About Stanford GSB
- The Leadership
- Dean’s Updates
- School News & History
- Commencement
- Business, Government & Society
- Centers & Institutes
- Center for Entrepreneurial Studies
- Center for Social Innovation
- Stanford Seed

About the Experience
- Learning at Stanford GSB
- Experiential Learning
- Guest Speakers
- Entrepreneurship
- Social Innovation
- Communication
- Life at Stanford GSB
- Collaborative Environment
- Activities & Organizations
- Student Services
- Housing Options
- International Students
Full-Time Degree Programs
- Why Stanford MBA
- Academic Experience
- Financial Aid
- Why Stanford MSx
- Research Fellows Program
- See All Programs
Non-Degree & Certificate Programs
- Executive Education
- Stanford Executive Program
- Programs for Organizations
- The Difference
- Online Programs
- Stanford LEAD
- Seed Transformation Program
- Aspire Program
- Seed Spark Program
- Faculty Profiles
- Academic Areas
- Awards & Honors
- Conferences
Faculty Research
- Publications
- Working Papers
- Case Studies
Research Hub
- Research Labs & Initiatives
- Business Library
- Data, Analytics & Research Computing
- Behavioral Lab
Research Labs
- Cities, Housing & Society Lab
- Golub Capital Social Impact Lab
Research Initiatives
- Corporate Governance Research Initiative
- Corporations and Society Initiative
- Policy and Innovation Initiative
- Rapid Decarbonization Initiative
- Stanford Latino Entrepreneurship Initiative
- Value Chain Innovation Initiative
- Venture Capital Initiative
- Career & Success
- Climate & Sustainability
- Corporate Governance
- Culture & Society
- Finance & Investing
- Government & Politics
- Leadership & Management
- Markets & Trade
- Operations & Logistics
- Opportunity & Access
- Organizational Behavior
- Political Economy
- Social Impact
- Technology & AI
- Opinion & Analysis
- Email Newsletter
Welcome, Alumni
- Communities
- Digital Communities & Tools
- Regional Chapters
- Women’s Programs
- Identity Chapters
- Find Your Reunion
- Career Resources
- Job Search Resources
- Career & Life Transitions
- Programs & Services
- Career Video Library
- Alumni Education
- Research Resources
- Volunteering
- Alumni News
- Class Notes
- Alumni Voices
- Contact Alumni Relations
- Upcoming Events
Admission Events & Information Sessions
- MBA Program
- MSx Program
- PhD Program
- Alumni Events
- All Other Events
- Operations, Information & Technology
- Classical Liberalism
- The Eddie Lunch
- Accounting Summer Camp
- Videos, Code & Data
- California Econometrics Conference
- California Quantitative Marketing PhD Conference
- California School Conference
- China India Insights Conference
- Homo economicus, Evolving
- Political Economics (2023–24)
- Scaling Geologic Storage of CO2 (2023–24)
- A Resilient Pacific: Building Connections, Envisioning Solutions
- Adaptation and Innovation
- Changing Climate
- Civil Society
- Climate Impact Summit
- Climate Science
- Corporate Carbon Disclosures
- Earth’s Seafloor
- Environmental Justice
- Operations and Information Technology
- Organizations
- Sustainability Reporting and Control
- Taking the Pulse of the Planet
- Urban Infrastructure
- Watershed Restoration
- Junior Faculty Workshop on Financial Regulation and Banking
- Ken Singleton Celebration
- Marketing Camp
- Quantitative Marketing PhD Alumni Conference
- Presentations
- Theory and Inference in Accounting Research
- Stanford Closer Look Series
- Quick Guides
- Core Concepts
- Journal Articles
- Glossary of Terms
- Faculty & Staff
- Researchers & Students
- Research Approach
- Charitable Giving
- Financial Health
- Government Services
- Workers & Careers
- Short Course
- Adaptive & Iterative Experimentation
- Incentive Design
- Social Sciences & Behavioral Nudges
- Bandit Experiment Application
- Conferences & Events
- Get Involved
- Reading Materials
- Teaching & Curriculum
- Energy Entrepreneurship
- Faculty & Affiliates
- SOLE Report
- Responsible Supply Chains
- Current Study Usage
- Pre-Registration Information
- Participate in a Study
A How-To Guide for Conducting Retrospective Analyses: Example COVID-19 Study
In the urgent setting of the COVID-19 pandemic, treatment hypotheses abound, each of which requires careful evaluation. A randomized controlled trial generally provides the strongest possible evaluation of a treatment, but the efficiency and effectiveness of the trial depend on the existing evidence supporting the treatment. The researcher must therefore compile a body of evidence justifying the use of time and resources to further investigate a treatment hypothesis in a trial. An observational study can help provide this evidence, but the lack of randomized exposure and the researcher’s inability to control treatment administration and data collection introduce significant challenges for non-experimental studies. A proper analysis of observational health care data thus requires an extensive background in a diverse set of topics ranging from epidemiology and causal analysis to relevant medical specialties and data sources. Here we provide 10 rules that serve as an end-to-end introduction to retrospective analyses of observational health care data. A running example of a COVID-19 study presents a practical implementation of each rule in the context of a specific treatment hypothesis. When carefully designed and properly executed, a retrospective analysis framed around these rules will inform the decisions of whether and how to investigate a treatment hypothesis in a randomized controlled trial.
- Priorities for the GSB's Future
- See the Current DEI Report
- Supporting Data
- Research & Insights
- Share Your Thoughts
- Search Fund Primer
- Affiliated Faculty
- Faculty Advisors
- Louis W. Foster Resource Center
- Defining Social Innovation
- Impact Compass
- Global Health Innovation Insights
- Faculty Affiliates
- Student Awards & Certificates
- Changemakers
- Dean Jonathan Levin
- Dean Garth Saloner
- Dean Robert Joss
- Dean Michael Spence
- Dean Robert Jaedicke
- Dean Rene McPherson
- Dean Arjay Miller
- Dean Ernest Arbuckle
- Dean Jacob Hugh Jackson
- Dean Willard Hotchkiss
- Faculty in Memoriam
- Stanford GSB Firsts
- Certificate & Award Recipients
- Teaching Approach
- Analysis and Measurement of Impact
- The Corporate Entrepreneur: Startup in a Grown-Up Enterprise
- Data-Driven Impact
- Designing Experiments for Impact
- Digital Business Transformation
- The Founder’s Right Hand
- Marketing for Measurable Change
- Product Management
- Public Policy Lab: Financial Challenges Facing US Cities
- Public Policy Lab: Homelessness in California
- Lab Features
- Curricular Integration
- View From The Top
- Formation of New Ventures
- Managing Growing Enterprises
- Startup Garage
- Explore Beyond the Classroom
- Stanford Venture Studio
- Summer Program
- Workshops & Events
- The Five Lenses of Entrepreneurship
- Leadership Labs
- Executive Challenge
- Arbuckle Leadership Fellows Program
- Selection Process
- Training Schedule
- Time Commitment
- Learning Expectations
- Post-Training Opportunities
- Who Should Apply
- Introductory T-Groups
- Leadership for Society Program
- Certificate
- 2023 Awardees
- 2022 Awardees
- 2021 Awardees
- 2020 Awardees
- 2019 Awardees
- 2018 Awardees
- Social Management Immersion Fund
- Stanford Impact Founder Fellowships and Prizes
- Stanford Impact Leader Prizes
- Social Entrepreneurship
- Stanford GSB Impact Fund
- Economic Development
- Energy & Environment
- Stanford GSB Residences
- Environmental Leadership
- Stanford GSB Artwork
- A Closer Look
- California & the Bay Area
- Voices of Stanford GSB
- Business & Beneficial Technology
- Business & Sustainability
- Business & Free Markets
- Business, Government, and Society Forum
- Second Year
- Global Experiences
- JD/MBA Joint Degree
- MA Education/MBA Joint Degree
- MD/MBA Dual Degree
- MPP/MBA Joint Degree
- MS Computer Science/MBA Joint Degree
- MS Electrical Engineering/MBA Joint Degree
- MS Environment and Resources (E-IPER)/MBA Joint Degree
- Academic Calendar
- Clubs & Activities
- LGBTQ+ Students
- Military Veterans
- Minorities & People of Color
- Partners & Families
- Students with Disabilities
- Student Support
- Residential Life
- Student Voices
- MBA Alumni Voices
- A Week in the Life
- Career Support
- Employment Outcomes
- Cost of Attendance
- Knight-Hennessy Scholars Program
- Yellow Ribbon Program
- BOLD Fellows Fund
- Application Process
- Loan Forgiveness
- Contact the Financial Aid Office
- Evaluation Criteria
- GMAT & GRE
- English Language Proficiency
- Personal Information, Activities & Awards
- Professional Experience
- Letters of Recommendation
- Optional Short Answer Questions
- Application Fee
- Reapplication
- Deferred Enrollment
- Joint & Dual Degrees
- Entering Class Profile
- Event Schedule
- Ambassadors
- New & Noteworthy
- Ask a Question
- See Why Stanford MSx
- Is MSx Right for You?
