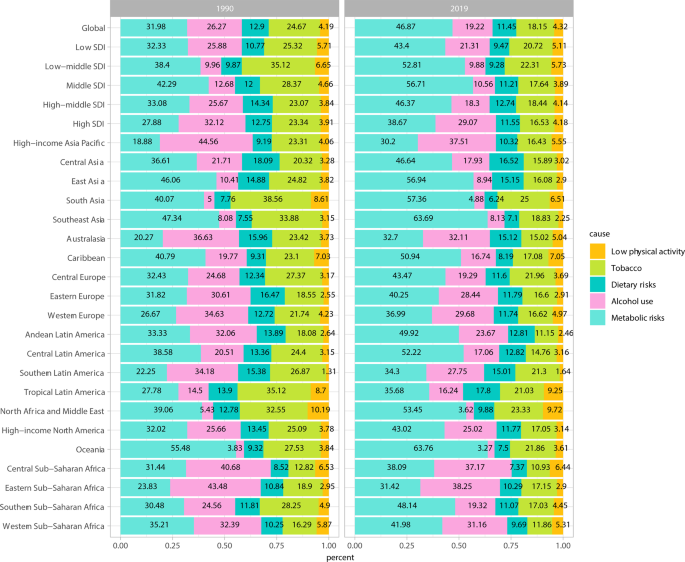
GBD of BC attributable to risk factors in 1990 and 2019. BC: breast cancer; GBD: global burden of disease; SDI, socio-demographic index.
Factors influencing the estimated annual percentage change in the global burden of disease
To better explain GBD in BC, we analyzed influencing factors that may affect EAPC, including ASIR, ASDR, and HDI (which can be used as an indicator of the level and availability of medical care in each country) (Fig. 4 ). As illustrated in the Figs. 4a,b , a significant negative correlation was found between EAPC and ASIR, ASDR in 1990 ( r = −0.607, −0.583; P all < 0.001). In contrast, this negative correlation in 2019 gradually weakened or disappeared. EAPC had a weak negative correlation with ASIR ( r = −0.152; P = 0.030) in 2019, but a positive correlation with ASDR ( r = 0.315; P < 0.001). Figure 4c,d show the correlation between the EAPC and HDI. As revealed in the figure, whether in 1990 or 2019, the relationship between EAPC and HDI is not a simple linear correlation, on the contrary it is more like a “parabola”. when the HDI was limited to below 0.50 in 1990 or 0.55 in 2019, a significant positive correlation was found between EAPC for incidence and deaths and HDI. In contrast, for a HDI above 0.50 in 1990 or 0.55 in 2019, the positive association gradually disappeared, and EAPC for incidence and deaths has a significant negative correlation with HDI in 1990 ( r = −0.312, −0.548; P all < 0.001) and 2019 ( r = −0.300, −0.582; P all < 0.001).
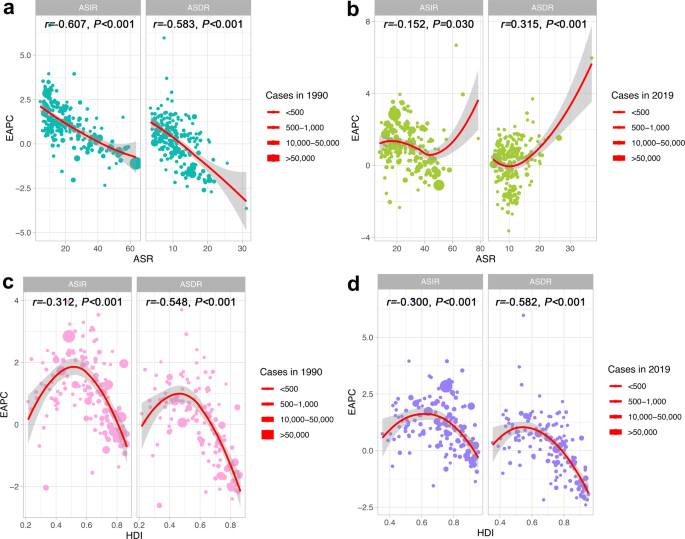
Factors Influencing EAPC in the GBD. ASR: age standardized rate; ASIR: age standardized incidence rate; ASDR: age standardized death rate; BC: breast cancer; EAPC: estimated annual percentage change; GBD: global burden of disease; HDI: human development index. ( a ) The correlation between EAPC and ASR in 1990. ( b ) The correlation between EAPC and ASR in 2019. ( c ) The correlation between EAPC and HDI in 1990. ( d ) The correlation between EAPC and HDI in 2019.
Future forecasts of global burden of disease in breast cancer
Figure 5 show the future forecasts of GBD in BC. As illustrated in the Fig. 5a,b , the ASR of BC incidence in the world will gradually increase. It is estimated that by 2050, the ASR of BC incidence in female will be 59.63 per 100,000, an increase of 32.13% compared with 2019; the ASR of BC incidence in male will be 0.65 per 100,000, an increase of 1.74% compared with 2019. Subsequently, we also estimated the ASR of global BC deaths from 2020 to 2050 (Fig. 5c,d ). Over time, the ASR of BC death in female increased slightly, but the ASR of BC deaths in male gradually decreased. It is estimated that by 2050, the ASR of female BC deaths will be 16.42/100,000, an increase of 4.69% compared with 2019; the ASR of BC deaths in male will be 0.26 cases per 100,000, a decrease of 19.84% compared with 2019. According to the United Nations world population forecast data, there will be 4,781,849 incident cases (4,714,393 women and 67,456 men) and 1,503,694 death cases (1,481,463 women and 22,231 men) of BC in the world in 2050.
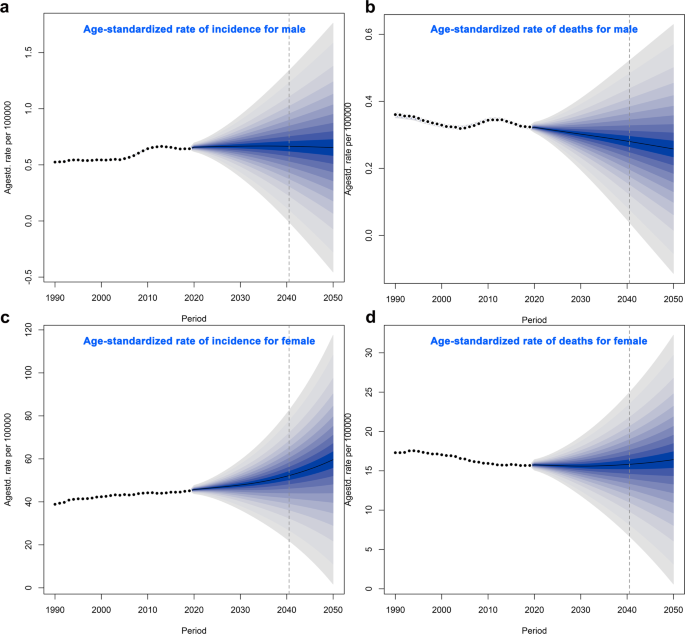
Future Forecasts of GBD in BC. ASIR: age standardized incidence rate; ASDR: age standardized death rate; BC: breast cancer. ( a ) The ASIR per 100,000 for male; ( b ) The ASDR per 100,000 for male; ( c ) The ASIR per 100,000 for female; ( d ) The ASDR per 100,000 for female.
Breast cancer incidence burden
Our analysis found that the global incident cases of BC increased from 876,990 in 1990 to 2,002,350 in 2019, a total increase of 1.28 times. This is an increase of another 5 percentage points compared to the 2017 GBD data for BC 11 , which showed that the global incident cases of BC increased by 123% between 1990 and 2017. Although we have seen a sharp increase in the BC incident cases worldwide in the past 20 years, the ASR has not shown a trend of rapid growth. And this slow growth trend is also confirmed by our EAPC results and other study 11 , which also found that from 1990 to 2017, the incidence of breast cancer worldwide increased by 123%, but the change in ASR was not obvious. Previous study 12 has found that the changes in the number of BC cases are largely attributable to population growth and aging. This seems to explain the findings in this study well, since our study only found a significant increase in the incident cases of BC, not ASR. It suggests that reducing the global population may be one of the key factors in reducing BC incidence.
For the gender, we saw an absolute predominance of women, which is logical, but it is worth noting that the EAPC for incidence in men is significantly higher than that in women and continues to increase at an average rate of 0.91% per year. These results suggest that we should not ignore men in the health monitoring of BC in the future, especially for those who have bad behavior factors, such as smoking, alcohol use. The latest study 1 found that tobacco is the main risk factor of cancer for male, followed by alcohol use, dietary risks and air pollution.
SDI is a composite index calculated based on the total fertility rate of women under the age of 25, the per capita lagged distribution income and the average education level of individuals aged 15 and above 13 . Our results showed that the higher the SDI level, the higher incident cases and ASR of BC, but the EAPC did not appear consistent. On the contrary, in the meddle-high and high SDI regions, the EAPC of BC incidence was significantly reduced, especially in the high SDI region even showed negative growth. These findings were also confirmed by further association analysis, and it was found that EAPC showed a significant negative correlation with ASIR. One possible explanation is that the ASR of BC incidence in these regions was higher in the past, with limited room for increase. Furthermore, due to the general increase in the education level of the population in these areas, people’s awareness of health has been continuously strengthened, which has limited the growth of BC to a certain extent. However, it is worth noting that in low, low-middle, and middle SDI regions, changes in the ASR and EAPC due to population growth and due to the global rise in SDI levels, they are re expected to impose increasing burdens on individuals and societies.
From the analysis of countries or regions, the countries with high ASR of BC incidence 20 years ago were mainly concentrated in high-income countries (such as the United States, New Zealand and the Netherlands), but in 2019, some low-income countries (such as Solomon Islands, Lebanon) rapidly occupy the position of high ASR incidence. These results support our previous hypothesis that low, low-meddle, and middle SDI regions are projected to impose increasing burdens on individuals and society. Furthermore, East Asia is the region with the highest ASR of BC incidence, sub-Saharan Africa is the only region where the EAPC of BC continues to grow, and Solomon Islands is the only country where EAPC has increased by more than 6%. These countries and regions should be the focus of future BC disease burden monitoring.
Further GBD future forecasts for BC demonstrated that that from 2020 to 2050, the global BC incidence and total incidence will increase year by year. Therefore, how to control modifiable risk factors and reduce the incidence of BC becomes the key to alleviating GBD of BC.
Breast cancer deaths burden
ASR for deaths, as one of the commonly used indicators in disease burden research, can measure the level of risk to the population from the perspective of life 9 . Our study demonstrated that the global death cases of BC in 2019 (700,660 cases) was higher than in 1990 (380,910 cases). There will be 1,503,694 death cases (1,481,463 women and 22,231 men) of BC in the world in 2050. These results suggest that the GBD from breast cancer deaths will remain severe for some time to come. The incidence of BC is dominant in females, so the relatively higher death rate in females may be related to the higher incidence of BC in females than in males. Previous studies 9 , 11 have shown that high-income countries such as North America and Western Europe have a higher GBD of BC due to death. Our GBD study based on 1990 also came to a similar conclusion. But what is exciting is that by 2019, the ASR for deaths in high-income countries such as North America and Western Europe has gradually declined the most obvious in all countries. These findings were also confirmed by the results of death cases and death ASR in different SDI index countries and the significant negative association between HDI and EPAC. A logical explanation is that the application in widespread mammography for early-stage BC diagnosis in high-income and high-SDI countries 7 , 14 and improved treatment facilities in terms of chemotherapy, radiation therapy, and targeted approaches may be the underlying reasons for the decline in BC mortality in these countries. In addition, our study also found that the growth of EAPC for deaths was particularly rapid in low and low-medium SDI regions and in sub-Saharan Africa. Possible solutions behind this growing trend are access to widespread mammograms, improved BC awareness, increased exercise and greater access to healthcare, among others. It is worth noting that in low-income countries, individuals suffering from severe illnesses may opt to discontinue their treatment because of the considerable financial burden it places on their families. This decision can lead to a rapid deterioration of their condition and ultimately hasten their demise, a phenomenon known as “near-suicide.” Research indicates that as the severity of the illness increases, patients are more likely to forego treatment due to familial responsibilities 15 . These findings underscore the importance of providing accessible and affordable healthcare for individuals dealing with serious illnesses.
Risk factors attributable to breast cancer burden
The latest research evidence 1 shown that 44.4% of global cancer deaths and 42.0% of global cancer disability-adjusted life years can be attributed to GBD 2019 estimated risk factors. Our study demonstrates that the major risk factor globally attributable to BC deaths is metabolic risks. High body mass index and high fasting glucose have also been identified as potential risk factors attributable to BC deaths 11 , and our study found that the proportion of contribution of the two risk factors was quite different in various SDI regions of the world. In most countries with high SDI, the growth rate of national wealth is also the fastest, and the growth rate of national wealth is often proportional to the increase in body weight 16 . Our study did not observe a significant increase in the proportion of BC death risk attributable to high body mass index in high-income countries, which may be related to the traditional low-calorie diet 17 and high physical activity in the part of countries, such as walking 18 . Conversely, the proportion of BC deaths attributable to high body mass index is increasing in low, low-middle SDI regions. It suggests that the body weight control is the key to reduce the risk of BC disease in the future, in these regions, especially in low-middle SDI region. However, glycemic control may be more important for middle and middle-high SDI regions, where a very high proportion of BC deaths are attributable to high fasting glucose.
Alcohol use is one of the important risk factors for BC death 11 , and a pioneering study 19 has revealed a possible dose-response relationship between alcohol consumption and BC. Our study found that the proportion of disease burden of BC deaths attributable to alcohol use gradually decreased in meddle-high and high SDI countries, which may be very much related to the significant decline in the prevalence of daily alcohol consumption globally 20 . These results may also better explain why the incidence and deaths of BC in high-income countries such as North America and Europe have gradually decreased, despite high-calorie, high-metabolic diets.
The GBD 2019 Study shows that smoking remains the leading cause of cancer death and health loss worldwide 1 . Our study found that the proportion of BC disease burden attributable to smoking decreased gradually over time in low, low- middle, and middle SDI regions, which may be related to the decline in smoking prevalence in these regions. Because previous study 21 has shown that smoking rates decline with the lower SDI. In addition, our study indicates that the dietary risk and low physical activity also play a role in the burden of BC disease. Therefore, reducing the global burden of breast cancer requires a comprehensive cancer prevention and control strategy. On the one hand, reduce the incidence and death of breast cancer by controlling adverse metabolic risks and behavioral risks (such as alcohol use, tobacco, dietary risk, low physical activity); on the other hand, by promoting mammography for early diagnosis of breast cancer, and improvements in effective treatments to effectively reduce the global burden of disease.
Strengths and limitations
To our knowledge, this GBD-based study is the largest effort to date to reveal global BC incidence and deaths, determine the global cancer burden attributable to the most relevant risk factors, and predict the future burden of BC. The study will help to enrich the research evidence of global BC risk and attributable disease burden 11 , 22 , 23 , 24 , 25 , which is of great important to prevent and control the occurrence and development of BC and improve health. However, our study also has limitations. First, some countries (or territories) do not have population-based cancer registries, leaving an important source of data for estimating cancer burden missing. Second, the GBD2019 only provides some behavioral risks (such as tobacco, alcohol use, dietary risks and low physical activity) and metabolic risks (including high fasting glucose and high body mass index) that can be used for further research 26 , are important for a comprehensive assessment of the burden of breast cancer attributable to risk factors. Finally, the disability-adjusted life years, as an index that can simultaneously consider premature death from disease and health loss from disability, has received increasing attention in the field of international cancer disease burden evaluation 27 , and this study focuses on diseases caused by BC incidence and deaths burden.
Moreover, data sharing, a practice that enhances research integrity and transparency, facilitating peer validation and enabling further exploration of the study’s findings, offers valuable resources for scientific research and evidence-based policymaking, particularly relevant to developing countries 28 , 29 . In this sense, our research has significant meaning, because all data available free of charge. Our data provide a rigorous and comparable measure of the global disease burden of breast cancer, all freely downloadable, and can be used by policymakers in the future to generate the evidence they need on how to allocate resources to best improve the population Health makes informed decisions. Nonetheless, it is worth noting that our findings may be delayed as they reflect past disease burden. While our analysis provides valuable insights into the historical trends of breast cancer, predicting future trends necessitates confirmation by more recent data.
Overall, our study provides some evidence that regions with low levels of SDI will have the largest disease burden of breast cancer in the future. Metabolic risk factors increased the most from 1990 to 2019, compared with the behavioral factors. The findings of this study may be of great value for preventing and controlling the incidence and deaths of BC, as well as for improving the health of population. Furthermore, our study results may aid decision makers in formulating more reasonable and effective preventive health policies, and solutions for BC, and related health inequalities.
Study design
In this study covering data of GBD on incidence, deaths, and their temporal trends in 204 countries or territories and 21 regions from 1990 to 2019, different changing trends of BC burden were observed, with significant differences by sex, region, country, and sociodemographic index. The logical flowchart of this study is shown in Supplementary Fig. 4 .
Data sources
Annual incident cases, age standardized incidences and deaths of BC from 1990 to 2019, by sex, region, country, and risk factors (metabolic risks, dietary risks, tobacco, alcohol use and low physical activity) were obtained from the GBD 2019 through the Global Health Data Exchange (GHDx) query tool ( https://ghdx.healthdata.org/gbd-2019 ).
To create the source dataset, we follow a procedure. First, we access the data acquisition interface of the database and click on the “query tool” hyperlink located under the “GBD Results Tool” menu. This leads us to the data retrieval interface where we have the option to select different GBD evaluation options from the “GBD Estimate” drop-down menu. By default, cause of death or injury is selected. Next, we can choose from a variety of disease evaluation indicators such as morbidity, prevalence, mortality, and disease burden, including disability-adjusted life years, from the “Measure” drop-down menu. We can also select different measurement indicators like number, percent, and rate from the “Metric” drop-down menu. The “Cause” drop-down menu provides an extensive list of common causes such as tumor, high blood pressure, and diabetes, among others. Similarly, the “Location” drop-down menu displays all the countries and regions in the world which are categorized in great detail, including China (national level) and East Asia (regional level). For some countries like the United States and the United Kingdom, intra-country state or provincial level data is also available although this feature is not currently available for China. Moreover, we can filter data by age and sex using the “Age and Sex” drop-down menu, while the “Year” drop-down menu allows us to choose a time range between 1990–2019. GBD 2019 is the most up to date and ongoing global collaboration, and all epidemiological data are available as open source. Simply enter your desired query in the search box above and click “Search” to retrieve the relevant information. Alternatively, you may choose to directly download the CSV file by clicking on the “Download CSV” button.

Data records
A total of 204 countries or territories and 21 regions were selected in this study. The human development index (HDI) data at the national level were collected from the United Nations Development Programme ( https://hdr.undp.org/data-center/human-development-index#/indicies/HDI ). Rates in this study are reported per 100,000 people, and age-standardized rates are calculated based on GBD world population standards 30 . Some of the results were provided by the sociodemographic index (SDI) to describe differences in GBD of BC. The quintiles of the SDI index are used to define low (~20), low-middle (~40), middle (~60), middle-high (~80) and high (~100) SDI countries in 2019 27 . The global population forecast data for 2017–2100 were obtained from the Institute for Health Metrics and Evaluation ( https://ghdx.healthdata.org/record/ihme-data/global-population-forecasts-2017-2100 ). The data supports this finding have recorded in the Figshare 31 ( https://doi.org/10.6084/m9.figshare.22787405 ). The document “GBD for BC.xlsx” comprises six main worksheets. The first worksheet, named “BC_nation,” is primarily utilized to analyze the country’s morbidity and mortality related to BC, enabling quantification of this data. The following worksheets - “BC_region,” “BC_region_SDI,” and “BC_region_SEX” - are used to examine the morbidity and mortality of BC quantified by region, SDI, and sex. To assess trends in BC incidence and mortality, an estimation of the change in cancer cases from 1990 to 2019, along with the EAPC and its 95% confidence interval, are used. Finally, the “BC_percent” worksheet focuses on estimating the cancer burden attributable to risk factors.
Data analysis
Referring to previous literature report 32 , the age-standardized ratio (ASR) and its 95% uncertainty interval was used to quantify the incidence and deaths of BC by time, sex, region, country and SDI. Then, the changes in cancer cases, the estimated annual percentage change (EAPC) and its 95% confidence interval from 1990 to 2019 was used to assess the incidences and deaths trend of BC. Finally, we combined EAPC data for incidences and deaths to perform hierarchical cluster analysis to identify countries with similar annual increases in incidences and deaths. All countries were divided into 4 groups, including minor increase, remained stable or minor decrease, significant decrease, and significant increase.
GBD 2019 includes three categories of attributable risks, such as environment or occupation risks, behavior risks and metabolism risks. We first identified the BC risk factors with convincing or likely causal evidence based on World Cancer Research Fund criteria. Then, the proportion of cancer-specific burden attributable to each risk factor was calculated in different year, region, country and SDI. Finally, temporal trends of attributable risk factors were assessed at the SDI level.
We selected two-time nodes, 1990 and 2019, and calculated the age-standardized incidence rates (ASIR) and age-standardized deaths rates (ASDR) at the country level. Then, HDI, ASIR, ASDR were selected as the candidate indicators to determine the influencing factors of EAPC by correlation analysis.
Considering that the incidence and mortality rates of different sexes are different, in this study we separately predicted the incidence and deaths rates of men and women from 2020 to 2050 to assess the future GBD of BC. This GBD forecasts is primarily based on the Global Population Forecasts 2017–2100 data and age-standardized BC incidence and deaths data from 1990 to 2019.
All statistical analysis of data were performed using the R Project for Statistical Computing (version 4.2.2; R Core Team). We used the ASR and EAPC to quantify the BC incidence and deaths trends. Constituent ratios were used to evaluate the cancer burden attributable to risk factors. Pearson correlation analysis was used to determine the association of HDI, ASIR, ASDR with EAPC. For the future forecasts of GBD in BC, we used the BACP package. A threshold of P value less than 0.05 was set to determine the significant differences.
Usage Notes
Our data and code are freely available as open source. The analysis codes presented in the article were written using the R language. To conduct your own analysis, you will need to first install the necessary environment for R, including packages such as dplyr, ggplot2, ggsci, factoextra, ggmap, rgdal, maps, devtools, and others. Moving forward, these data can be utilized to examine the disease burden of breast cancer and its changing trends, categorized by time, sex, region, country, and SDI. Additionally, if you intend to analyze other disease burdens apart from breast cancer, our open-source R language code is also well-suited for your needs.
Data availability
The data supports this finding can be accessed from the Figshare 31 ( https://doi.org/10.6084/m9.figshare.22787405 ). The “Date.xlsx” file contains separate sheets that provide pertinent metadata for assessing the incidence and mortality rates of breast cancer based on various factors such as time, gender, region, country, and socio-demographic index (SDI). In addition to this information, the document also includes data on the World population age standard, the HDI of different countries in 1990, and Global Population Forecasts spanning from 2017 to 2100.