- MSx Stories
- Leadership Development
- Career Advancement
- Career Change
- How You Will Learn
- Admission Events
- Personal Information
- Information for Recommenders
- GMAT, GRE & EA
- English Proficiency Tests
- After You’re Admitted
- Daycare, Schools & Camps
- U.S. Citizens and Permanent Residents
- Requirements
- Requirements: Behavioral
- Requirements: Quantitative
- Requirements: Macro
- Requirements: Micro
- Annual Evaluations
- Field Examination
- Research Activities
- Research Papers
- Dissertation
- Oral Examination
- Current Students
- Education & CV
- International Applicants
- Statement of Purpose
- Reapplicants
- Application Fee Waiver
- Deadline & Decisions
- Job Market Candidates
- Academic Placements
- Stay in Touch
- Faculty Mentors
- Current Fellows
- Standard Track
- Fellowship & Benefits
- Group Enrollment
- Program Formats
- Developing a Program
- Diversity & Inclusion
- Strategic Transformation
- Program Experience
- Contact Client Services
- Campus Experience
- Live Online Experience
- Silicon Valley & Bay Area
- Digital Credentials
- Faculty Spotlights
- Participant Spotlights
- Eligibility
- International Participants
- Stanford Ignite
- Frequently Asked Questions
- Founding Donors
- Location Information
- Participant Profile
- Network Membership
- Program Impact
- Collaborators
- Entrepreneur Profiles
- Company Spotlights
- Seed Transformation Network
- Responsibilities
- Current Coaches
- How to Apply
- Meet the Consultants
- Meet the Interns
- Intern Profiles
- Collaborate
- Research Library
- News & Insights
- Program Contacts
- Databases & Datasets
- Research Guides
- Consultations
- Research Workshops
- Career Research
- Research Data Services
- Course Reserves
- Course Research Guides
- Material Loan Periods
- Fines & Other Charges
- Document Delivery
- Interlibrary Loan
- Equipment Checkout
- Print & Scan
- MBA & MSx Students
- PhD Students
- Other Stanford Students
- Faculty Assistants
- Research Assistants
- Stanford GSB Alumni
- Telling Our Story
- Staff Directory
- Site Registration
- Alumni Directory
- Alumni Email
- Privacy Settings & My Profile
- Success Stories
- The Story of Circles
- Support Women’s Circles
- Stanford Women on Boards Initiative
- Alumnae Spotlights
- Insights & Research
- Industry & Professional
- Entrepreneurial Commitment Group
- Recent Alumni
- Half-Century Club
- Fall Reunions
- Spring Reunions
- MBA 25th Reunion
- Half-Century Club Reunion
- Faculty Lectures
- Ernest C. Arbuckle Award
- Alison Elliott Exceptional Achievement Award
- ENCORE Award
- Excellence in Leadership Award
- John W. Gardner Volunteer Leadership Award
- Robert K. Jaedicke Faculty Award
- Jack McDonald Military Service Appreciation Award
- Jerry I. Porras Latino Leadership Award
- Tapestry Award
- Student & Alumni Events
- Executive Recruiters
- Interviewing
- Land the Perfect Job with LinkedIn
- Negotiating
- Elevator Pitch
- Email Best Practices
- Resumes & Cover Letters
- Self-Assessment
- Whitney Birdwell Ball
- Margaret Brooks
- Bryn Panee Burkhart
- Margaret Chan
- Ricki Frankel
- Peter Gandolfo
- Cindy W. Greig
- Natalie Guillen
- Carly Janson
- Sloan Klein
- Sherri Appel Lassila
- Stuart Meyer
- Tanisha Parrish
- Virginia Roberson
- Philippe Taieb
- Michael Takagawa
- Terra Winston
- Johanna Wise
- Debbie Wolter
- Rebecca Zucker
- Complimentary Coaching
- Changing Careers
- Work-Life Integration
- Career Breaks
- Flexible Work
- Encore Careers
- Join a Board
- D&B Hoovers
- Data Axle (ReferenceUSA)
- EBSCO Business Source
- Global Newsstream
- Market Share Reporter
- ProQuest One Business
- Student Clubs
- Entrepreneurial Students
- Stanford GSB Trust
- Alumni Community
- How to Volunteer
- Springboard Sessions
- Consulting Projects
- 2020 – 2029
- 2010 – 2019
- 2000 – 2009
- 1990 – 1999
- 1980 – 1989
- 1970 – 1979
- 1960 – 1969
- 1950 – 1959
- 1940 – 1949
- Service Areas
- ACT History
- ACT Awards Celebration
- ACT Governance Structure
- Building Leadership for ACT
- Individual Leadership Positions
- Leadership Role Overview
- Purpose of the ACT Management Board
- Contact ACT
- Business & Nonprofit Communities
- Reunion Volunteers
- Ways to Give
- Fiscal Year Report
- Business School Fund Leadership Council
- Planned Giving Options
- Planned Giving Benefits
- Planned Gifts and Reunions
- Legacy Partners
- Giving News & Stories
- Giving Deadlines
- Development Staff
- Submit Class Notes
- Class Secretaries
- Board of Directors
- Health Care
- Sustainability
- Class Takeaways
- All Else Equal: Making Better Decisions
- If/Then: Business, Leadership, Society
- Grit & Growth
- Think Fast, Talk Smart
- Spring 2022
- Spring 2021
- Autumn 2020
- Summer 2020
- Winter 2020
- In the Media
- For Journalists
- DCI Fellows
- Other Auditors
- Academic Calendar & Deadlines
- Course Materials
- Entrepreneurial Resources
- Campus Drive Grove
- Campus Drive Lawn
- CEMEX Auditorium
- King Community Court
- Seawell Family Boardroom
- Stanford GSB Bowl
- Stanford Investors Common
- Town Square
- Vidalakis Courtyard
- Vidalakis Dining Hall
- Catering Services
- Policies & Guidelines
- Reservations
- Contact Faculty Recruiting
- Lecturer Positions
- Postdoctoral Positions
- Accommodations
- CMC-Managed Interviews
- Recruiter-Managed Interviews
- Virtual Interviews
- Campus & Virtual
- Search for Candidates
- Think Globally
- Recruiting Calendar
- Recruiting Policies
- Full-Time Employment
- Summer Employment
- Entrepreneurial Summer Program
- Global Management Immersion Experience
- Social-Purpose Summer Internships
- Process Overview
- Project Types
- Client Eligibility Criteria
- Client Screening
- ACT Leadership
- Social Innovation & Nonprofit Management Resources
- Develop Your Organization’s Talent
- Centers & Initiatives
- Student Fellowships
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, automatically generate references for free.
- Knowledge Base
- Methodology
- What Is a Retrospective Cohort Study? | Definition & Examples
What Is a Retrospective Cohort Study? | Definition & Examples
Published on 10 February 2023 by Tegan George . Revised on 19 June 2023.
A retrospective cohort study is a type of observational study that focuses on individuals who have an exposure to a disease or risk factor in common. Retrospective cohort studies analyse the health outcomes over a period of time to form connections and assess the risk of a given outcome associated with a given exposure.
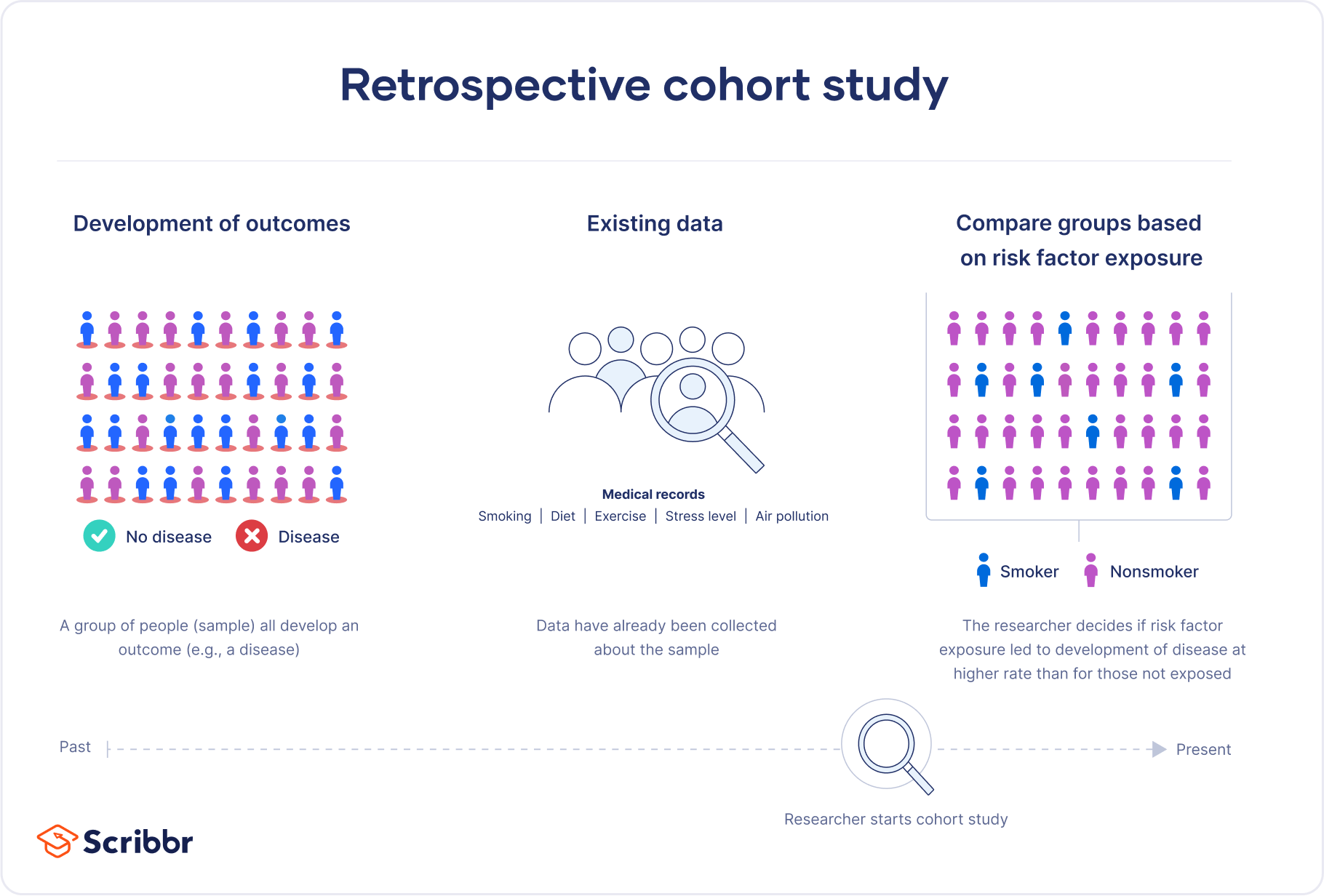
It is crucial to note that in order to be considered a retrospective cohort study, your participants must already possess the disease or health outcome being studied.
Table of contents
When to use a retrospective cohort study, examples of retrospective cohort studies, advantages and disadvantages of retrospective cohort studies, frequently asked questions.
Retrospective cohort studies are a type of observational study . They are often used in fields related to medicine to study the effect of exposures on health outcomes. While most observational studies are qualitative in nature, retrospective cohort studies are often quantitative , as they use preexisting secondary research data. They can be used to conduct both exploratoy research and explanatory research .
Retrospective cohort studies are often used as an intermediate step between a weaker preliminary study and a prospective cohort study , as the results gleaned from a retrospective cohort study strengthen assumptions behind a future prospective cohort study.
A retrospective cohort study could be a good fit for your research if:
- A prospective cohort study is not (yet) feasible for the variables you are investigating.
- You need to quickly examine the effect of an exposure, outbreak, or treatment on an outcome.
- You are seeking to investigate an early-stage or potential association between your variables of interest.
Retrospective cohort studies use secondary research data, such as existing medical records or databases, to identify a group of people with an exposure or risk factor in common. They then observe their health outcomes over time. Case-control studies rely on primary research , comparing a group of participants with a condition of interest to a group lacking that condition in real time.
Prevent plagiarism, run a free check.
Retrospective cohort studies are common in fields like medicine, epidemiology, and healthcare.
You collect data from participants’ exposure to organophosphates, focusing on variables like the timing and duration of exposure, and analyse the health effects of the exposure. Example: Healthcare retrospective cohort study You are examining the relationship between tanning bed use and the incidence of skin cancer diagnoses.
Retrospective cohort studies can be a good fit for many research projects, but they have their share of advantages and disadvantages.
Advantages of retrospective cohort studies
- Retrospective cohort studies are a great choice if you have any ethical considerations or concerns about your participants that prevent you from pursuing a traditional experimental design .
- Retrospective cohort studies are quite efficient in terms of time and budget. They require fewer subjects than other research methods and use preexisting secondary research data to analyse them.
- Retrospective cohort studies are particularly useful when studying rare or unusual exposures, as well as diseases with a long latency or incubation period where prospective cohort studies cannot yet form conclusions.
Disadvantages of retrospective cohort studies
- Like many observational studies, retrospective cohort studies are at high risk for many research biases . They are particularly at risk for recall bias and observer bias due to their reliance on memory and self-reported data.
- Retrospective cohort studies are not a particularly strong standalone method, as they can never establish causality . This leads to low internal validity and external validity .
- As most patients will have had a range of healthcare professionals involved in their care over their lifetime, there is significant variability in the measurement of risk factors and outcomes. This leads to issues with reliability and credibility of data collected.
The primary difference between a retrospective cohort study and a prospective cohort study is the timing of the data collection and the direction of the study.
A retrospective cohort study looks back in time. It uses preexisting secondary research data to examine the relationship between an exposure and an outcome. Data is collected after the outcome you’re studying has already occurred.
Alternatively, a prospective cohort study follows a group of individuals over time. It collects data on both the exposure and the outcome of interest as they are occurring. Data is collected before the outcome of interest has occurred.
Retrospective cohort studies are at high risk for research biases like recall bias . Whenever individuals are asked to recall past events or exposures, recall bias can occur. This is because individuals with a certain disease or health outcome of interest are more likely to remember and/or report past exposures differently to individuals without that outcome. This can result in an overestimation or underestimation of the true relationship between variables and affect your research.
No, retrospective cohort studies cannot establish causality on their own.
Like other types of observational studies , retrospective cohort studies can suggest associations between an exposure and a health outcome. They cannot prove without a doubt, however, that the exposure studied causes the health outcome.
In particular, retrospective cohort studies suffer from challenges arising from the timing of data collection , research biases like recall bias , and how variables are selected. These lead to low internal validity and the inability to determine causality.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the ‘Cite this Scribbr article’ button to automatically add the citation to our free Reference Generator.
George, T. (2023, June 19). What Is a Retrospective Cohort Study? | Definition & Examples. Scribbr. Retrieved 14 May 2024, from https://www.scribbr.co.uk/research-methods/retrospective-cohort-studies/
Is this article helpful?
Tegan George
Other students also liked, what is a case-control study | definition & examples, what is an observational study | guide & examples, what is recall bias | definition & examples.
Retrospective Research
‘Is the Use of Broad Consent for Retrospective Research on Data and Tissue Possible in the Framework of GDPR?’
- First Online: 27 December 2023
Cite this chapter

- Balázs Hohmann 7 &
- Gergő Kollár 7
97 Accesses
The study outlines the framework for the possibility of using previously collected and stored personal health data where the data subject has given broad consent to the processing of his or her data but the consent does not necessarily extend expressly in its wording to all subsequent research and health uses. In the light of the findings of the study, while, in the case of prospective research, consent can be an excellent legal basis for the data management of research activities, in the case of retrospective research, broad consent may in some cases raise more concerns about the lawfulness of data processing than dissolving. In these cases, where research is carried out on personal health data already obtained, the public interest or legitimate interests pursued by the controller may be the appropriate legal basis in the first place, provided that the conditions are met. This makes data processing more predictable, independent of the data subject’s consent, while, of course, maintaining the rights of other data subjects. Nevertheless, in the case of biobanks, consent was typically the legal basis used when the personal data were originally collected, and the study clarifies the requirements to be taken into account in this case.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC (General Data Protection Regulation) (Text with EEA relevance), O.J. 4.5.2016 L 119/1.
Directive 95/46/EC of the European Parliament and of the Council of 24 October 1995 on the protection of individuals with regard to the processing of personal data and on the free movement of such data.
Del Rio C, Malani PN (2020) COVID-19—new insights on a rapidly changing epidemic. Jama 323:1339–1340. https://doi.org/10.1001/jama.2020.3072
Article Google Scholar
European Commission (2012) Biobanks for Europe – a challenge for governance. Report of the Expert Group on Dealing with Ethical and Regulatory Challenges of International Biobank Research
Google Scholar
European Data Protection Board (2020) Guidelines 03/2020 on the processing of data concerning health for the purpose of scientific research in the context of the COVID-19 outbreak
Gefen G, Ben-Porat O, Tennenholtz M, Yom-Tov E (2020) Privacy, altruism, and experience: estimating the perceived value of Internet data for medical uses. In: Seghrouchni et al (eds) Companion proceedings of the web conference 2020. Association for Computing Machinery, New York, pp 552–556
Chapter Google Scholar
Kaye J, Briceño Moraia L, Curren L, Bell J, Mitchell C, Soini S, Hoppe N, Øien M, Rial-Sebbag E (2016) Consent for biobanking: the legal frameworks of countries in the BioSHaRE-EU Project. Biopreserv Biobank 14:195–200
Sim J, Wright C (2000) Research in health care: concepts, designs and methods. Nelson Thornes, Cheltenham
Staunton C, Slokenberga S, Mascalzoni D (2019) The GDPR and the research exemption: considerations on the necessary safeguards for research biobanks. Eur J Hum Genet 27:1159–1167
Steinsbekk KS, Kåre Myskja B, Solberg B (2013) Broad consent versus dynamic consent in biobank research: is passive participation an ethical problem? Eur J Hum Genet 21:897–902. https://doi.org/10.1038/ejhg.2012.282
Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ (2006) Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc 13:121–126
Wendler D (2006) One-time general consent for research on biological samples. BMJ 332(7540):544–547. https://doi.org/10.1136/bmj.332.7540.544
Widmer MA, Swanson RC, Zink BJ, Pines JM (2018) Complex systems thinking in emergency medicine: a novel paradigm for a rapidly changing and interconnected health care landscape. J Eval Clin Pract 24:629–634. https://doi.org/10.1111/jep.12862
Download references
Author information
Authors and affiliations.
Faculty of Law, University of Pécs, Pécs, Hungary
Balázs Hohmann & Gergő Kollár
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Balázs Hohmann .
Editor information
Editors and affiliations.
Institute CNR-IFAC, National Research Council of Italy, Florence Research Area, Italy
Valentina Colcelli
Roberto Cippitani
Pathologisches Institut, Universitätsklinikum Mannheim GmbH, Mannheim, Germany
Christoph Brochhausen-Delius
Faculty of Law, University of Regensburg, Regensburg, Germany
Rainer Arnold
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Hohmann, B., Kollár, G. (2023). Retrospective Research. In: Colcelli, V., Cippitani, R., Brochhausen-Delius, C., Arnold, R. (eds) GDPR Requirements for Biobanking Activities Across Europe. Springer, Cham. https://doi.org/10.1007/978-3-031-42944-6_40
Download citation
DOI : https://doi.org/10.1007/978-3-031-42944-6_40
Published : 27 December 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-42943-9
Online ISBN : 978-3-031-42944-6
eBook Packages : Law and Criminology Law and Criminology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
- Retrospective studies
- Research design
- Get an email alert for Retrospective studies
- Get the RSS feed for Retrospective studies
Showing 1 - 13 of 139
View by: Cover Page List Articles
Sort by: Recent Popular
Catheter ablation of atrial arrhythmias in cardiac amyloidosis: Impact on heart failure and mortality
Philippe Maury, Kevin Sanchis, [ ... ], Nicolas Lellouche
A retrospective comparison of the biceps femoris long head muscle structure in athletes with and without hamstring strain injury history
Gokhan Yagiz, Meiky Fredianto, [ ... ], Hans-Peter Kubis
The effect of obligatory Padua prediction scoring in hospitalized medically ill patients: A retrospective cohort study
Genady Drozdinsky, Oren Zusman, [ ... ], Anat Gafter-Gvili
Screening for the risk of canine impaction, what are the presumptive signs and how does it affect orthodontics? A cross-sectional study in France
Damien Brézulier, Steeven Carnet, Alexia Marie-Cousin, Jean-Louis Sixou
Topical gabapentin solution for the management of burning mouth syndrome: A retrospective study
Amanda Gramacy, Alessandro Villa
Contraction reserve in high resolution manometry is correlated with lower esophageal acid exposure time in patients with normal esophageal motility: A retrospective observational study
Yaoyao Lu, Linling Lv, Jinlin Yang, Zhihui Yi
2 and all-cause mortality of patients suffering from sepsis-associated encephalopathy after ICU admission: A retrospective study">Association between the first 24 hours PaCO 2 and all-cause mortality of patients suffering from sepsis-associated encephalopathy after ICU admission: A retrospective study
Honglian Luo, Gang Li, [ ... ], Wei Shen
Test cricketers score quickly during the ‘nervous nineties’: Evidence from a regression discontinuity design
Leo Roberts, Daniel R. Little, Mervyn Jackson, Matthew J. Spittal
The rupture risk factors of mirror intracranial aneurysms: A systematic review and meta-analysis based on morphological and hemodynamic parameters
Huang Yong-Wei, Xiao-Yi Wang, Zong-Ping Li, Xiao-Shuang Yin
Propensity score-matched analysis of physician-controlled wire-guided cannulation as an effective technique against difficult cannulation in endoscopic retrograde cholangiopancreatography: A retrospective study
Han Jo Jeon, Jae Min Lee, [ ... ], Hong Sik Lee
Hypoxia as a potential cause of dyspareunia
Karel Hurt, Frantisek Zahalka, [ ... ], Martin Halad
Efficacy and tolerance of second-generation antipsychotics in anorexia nervosa: A systematic scoping review
Solène Thorey, Corinne Blanchet, [ ... ], Emilie Carretier
Exposure to dogs and cats and risk of asthma: A retrospective study
Yu Taniguchi, Maasa Kobayashi
Connect with Us
- PLOS ONE on Twitter
- PLOS on Facebook
- Search Menu
- Advance articles
- Author Interviews
- Research Curations
- Author Guidelines
- Open Access
- Submission Site
- Why Submit?
- About Journal of Consumer Research
- Editorial Board
- Advertising and Corporate Services
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
- WHAT IS THE FUTURE OF METHODOLOGY IN JCR?
Author notes
- < Previous
The Future of Consumer Research Methods: Lessons of a Prospective Retrospective
- Article contents
- Figures & tables
- Supplementary Data
Stacy Wood, The Future of Consumer Research Methods: Lessons of a Prospective Retrospective, Journal of Consumer Research , Volume 51, Issue 1, June 2024, Pages 151–156, https://doi.org/10.1093/jcr/ucae017
- Permissions Icon Permissions
Looking back at 50 years of Journal of Consumer Research methods and interviewing some of the field’s most respected methodologists, this article seeks to craft a core set of best practices for scholars in consumer research. From perennial issues like conceptual validity to emerging issues like data integrity and replicability, the advice offered by our experts can help scholars improve the way they approach their research questions, provide empirical evidence that instills confidence, use new tools to make research more inclusive or descriptive of the “real world,” and seek to become thought leaders.
Turning 50 is a reflective milestone for people and for journals. We can look back on fifty years of arduous labor, fruitful creation, bitter debate, and hard-won evolution. And, if we ignore theory, simply reflecting on the past, present, and future of consumer research methods , we have more than enough to consider. What does the history of consumer research methodology say about what could (or should) emerge in the next 50 years?
To begin, we can look back to the first episode of the Journal of Consumer Research ( JCR ), Volume 1(1), published in June 1974 and containing nine articles. The authors’ names are a Who’s Who list that we know primarily from legend (e.g., Katona, Day, Jacoby, Ferber), though one author, the prolific James R. Bettman, retired only this year. The methodologies used in the empirical papers are a pragmatic and effort-intensive collection: a set of four 20–30 minute interviews with 289 school-age boys (1st, 3rd, 5th grades) using independently trained interviewers and coders; personal interviews with 793 heads of household (HOH) in California with sample representative to state demographics and a second follow-up interview with 192 HOHs, a 4 × 4 experimental design of 192 “paid volunteer” Indiana housewives, a set of two interviews after 1 year of marriage and 2 years of marriage of ∼230 Illinois newlyweds, questionnaires about 25 purchases separately presented to husband–wife dyads in Belgium, and a questionnaire to 108 Indiana University students who reported being smokers. One methodological paper proposed a novel statistical analysis of consumer decision nets and verbal decision protocols. For those who believe that it used to be easy to do “just one study” for JCR in the good old days, the effort and deep care put into both the conceptual and external validity of data collection will belie that myth.
WHAT IS THE FUTURE OF METHODOLOGY IN JCR ?
The very first article in the very first issue of JCR speaks directly to our question of the future of consumer research. Fifty years ago, George Katona argued that the distinction between consumer research and traditional economic research on consumption (as would be appropriate in this then-new journal) was primarily a function of methodology . Katona (1974) sees the origin of true consumer research in the 1940s, saying “The survey method for collecting data on consumer behavior was practically unknown in economics immediately after World War II when the first surveys on the size and distribution of income, asset, and major expenditures were initiated with representative samples. Measures of both consumer attitudes and expectations were then developed” (1). While traditional economists might seek to find a single immutable human tendency underpinning a focal economic phenomenon, the consumer researcher was more interested in a wider descriptive exploration that would yield richer understanding. The consumer researcher, then, needed different data, including subjective reports of satisfaction, expectations, and perceived wealth. With different research questions, Katona explained that consumer research would focus more on micro-data and patterns of small situational moderators. He predicted that many economists would struggle to adopt behavioral research questions and methods but ended by stating “Looking back on three decades of research on consumer behavior, the proponents of behavioral studies of economic affairs have good reason for satisfaction.”
Katona argued that methodologies needed to evolve because the questions being asked about consumers were changing—a phenomenon we see today. Similarly, we can look at the “why and how” of our current labors to predict emergent methodologies and methodological issues. To this end, I conducted interviews with four consumer scholars known for their mastery of method and analysis, John Lynch, Leigh McAlister, Craig Thompson, and Rebecca Ratner, and asked them to reflect on the methodological history of JCR with an eye to the future.
Better Research Questions
A common refrain from our experts was the perennial challenge of starting with a “really good” research question. When asked, “What is the most important thing with methodology?” Leigh McAlister was quick to reply, “We are so obsessed with methodology, we’ve lost track of the questions .” The question, then, is what makes a question good? The answer, as I heard it, was less intuitive than might be expected.
First, we must distinguish between our research question as a program of work and as a particular project. For the former, our research questions are often too small. Good questions require that we sit and listen to real practitioners, that we learn how systems and supply chains work, that we actively explore the perspective from different communities’ lens, that we talk to people we disagree with, that we assume that effects will always be conditional, that we assume that effects are likely to change with time, that we wonder about downstream phenomena, and that we “get meta.” When we have that expansive expertise as our research raison d’etre , then we are better able to see what specific projects are interesting, how they could have impact, and how they might best be tested with confidence.