Code availability
All R code supporting the conclusions of this study can be accessed and downloaded via Github 33 ( https://doi.org/10.5281/zenodo.7915783 ). The main computational tools used in this study are R language based. The scripts used in this study include “GBD_Incidence_region.R,” which calculates incident cases, deaths, ASR, and EAPC for BC worldwide during 1990 and 2019. Another script, “GBD_Incidence_map.R” is employed to generate visualizations of BC incidence and mortality using GBD data from 204 countries and regions around the world. Additionally, “GBD_cluster.R” was used to perform hierarchical cluster analysis to identify countries with similar annual increases in BC incidence and mortality. To calculate the percentage of major risk factors globally attributable to BC mortality, “GBD_Percent.R” was utilized. The correlation between EAPC and ASIR, ASDR, and HDI was analyzed using “GBD_COR.R”. Finally, “Global_BAPC_prediction.R” was implemented to predict the future burden of BC using GBD data.
Collaborators, G. B. D. C. R. F. The global burden of cancer attributable to risk factors, 2010-19: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 400 , 563–591, https://doi.org/10.1016/S0140-6736(22)01438-6 (2022).
Article Google Scholar
Sung, H. et al . Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 71 , 209–249, https://doi.org/10.3322/caac.21660 (2021).
Article PubMed Google Scholar
Winn, A. N., Ekwueme, D. U., Guy, G. P. Jr. & Neumann, P. J. Cost-Utility Analysis of Cancer Prevention, Treatment, and Control: A Systematic Review. Am J Prev Med 50 , 241–248, https://doi.org/10.1016/j.amepre.2015.08.009 (2016).
Global Burden of Disease Cancer, C. et al . Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-Years for 29 Cancer Groups, 1990 to 2017: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol 5 , 1749–1768, https://doi.org/10.1001/jamaoncol.2019.2996 (2019).
Safiri, S. et al . Burden of female breast cancer in the Middle East and North Africa region, 1990-2019. Arch Public Health 80 , 168, https://doi.org/10.1186/s13690-022-00918-y (2022).
Article PubMed PubMed Central Google Scholar
Mubarik, S. et al . Evaluation of lifestyle risk factor differences in global patterns of breast cancer mortality and DALYs during 1990-2017 using hierarchical age-period-cohort analysis. Environ Sci Pollut Res Int 28 , 49864–49876, https://doi.org/10.1007/s11356-021-14165-1 (2021).
Mubarik, S. et al . A Hierarchical Age-Period-Cohort Analysis of Breast Cancer Mortality and Disability Adjusted Life Years (1990-2015) Attributable to Modified Risk Factors among Chinese Women. Int J Environ Res Public Health 17 , https://doi.org/10.3390/ijerph17041367 (2020).
Mubarik, S., Hu, Y. & Yu, C. A multi-country comparison of stochastic models of breast cancer mortality with P-splines smoothing approach. BMC Med Res Methodol 20 , 299, https://doi.org/10.1186/s12874-020-01187-5 (2020).
Mubarik, S. et al . Epidemiological and sociodemographic transitions of female breast cancer incidence, death, case fatality and DALYs in 21 world regions and globally, from 1990 to 2017: An Age-Period-Cohort Analysis. J Adv Res 37 , 185–196, https://doi.org/10.1016/j.jare.2021.07.012 (2022).
Li, Y. et al . Global Burden of Female Breast Cancer: Age-Period-Cohort Analysis of Incidence Trends From 1990 to 2019 and Forecasts for 2035. Front Oncol 12 , 891824, https://doi.org/10.3389/fonc.2022.891824 (2022).
Li, N. et al . Global burden of breast cancer and attributable risk factors in 195 countries and territories, from 1990 to 2017: results from the Global Burden of Disease Study 2017. J Hematol Oncol 12 , 140, https://doi.org/10.1186/s13045-019-0828-0 (2019).
Global Burden of Disease Cancer, C. et al . Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol 3 , 524–548, https://doi.org/10.1001/jamaoncol.2016.5688 (2017).
Deng, Y. et al . Global Burden of Thyroid Cancer From 1990 to 2017. JAMA Netw Open 3 , e208759, https://doi.org/10.1001/jamanetworkopen.2020.8759 (2020).
Arshi, A. et al . Expression Analysis of MALAT1, GAS5, SRA, and NEAT1 lncRNAs in Breast Cancer Tissues from Young Women and Women over 45 Years of Age. Mol Ther Nucleic Acids 12 , 751–757, https://doi.org/10.1016/j.omtn.2018.07.014 (2018).
Article CAS PubMed PubMed Central Google Scholar
Vuong, Q. H. et al . Near-Suicide Phenomenon: An Investigation into the Psychology of Patients with Serious Illnesses Withdrawing from Treatment. Int J Environ Res Public Health 20 , https://doi.org/10.3390/ijerph20065173 (2023).
Masood, M. & Reidpath, D. D. Effect of national wealth on BMI: An analysis of 206,266 individuals in 70 low-, middle- and high-income countries. PLoS One 12 , e0178928, https://doi.org/10.1371/journal.pone.0178928 (2017).
Lee, M. J., Popkin, B. M. & Kim, S. The unique aspects of the nutrition transition in South Korea: the retention of healthful elements in their traditional diet. Public Health Nutr 5 , 197–203, https://doi.org/10.1079/PHN2001294 (2002).
Article CAS PubMed Google Scholar
Mori, N., Armada, F. & Willcox, D. C. Walking to school in Japan and childhood obesity prevention: new lessons from an old policy. Am J Public Health 102 , 2068–2073, https://doi.org/10.2105/AJPH.2012.300913 (2012).
Seitz, H. K., Pelucchi, C., Bagnardi, V. & La Vecchia, C. Epidemiology and pathophysiology of alcohol and breast cancer: Update 2012. Alcohol Alcohol 47 , 204–212, https://doi.org/10.1093/alcalc/ags011 (2012).
Zakhari, S. & Hoek, J. B. Alcohol and breast cancer: reconciling epidemiological and molecular data. Adv Exp Med Biol 815 , 7–39, https://doi.org/10.1007/978-3-319-09614-8_2 (2015).
Collaborators, G. B. D. T. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990-2015: a systematic analysis from the Global Burden of Disease Study 2015. Lancet 389 , 1885–1906, https://doi.org/10.1016/S0140-6736(17)30819-X (2017).
Guerra, M. R. et al . Inequalities in the burden of female breast cancer in Brazil, 1990-2017. Popul Health Metr 18 , 8, https://doi.org/10.1186/s12963-020-00212-5 (2020).
Liu, W. et al . [Disease burden of breast cancer in women in China, 1990-2017]. Zhonghua Liu Xing Bing Xue Za Zhi 42 , 1225–1230, https://doi.org/10.3760/cma.j.cn112338-20200908-01139 (2021).
Yan, X. X. et al . [DALYs for breast cancer in China, 2000-2050: trend analysis and prediction based on GBD 2019]. Zhonghua Liu Xing Bing Xue Za Zhi 42 , 2156–2163, https://doi.org/10.3760/cma.j.cn112338-20210506-00373 (2021).
Azamjah, N., Soltan-Zadeh, Y. & Zayeri, F. Global Trend of Breast Cancer Mortality Rate: A 25-Year Study. Asian Pac J Cancer Prev 20 , 2015–2020, https://doi.org/10.31557/APJCP.2019.20.7.2015 (2019).
Britt, K. L., Cuzick, J. & Phillips, K. A. Key steps for effective breast cancer prevention. Nat Rev Cancer 20 , 417–436, https://doi.org/10.1038/s41568-020-0266-x (2020).
Diseases, G. B. D. & Injuries, C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396 , 1204–1222, https://doi.org/10.1016/S0140-6736(20)30925-9 (2020).
Vuong, Q.-H. The (ir)rational consideration of the cost of science in transition economies. Nature Human Behaviour 2 , 5, https://doi.org/10.1038/s41562-017-0281-4 (2018).
Vuong, Q.-H. Reform retractions to make them more transparent. Nature 582 , 149, https://doi.org/10.1038/d41586-020-01694-x (2020).
Article ADS CAS Google Scholar
Collaborators, G. B. D. D. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950-2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet 396 , 1160–1203, https://doi.org/10.1016/S0140-6736(20)30977-6 (2020).
Zeng, Q. GBD for Breast Cancer, Figshare , https://doi.org/10.6084/m9.figshare.22787405 (2023).
Liu, Z. et al . The trends in incidence of primary liver cancer caused by specific etiologies: Results from the Global Burden of Disease Study 2016 and implications for liver cancer prevention. J Hepatol 70 , 674–683, https://doi.org/10.1016/j.jhep.2018.12.001 (2019).
Zeng, Q. zengqibing/GBD-for-Breast-Cancer: Code of GBD for Breast Cancer (Code-GBD-for-Breast-Cancer), Zenodo , https://doi.org/10.5281/zenodo.7915783 (2023).
Download references
Acknowledgements
We highly appreciate the works by the Global Burden of Disease Study 2019 collaborators. This work was supported by the National Key Research and Development Program “Precision Medicine Initiative” of China (Grant 2017YFC0907301).
Author information
These authors contributed equally: Yuyan Xu, Maoyuan Gong.
Authors and Affiliations
Guizhou Medical University, the Key Laboratory of Environmental Pollution Monitoring and Disease Control, Ministry of Education & Guizhou Provincial Engineering Research Center of Ecological Food Innovation & School of Public Health, Guiyang, 550025, China
Yuyan Xu, Maoyuan Gong, Yang Yang & Qibing Zeng
The Affiliated Hospital of Guizhou Medical University, Department of Breast Surgery, Guiyang, 550004, China
Yue Wang & Shu Liu
You can also search for this author in PubMed Google Scholar
Contributions
Y.X. and M.G. performed data collection and analysis, results visualization, and wrote the manuscript. Y.W. and Y.Y. made contributions to data acquisition and analysis. S.L. and Q.Z. made significant contributions to the conceptualization, methodology, data analysis, supervision, validation, and writing– review & editing of the study. Final manuscript read and approved by all authors. Correspondence to Shu Liu and Qibing Zeng.
Corresponding authors
Correspondence to Shu Liu or Qibing Zeng .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Xu, Y., Gong, M., Wang, Y. et al. Global trends and forecasts of breast cancer incidence and deaths. Sci Data 10 , 334 (2023). https://doi.org/10.1038/s41597-023-02253-5
Download citation
Received : 02 March 2023
Accepted : 18 May 2023
Published : 27 May 2023
DOI : https://doi.org/10.1038/s41597-023-02253-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Prospective study to evaluate efficacy of single versus double drains in breast cancer patients undergoing surgery.
- Shubhajeet Roy
- Shikhar S. Gupta
- Anand Kumar Misra
Indian Journal of Surgical Oncology (2024)
MDM2 Gene rs2279744 Polymorphism and Breast Cancer Risk: Evidence from Meta-Analysis and Meta-Regression Analysis
- Mohammad Masoud Eslami
- Payam Mohammadi
- Amirhossein Sahebkar
Indian Journal of Gynecologic Oncology (2024)
Restoring microRNA-34a overcomes acquired drug resistance and disease progression in human breast cancer cell lines via suppressing the ABCC1 gene
- Shaymaa M. M. Yahya
- Heba K. Nabih
- Sohair M. Salem
Breast Cancer Research and Treatment (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Cancer newsletter — what matters in cancer research, free to your inbox weekly.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.66; 2022 Dec
Current and future burden of breast cancer: Global statistics for 2020 and 2040
Melina arnold.
a Cancer Surveillance Branch, International Agency for Research on Cancer, Lyon, France
Eileen Morgan
Harriet rumgay, allini mafra, deependra singh, mathieu laversanne, jerome vignat, julie r. gralow.
b American Society of Clinical Oncology, Alexandria VA, USA
Fatima Cardoso
c Breast Unit, Champalimaud Clinical Center/Champalimaud Foundation, Lisbon, Portugal
Sabine Siesling
d Department of Research and Development, Netherlands Comprehensive Cancer Organisation (IKNL), Utrecht, Netherlands
e Department of Health Technology and Services Research, Technical Medical Centre, University of Twente, Enschede, Netherlands
Isabelle Soerjomataram
Associated data.