On the other hand, for the research question that drives any particular project, we are often much too broad. Here, we need focused purpose and focused conceptualization. A bad research question is one that posits an unreasonable generalization and then grudgingly offers a few boundary conditions. One characteristic of good questions is that they seem like something you could nail down with a few studies: (1) the population you need to study is identifiable, accessible, and compelling, (2) the context is specific and consequential, and (3) the conceptualization is clear, logical, and concrete enough to be operationalized closely.
Having invested in a broad research question for our program of study, we have the knowledge base, the long-term perspective, and the time to see the results of any single research question in a project as cumulative, adding to a more nuanced and more confident knowledge about what’s happening (and why) in our domain of interest. I know from experience that having a conceptually diverse portfolio of projects is a dangerously enticing temptation for scholars—so very interesting but requiring an exhausting amount of work to keep from doing each in a superficial way. At some point, scholars must find their one true thing—the research domain where they will invest their bounded resources, build grounded knowledge over years, and establish thought leadership. However, in a long and rich career, many of us will have more than one research focus in that span and that can help keep us motivated—what my old USC colleague, Bill Bearden, called the “fire in the belly.”
It is notable that our experts call us to consider how we choose our questions as two papers appearing in the special issue speak to the outcome. Wang et al. (2024) explore how the impact that any one paper may have is a function of its novelty in either topic, finding, or combinatorial approach—suggesting the core of what is an inherently interesting research question. Looking beyond any one paper, Pham, Wu, and Wang (2024) seek to recognize and conceptualize thought leadership as the combination of the amount of research that scholars publish and the impact of those publications. Their impact metric shows that having a clear focus on one’s work is often a common characteristic of scholars known as thought leaders. These articles offer both guidance to younger scholars seeking to build programs of research and, to more experienced scholars, a way to look at scholarly output through a new lens.
More Critical Consideration of Conceptual Validity
With an appropriately rich research question driving us and a sufficiently specific research question framing a project, are we then ready to talk about methodology? Not so fast, our experts warned; we have not yet emphasized the importance of conceptual validity ( MacKenzie 2003 ). As John Lynch said, “Validity is not a function of research technique, but a function of the inevitable incompleteness of our understanding of the phenomena we study.”
The experts note that, over the years, growing sophistication of analysis in the Journal of Consumer Research (and other journals, to be fair) has led some researchers to mistakenly believe “that fancy analytical models correct for everything.” Yet, others have outlined the danger of overemphasizing analytical sophistication to the detriment of other research basics ( Lehmann, McAlister, and Staelin 2011 ). In any study, what can we say with complete confidence about conceptual validity? We can say that we collected data in the form of specific questions or observations from a specific population under conditions that we altered in specific ways. As readers of scientific papers, we often struggle to understand exactly what these specifics were because they are re-named with conceptual labels assigned by the researcher. Thus, a researcher might require a participant to watch a clock while making a choice and then label that anything from time pressure to temporal salience to cognitive load. Perhaps, then, we need to be more descriptive about our operationalizations and, as our experts emphasize, more aware how stimulus-dependent and context-dependent our studies are. As we assess the nature of our own findings and those of others, we must try to learn from failures to replicate findings that are counter to expectations. It suggests that multi-pronged approaches are natural and necessary in any exploration. It suggests that we stop lamenting “the study didn’t work” but rather say “the study results were different and I’m going to see if I can tell why.”
Replications That Build Knowledge
By prioritizing conceptual reasoning, we accept the hard work of looking at the details of what is happening in any given study, but we also take the pressure off in different ways. Rebecca Ratner notes that “the review process exacerbates the file-drawer problem because researchers hear, ‘Don't include Study X because its findings aren't consistent and it complicates the story.’” And, while a focus on conceptual reasoning increases the difficulty in conducting and reporting replications (as we must consider whether a true conceptual replication is taking place rather than just copying stimuli), it takes the pressure off by reducing knee-jerk rejections of past work. Analyses over time allow for more data and therefore better understanding. This point echoes in our field; Sawyer and Peter (1983) wrote about the significance of significance, reminding us that using p < .05 as a certain and forever way of falsifying hypotheses is a false hope. They write, “Attention should be placed on the data themselves and their descriptions. Instead of relying solely on classical inferential statistics, researchers should make added use of replication, Bayesian statistics, meta-analysis, and strong inference to provide more meaningful examination of theoretical questions in marketing research.” This perspective is increasingly discussed in marketing ( McShane et al. 2024 ) and dominates other fields like biomedical research ( Savitz et al. 2024 ), where more studies of all sorts are simply ways to increase estimation accuracy. Ultimately, prioritizing conceptual validity is both harder and easier—it is harder to do, but easier to live with.
This echoes themes from two papers in the special issue. Eisend et al. (2024) contend that consumer research, as a distinct domain, demonstrates strong knowledge-building and is on an upward trajectory of increasingly distinct and robust effects, largely due to improvements in experimental methods and analysis. And, in moving forward, Urminsky and Dietvorst (2024) address estimation accuracy and the variability commonly observed in consumer research. They describe four types of replications that, when put into regular practice, can benefit researchers and knowledge-building.
New Populations, Methods, and Analyses
When asked what new methods and analyses are on the horizon, our experts had different perspectives. While Craig Thompson said, “new methods certainly arise over time in response to technological shifts—netnographies or more sophisticated QDA packages—but the foundational principles of anthropological, historical, and sociological analyses have remained fairly stable,” in contrast, Leigh McAlister enthused that the internet made so many more types and sources of data available and “new software fast followed” to allow better analysis of it. John Lynch and Rebecca Ratner saw some changes in field and lab studies but allowed they “weren’t that futuristic.” What then can we expect to see?
One overarching similarity our experts raised is a growing disillusionment with convenience samples, arguing that increased access to specific consumer populations suggests we should take greater care with how and where we recruit participants. There are two ways to increase the value of our participant groups; focus more tightly on the group of consumers who best illustrate our research question or cast a very wide net that captures consumer groups one would expect could differ. These strategies suggest different plans for analysis, but both serve to increase the reader’s confidence in the implications of the results. As Lynch (in a 1982 paper on external validity) argues, we don’t aim to “achieve” external validity, but rather to “assess” it by testing for background factor × treatment interactions and, for this, variation on background factors is needed.
Additionally, an increasingly networked and communication-enabled world means that we can share our findings with our participant populations and let them “speak back to the data.” Looking at JCR ’s first articles, while samples were often restricted to a convenience locale (e.g., a population of schoolboys in one town; Illinois newlyweds), they showed a depth of interaction (e.g., four interviews with each schoolboy; two surveys of the newlyweds spaced a year apart) which allowed for more of the participant’s input and interpretation to influence the researcher. That is the paradox of the new world of globally accessible data—we can use the internet to engage with a greater diversity of people, but we must be careful to not engage at the most distant or sterile remove.
If we can reach more or different people to be participants in our studies, we can also access and observe an expanded set of consumer behaviors. For example, we can study how people feel and think by looking at the language they use in public spaces; several of the experts saw textual analysis as a fast-growing and exciting research capability. We can track physiological measures to supplement or substitute for self-reports of affective and cognitive states; some experts saw the ability to better integrate physiological measures like eye-tracking or hormonal assays as a way to build new bridges between choice research and medical research. Online retail offers scope for large-scale field studies. Online choice contexts offer far more with attentional measures, process tracking, identity motivations, and following individuals across multiple platforms over time. The growth of large-scale databases (in both corporate and public policy sectors) over the last decade or two creates a promising opportunity to conduct longitudinal research without waiting years in primary research collection. A new methodological skill for the modern consumer researcher, then, is to become a better self-marketer, translator, and negotiator to those corporations and public organizations so that one is given access to existing longitudinal data. In university contexts, often the access to special populations or data is through grants and cooperative research projects that are common in other fields, but new to many in consumer research where we have long enjoyed the ability to do relatively inexpensive research under our own steam, oversight, and funding. Now, the modern consumer researcher will need methodological skills that improve interdisciplinary connections and serve to make them valued partners on multi-college grants.
Translation, Integration, and Intervention
Another new skill that consumer researchers are likely to need in the next 50 years in JCR is the ability to develop practical interfaces between real consumers/marketers and the knowledge we create. Our “job” in any one publication is to build knowledge, but there are many business school stakeholders (e.g., corporate and nonprofit partners, donors, students, administrators, society at large) who want more for their money; more so than in the past, academics are asked to take their ideas from the “bench” all the way to use. For example, the Journal of Marketing has a special issue that requires the inclusion of a web app designed for public use to help real-world marketers or consumers. This requires the ability to envision and design use-applications, but also to iterate more with practitioners to make sure our help really helps. Will this then lead to a research genre in consumer behavior akin to randomized clinical trial intervention studies? Either way, the ability to provide effective help relies on the rich breadth of knowledge advocated by our experts. As our experts agreed, if you do not know enough about the context of the domain, then you cannot understand whether any one consumer choice or behavior matters in the larger scheme. As with investigations of environmental sustainability, do our results show how shaping consumer choice is important, or rather that any attempt to ideally shape consumer choice is “a drop in the ocean”? When we try to create the intervention, we see how the importance of individual versus structural changes can shift with the cost/effort of the intervention and have a better appreciation for the constraints of the marketer acting in the real world.
Where Is Artificial Intelligence?
Artificial intelligence (AI) is a frequent topic in future-oriented discussions of business and business research. But, perhaps surprisingly, it did not emerge as a leading topic in these interviews. There is increasing research on the use of AI in the marketplace, such as consumer resistance ( Longoni, Bonezzi, and Morewedge 2019 ), but our editorial team believes that we should begin talking more comprehensively about where AI will potentially be in common use by researchers. We can see its use in background research and literature reviews. We can see its use in writing and content creation such as surveys, stimuli, and manuscripts. We can see its use in data collection, data generation, and data analysis. We can even see its use in review and publication. This expansive scope of possibilities and an uncertain timeline may be exactly why many experts are not quick to offer strong predictions, either descriptively or prescriptively. As a field, we should carefully consider a futurecast of AI in research systems and call for more editorial thinking on these issues.
Confidence versus Integrity
One thing that captures attention in the changing world of research is the issue of data integrity. JCR , like many journals, sought to increase the transparency and accountability of research published in the journal by requiring datasets be provided and open to the review team. Readers can see the current policies at https://consumerresearcher.com/research-ethics . But, though any given set of policies may evolve, our experts focused on the two key issues: integrity and confidence. In this distinction, integrity is the table-stakes of research. When a researcher’s integrity is in question, no methodology they offer will matter. This is because there are so many places where consumer research methodologies are vulnerable to bad actors. Where data can be made up or manipulated. Where studies can be analyzed and then hidden in file drawers. Where interviewees can be led. Where meanings can be misinterpreted. Where p s can be hacked. Where outliers can be cleaned from the dataset. Where hands can be waved over problematic inconsistencies. Where best practices change with new abilities. Because most of these vulnerabilities are hard to protect and harder to police, we rely necessarily on the integrity of the researcher—the core belief that the researcher is providing the most unbiased and truthful test of their research question even if that means disproving their theories or having to give up on their idea. In other words, integrity in research is the researcher’s true curiosity about the answer to their research question, convenient or inconvenient to their own ends, and their striving to do all in their abilities to provide that answer.
Confidence is a function of persuasion, as the authors attempt to make a compelling argument for the evidence presented. How confident are we, as readers, that the supporting evidence is strong and accurately interpreted? This is a high hurdle and assumes that the author is acting with integrity. If the researcher is sincere and acts with integrity, we as readers now assess whether the researcher has done a good job. For example, is the focal construct distinct from other related constructs? How has the constructed been measured? How has it been manipulated? Did the instructions prompt participants in a certain direction? Were the authors careful to create clear tests, realistic stimuli, and unbiased contexts? Were the authors careful to shape interview scripts in a way that minimized interviewer influence or social desirability? Were research populations the most relevant for the research question or were they convenience populations? What analyses were used to shape interpretation of the data and were they the most appropriate or up to date?
Thus, there are many ways that a researcher can make their empirical evidence instill confidence through thoughtful design and testing. Other means are emerging. For example, some scholars appreciate preregistration as a means to discourage questionable research practices in overfitting data—something that can give readers confidence in the analysis of the researchers. However, other scholars see preregistration as a practice privileged to researchers with the budget to conduct multiple studies or as performative virtue-signaling. Because of this debate perhaps, preregistration has not been shown to increase trust in findings ( Field et al. 2020 ). In the end, there are many aspects of consumer research analysis (no matter the specific methodology) that are not wrong but still fail to instill confidence in the reader. To this end, JCR has often published work that sets a standard, especially in new or evolving areas, for what constitutes excellent evidence in a methodological domain and these types of papers will continue to be important to our field.
A 50-year retrospective provides a trajectory that we can follow in imagining future changes in methodology. New methodologies may emerge with novel technological capabilities, but their adoption is a function of whether they better answer the questions we are currently asking about consumers. One of the best things we can do for our methodological success is to be more critical in defining our research questions—a skill that requires honing across one’s career. We are well-served by framing different questions for our program of research (pushing ourselves to embrace the rich breadth of a domain) versus a research project (pushing ourselves to focus on one important and answerable question). Next, our work profits by critically considering our construct definition (and operationalization)—this is critical, as poor construct validity cannot be overcome with novel sophisticated analyses. The good news of greater effort in conceptual clarity is that it helps take pressure off any one study and guides replication efforts to focus on increasing estimation accuracy rather than disproving famous effects. There are new types of data to explore (textual, physiological, digital), and best practices will continue to evolve—most conclusively with methodological papers published to propose and teach emerging norms. Importantly, there are new populations of consumers to study and many new means to reach them in a meaningful way. Our methods may shift in our need to be better translators of the behaviors we observe and better able to view those behaviors within the wider systematic context, where practitioners seek to solve big problems and make significant changes to consumer behaviors. Our methods may need to mimic other prescriptive sciences (e.g., public health, medicine, environmental science) if we seek to provide solutions. We must embrace our own integrity and avoid a cynical attitude toward research and the review process. JCR —as an arbiter of integrity—walks the narrow path that protects both the accuser and the accused when breaches of integrity are suspected. Ultimately, however, the larger threat to consumer research is when we fail to have confidence in the empirical support for a project because of vague, convenient, superficial, sloppy, or out-of-date practices in data collection and analysis. In the end, our methodologies lie within a scholarly toolbox that also contains our curiosity, motivation, critical thinking, integrity, and openness.
Stacy Wood ( [email protected] ) is the J. Lloyd Langdon Distinguished University Professor of Marketing at the Poole College of Management, North Carolina State University, Raleigh, NC, USA.
The author thanks the panel of esteemed consumer scholars—John Lynch, Leigh McAlister, Rebecca Ratner, and Craig Thompson—who shared their experiences, expertise, and love of research in deep and wide-ranging conversations. It is hoped that readers of this article benefit from their insights as much as the author who had the privilege of hearing them firsthand.
Eisend Martin , Pol Gratiana , Niewiadomska Dominika , Riley Joseph , Wedgeworth Rick ( 2024 ), “ How Much Have We Learned about Consumer Research? A Meta-Meta-Analysis ,” Journal of Consumer Research , 51 ( 1 ), forthcoming.
Google Scholar
Field Sarahane M. , Wagenmakers E. J. , Kiers H. A. L. , Hoekstra R. , Ernst A. F. , van Ravenzwaaij D. ( 2020 ), “ The Effect of Preregistration on Trust in Empirical Research Findings: Results of a Registered Report ,” Royal Society Open Science , 7 ( 4 ), 181351 .
Katona George ( 1974 ), “ Psychology and Consumer Economics ,” Journal of Consumer Research , 1 ( 1 ), 1 – 8 .
Lehmann Donald R. , McAlister Leigh , Staelin Richard ( 2011 ), “ Sophistication in Research in Marketing ,” Journal of Marketing , 75 ( 4 ), 155 – 65 .
Longoni Chiara , Bonezzi Andrea , Morewedge Carey K. ( 2019 ), “ Resistance to Medical Artificial Intelligence ,” Journal of Consumer Research , 46 ( 4 ), 629 – 50 .
Lynch John G. ( 1982 ), “ On the External Validity of Experiments in Consumer Research ,” Journal of Consumer Research , 9 (3), 225 – 39 . https://doi.org/10.1086/208919
MacKenzie Scott B. ( 2003 ), “ The Dangers of Poor Construct Conceptualization ,” Journal of the Academy of Marketing Science , 31 ( 3 ), 323 – 6 .
McShane Blake B. , Bradlow Eric T. , Lynch John G. , Meyer Robert J. ( 2024 ), “ “Statistical Significance” and Statistical Reporting: Moving beyond Binary ,” Journal of Marketing . https://doi.org/10.1177/00222429231216910
Pham Michel Tuan , Wu Alisa Yinghao , Wang Danqi ( 2024 ), “ Benchmarking Scholarship in Consumer Research: The p-Index of Thought Leadership ,” Journal of Consumer Research , 51 ( 1 ), forthcoming.
Savitz David A. , Wise Lauren A. , Bond Julia C. , Hatch Elizabeth E. , Ncube Collette N. , Wesselink Amelia K. , Willis Mary D. , Yland Jennifer J. , Rothman Kenneth J. ( 2024 ), “ Responding to Reviewers and Editors about Statistical Significance Testing ,” Annals of Internal Medicine , 177 ( 3 ), 385 – 6 . https://doi.org/ 10.7326/M23-2430
Sawyer Alan G. , Peter J. Paul ( 1983 ), “ The Significance of Statistical Significance Tests in Marketing Research ,” Journal of Marketing Research , 20 ( 2 ), 122 – 33 .
Urminsky Oleg , Dietvorst Berkeley J. ( 2024 ), “ Taking the Full Measure: Integrating Replication into Research Practice to Assess Generalizability ,” Journal of Consumer Research , 51 ( 1 ), forthcoming.
Wang Xin (Shane) , Hyun (Joseph) Ryoo Jun , Campbell Margaret C. , Inman J. Jeffrey ( 2024 ), “ Unraveling Impact: Exploring Effects of Novelty in Top Consumer Research Journals ,” Journal of Consumer Research , 51 ( 1 ), forthcoming.
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1537-5277
- Print ISSN 0093-5301
- Copyright © 2024 Journal of Consumer Research Inc.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Skip to main content
- Skip to primary sidebar
- Skip to footer
- QuestionPro

- Solutions Industries Gaming Automotive Sports and events Education Government Travel & Hospitality Financial Services Healthcare Cannabis Technology Use Case NPS+ Communities Audience Contactless surveys Mobile LivePolls Member Experience GDPR Positive People Science 360 Feedback Surveys
- Resources Blog eBooks Survey Templates Case Studies Training Help center
Home Surveys Academic Research
Retrospective Study: What it is & How to Do it

In a retrospective study , existing data are examined to identify risk factors for particular diseases. Interpretations are limited as it is impossible to go back in time and gather the missing information. Let’s talk about that.
What is a Retrospective Study?
A retrospective study is an analysis that compares two groups of individuals. A case group and a control group. Both groups are similar, but the case group has a key factor that is being studied or investigated that the control group does not.
It brings up key differences in individuals or groups of individuals based on some events/incidences. It’s a psychological approach to pinpoint key differences in individuals that are alike but differ slightly based on certain characteristics.
What is the importance of a Retrospective Study?
This study is greatly important in many aspects, be it personal development, socio-economic welfare, or professional development.
This study is also important to fixate certain characteristics within individuals by considering historical data and making rational decisions. In large organizations, this becomes very important because organizations deal with large groups of clients with almost (but not completely) alike behaviors.
This is the stage where retrospection comes into play to understand differences and similarities among clients and act accordingly.
Advantages and disadvantages of a Retrospective Study
Similar to other studies, there are benefits and drawbacks to retrospective studies. Researchers must critically evaluate the method that is used and carefully interpret the results of retrospective studies before putting them to practice.
Advantages:
- Researches have control of the number of participants in the case group and control group.
- Typically less expensive to conduct in comparison to other methods.
- Timeline of a retrospective study is quicker to complete
Disadvantages:
- Poor control over exposure factor
- If research is not thorough, there could be missing history/background and or information.
- If researchers are not careful, selection and recall bias can affect the results
How to conduct a Retrospective Study
There are certain ways to conduct a retrospective study. Most of them collect vast historical data and make sense of it statistically. Another way is by considering 2 groups with similar attributes and then conducting Surveys (That’s where QuestionPro shines!) to find out differing characteristics. In general, there are 2 parts to it:
Prospective Study
Retrospective study.
For the sake of this article, let’s just stick to the retrospective study. An organization can take many surveys and collect data from them. This data can then be processed to make important business decisions. This will help the organization understand its clients and help provide more viable products and services that would actually make a difference.
Retrospective Study Examples
These studies aim to study a situation, condition, event, or phenomenon that has already happened. This study is often used in the medical industry to study different medical conditions and illnesses. Using participants who have an existing condition compared to a group that does not have that particular condition.
Conclusion:
In conclusion, this study deals with enhancing minor differences amongst similar groups. These differences are brought up by studying and statistically sourcing historical data collected by various means. One such method to collect data and perform this study is by taking surveys.
QuestionPro has a rich arsenal of tools and products to bring the most out of such studies. These tools collect useful insights and help in procuring pinpoint differences within the most similar groups of individuals and further accelerating the study.
CREATE FREE ACCOUNT
Authors : Siddharth Kulkarni & Jenny Huang
MORE LIKE THIS
Data Information vs Insight: Essential differences
May 14, 2024
Pricing Analytics Software: Optimize Your Pricing Strategy
May 13, 2024

Relationship Marketing: What It Is, Examples & Top 7 Benefits
May 8, 2024
The Best Email Survey Tool to Boost Your Feedback Game
May 7, 2024
Other categories
- Academic Research
- Artificial Intelligence
- Assessments
- Brand Awareness
- Case Studies
- Communities
- Consumer Insights
- Customer effort score
- Customer Engagement
- Customer Experience
- Customer Loyalty
- Customer Research
- Customer Satisfaction
- Employee Benefits
- Employee Engagement
- Employee Retention
- Friday Five
- General Data Protection Regulation
- Insights Hub
- Life@QuestionPro
- Market Research
- Mobile diaries
- Mobile Surveys
- New Features
- Online Communities
- Question Types
- Questionnaire
- QuestionPro Products
- Release Notes
- Research Tools and Apps
- Revenue at Risk
- Survey Templates
- Training Tips
- Uncategorized
- Video Learning Series
- What’s Coming Up
- Workforce Intelligence
Asia & Oceania
Middle east & africa.
- United States
- Asia Pacific
- Australia & NZ
- Southeast Asia
- Czech Republic
- Deutschland
- España
- Switzerland
- United Kingdom

EMEA Thought Leadership
Developing IQVIA’s positions on key trends in the pharma and life sciences industries, with a focus on EMEA.
- Middle East and Africa
Life Sciences Solutions
Healthcare solutions.
- Medical Device and Diagnostic
- U.S. Government
Bringing together unparalleled healthcare data, advanced analytics, innovative technologies, and healthcare expertise to create intelligent connections that speed the development and commercialization of innovative medicines to improve patient lives.
- Commercial Solutions
- Contract Sales and Medical Solutions
- Financial Services
- Information Solutions
- Medical Affairs
- Real World Evidence
Accelerate digital innovation to enable smarter decisions that reduce cost, modernize patient and consumer engagement, and improve health outcomes.
- Health Plans
- Hospitals and Health Systems
- Insurers and Risk
- Medical Specialty Societies
- Patient Advocacy Organizations

Medical Device and Diagnostic Solutions
Your world is unique – and quite different from pharma. In the U.S., decision-making has shifted from individual physicians to integrated networks--GPOs, IDNs and payers. These groups have heightened the focus on proving your solution’s value, demanding outcomes analyses and putting pressure on pricing.
- Hospital Procedures and Diagnosis
- Medical Device Supply Audit
- MedTech Business Insights and Trends Podcast Series
U.S. Government Solutions
For government agencies and organizations at every level—from federal or national to regional and local—Big Data can have a huge impact on public health.