The dataset supporting the conclusions of this article is available at gco.iarc.fr.
Breast cancer is the most commonly diagnosed cancer worldwide, and its burden has been rising over the past decades. In this article, we examine and describe the global burden of breast cancer in 2020 and predictions for the year 2040.
Estimates of new female breast cancer cases and deaths in 2020 were abstracted from the GLOBOCAN database. Age-standardized incidence and mortality rates were calculated per 100,000 females by country, world region, and level of human development. Predicted cases and deaths were computed based on global demographic projections for the year 2040.
Over 2.3 million new cases and 685,000 deaths from breast cancer occurred in 2020. Large geographic variation across countries and world regions exists, with incidence rates ranging from <40 per 100,000 females in some Asian and African countries, to over 80 per 100,000 in Australia/New Zealand, Northern America, and parts of Europe. Smaller geographical variation was observed for mortality; however, transitioning countries continue to carry a disproportionate share of breast cancer deaths relative to transitioned countries. By 2040, the burden from breast cancer is predicted to increase to over 3 million new cases and 1 million deaths every year because of population growth and ageing alone.
Breast cancer is the most common cancer worldwide and continues to have a large impact on the global number of cancer deaths. Global efforts are needed to counteract its growing burden, especially in transitioning countries where incidence is rising rapidly, and mortality rates remain high.
- • With over 2.3 million new cases and 685,000 deaths in 2020, breast cancer is the most commonly diagnosed cancer worldwide.
- • Most cases occur in transitioned countries yet transitioning countries have disproportionate share of breast cancer deaths.
- • The future burden of breast cancer is predicted to increase to over 3 million new cases and 1 million deaths in 2040.
1. Introduction
Having replaced lung cancer as the most commonly diagnosed cancer globally, breast cancer today accounts for 1 in 8 cancer diagnoses and a total of 2.3 million new cases in both sexes combined [ 1 ]. Representing a quarter of all cancer cases in females, it was by far the most commonly diagnosed cancer in women in 2020, and its burden has been growing in many parts of the world, particularly in transitioning countries [ 2 ]. An estimated 685,000 women died from breast cancer in 2020, corresponding to 16% or 1 in every 6 cancer deaths in women. Previously insufficient public health response to this development has led to the recent launch of the Global Breast Cancer Initiative by the World Health Organization (WHO) [ 3 ]. By engaging global partners and coordinating sustainable efforts to improve outcomes, WHO and collaborators aim to reduce breast cancer mortality by fostering timely diagnosis and adequate treatment and patient management. As a foundation to these efforts, a good understanding of global patterns and variation in the disease burden is vital.
Herein, we examine and describe the burden of invasive breast cancer worldwide in 2020 based on the GLOBOCAN estimates of cancer incidence and mortality developed by the International Agency for Research on Cancer (IARC). We assess geographic variation and describe the magnitude and distribution of the disease for the year 2020 and predict the future burden in 2040.
2. Data sources and methods
The number of new cases of, and deaths from, primary invasive cancers of the female breast (International Classification of Diseases tenth revision (ICD-10) C50) were extracted from the GLOBOCAN 2020 database for 185 countries or territories, by sex and 18 age groups (0–4, 5–9, …, 80–84, 85 and over) [ 1 , 4 , 5 ]. Corresponding population data for 2020 were extracted from the United Nations (UN) website [ 6 ]. The data sources and hierarchy of methods used in compiling the cancer estimates have been described in detail elsewhere [ 4 ]. In brief, the GLOBOCAN estimates are assembled at the national level using the best available sources of cancer incidence and mortality data within a given country. The methods used to derive the 2020 estimates correspond to those used in previous years [ [7] , [8] , [9] ]; where applicable, priority is given to short-term predictions and modelled mortality to incidence (M:I) ratios, while validity is dependent on the degree of representativeness and quality of the source information [ 4 ].
We present tables and figures on the estimated new cases and deaths, as well as two summary measures using direct standardization, namely the age-standardized (incidence or mortality) rate (ASR) per 100,000 females based on the adapted 1966 Segi World standard population [ 10 , 11 ] for all ages combined, and truncated ASRs for ages below and above 50 years (also referred to as pre- and postmenopausal ages), alongside the cumulative risk of developing or dying from cancer before the age of 75 (as one representation of the lifetime risk of developing breast cancer) expressed as a percentage, assuming the absence of competing causes of death [ 12 ]. These measures allow comparisons between populations adjusted for differences in age structures. We also provide a prediction of the future number of female breast cancer cases and deaths worldwide for the year 2040, based on demographic projections and in a scenario where rates remain stable from the baseline year of 2020. Predictions were calculated by applying the 2020 rates to the predicted population data as estimated by the United Nations Development Programme (UNDP).
The results are presented by country, and aggregated according to 20 UN-defined world regions [ 6 ] and to the UN's four-tier Human Development Index (HDI) in 2020 [ 13 ], the latter a means to assess the cancer burden at varying levels of development (low, medium, high and very high HDI). Throughout we use the terms transitioning , emerging and lower HDI countries/economies as synonyms for nations classified as low or medium HDI, and transitioned or higher HDI countries/economies for those classified as high or very high HDI.
The Global Cancer Observatory (GCO, https://gco.iarc.fr ) includes facilities for the tabulation and graphical visualization of the GLOBOCAN database, including explorations of the current [ 5 ] and future [ 14 ] burden for 36 cancer types, including female breast cancer as presented in this overview.
3.1. Breast cancer cases and deaths by world region
In 2020, an estimated 2.3 million cases of female breast cancer were diagnosed globally, and about 685,000 women died from the disease. Table 1 shows the number of newly diagnosed breast cancer cases and deaths, the incidence and mortality ASR, and the cumulative risk of developing and dying from breast cancer by world region. The highest incidence rates (>80 per 100,000 females) were observed in Australia/New Zealand, Western Europe, Northern America and Northern Europe and the lowest rates (<40 per 100,000) in Central America, Eastern and Middle Africa, and South-Central Asia. The highest mortality rates (>20 per 100,000) were found in Melanesia, Western Africa and Micronesia/Polynesia, while rates in most other world regions ranged between 10 and 15 per 100,000.
Breast cancer incidence (new cases) and mortality (deaths) in 2020 by world region and Human Development Index level.
Fig. 1 presents the distribution of breast cancer cases and deaths across world regions. Close to a quarter of all cases occurred in Eastern Asia, followed by Northern America (12.5%), South-Central Asia (11.3%) and Western Europe (7.5%). Close to half of all global breast cancer deaths were observed in Eastern, South Central and South-Eastern Asia combined, and North America (7.1%) and Western Europe (6.4%) ranked 5th and 6th in terms of numbers of deaths. While 8.3% of all breast cancer cases occurred in Africa, the continent's share of breast cancer deaths was considerably higher (12.5% of the global deaths).

Distribution of breast cancer cases and deaths by world area in 2020.
With over 70% of all new cases and 81% of all deaths observed in women aged 50 and above, the global burden from breast cancer remains concentrated in this age group ( Table 2 ). The age distribution of cases and deaths however differed considerably across world regions, ranging from 43% of cases and 49% of deaths occurring at postmenopausal ages in Middle Africa, to over 80% of cases and 90% of deaths in Northern America, as well as Western and Northern Europe. The latter regions however continue to carry the highest (age-standardized) incidence rates of both pre- (>30 per 100,000) and postmenopausal breast cancer (>300 per 100,000). Mortality rates at premenopausal ages were highest in Melanesia, Middle and Western Africa (>8 per 100,000) and lowest in Australia/New Zealand (2.9 per 100,000).
Breast cancer incidence (new cases) and mortality (deaths) in 2020 by age at diagnosis, world region and Human Development Index level.
3.2. Breast cancer cases and deaths by level of human development
In 2020, breast cancer incidence rates were almost double in transitioned compared to transitioning countries (ASR 55.9 versus 29.7 per 100,000, respectively). However, women living in transitioning countries had 17% higher mortality rates compared with women in transitioned countries (15.0 and 12.8 per 100,000, respectively). In terms of absolute cases and deaths, about 20% of all cases and 30% of all deaths from breast cancer worldwide in 2020 occurred in transitioning countries. A gradient across human development level was also observed for the cumulative risk of developing breast cancer before the age of 75, ranging from 3.9 to 3.0% in low and medium HDI countries, respectively, to 4.6 and 8.2% in high and very high HDI countries, respectively ( Table 1 ). However, patterns were different for mortality, where the cumulative risk of dying from breast cancer below the age of 75 was 2.2% in low HDI countries and 1.4–1.5% in the remaining HDI levels.
Similar gradients were observed at pre- and postmenopausal ages, with mortality rates in premenopausal women being about twice as high in low HDI countries when compared with other HDI levels and yet less pronounced mortality differences in women aged 50 and above ( Table 2 ).
In women, breast cancer was the most diagnosed cancer in 157 (out of 185) countries, followed by cervical cancer in 23, mainly sub-Saharan African, countries and the leading cause of cancer death in 110 countries, followed by cervical cancer in 36 and lung cancer in 25 countries. Yet, great geographic variation exists in incidence and mortality rates ( Fig. 2 ). Across the globe, incidence varied 23-fold (from 5.0 per 100,000 in Bhutan to 113.2 per 100,000 in Belgium) and mortality 16-fold (from 2.6 per 100,000 in Bhutan to 42.2 per 100,000 in Barbados). Considerable variation in breast cancer incidence was also observed within world regions, for example in South-Eastern Asia rates were as low as 9.6 per 100,000 in Myanmar and as high as 77.9 in Singapore. Breast cancer mortality showed less variation than incidence within world regions, except for the Caribbean where mortality rates ranged between 12.9 in Cuba and 42.2 in Barbados ( Fig. 3 ).

Age-standardized breast cancer incidence (top, blue) and mortality (bottom, red) rates per 100,000 females. Breast cancer cases and deaths by country. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)

Age-standardized breast cancer incidence (top, blue) and mortality (bottom, red) rates per 100,000 females by country and world region; countries with highest and lowest rates within region mentioned with their name; full country-level results are available at gco.iarc.fr. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
3.3. The future burden of breast cancer in 2040
By 2040, the number of newly diagnosed breast cancers is projected to grow by over 40%, to about 3 million cases every year. Similarly, deaths from breast cancer are set out to increase more than 50%, from 685,000 in 2020 to 1 million in 2040 ( Fig. 4 ). A particularly large relative increase will be seen in transitioning countries, especially in low HDI countries where the number of new cases and deaths is expected to double by 2040 (from 110,000 to 216,000 and from 59,000 to 116,000, respectively). While in 2020, 18.4% of breast cancer cases and 30.1% of deaths occurred in transitioning countries, by 2040 this share will rise to 22.2% and 35.2%, respectively. This projection is solely due to the growth and aging of the population and may be further modified by changes in incidence rates.

Estimated number of breast cancer cases and deaths from 2020 to 2040, by level of Human Development Index (HDI).
4. Discussion
With over 2.3 million new cases estimated in 2020, breast cancer has become the most commonly diagnosed cancer worldwide and represents a major burden to public health. Large geographic variation exists in its burden across countries and world regions. While most cases occur in transitioned countries, transitioning countries continue to carry a disproportionate share of breast cancer deaths. If current trends remain unchanged, the burden of breast cancer is set to grow to over 3 million new cases and 1 million deaths per year by 2040 as a result of population growth and ageing alone.