U.S. PROGRESS POINT
A curation of IQVIA's best thinking on topics and trends driving change, disruption, and progress in the United States healthcare market.
Get the latest insights on our life sciences, healthcare, and medical technology solutions in the United States. Follow our blog today!

U.S. INSIGHTS LIBRARY
"Browse our library of insights and thought leadership.
ON-DEMAND WEBINARS
Visit our library of on-demand webinars.
UPCOMING EVENTS & WEBINARS
View our upcoming events and webinars.

FEATURED WEBINAR
"Top Issues for Pharma to Watch in 2022 and 2023
Get instant access
You may also be interested in.
For this browsing session please remember my choice and don't ask again.
- Biostatistics
- Data Science
- Programming
- Social Science
- Certificates
- Undergraduate
- For Businesses
- FAQs and Knowledge Base
- Test Yourself
- Instructors
Prospective vs. Retrospective
A prospective study is one that identifies a scientific (usually medical) problem to be studied, specifies a study design protocol (e.g. what you’re measuring, who you’re measuring, how many subjects, etc.), and then gathers data in the future in accordance with the design. The definition of the problem under study does not change once the data collection starts.
A retrospective study is one in which you look backwards at data that have already been collected or generated, to answer a scientific (usually medical) problem.
Prospective studies are generally regarded as cleaner and more reliable, due to several shortcomings of retrospective studies:
- Since the data are already available, the question to be answered can be influenced by the data
- Similarly, the exact data (or subset of data) used to answer the question can be drawn in a way that produces the desired answer, or a more noteworthy or interesting answer
- There is a temptation to modify the question being studied as the data are examined
Some prospective studies have retrospective aspects. Cohort and panel studies, which often follow a group over time, often collect information about the past. For example, participants may be asked if they had any medical conditions as a child, e.g. exposure to severe sunburn. However, in such cases, there is also an aspect of tracking events into the future.
A good example is a study following cigarette smokers over time, to see what medical conditions they contract during the study. This information would typically be compared to similar information from non-smokers. Although prior information from the participants might be used, the primary focus is what happens to each group during the period of the study. Sometimes called a “prospective cohort study,” these studies often fall short of the “gold standard” of a randomized trial, because the assignment to the treatment or control group is usually not random. One could not assign a person randomly to be a lifetime cigarette smoker or non-smoker. However, the outcome of interest (e.g. lung cancer) is something that develops or becomes apparent during the course of the study. Nobody is being selected on that basis, so the opportunity for selection bias is limited.
Another type of study is fully retrospective: the groups are selected on the basis of the outcome of interest. For example, one might look at a group of lung cancer patients and compare them to a group of patients without lung cancer to examine the prevalence of smoking in each group. The conclusions from such a study may not be as solid as those from prospective studies. You can demonstrate correlation, but external factors and aspects outside the scope of the study have a greater opportunity to creep in and bias the results (see selection bias ) than with a prospective study where you identify groups beforehand and then observe what happens to them. In addition to bias, there can be problems with data quality. Some records may be missing. Subjects’ recall may be faulty. Plus, you don’t have the opportunity to collect data tailored to the needs of the study that you would with a prospective study. It may, as a result, be more difficult to make the leap from correlation to causation with a retrospective study than a prospective study.
The long process of proving a relationship between cigarette smoking and lung cancer is a good case study. Rates of smoking increased dramatically in the U.S. in the 1940’s and 1950’s, as cigarettes became more widely available and advertising glamorized their use. The incidence of lung cancer (which had been at relatively low rates prior to the wars) also increased. However, strong evidence of a link between the two was lacking.
This began to change in the 1950s. Five larger retrospective studies were published in the early 1950’s that again showed a link between cigarette smoking and lung cancer. Though important, these studies still didn’t make a convincing enough case as they relied on the self-reported smoking habits of people who already had lung cancer, and compared them to those who didn’t. One potential problem with this type of study is that people with lung cancer are more likely to overestimate how much they smoked, while those who don’t have lung cancer are more likely to underestimate how much they smoked.
To address this issue, a prospective (cohort) study was needed – recruiting healthy people and following them over time to see who develops or dies from lung cancer and who does not. Without such evidence, the tobacco industry was able to cast doubt on the link between smoking and death from lung cancer and other diseases, says Eric Jacobs, Ph.D., an epidemiologist at the American Cancer Society.
It was not until 1952 that Cuyler Hammond and Daniel Horn organized a prospective study with 22,000 volunteers that solid evidence of the link between cancer and smoking was established. Ironically, in a photo of the two researchers presenting their results at a meeting of the 1954 American Medical Association, they are both shown smoking pipes!
You can learn more about different study designs in these Statistics.com courses:
- Designing Valid Statistical Studies : Learn about different study designs (randomized trial, observational study, case-control), and sources of bias
- Epidemiologic Statistics : Learn about disease metrics (risk, morbidity, prevalence, …) and statistical approaches to measurement
- Introduction to Statistical Issues in Clinical Trials : Learn about randomized clinical trials (RCTs), principles of design, including power, and statistical approaches for different study metrics (also called endpoints)
- Introduction to Statistics : Learn the basic concepts of inference (p-values, confidence intervals)
Read more about the smoking studies in Elizabeth Mendes’ report at the American Cancer Society ( https://www.cancer.org/latest-news/the-study-that-helped-spur-the-us-stop-smoking-movement.html ).
- Open access
- Published: 12 May 2024
The impact of inhalation injury on fluid resuscitation in major burn patients: a 10-year multicenter retrospective study
- Shuao Xiao 1 na1 ,
- Zeping Pan 2 na1 ,
- Hang Li 1 ,
- Yuheng Zhang 3 ,
- Tian Li 4 ,
- Hao Zhang 2 &
- Jinbin Ning 1
European Journal of Medical Research volume 29 , Article number: 283 ( 2024 ) Cite this article
63 Accesses
Metrics details
It remains unclear whether additional fluid supplementation is necessary during the acute resuscitation period for patients with combined inhalational injury (INHI) under the guidance of the Third Military Medical University (TMMU) protocol.
A 10-year multicenter, retrospective cohort study, involved patients with burns ≥ 50% total burn surface area (TBSA) was conducted. The effect of INHI, INHI severity, and tracheotomy on the fluid management in burn patients was assessed. Cumulative fluid administration, cumulative urine output, and cumulative fluid retention within 72 h were collected and systematically analyzed.
A total of 108 patients were included in the analysis, 85 with concomitant INHI and 23 with thermal burn alone. There was no significant difference in total fluid administration during the 72-h post-burn between the INHI and non-INHI groups. Although no difference in the urine output and fluid retention was shown in the first 24 h, the INHI group had a significantly lower cumulative urine output and a higher cumulative fluid retention in the 48-h and 72-h post-burn (all p < 0.05). In addition, patients with severe INHI exhibited a significantly elevated incidence of complications (Pneumonia, 47.0% vs. 11.8%, p = 0.012), (AKI, 23.5% vs. 2.9%, p = 0.037). For patients with combined INHI, neither the severity of INHI nor the presence of a tracheotomy had any significant influence on fluid management during the acute resuscitation period.
Conclusions
Additional fluid administration may be unnecessary in major burn patients with INHI under the guidance of the TMMU protocol.
Introduction
Inhalation injury (INHI) refers to damage to the respiratory tract caused by inhaling hot air, smoke, toxic gases, steam, combustible vapors, or particles in the mouth, nose, throat, and trachea [ 1 ]. Approximately 10–20% of burn patients also suffer from INHI, which has been identified as an independent predictor of mortality in most epidemiological surveys of burn injuries [ 2 , 3 ]. Shock is the leading cause of death during the acute resuscitation period, with most deaths occurring within the first 72 h after injury [ 4 ]. Therefore, prompt and effective fluid resuscitation is of paramount importance in managing shock and improving patient outcomes. While poor administration of resuscitation fluid can lead to adverse clinical outcomes, excessive fluid volumes are associated with an increased risk of morbidity and life-threatening complications [ 5 ].
Despite the use of various fluid resuscitation methods, such as the Parkland, Evans, and Brook formulas, there is no international consensus on fluid resuscitation protocols in burn care. This has resulted in considerable variation in fluid management practices across different regions and burn center guidelines. In China, the Third Military Medical University (TMMU) formula has gained widespread acceptance for fluid resuscitation during the early phase of severe burn treatment [ 6 ]. Notably, the TMMU protocol differs from other fluid resuscitation protocols primarily in its early use of colloids [ 7 ]. However, limited research has been conducted on the effects of INHI on fluid resuscitation during the shock phase under the guidance of the TMMU protocol.
Debates have been ongoing for decades regarding whether burn patients with combined INHI should receive more fluid resuscitation than those with similar thermal injuries but no respiratory tract involvement. The inclusion criteria for %TBSA have varied widely in previous studies, and the lack of a unified criterion for %TBSA inclusion may be one reason for the differing conclusions reached. Furthermore, patients with smaller burn areas may have the ability to maintain fluid balance and normal tissue perfusion through compensatory mechanisms, potentially leading to higher tolerance for insufficient or excessive fluid replacement, which makes it difficult to assess the impact of INHI on fluid resuscitation needs. It is, therefore, imperative to investigate whether the presence of INHI results in additional fluid resuscitation requirements in burn patients with larger %TBSA. In addition, the severity of INHI and whether a tracheostomy was performed may also affect fluid resuscitation volume during the shock phase [ 8 , 9 ].
Thus, we aimed to investigate the influence of INHI, INHI severity, and tracheotomy on the fluid management during acute resuscitation phase in burn patients with TBSA ≥ 50% guided by the TMMU protocol.
Study population
We conducted a multicenter retrospective study, selecting four tertiary hospitals in the northwest of China: Second Affiliated Hospital of Air Force Medical University, Shaanxi Provincial People's Hospital, Xi'an Central Hospital, and Yan’an University First Affiliated Hospital. We enrolled patients who suffered from severe thermal injury between May 2009 and December 2019 and met the following inclusion criteria (Fig. 1 ): %TBSA burned of ≥ 50%; age ≥ 18 years; complete data; the time between thermal injury and fluid therapy was less than 4 h; and arrival at the BICU less than 6-h post-burn. Patients were excluded if they met any of the following criteria: electrical burns; pre-existing hepatic, respiratory, cardiac, neural or renal dysfunction, pre-existing coagulopathy, or those requiring compassionate care only; patients who died upon admission or refused any treatment.
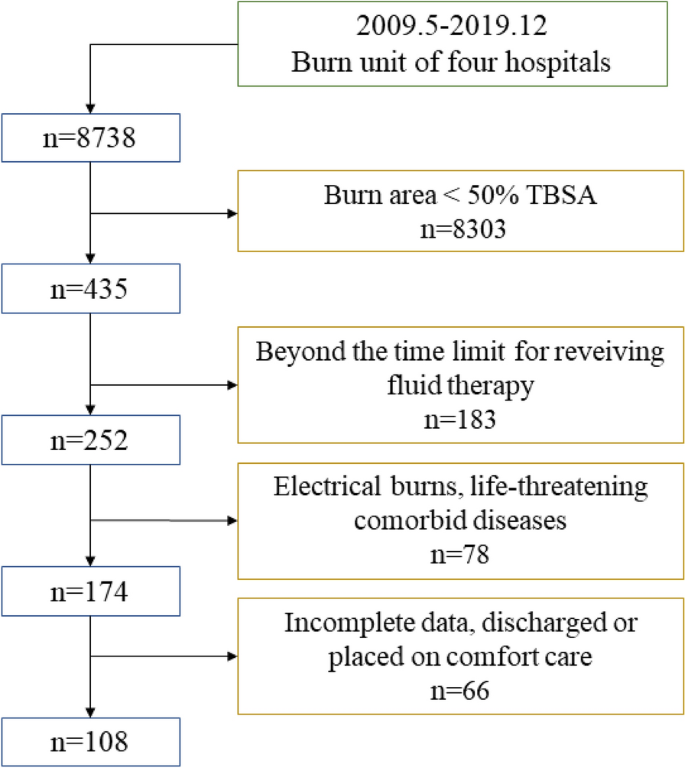
Flow chart of this study
Upon admission, patients were routinely given high-concentration oxygen therapy or high-flow nasal oxygen therapy. Mechanical ventilation was initiated under the following conditions: continued deterioration despite active treatment; disorders of consciousness; severe abnormal breathing patterns, such as a respiratory rate > 35–40 times/min or < 6–8 times/min, irregular rhythm, weak or absent spontaneous breathing; blood gas analysis indicating severe impairment of ventilation and oxygenation: PaO 2 < 50mmHg; progressive increase in PaCO 2 , dynamic decrease in pH. Patients without INHI were assisted with endotracheal intubation for ventilation, while those with INHI underwent tracheostomy for mechanical ventilation [ 10 ]. The initial mode of mechanical ventilation for major burn patients was synchronized intermittent mandatory ventilation (SIMV). The level of inspired oxygen was adjusted to maintain the patient's pulse oxygen saturation at 90–95% and PaO 2 at 60–80 mmHg or above. For early treatment of patients with extensive burns, broad-spectrum antibiotics should be administered to prevent infection, enteral nutrition support should be initiated as early as possible, and airway lavage should be performed to remove harmful substances in cases of INHI. Early surgical intervention included prompt debridement, removal of necrotic tissue, and early extensive skin grafting to close the wound and reduce infection and fluid loss [ 10 ].
Data sources
We retrospectively aggregated data from the electronic medical record system, categorizing it into demographics, clinical outcomes, and resuscitation-assessment parameters. Demographic information included gender, age, weight, %TBSA, %full-thickness burn, INHI grade, and mortality. Bronchoscopy was utilized to ascertain the diagnosis of INHI. Microscopic signs of airway congestion, edema, soot deposition, and mucosal sloughing were compelling evidence for the diagnosis of inhalation injury [ 11 ]. The degree of INHI was established from initial bronchoscopy findings, according to the Abbreviated Injury Score criteria [ 12 ]. The representative photographs of patients with extensive burns and endoscopic images illustrating the degree of inhalation injury were shown in Fig. 2 . We also recorded the occurrence of tracheotomy within 24 h of admission. Clinical outcomes within 72 h of admission included the occurrence rates of pneumonia, acute respiratory distress syndrome (ARDS), acute kidney injury (AKI), and sepsis. Pneumonia was defined as a positive bronchoalveolar lavage (BAL) with > 100,000 colony forming units and clinical suspicion of pneumonia. The incidence of acute respiratory distress syndrome (ARDS) was defined according to the Berlin definition [ 13 ]. The incidence of acute kidney injury (AKI) was assessed according to AKIN definition [ 14 ]. Sepsis was diagnosed when hemodynamic instability coincided with documented evidence of infection from blood, urine, BAL, or wound samples. Resuscitation-assessment parameters included the cumulative fluid administration volume (total of all fluids administered, orally and intravenously), the cumulative urine output volume, and the cumulative fluid retention volume during 24-, 48-, and 72-h post-burn. To calculate the fluid retention, the formula described by Boer et al. was applied: Cumulative fluid retention = (cumulative fluid administration volume–cumulative urine output volume)/weight /%TBSA, where weight refers to the weight prior to hospitalization [ 9 ].
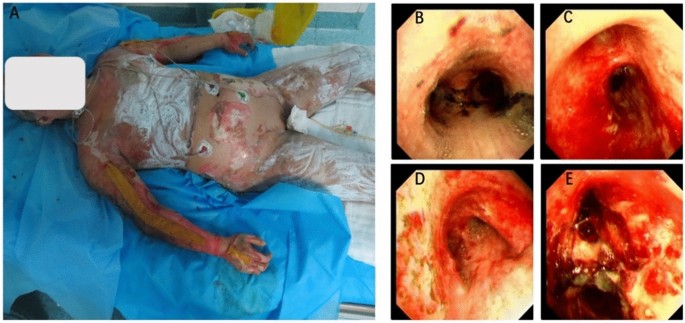
Representative photographs of patients with extensive burns and endoscopic images illustrating the degree of inhalation injury. A Patient with extensive burns; B Grade 1; C Grade 2; D Grade 3; E Grade 4
TMMU fluid resuscitation
Patients in this study were given fluid resuscitation therapy based on the established TMMU protocol [ 6 ]. The initial fluid requirements were calculated as 1.5 ml/kg/% TBSA + 2000 ml for the first 24 h and 0.75 ml/kg/% TBSA + 2000 ml for the second 24-h post-burn. Lactated Ringer’s solution was used as a crystalloid, and the frozen plasma or 5% albumin solution was given as a colloid. The ratio of colloid to crystal volumes was expected to be 1:2. An additional 2000 ml of 5% glucose solution was administered daily to meet the patient's physical demand for water. One-half of the calculated crystalloid solution and colloid should be administered within the first 8h post-burn, with the remainder given homogeneously over the next 16 h. Subsequently, fluid resuscitation was guided based on clinical parameters. The TMMU formula only provides an estimation of the required fluid volume for burn patients. The fluid resuscitation should be individualized based on the situation of patient, such as age, gender, burn depth, patient response, and overall condition. Specifically, the rate of fluid resuscitation should be adjusted according to a comprehensive assessment of the patient and monitoring of urine output, vital signs, mental status, and tissue perfusion [ 6 ].
Statistical analysis
Continuous variables are reported as means and standard deviations or medians and interquartile ranges, while dichotomous and categorical variables are presented as counts and relative percentages in each group. The student’s t test was used to analyze differences between groups with normally distributed data, while the Mann–Whitney U test was performed to analyze differences between groups with non-normally distributed data. Pearson’s Chi-squared test or Fisher’s exact test were also used to examine differences between categorical data, frequencies or rates. To adjust for intergroup difference (INHI vs. non-INHI; high-grade INHI vs. low-grade INHI), a case–control matching analysis was conducted using a one-to-two matching without replacement approach. Further analyses between groups were performed before and after matching. For all analyses, p < 0.05 was considered to suggest statistical significance. All procedures were conducted using SPSS (version 25.0; IBM, USA) and R software (version 3.6.1; R Foundation for Statistical Computing, Vienna, Austria).
Patient characteristics and outcomes when grouped by INHI
A total of 108 patients were enrolled in the study, with 85 patients having concomitant INHI and 23 patients having a thermal burn alone. The cohort was predominantly male (82.4%) with a mean age of 40.6 ± 11.6, a mean weight of 67.3 ± 10.4, and a median %TBSA of 70 (55–84.5). Of these 85 patients with INHI, 24 patients had grade 1 injury, 38 patients had grade 2 injury, 20 patients had grade 3 injury, and 3 patients had grade 4 injury. To evaluate the effect of INHI on fluid resuscitation in severe burn patients, we first classified patients into INHI and non-INHI groups. Patient characteristics by group are reported in Table 1 . There were no significant differences in gender, age, weight, or mortality between the two groups. However, the %TBSA in the INHI group was significantly larger than that in the non-INHI group (71.2% vs. 61.3%, p = 0.008). In addition, %full-thickness burn was also found larger in the INHI group, but without reaching statistical significance (37.8% vs. 27.5%, p = 0.080). To adjust for intergroup differences, we conducted a case–control matching analysis performing one-to-two matching (non-INHI group to INHI group) without replacement in terms of gender, age, weight, %TBSA and %full-thickness burn. After matching, 20 patients of the non-INHI group and 40 patients of the INHI group were identified, and no significant difference in demographic variables was demonstrated (Table 1 ). Regarding morbidity, the incidence of pneumonia was significantly higher in the INHI group before and after matching (24.7% vs. 4.3%, p = 0.039; 27.5% vs. 5.0%, p = 0.047), whereas no difference was found in the incidence of ARDS, AKI and sepsis.
Patient resuscitation-assessment parameters when grouped by INHI
There was no significant difference between the two groups in total fluid administration during the 72-h post-burn period. Although no difference in the urine output and fluid retention was observed in the first 24 h, the INHI group had a significantly lower cumulative urine output and a higher cumulative fluid retention in the 48-h and 72-h post-burn after matching, when compared to the non-INHI group (all p < 0.05) (Table 2 ).
Patient characteristics and outcomes when grouped by INHI severity
To assess the impact of INHI severity on fluid administration requirements, we further categorized patients with concomitant INHI ( n = 85) into low-grade (grades 1 and 2) ( n = 62) and high-grade (grades 3 and 4) ( n = 23) groups. As shown in Table 3 , the high-grade INHI group had a significantly larger burn surface area than those in the low-grade INHI group (%TBSA, 78.9% vs. 68.3%, p = 0.007), (%full-thickness burn, 53.5% vs. 32%, p = 0.001). To control for intergroup bias, we also performed a case–control matching analysis at a ratio of 1:2 based on clinical parameters. A total of 17 patients belonging to the high-grade INHI group and 34 patients belonging to the low-grade INHI group were identified. After matching, no significant difference in demographic variables was reported (Table 3 ). The high-grade INHI group showed a significantly elevated incidence of complications (Pneumonia, 47.0% vs. 11.8%, p = 0.012), (ARDS, 23.5% vs. 5.9%, p = 0.087), (AKI, 23.5% vs. 2.9%, p = 0.037).
Patient resuscitation-assessment parameters when grouped by INHI severity
As shown in Table 4 , there was no difference in fluid administration, urine output, or fluid retention during the 72-h post-burn between patients with low-grade and high-grade INHI, before and after matching (all p > 0.05).
INHI patient characteristics and outcomes when grouped by tracheotomy
Patients with combined INHI often require prophylactic tracheostomy to prevent airway obstruction. We sought to determine whether there was a difference in fluid management between the tracheostomy and non-tracheostomy groups, and 85 patients were subsequently divided into two groups: tracheostomy and non-tracheostomy. As presented in Table 5 , the tracheotomy group showed a larger %full-thickness burn than that in the non-tracheotomy group, but without reaching statistical difference (median 41 vs. 31.1, p = 0.104). The two groups did not differ in other variables and showed no difference in overall morbidity and mortality.
INHI patient resuscitation-assessment parameters when grouped by tracheotomy
There was no significant difference in cumulative fluid administration, urine output, or fluid retention between the two groups during the 72-h post-burn, between and after matching (all p > 0.05) (Table 6 ).
Main finding and interpretation
Severe burns are among the most critical injuries, and appropriate fluid resuscitation is critical in the early post-injury period. Under-resuscitation can lead to organ hypoperfusion, shock, and other hazards, but over-resuscitation can lead to the risk of serious complications, such as pneumonia, sepsis, and cardiopulmonary dysfunction [ 15 ]. Thus, investigating whether INHI increases the need for additional fluid resuscitation is of great significance for the management of major burn patients during the acute resuscitation phase. In this multicenter retrospective study, a total of 108 patients with %TBSA ≥ 50% were included in the analysis. We did not observe a significant increase in fluid resuscitation requirements in major burn patients with combined INHI. However, INHI may have an impact on fluid balance in major burn patients, as evidenced by lower cumulative urine output and higher cumulative fluid retention in the 48-h and 72-h post-burn in the INHI group. In addition, the severity of INHI and tracheotomy did not appear to have a significant impact on fluid management in patients with combined INHI.
Upon reviewing previous literature, we found that the inclusion criterion for %TBSA in related studies varied greatly, ranging from 0 to 30% [ 8 , 16 , 17 , 18 , 19 , 20 ]. Some studies even lacked clear inclusion criterion for %TBSA [ 12 ]. This may be one of the reasons for the different conclusions drawn by these studies. To better assess the impact of INHI on fluid resuscitation requirements, we set a relatively high inclusion criterion of 50% TBSA. The reasons were as follows: First, in our clinical practice, we have noticed that patients with minor burns are able to maintain fluid balance and normal tissue perfusion through compensatory mechanisms, which can confer greater tolerance to suboptimal fluid replacement. However, patients with %TBSA ≥ 50% are faced with a more severe state of shock, and fluid resuscitation becomes a critical and essential treatment measure. Second, for patients with %TBSA ≥ 50%, fluid resuscitation requirements for shock management need to be more precise and carefully regulated to avoid adverse outcomes resulting from under- or over-resuscitation. Investigating whether INHI increases fluid resuscitation needs is particularly relevant and clinically informative in the context of burn injuries of this severity, as it highlights the impact of INHI on fluid resuscitation requirements. Third, another major complication of excessive fluid resuscitation is compartment syndrome of the limbs or abdomen. Excessive fluid resuscitation in severe burn patients can cause massive edema in burned and unburned tissues, increasing the risk of abdominal hypertension and subsequent abdominal compartment syndrome. Markell et al. found that patients with %TBSA ≥ 50% combined with INHI are more likely to develop abdominal compartment syndrome [ 5 ]. Thus, in this study, we established a 50% TBSA inclusion criterion to ensure that we were capturing patients in the most critical and relevant cases for fluid resuscitation.