Higher incidence rates in transitioned countries reflect a longstanding higher prevalence of reproductive, hormonal, and behavioral risk factors. Established risk factors for breast cancer include early age at menarche, later age at menopause, advanced age at first birth, fewer number of children, less breastfeeding, menopausal hormone-replacement therapy, oral contraceptives, but also alcohol consumption, excess body weight, and physical inactivity [ 15 , 16 ]. Changes in the prevalence of these risk factors coupled with increased detection through organized or opportunistic mammographic screening have been reflected in past incidence trends, most notably rapidly rising rates during the 1980s and 1990s in Northern America, Oceania and Europe. This was followed by a stabilization or decline of trends in the early 2000s [ 17 ], likely a consequence of reduced use of menopausal hormone-replacement therapy and possibly a plateau in the detection of precancerous lesions/DCIS [ 18 , 19 ]. Rising incidence rates have been reported in several high-income countries in North America, Europe and Oceania since 2007 for pre- and postmenopausal breast cancer [ 2 , 20 ]. Most of this rise has been attributed to the increased detection of small, early stage tumors with very good prognosis in countries with well-established screening programmes. The increased detection of slow-growing estrogen receptor-positive cancers during mammographic screening might have added to the rising incidence of estrogen receptor-positive tumors, while the incidence of estrogen receptor-negative tumors is declining [ [21] , [22] , [23] , [24] , [25] ]. The diverging trends in estrogen receptor-specific breast cancer incidence have been linked to dual effects of certain environmental risk factors such as obesity. Estrogen receptor-positive cancers show a stronger and more consistent relation with excess body weight and their increasing incidence could be a consequence of the growing obesity epidemic in many countries [ 26 ]. These changes in breast cancer incidence have coincided with generally decreasing mortality rates linked to the combination of progress in treatment and early detection through screening in most transitioned, and historically high-risk countries since the late 1980s and the early 1990s [ 27 ]. As a consequence, the number of women living with a history of breast cancer has also increased markedly, amounting to an estimated 7.8 million in 2020 (5-year prevalence), making long-term outcomes such as disease progression and recurrence important metrics that are however to-date still poorly understood from a global perspective. Given the increasing number of survivors and the changing landscape of breast cancer, improvements in other indicators that aim to measure quality of life and years of life with disability should be considered.
Different patterns and trends have been observed in transitioning countries in South America, Africa and Asia, where breast cancer incidence is historically low but has been rising rapidly in past decades. This has been linked to dramatic changes in behavioral factors (e.g., rising obesity and physical inactivity), reproductive health (e.g., fewer children, postponement of childbearing), increasing life expectancy and socio-cultural environments that together have led to changes in risk factor profiles that are similar to those of transitioned countries. As a result, breast cancer incidence rates have risen and are slowly approaching levels observed in transitioned countries. Evidence from sub-Saharan Africa shows that incidence rates have increased by more than 5% every year in Malawi, Nigeria and the Seychelles and by 3–4% per year in South Africa and Zimbabwe [ 28 ]. Higher proportions of women developing breast cancer at premenopausal ages in these world regions is directly related to the much younger age structure, although women of African descent have been shown to have an increased risk of Triple Negative Breast Cancer (TNBC) that is often characterized by an earlier age at onset relative to other breast cancer subtypes [ 29 ]. Whether the age at diagnosis, adjusted for demographics, is truly different across countries remains to be elucidated.
Mortality rates from breast cancer have increased in sub-Saharan Africa and are among the highest in the world. While 5-year survival rates for breast cancer exceed 90% in most high-income countries, this figure was 66% for 12 sub-Saharan African countries combined for cases diagnosed 2008–2015 [ 30 ], with country-specific estimates as low as 12% in Uganda [ 31 ]. Higher mortality in sub-Saharan Africa is mainly attributable to late-stage presentation and inadequate access to high-quality care [ 32 ]. Among patients with known stage, 64.9% were diagnosed with advanced disease (stages III and IV) and 18.4% had distant metastases at diagnosis (stage IV), where survival is low [ 31 ]. According to a meta-analysis summarizing evidence from 83 studies across 17 sub-Saharan African countries, 77% of all staged cases were advanced (stage III) or metastatic (stage IV) at diagnosis [ 33 ]. In contrast, only about 15% of all breast cancer cases are diagnosed at advanced stages (III and IV) in high-income countries, such as the Netherlands [ 34 ]. In the absence of organized screening programmes, early diagnosis focusing on breast self-awareness and improved access to quality diagnosis and treatment are crucial elements in breast cancer control in transitioning countries. Multiple coordinated interventions, including the reduction of stigmas through public education and improved awareness, such as the recognition of signs and symptoms of early breast cancer are required to improve and accelerate referral for adequate diagnostic evaluation and timely, evidence-based treatment [ 3 , 35 , 36 ]. These also represent the main goals of the ABC Global Alliance ( https://www.abcglobalalliance.org/ ), a multi-stakeholder platform focusing on advanced breast cancer (ABC). A recent study conducted in 5 sub-Saharan African countries estimated that at least a third of all breast cancer deaths in these countries could be prevented through earlier diagnosis of symptomatic disease alongside improvements in treatment [ 37 ].
In response to the growing global breast cancer burden and particularly the premature mortality in transitioning countries, the Global Breast Cancer Initiative [ 3 ] was launched by the WHO and international partners in early 2021. Together with allies and global collaborators, the initiative aims to reduce global breast cancer mortality by increasing access to breast cancer early diagnosis and prompt, comprehensive cancer management. In addition, a series of evidence-based, resource-stratified guidelines that support phased implementation into real-world practice has been developed by the Breast Health Global Initiative [ [38] , [39] , [40] ]. Only few established risk factors of breast cancer are truly modifiable. Primary prevention efforts are therefore limited to decreasing excess body weight and alcohol consumption and to encourage physical activity and breastfeeding. More importantly, educational and awareness efforts to increase early detection in countries with high proportions of late stage disease, and population-based breast cancer screening programs in countries with low proportions of late stage disease, are crucial to reduce breast cancer mortality, together with equal access to high quality multidisciplinary and specialized care [ 41 ]. The WHO recommends organized, population-based mammography screening every 2 years for women at average risk for breast cancer aged 50–69 years in well-resourced settings. In limited resource settings, where most women with breast cancer are diagnosed in late stages and mammography screening is not cost-effective or feasible, available resources should be focused on early diagnosis by ensuring access of women with symptomatic lesions to prompt and effective diagnosis and treatment [ 42 ].
The numbers and rates presented in this article are estimates based on the best available data from population-based cancer registries that have been thoroughly reviewed. Yet, some caution is warranted when interpreting the findings, especially for countries where estimates are based on proxy data [ 4 ]. While the introduction of screening in many parts of the world has led to an increasing detection and incidence of in-situ carcinomas of the breast, this global assessment only includes invasive breast cancer. Moreover, estimates do not reflect the impact of the COVID-19 pandemic as they are based on extrapolations of cancer data collected in earlier years. In the first half of 2020, breast cancer screening and diagnostic imaging have been dramatically disrupted and temporarily suspended in many countries such as the United States [ 43 ], the Netherlands [ 44 ] or the UK [ 45 ]. In the United States, the COVID-19 pandemic has led to a near-total cessation of mammography services in mid-March 2020. Screening and diagnostic mammography volumes however recovered by July 2020, with a lag observed for certain sub-populations [ 43 ]. A subsequent short-term reduction in the number of referrals, and an overall decline in the number of breast cancer diagnoses were observed in several countries [ [44] , [45] , [46] , [47] ]. A study from Italy [ 48 ] reported an increase in diagnoses of node-positive and stage III breast cancer after a 2-month interruption of mammographic screening. In the Netherlands no shift in stage could be seen until August 2020, while a clear change in initial treatment was observed during the pandemic, with fewer patients undergoing breast conserving therapy or mastectomy plus breast reconstruction and more neoadjuvant hormonal treatment [ 47 , 49 ]. The full extent of the impact of the COVID-19 pandemic on breast cancer diagnoses and deaths in different world regions, however, currently remains unknown. Forthcoming research is warranted to assess whether the decreased diagnostic scrutiny resulted in stage migration and/or altered clinical management in poorer outcomes.
Finally, the future projections presented here are based on demographic forecasts (population growth and ageing) and past global incidence and mortality trends and do not account for geographic and generational variation. Changes in the prevalence of risk factors may further exacerbate these predictions, especially in countries where incidence and mortality rates continue rising. Incidence predictions thus likely represent a conservative estimate (an underestimation) of the future breast cancer burden and need to be interpreted with great caution. Additionally, the mortality projections are based on current survival rates, which could be significantly impacted by strategies that improve more equitable access to early diagnosis and availability of treatments, along with possible development of effective new treatments.
4.1. Conclusion
Breast cancer is by far the most commonly diagnosed malignancy worldwide, with the majority of the disease burden occurring in females. While great geographical variation exists in its burden, breast cancer continues to represent an important cause of premature mortality, particularly in women living in transitioning countries. Global efforts and public health measures targeting the whole continuum of cancer control – ranging from primary prevention to early diagnosis, screening, and treatment – are needed to reduce breast cancer mortality and to tackle the overall burden from the disease.
Declarations
Data availability statement, competing interests.
The authors declare that they have no competing interests.
Ethical approval
Not required.
This work was supported by the Susan G. Komen Foundation (Career Catalyst Grant CCR19608129 to MA). The funder had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Author contributions
MA initiated the study, interpreted the results, and drafted the manuscript. JV and ML conducted the statistical analysis and prepared the figures and tables. EM, HR, AM, DS, JRG, FC, SS and IS provided comments on the draft and the final version of the manuscript. All authors read and approved the final manuscript.
Acknowledgements
Where authors are identified as personnel of the International Agency for Research on Cancer/World Health Organization, the authors alone are responsible for the views expressed in this article, and they do not necessarily represent the decisions, policy, or views of the International Agency for Research on Cancer/World Health Organization.
- IT’S ADVANCING OUR UNDERSTANDING OF BREAST CANCER
- IT’S SAVING LIVES, IMPROVING OUTCOMES
- IT’S LEADING TO PREVENTION & A CURE
- RESEARCH IS THE REASON STORIES
- Our Approach
- The Ground We’ve Gained
- Areas of Focus
- Meet Our Researchers
- Collaborative Initiatives
- Start Your Fundraiser
- Make a planned gift
- Game for BCRF
- Other Ways to Give
- Become a Partner
- Find an event
Our History
- Board of Directors
- Scientific Advisors
- Corporate Partners
- Affiliate Organizations
- Major Donors
- Blog: The Progress Report
- Podcasts: Investigating Breast Cancer
- Video Series: Behind the Breakthroughs
- Stories: Research is the reason
- BCRF Publications
- Research is the reason

Since our founding in 1993 by Evelyn H. Lauder, BCRF has raised more than a billion dollars to fuel its mission to be the end of breast cancer. Through a unique and streamlined grants program, we seek out the brightest minds in science and medicine and give them the necessary resources to pursue their best ideas. This enables researchers to make discoveries and design new approaches to address all aspects of breast cancer—and do so in record time.
In 2023-2024, BCRF will award $60.2 million in annual grants to more than 250 scientists from top universities and medical institutions around the globe. In addition, BCRF has established the Evelyn H. Lauder Founder’s Fund , a multi-year international program to unravel the biology of metastasis. It is the largest privately funded project exclusively focused on metastasis in the world.
The thousands of women and men suffering from breast cancer today depend on us. No institution can conquer this disease alone. Together, we can.
BCRF Mission
Our mission is to prevent and cure breast cancer by advancing the world’s most promising research.
BCRF is recognized as one of the most financially efficient nonprofits in the country. We are the highest-rated breast cancer research nonprofit in the U.S.
Frequently Asked Questions
Find answers to the most commonly asked questions about BCRF, including ways to give.

It all started in 1993 at Evelyn Lauder’s kitchen table. Over a cup of coffee, Mrs. Lauder and her dear friend Dr. Larry Norton began a conversation that would change breast cancer history. Recognizing the power of research and its potential to change the lives of millions of women and men worldwide, they realized that a new approach was critical to tackle breast cancer.
Day in and day out, BCRF staff work to end breast cancer.
BOARD OF DIRECTORS
These experts in their fields lend their leadership to BCRF.
SCIENTIFIC ADVISORS
This board of world-renowned investigators shapes our grants program.
MAJOR DONORS
Thanks to their generosity, BCRF can support more than 250 investigators worldwide.
When you give to BCRF, you're funding critical hours in the lab. More time for research means longer, healthier lives for the ones we love.

Get The Latest
Connect with us.
Please remember BCRF in your will planning. Learn More
Breast Cancer Research Foundation 28 West 44th Street, Suite 609, New York, NY 10036
General Office: 646-497-2600 | Toll Free: 1-866-346-3228 [email protected] | BCRF is a 501 (c)(3) | EIN: 13-3727250
- Privacy Policy
- About Breast Cancer
- Find Support
- Get Involved
- Free Resources
- Mammogram Pledge
- Wall of Support
- In The News
- Recursos en Espa ñ ol
- National Mammography Program
- Patient Navigator Program
- Metastatic Retreats
- Support Group
- Breast Health Education
- Breast Cancer Awareness in the Workplace
Breast Cancer Research
Research philosophy.
NBCF’s mission is to help now and inspire hope to those affected by breast cancer through early detection, education, and support services. This distinguishes NBCF from other breast cancer charities . While we fully support investments in research for a cure or new life-extending therapies, we are focused on helping the patient diagnosed today. Patients diagnosed today need life-saving interventions now, and many of these patients face barriers like cost, fear, and misinformation, and simply need navigation. Research that leads to a future medical breakthrough won’t help now and will be too late for many of these patients.
Since our start in 1991, we have invested millions into research to improve early detection, diagnostics, and improvements to current therapies. While some of our funded projects have yielded impactful results, the overall investment is a drop in the bucket.
National Institutes of Health invests over $40 billion each year to medical research. Other major cancer nonprofits add hundreds of millions to that number. Meanwhile, the overall cost of cancer care in the U.S. is over $150 billion a year. While every cancer patient wants a cure, there is a bigger problem cancer patients face today – navigating cost of care and the complexities of the cancer care system.
History of Our Research Projects
NBCF was founded in 1991 with the mission to help women now. Since that time, NBCF has funded over $7 million in research projects. This investment led to the following discoveries:
- Discovery of a homologue gene of HER2 which led to the development of Herceptin.
- Founding member of Worldwide Innovative Network (WIN), created to accelerate the pace and reduce the cost of translating novel cancer treatments to the bedside by developing and applying, through worldwide clinical trials and research projects, the most promising advances in genomic-based cancer research.
- Launch of WINTHER Trial, which aimed to expand precision oncology to patients with advanced solid tumors that progressed after treatment with standard therapies.
- MD Anderson’s Breast Cancer Moon Shots Program – researching novel genetic markers to identify new plans of attack and improve triple negative breast cancer patient outcomes.
NBCF also funded breakthroughs in breast cancer early detection and patient navigation programs at Cleveland Clinic, UC San Francisco, and C-Change.
Our Research Now
NBCF supports research projects to study and improve existing programs in order to help improve quality of life for metastatic breast cancer patients and their caregivers as well as increase access to knowledge, resources, and training for patient navigators. NBCF funds the following research projects:
Metastatic Breast Cancer Retreat Research
- Research partners: Saint Luke’s Cancer Institute & Koontz Center for Advanced Breast Cancer
- Quantitative analysis
- Qualitative analysis
Patient Navigation Research
- Research partners: Academy of Oncology Nurse & Patient Navigators
- Multisite study of patient navigation programs
- Creation of navigation metrics toolkit
Metastatic Breast Cancer Retreats
Study 1 : outcomes from a metastatic breast cancer retreat for patients and caregivers: improvements in gratitude and personal meaning .
Larson, C., Harry, K. M., Geske, S. J., Metsker, J., Miller, M., Eyler, J., Adams, H., & Pluard, T. J. (2020, March). Outcomes from a Metastatic Breast Cancer Retreat for Patients and Caregivers: Improvements in Gratitude and Personal Meaning . Virtual poster presented at the annual conference of the American Psychosocial Oncology Society.
Saint Luke’s Cancer Institute & Koontz Center for Advanced Breast Cancer
Background/Purpose
Lillie Shockney’s “A Journey of Courage and Hope” three-day retreat protocol is designed to address the specific psychosocial needs of women with metastatic breast cancer (MBC) and their caregivers. Over the course of three days, patients and caregivers participated in guided activities that supported the medical, spiritual, psychological, and relational challenges of MBC. Thus, this study investigated how the three-day psychosocial retreat affected self-reported measures of gratitude, personal meaning, and emotional intimacy.
Study 2 : Experiences of Metastatic Breast Cancer Retreat: A Qualitative Analysis Comparing Patients and Their Caregivers
Carly Larson, M.A.; Savannah Geske, Ph.D., Janie Metsker, RN BSN CN-BN; Monty Miller, LCSW; Jake Eyler, MDiv., BCC
Saint Luke’s Hospital Koontz Center for Advanced Breast Cancer
Over the course of two years, Saint Luke’s Cancer Institute hosted three weekend-long therapeutic retreats for women with metastatic breast cancer and their significant others. The three-day long program was based on Lillie Shockney’s, A Journey of Courage and Hope retreat protocol. At the end of each retreat, all participants completed open-ended survey questions about their experience. This quality improvement research project reviewed the responses in order to improve and enhance the retreat curriculum to best serve both patients and their caregivers.
Patient Navigation
National evidence-based oncology navigation metrics: multisite exploratory study to demonstrate value and sustainability of navigation programs.
Over the past 3 years, a dedicated task force comprised of the Academy of Oncology Nurse & Patient Navigators ( AONN+ ) leadership and members, in collaboration with the American Cancer Society and Chartis Oncology Solutions, has been involved in the extensive exploratory multisite study to demonstrate the value and sustainability of navigation programs.
The purpose of the study is to (1) assess the reliability and validity of 10 key metrics selected from the list of 35 developed by AONN+, and (2) gain insight into the barriers and challenges navigation programs encounter during the implementation of navigation metrics. Harnessing the power of this information to create best practices will elevate navigation and garner industry support for advancing patient-centered care delivery.
The result of those efforts is the Navigation Metrics Toolkit . This new resource will be an invaluable aid to navigators, oncology program administrators, healthcare executives, and other clinicians who are linked to navigation in creating transformative patient care and defining oncology navigation professional practice.
Help support women in need
Donations are always appreciated, but there are lots of great ways to get involved.
We use cookies on our website to personalize your experience and improve our efforts. By continuing, you agree to the terms of our Privacy & Cookies Policies.
- Patient Care & Health Information
- Diseases & Conditions
- Breast cancer
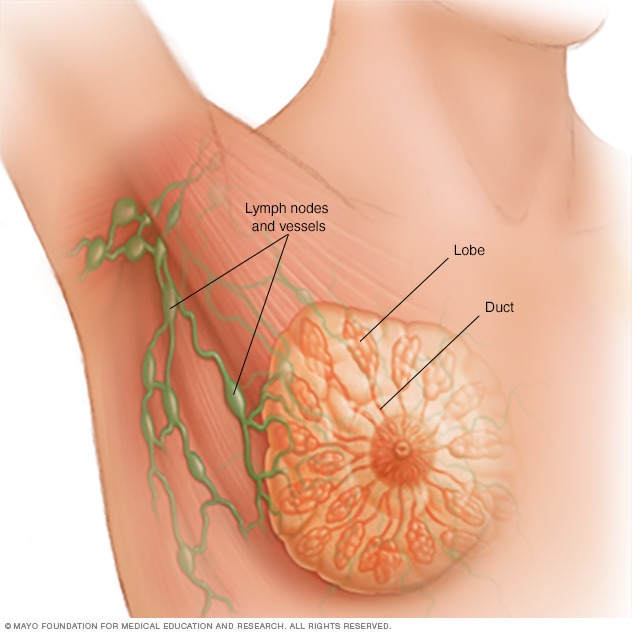
Breast anatomy
Each breast contains 15 to 20 lobes of glandular tissue, arranged like the petals of a daisy. The lobes are further divided into smaller lobules that produce milk for breastfeeding. Small tubes, called ducts, conduct the milk to a reservoir that lies just beneath your nipple.
Breast cancer is a kind of cancer that begins as a growth of cells in the breast tissue.
After skin cancer, breast cancer is the most common cancer diagnosed in women in the United States. But breast cancer doesn't just happen in women. Everyone is born with some breast tissue, so anyone can get breast cancer.
Breast cancer survival rates have been increasing. And the number of people dying of breast cancer is steadily going down. Much of this is due to the widespread support for breast cancer awareness and funding for research.
Advances in breast cancer screening allow healthcare professionals to diagnose breast cancer earlier. Finding the cancer earlier makes it much more likely that the cancer can be cured. Even when breast cancer can't be cured, many treatments exist to extend life. New discoveries in breast cancer research are helping healthcare professionals choose the most effective treatment plans.
Breast cancer care at Mayo Clinic
Products & Services
- A Book: Beyond Breast Cancer
- A Book: Taking Care of You
- Angiosarcoma
- Ductal carcinoma in situ (DCIS)
- Inflammatory breast cancer
- Invasive lobular carcinoma
- Lobular carcinoma in situ (LCIS)
- Male breast cancer
- Paget's disease of the breast
- Recurrent breast cancer
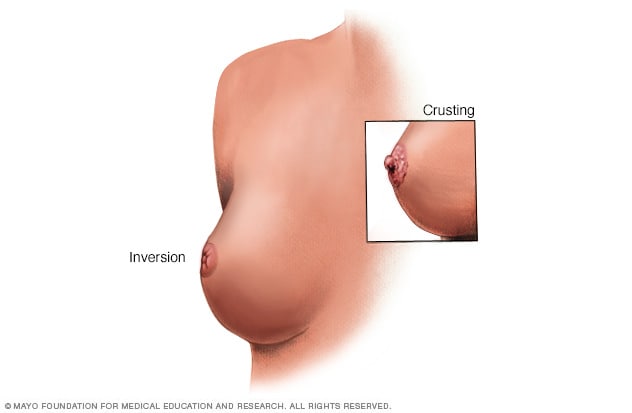
- Nipple changes
Breast and nipple changes can be a sign of breast cancer. Make an appointment with a healthcare professional if you notice any changes.
Signs and symptoms of breast cancer may include:
- A breast lump or thickened area of skin that feels different from the surrounding tissue.
- A nipple that looks flattened or turns inward.
- Changes in the color of the breast skin. In people with white skin, the breast skin may look pink or red. In people with brown and Black skin, the breast skin may look darker than the other skin on the chest or it may look red or purple.
- Change in the size, shape or appearance of a breast.
- Changes to the skin over the breast, such as skin that looks dimpled or looks like an orange peel.
- Peeling, scaling, crusting or flaking of the skin on the breast.
When to see a doctor
If you find a lump or other change in your breast, make an appointment with a doctor or other healthcare professional. Don't wait for your next mammogram to see if the change you found is breast cancer. Report any changes in your breasts even if a recent mammogram showed there was no breast cancer.
The exact cause of most breast cancers isn't known. Researchers have found things that increase the risk of breast cancer. These include hormones, lifestyle choices and things in the environment. But it's not clear why some people who don't have any factors get cancer, yet others with risk factors never do. It's likely that breast cancer happens through a complex interaction of your genetic makeup and the world around you.
Healthcare professionals know that breast cancer starts when something changes the DNA inside cells in the breast tissue. A cell's DNA holds the instructions that tell a cell what to do. In healthy cells, the DNA gives instructions to grow and multiply at a set rate. The instructions tell the cells to die at a set time. In cancer cells, the DNA changes give different instructions. The changes tell the cancer cells to make many more cells quickly. Cancer cells can keep living when healthy cells would die. This causes too many cells.
The cancer cells might form a mass called a tumor. The tumor can grow to invade and destroy healthy body tissue. In time, cancer cells can break away and spread to other parts of the body. When cancer spreads, it's called metastatic cancer.
The DNA changes that lead to breast cancer most often happen in the cells that line the milk ducts. These ducts are tubes designed to carry milk to the nipple. Breast cancer that starts in the ducts is called invasive ductal carcinoma. Breast cancer also can start in cells in the milk glands. These glands, called lobules, are designed to make breast milk. Cancer that happens in the lobules is called invasive lobular carcinoma. Other cells in the breast can become cancer cells, though this isn't common.
Risk factors
Factors that may increase the risk of breast cancer include:
- A family history of breast cancer. If a parent, sibling or child had breast cancer, your risk of breast cancer is increased. The risk is higher if your family has a history of getting breast cancer at a young age. The risk also is higher if you have multiple family members with breast cancer. Still, most people diagnosed with breast cancer don't have a family history of the disease.
- A personal history of breast cancer. If you've had cancer in one breast, you have an increased risk of getting cancer in the other breast.
- A personal history of breast conditions. Certain breast conditions are markers for a higher risk of breast cancer. These conditions include lobular carcinoma in situ, also called LCIS, and atypical hyperplasia of the breast. If you've had a breast biopsy that found one of these conditions, you have an increased risk of breast cancer.
- Beginning your period at a younger age. Beginning your period before age 12 increases your risk of breast cancer.
- Beginning menopause at an older age. Beginning menopause after age 55 increases the risk of breast cancer.
- Being female. Women are much more likely than men are to get breast cancer. Everyone is born with some breast tissue, so anyone can get breast cancer.
- Dense breast tissue. Breast tissue is made up of fatty tissue and dense tissue. Dense tissue is made of milk glands, milk ducts and fibrous tissue. If you have dense breasts, you have more dense tissue than fatty tissue in your breasts. Having dense breasts can make it harder to detect breast cancer on a mammogram. If a mammogram showed that you have dense breasts, your risk of breast cancer is increased. Talk with your healthcare team about other tests you might have in addition to mammograms to look for breast cancer.
- Drinking alcohol. Drinking alcohol increases the risk of breast cancer.
- Having your first child at an older age. Giving birth to your first child after age 30 may increase the risk of breast cancer.
- Having never been pregnant. Having been pregnant one or more times lowers the risk of breast cancer. Never having been pregnant increases the risk.
- Increasing age. The risk of breast cancer goes up as you get older.
- Inherited DNA changes that increase cancer risk. Certain DNA changes that increase the risk of breast cancer can be passed from parents to children. The most well-known changes are called BRCA1 and BRCA2. These changes can greatly increase your risk of breast cancer and other cancers, but not everyone with these DNA changes gets cancer.
- Menopausal hormone therapy. Taking certain hormone therapy medicines to control the symptoms of menopause may increase the risk of breast cancer. The risk is linked to hormone therapy medicines that combine estrogen and progesterone. The risk goes down when you stop taking these medicines.
- Obesity. People with obesity have an increased risk of breast cancer.
- Radiation exposure. If you received radiation treatments to your chest as a child or young adult, your risk of breast cancer is higher.
Things you can do to lower your risk of breast cancer
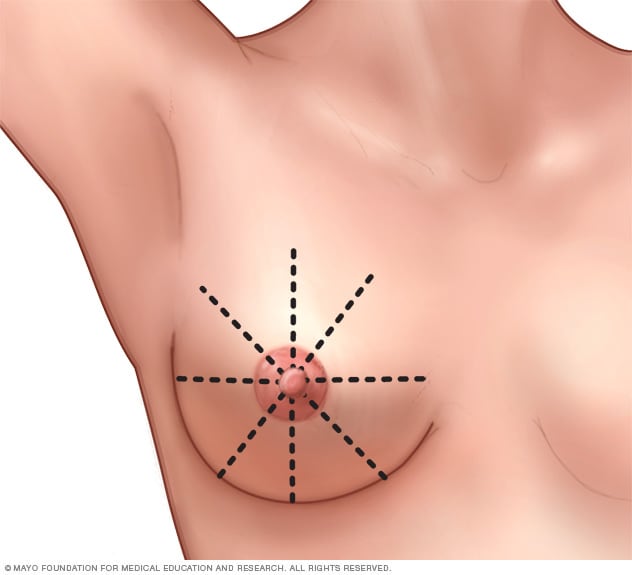
Breast self-exam
To perform a breast self-exam for breast awareness, use a methodical approach that ensures you cover your entire breast. For instance, imagine that your breasts are divided into equal wedges, like pieces of a pie, and sweep your fingers along each piece in toward your nipple.
Making changes in your daily life may help lower your risk of breast cancer. Try to:
- Ask about breast cancer screening. Talk with your doctor or other healthcare professional about when to begin breast cancer screening. Ask about the benefits and risks of screening. Together, you can decide what breast cancer screening tests are right for you.
Become familiar with your breasts through breast self-exam for breast awareness. You may choose to become familiar with your breasts by occasionally inspecting them during a breast self-exam for breast awareness. If there is a new change, a lump or something not typical in your breasts, report it to a healthcare professional right away.
Breast awareness can't prevent breast cancer. But it may help you to better understand the look and feel of your breasts. This might make it more likely that you'll notice if something changes.
- Drink alcohol in moderation, if at all. Limit the amount of alcohol you drink to no more than one drink a day, if you choose to drink. For breast cancer prevention, there is no safe amount of alcohol. So if you're very concerned about your breast cancer risk, you may choose to not drink alcohol.
- Exercise most days of the week. Aim for at least 30 minutes of exercise on most days of the week. If you haven't been active lately, ask a healthcare professional whether it's OK and start slowly.
Limit menopausal hormone therapy. Combination hormone therapy may increase the risk of breast cancer. Talk with a healthcare professional about the benefits and risks of hormone therapy.
Some people have symptoms during menopause that cause discomfort. These people may decide that the risks of hormone therapy are acceptable in order to get relief. To reduce the risk of breast cancer, use the lowest dose of hormone therapy possible for the shortest amount of time.
- Maintain a healthy weight. If your weight is healthy, work to maintain that weight. If you need to lose weight, ask a healthcare professional about healthy ways to lower your weight. Eat fewer calories and slowly increase the amount of exercise.
Medicines and operations for those a high risk of breast cancer
If you have a high risk of breast cancer, you might consider other options to lower the risk. You might have a high risk if you have a family history of breast cancer. Your risk also might be higher if you have a history of precancerous cells in the breast tissue. Talk about your risk with your healthcare team. Your team might have options for lowering your risk, such as:
Preventive medicines. Using estrogen-blocking medicines can lower the risk of breast cancer in those who have a high risk. Options include medicines called selective estrogen receptor modulators and aromatase inhibitors. These medicines also are used as hormone therapy treatment for breast cancer.
These medicines carry a risk of side effects. For this reason, they're only used in those who have a very high risk of breast cancer. Discuss the benefits and risks with your healthcare team.
- Preventive surgery. If you have a very high risk of breast cancer, you may consider having surgery to lower the risk of breast cancer. One option might be surgery to remove the breasts, called prophylactic mastectomy. Another option is surgery to remove the ovaries, called prophylactic oophorectomy. This operation lowers the risk of breast cancer and ovarian cancer.
More Information
- Breast cancer chemoprevention
- Genetic testing for breast cancer: Psychological and social impact
Living with breast cancer?
Connect with others like you for support and answers to your questions in the Breast Cancer support group on Mayo Clinic Connect, a patient community.
Breast Cancer Discussions

95 Replies Fri, Apr 19, 2024

45 Replies Fri, Apr 19, 2024

56 Replies Fri, Apr 19, 2024
- Cancer facts and figures 2023. American Cancer Society. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/2023-cancer-facts-figures.html. Accessed Aug. 9, 2023.
- Abraham J, et al., eds. Breast cancer. In: The Bethesda Handbook of Clinical Oncology. 6th ed. Kindle edition. Wolters Kluwer; 2023. Accessed March 30, 2023.
- Breast cancer. Cancer.Net. https://www.cancer.net/cancer-types/breast-cancer/view-all. Accessed Aug. 2, 2023.
- Mukwende M, et al. Erythema. In: Mind the Gap: A Handbook of Clinical Signs in Black and Brown Skin. St. George's University of London; 2020. https://www.blackandbrownskin.co.uk/mindthegap. Accessed Aug. 10, 2023.
- Townsend CM Jr, et al. Diseases of the breast. In: Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 21st ed. Elsevier; 2022. https://www.clinicalkey.com. Accessed Aug. 2, 2023.
- Breast cancer risk reduction. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1420. Accessed Aug. 2, 2023.
- Breast cancer prevention (PDQ) – Patient version. National Cancer Institute. https://www.cancer.gov/types/breast/patient/breast-prevention-pdq. Accessed Aug. 2, 2023.
- Breast cancer. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1419. Accessed Aug. 2, 2023.
- Klimberg VS, et al., eds. Breast cancer diagnosis and techniques for biopsy. In: Bland and Copeland's The Breast: Comprehensive Management of Benign and Malignant Diseases. 6th ed. Elsevier; 2024. https://www.clinicalkey.com. Accessed Aug. 2, 2023.
- Palliative care. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=3&id=1454. Accessed Aug. 2, 2023.
- Cancer-related fatigue. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=3&id=1424. Accessed Aug. 2, 2023.
- Breast SPOREs. National Cancer Institute. https://trp.cancer.gov/spores/breast.htm. Accessed Aug. 9, 2023.
- Ami TR. Allscripts EPSi. Mayo Clinic. Jan. 31, 2023.
- Ami TR. Allscripts EPSi. Mayo Clinic. April 5, 2023.
- Member institutions. Alliance for Clinical Trials in Oncology. https://www.allianceforclinicaltrialsinoncology.org/main/public/standard.xhtml?path=%2FPublic%2FInstitutions. Accessed Aug. 9, 2023.
- Giridhar KV (expert opinion). Mayo Clinic. Oct. 18, 2023.
- Breast Cancer Education Tool
- Breast cancer staging
- Breast cancer types
- Breast self-examination
- Common questions about breast cancer treatment
- Dragon Boats and Breast Cancer
- Genetic Testing for Breast Cancer
- HER2-positive breast cancer: What is it?
- Infographic: Breast Cancer Risk
- Modified radical mastectomy
- Paulas story A team approach to battling breast cancer
- Pink Sisters
- Simple mastectomy and modified radical mastectomy
- The Long Race Beating Cancer
- Weight Loss After Breast Cancer
- What is breast cancer? An expert explains
Associated Procedures
- 3D mammogram
- Brachytherapy
- BRCA gene test
- Breast cancer risk assessment
- Breast cancer supportive therapy and survivorship
- Breast cancer surgery
- Breast self-exam for breast awareness
- Chemotherapy
- Chemotherapy for breast cancer
- Chest X-rays
- Complete blood count (CBC)
- Hormone therapy for breast cancer
- Molecular breast imaging
- Positron emission tomography scan
- Precision medicine for breast cancer
- Radiation therapy
- Radiation therapy for breast cancer
- Sentinel node biopsy
News from Mayo Clinic
- New study finds triple-negative breast cancer tumors with an increase in immune cells have lower risk of recurrence after surgery April 02, 2024, 04:31 p.m. CDT
- Understanding triple-negative breast cancer and its treatment Jan. 04, 2024, 04:00 p.m. CDT
- Mayo Clinic's DNA study reveals BRCA1 mutations in 3 sisters, prompts life-changing decisions Nov. 04, 2023, 11:00 a.m. CDT
- Beyond BRCA1/2: Pinpointing the risk of inherited breast cancer genes Oct. 28, 2023, 11:00 a.m. CDT
- 17-gene signature linked to remission after triple-negative breast cancer treatment Oct. 21, 2023, 11:00 a.m. CDT
- Mayo Clinic Minute: Does soy increase breast cancer risk? Oct. 17, 2023, 06:30 p.m. CDT
- Mayo Clinic Minute: The importance of supplemental screenings for dense breasts Sept. 26, 2023, 02:28 p.m. CDT
- Mayo Clinic Minute: Why Black women should consider screening for breast cancer earlier June 15, 2023, 04:30 p.m. CDT
- Mayo Clinic Minute: Why some patients with breast tumors could possibly avoid a mastectomy April 18, 2023, 01:30 p.m. CDT
- Patients with multiple tumors in one breast may not need mastectomy, research finds March 28, 2023, 09:00 p.m. CDT
- Mayo Clinic researchers identify women with twice the risk of cancer in both breasts Jan. 19, 2023, 02:58 p.m. CDT
- Short journey for quicker breast cancer care Nov. 17, 2022, 12:00 p.m. CDT
- Mayo Clinic Minute: Why people with breast cancer should ask their health care team about clinical trials Oct. 21, 2022, 04:00 p.m. CDT
- Mayo Clinic receives National Cancer Institute grant for breast cancer research Oct. 20, 2022, 06:47 p.m. CDT
- Mayo Clinic Minute: Determining if you have dense breasts Oct. 13, 2022, 02:05 p.m. CDT
- Mayo Clinic Q&A podcast: Surgical options for breast cancer treatment Oct. 04, 2022, 01:00 p.m. CDT
- Science Saturday: The Living Breast Biobank July 30, 2022, 11:00 a.m. CDT
- Collaborative care, individualized therapy allows patient to celebrate despite cancer diagnosis July 01, 2022, 05:00 p.m. CDT
- Mayo Clinic, Médica Sur expand relationship to advance cancer care June 21, 2022, 09:00 p.m. CDT
- Mayo Clinic Q&A podcast: What to expect after breast cancer June 21, 2022, 12:42 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
For the best browsing experience please enable JavaScript. Instructions for Microsoft Edge and Internet Explorer , other browsers

- About cancer
- Get involved
- Our research
- Funding for researchers
- Cancer types
- Cancer in general
- Causes of cancer
- Coping with cancer
- Health professionals
- Do your own fundraising
- By cancer type
- By cancer subject
- Our funding schemes
- Applying for funding
- Managing your research grant
- How we deliver our research
- Find a shop
- Shop online
- Our eBay shop
- Our organisation
- Current jobs
- Cancer news
Breast cancer
Breast cancer is cancer that starts in the breast tissue. The treatment you need depends on the type of breast cancer you have as well as your general health. Treatments include surgery, chemotherapy, hormone therapy, and radiotherapy.
If breast cancer spreads to another part of the body, it is called secondary breast cancer.
What is breast cancer?
Breast cancer is cancer that starts in the breast tissue. Find out about who gets breast cancer and where it starts.
Symptoms of breast cancer
Symptoms of breast cancer include a lump or thickening in the breast. Find out more about this and other possible symptoms and when you should see your GP.
Getting diagnosed with breast cancer
You usually start by seeing your GP. Or you may have had changes picked up through breast screening. Find out about being referred to a breast clinic and the tests you might have.
Survival for breast cancer
Survival is generally very good for breast cancer, particularly if you are diagnosed early. This is probably because of screening, early diagnosis and improved treatment. Find out more.
Treatment for breast cancer
Treatment for breast cancer depends on a number of factors. Find out about breast cancer treatments, where and how you have them, and how to cope with possible side effects.
Stages and grades of breast cancer
Get information about how doctors stage and grade breast cancer. In the UK, doctors use the TNM system to stage breast cancer. You may also be told about the number staging system.
Types of breast cancer and related breast conditions
There are different types of breast cancer and breast conditions, including breast cancer in men, and conditions related to breast cancer. Find out more about the different types.
Secondary breast cancer
Secondary breast cancer means that a cancer that began in the breast has spread to another part of the body such as the bones or lungs.
Research and clinical trials for breast cancer
Research is looking into all aspects of breast cancer. Find out about the latest UK breast cancer research and clinical trials, and how you can take part.
Living with breast cancer
Get practical, physical and emotional support to help you cope with a diagnosis of breast cancer, and life during and after treatment.
Risks and causes of breast cancer
Read about the factors that can increase or reduce your risk of developing breast cancer.
Breast cancer resources and support organisations
There are many organisations, support groups, books, videos and other resources to help you cope with breast cancer and its treatment. There is also information about mastectomy wear and prosthesis suppliers.
It’s a worrying time for many people and we want to be there for you whenever - and wherever - you need us. Cancer Chat is our fully moderated forum where you can talk to others affected by cancer, share experiences, and get support. Cancer Chat is free to join and available 24 hours a day.
Visit the Cancer Chat forum
About Cancer generously supported by Dangoor Education since 2010.

Find a clinical trial
Search our clinical trials database for all cancer trials and studies recruiting in the UK
Cancer Chat forum
Talk to other people affected by cancer
Nurse helpline 0808 800 4040
Questions about cancer? Call freephone 9 to 5 Monday to Friday or email us

IMAGES
COMMENTS
Advances in Breast Cancer Research. A polyploid giant cancer cell (PGCC) from triple-negative breast cancer. NCI-funded researchers are working to advance our understanding of how to prevent, detect, and treat breast cancer. They are also looking at how to address disparities and improve quality of life for survivors of the disease.
Breast cancer is currently one of the most prevalently diagnosed cancers and the 5th cause of cancer-related deaths with an estimated ... Colombet M., Mery L., Piñeros M., Znaor A., Soerjomataram I., Bray F. International Agency for Research on Cancer; Lyon, France: 2020. [(accessed on 9 July 2021)]. Global Cancer Observatory: Cancer Tomorrow. ...
The Breast Cancer Research Foundation is dedicated to ending breast cancer by advancing the world's most promising research. This year, BCRF is the largest private funder of breast cancer research—and metastatic breast cancer research—worldwide and is the highest-rated breast cancer research organization in the country. Learn More Donate.
Breast Cancer Research Highlights. The American Cancer Society (ACS) helps people with breast cancer in every community. Our research programs have played a role in many of the prevention, screening, and treatment advances that save lives from breast cancer today. And, we continue to fund research to help save even more lives in the future.
Breast Cancer Research is an international, peer-reviewed online journal, publishing original research, reviews, editorials and reports. Open access research articles of exceptional interest are published in all areas of biology and medicine relevant to breast cancer, including normal mammary gland biology, with special emphasis on the genetic, biochemical, and cellular basis of breast cancer.
Research Is the Reason. On the heels of her mom's breast cancer diagnosis, Melissa found out she, too, had breast cancer. Today she credits research for giving them both the best outcome. Breast cancer research is improving care, producing better outcomes and transforming lives while helping us learn more about breast cancer than ever before.
Breast Cancer Research is the highest ranking breast cancer-specific title in the top quartile of oncology journals worldwide. Primarily publishing original ...
Breast Cancer Translational Research Laboratory J.-C. Heuson, Institut Jules Bordet, Hôpital Universitaire de Bruxelles (HUB), Université Libre de Bruxelles (ULB), Brussels, Belgium.
Mortality. The overall breast cancer death rate increased by 0.4% per year from 1975 to 1989, but since has decreased steadily, for a total decline of 43% through 2020. As a result, 460,000 breast cancer deaths were averted in US women from 1989 through 2020.
The Breast Cancer Facts & Figures 2022-2024 report is an educational companion for Breast Cancer Statistics, 2022, a scientific paper published in the American Cancer Society flagship journal, CA: A Cancer Journal for Clinicians. Breast cancer is the most common cancer diagnosed among women in the United States.
The latest research evidence 1 shown that 44.4% of global cancer deaths and 42.0% of global cancer disability-adjusted life years can be attributed to GBD 2019 estimated risk factors. Our study ...
1. Introduction. Having replaced lung cancer as the most commonly diagnosed cancer globally, breast cancer today accounts for 1 in 8 cancer diagnoses and a total of 2.3 million new cases in both sexes combined [].Representing a quarter of all cancer cases in females, it was by far the most commonly diagnosed cancer in women in 2020, and its burden has been growing in many parts of the world ...
The Breast Cancer Research Foundation is a nonprofit organization committed to achieving prevention and a cure for breast cancer. We provide critical funding for cancer research worldwide to fuel advances in tumor biology, genetics, prevention, treatment, metastasis and survivorship.
Research Philosophy. NBCF's mission is to help now and inspire hope to those affected by breast cancer through early detection, education, and support services. This distinguishes NBCF from other breast cancer charities. While we fully support investments in research for a cure or new life-extending therapies, we are focused on helping the ...
Breast cancer is a disease in which abnormal breast cells grow out of control and form tumours. If left unchecked, the tumours can spread throughout the body and become fatal. Breast cancer cells begin inside the milk ducts and/or the milk-producing lobules of the breast. The earliest form (in situ) is not life-threatening and can be detected ...
Possible environmental causes of breast cancer have also received more attention in recent years. While much of the science on this topic is still in its earliest stages, this is an area of active research. Breast cancer prevention. Researchers are looking for ways to help reduce breast cancer risk, especially for women who are at high risk.
Affiliated with the Australasian Society for Breast Disease (ASBD), the European Society for Medical Oncology (ESMO), and the Hong Kong Breast Oncology Group (HKBOG). The Breast is a multidisciplinary open access journal for researchers and clinicians, which focuses on translational and clinical research for the advancement of breast cancer prevention, diagnosis and treatment of all stages.
Breast cancer survival rates have been increasing. And the number of people dying of breast cancer is steadily going down. Much of this is due to the widespread support for breast cancer awareness and funding for research. Advances in breast cancer screening allow healthcare professionals to diagnose breast cancer earlier.
Sadly, secondary breast cancer can't be cured. Researchers are looking at new treatments and combining different treatments to help control the disease and give a good quality of life for as long as possible. Find out about research into treatment for secondary breast cancer.
We champion the latest and most authoritative scientific research from around the world on cancer prevention and survival through diet, weight and physical activity, so that we can help people make informed lifestyle choices to reduce their cancer risk. Choose a one-time amount. $500. $100. $50.
Breast cancer is a group of diseases in which cells in breast tissue change and divide uncontrolled, typically ... ©2019, American Cancer Society, Inc., Surveillance Research Figure 1. Distribution of Female Breast Cancer Subtypes, US, 2012-2016 HR+/HER2-73% HR+/HER2+ 11% HR-/HER2-12%
Find out about breast cancer, including symptoms, diagnosis, treatment, survival, ... Cancer Research UK is a registered charity in England and Wales (1089464), Scotland (SC041666), the Isle of Man (1103) and Jersey (247). A company limited by guarantee. Registered company in England and Wales (4325234) and the Isle of Man (5713F).