The demographic data showed that patients with combined INHI had significantly larger and deeper burns, consistent with previous literature reports [ 16 , 17 , 20 ]. As burns increase in size and depth, patients typically require more fluid, but the increase in fluid requirements is not entirely linear, and there is great individual variability [ 21 , 22 ]. To control for differences in burn area between groups, we used a case–control matching approach to assess the impact of INHI on fluid requirements in similar burn areas and depths. We found that patients in the combined INHI group did not require additional fluid resuscitation, even when subjects were divided into low-grade and high-grade groups. In addition, we observed that patients subjected to mechanical ventilation via tracheostomy exhibited a notable trend towards increased fluid retention, reaching near statistical significance by the third-day post-intervention. This phenomenon can be elucidated through several physiological mechanisms. First, the elevation in mean intrathoracic pressure associated with mechanical ventilation reduced venous return, leading to an increase in central venous pressure. Such changes imposed a greater afterload on the right ventricle, subsequently diminishing cardiac output and augmenting sympathetic nervous system activity [ 23 ]. Moreover, the application of positive pressure for lung expansion triggered an extensive endocrine response, characterized by elevated plasma levels of norepinephrine, increased renin activity, and a rise in atrial natriuretic peptide. These hormonal shifts contributed to heightened sympathetic tone, promoting renal retention of fluids [ 24 ]. Boer et al. reported that the increased fluid retention, traditionally linked with INHI, results from the effects of ventilation rather than from INHI itself [ 9 ].
Although there was no significant difference in fluid demand, we found that patients in the INHI group had significantly lower urine output and higher fluid retention. This indicates that although both groups of patients received the same amount of fluid resuscitation, the volume of fluid circulating in the INHI patients was significantly reduced. The physiological and pathological processes of INHI contributed to this finding. INHI is caused by direct local thermal injury and exposure to numerous toxic chemicals that can directly cause mucous shedding, bronchial edema, airway obstruction, hypoxia, and severe inflammatory reactions in the respiratory tract and even throughout the body [ 25 ]. These processes can lead to lung infections and increased blood vessel permeability, which worsens tissue edema and reduces circulating volume [ 2 ]. This is further supported by subsequent analysis of complications. INHI is associated with higher levels of local and systemic inflammation, and fluid overload, rather than INHI, may mediate the development of acute kidney injury in major burn patients [ 18 , 26 ]. Therefore, we believe that additional fluid resuscitation may not be required for major burn patients with combined INHI. To avoid over-resuscitation, the appropriate use of high doses of vitamin C and hypertonic saline solution may play a more active role [ 27 , 28 , 29 ].
In the late twentieth century, it was believed that INHI had escalated fluid resuscitation needs of burn victims. However, in recent years, medical concepts and technologies have been advancing, and this view has been increasingly challenged. Endorff and Gamelli found no difference in the initial 24-h fluid requirements between 25 patients with grades 0 and 1 injury (6.6 ± 0.7ml/kg/%TBSA) and 35 patients with grades 2, 3, or 4 injury (6.7 ± 0.4ml/kg/%TBSA) [ 12 ]. Similarly, in a prospective observational study conducted by Albright et al., no significant association was observed between inhalation severity grades ranging from 0 to 4 and 24-h or 72-h fluid requirements, even when comparing patients with low-grade INHI (grades 1 and 2, n = 30) to those with high-grade INHI (grades 3 and 4, n = 21) [ 18 ]. Spano et al. also found no correlation between INHI severity grades and 24-h or 48-h fluid demand. Even when the INHI subjects were divided into low-grade ( n = 78) and high-grade ( n = 20) groups, no significant difference was discovered between low-grade (6.4 ml/kg/%TBSA) and high-grade (6.6 ml/kg/%TBSA) INHI in terms of the initial 24-h fluids [ 19 ]. Our findings are in line with those of prior studies. Tracheotomy was previously thought to increase fluid resuscitation requirements in patients, but we did not observe this phenomenon in major burn patients with combined INHI. This may be due to the fact that major burn patients require a large amount of fluid resuscitation, masking the small increase in fluid requirements caused by tracheotomy.
The fluid resuscitation strategy for managing burn shock is a significant milestone in burn care. During the 1960s and 1970s, multiple protocols and formulas were developed, including the Evans, Brooke, and Parkland formula, to provide guidelines for fluid resuscitation of burns. The TMMU formula, derived from the Evans formula, is widely used in China and is considered to be more appropriate for the Chinese population. This study showed that patients with TBSA ≥ 50% required an average of 2.4 ± 0.9 ml/kg/%TBSA of fluid within the first 24 h, which is significantly lower than what Spano et al. reported using the Parkland formula (6.1 ml/kg/%TBSA). This disparity can be attributed to the earlier emphasis of the TMMU formulation on colloidal applications, which are better able to maintain vessel volume and reduce fluid requirements. Tan et al. reported similar findings, where patients with TBSA ≥ 40% who received fluid resuscitation using the TMMU formula required an average of 2.35 ± 0.59 ml/kg/%TBSA of fluid during the first 24 h [ 22 ]. After excluding the possibility of excessive resuscitation based on urine output, our findings indicate that the TMMU fluid regimen underestimated the fluid requirements of patients with extensive burns. Notably, instances of fluid administration exceeding the calculated amount based on the formula also occurred in other studies using TMMU-based resuscitation protocols [ 22 , 30 ]and crystalloid-based resuscitation formulas [ 31 , 32 ].
Limitations
There are several limitations to this study. First, despite being a multicenter retrospective study, our stringent inclusion criteria resulted in only 108 patients being included, potentially leading to a false negative result. Second, we did not evaluate lung function, pulmonary inflammation, or systemic inflammation levels, which could have provided additional insight into the pathophysiological mechanisms underlying our observations. Third, the estimation of fluid retention may not be accurate, as we did not subtract the daily explicit water loss, and the complexity of care for major burn patients may have influenced the calculation of fluid retention. Finally, Outcome differences may be due to the differing aetiologies of cause of burn, and secondary to differences in hemodynamics during resuscitation, for which we currently lack the corresponding data.
Compared to non-INHI patients, patients with concomitant INHI may not require additional fluid resuscitation. In addition, the tracheostomy may not significantly affect fluid management in major burn patients with combined INHI. Further studies are necessary to explore fluid management in burn patients with INHI and to prevent potential complications while improving overall treatment outcomes.
Availability of data and materials
The data sets used and analyzed in this study are on https://www.jianguoyun.com/p/DdI-JZoQuaiFChjVlrEFIAA
Abbreviations
- Inhalation injury
Third Military Medical University
Total burn surface area
Acute respiratory distress syndrome
Acute kidney injury
Walker PF, Buehner MF, Wood LA, Boyer NL, Driscoll IR, Lundy JB, et al. Diagnosis and management of inhalation injury: an updated review. Crit Care. 2015. https://doi.org/10.1186/s13054-015-1077-4 .
Article PubMed PubMed Central Google Scholar
Sheridan RL. Fire-related inhalation injury. N Engl J Med. 2016;375(5):464–9. https://doi.org/10.1056/NEJMra1601128 .
Article PubMed Google Scholar
Bagheri Toolaroud P, Attarchi M, Afshari Haghdoust R, Feizkhah A, Esmailzadeh M, Rimaz S, et al. Epidemiology of work-related burn injuries: a ten-year retrospective study of 429 patients at a referral burn centre in the north of iran. Int Wound J. 2023. https://doi.org/10.1111/iwj.14238 .
Swanson JW, Otto AM, Gibran NS, Klein MB, Kramer CB, Heimbach DM, et al. Trajectories to death in patients with burn injury. J Trauma Acute Care Surg. 2013;74(1):282–8. https://doi.org/10.1097/TA.0b013e3182788a1c .
Markell KW, Renz EM, White CE, Albrecht ME, Blackbourne LH, Park MS, et al. Abdominal complications after severe burns. J Am Coll Surg. 2009;208(5):940–7. https://doi.org/10.1016/j.jamcollsurg.2008.12.023 .
Li H, Wang F, Zhou J, Peng Y, Zhang J, Peng X, et al. The progress of chinese burn medicine from the third military medical university—in memory of its pioneer, professor li ao. Burns Trauma. 2017. https://doi.org/10.1186/s41038-017-0082-z .
Luo G, Peng Y, Yuan Z, Cheng W, Wu J, Tang J, et al. Fluid resuscitation for major burn patients with the tmmu protocol. Burns. 2009;35(8):1118–23. https://doi.org/10.1016/j.burns.2009.02.020 .
Sutton T, Lenk I, Conrad P, Halerz M, Mosier M. Severity of inhalation injury is predictive of alterations in gas exchange and worsened clinical outcomes. J Burn Care Res. 2017;38(6):390–5. https://doi.org/10.1097/BCR.0000000000000574 .
Mackie DP, Spoelder EJ, Paauw RJ, Knape P, Boer C. Mechanical ventilation and fluid retention in burn patients. J Trauma: Injury, Infect Crit Care. 2009;67(6):1233–8. https://doi.org/10.1097/TA.0b013e3181be9c67 .
Article Google Scholar
Guo F, Zhu YS, Huang J, Wu YH, Sun ZF, Xia XB, et al. National experts consensus on clinical diagnosis and treatment of inhalation injury (2018 version). Zhonghua Shao Shang Za Zhi. 2018;34(11):E004. https://doi.org/10.3760/cma.j.issn.1009-2587.2018.11.E004 .
Article CAS PubMed Google Scholar
Enkhbaatar P, Pruitt BJ, Suman O, Mlcak R, Wolf SE, Sakurai H, et al. Pathophysiology, research challenges, and clinical management of smoke inhalation injury. Lancet. 2016;388(10052):1437–46. https://doi.org/10.1016/S0140-6736(16)31458-1 .
Endorf FW, Gamelli RL. Inhalation injury, pulmonary perturbations, and fluid resuscitation. J Burn Care Res. 2007;28(1):80–3. https://doi.org/10.1097/BCR.0B013E31802C889F .
Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, et al. Acute respiratory distress syndrome: the berlin definition. JAMA. 2012;307(23):2526–33. https://doi.org/10.1001/jama.2012.5669 .
Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, et al. Acute kidney injury network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11(2):R31. https://doi.org/10.1186/cc5713 .
Park SH, Hemmila MR, Wahl WL. Early albumin use improves mortality in difficult to resuscitate burn patients. J Trauma Acute Care Surg. 2012;73(5):1294–7. https://doi.org/10.1097/TA.0b013e31827019b1 .
Navar PD, Saffle JR, Warden GD. Effect of inhalation injury on fluid resuscitation requirements after thermal injury. Am J Surg. 1985;150(6):716–20. https://doi.org/10.1016/0002-9610(85)90415-5 .
Inoue T, Okabayashi K, Ohtani M, Yamanoue T, Wada S, Iida K. Effect of smoke inhalation injury on fluid requirement in burn resuscitation. Hiroshima J Med Sci. 2002;51(1):1–5.
PubMed Google Scholar
Albright JM, Davis CS, Bird MD, Ramirez L, Kim H, Burnham EL, et al. The acute pulmonary inflammatory response to the graded severity of smoke inhalation injury*. Crit Care Med. 2012;40(4):1113–21. https://doi.org/10.1097/CCM.0b013e3182374a67 .
Article CAS PubMed PubMed Central Google Scholar
Spano S, Hanna S, Li Z, Wood D, Cartotto R. Does bronchoscopic evaluation of inhalation injury severity predict outcome? J Burn Care Res. 2016;37(1):1–11. https://doi.org/10.1097/BCR.0000000000000320 .
Dai NT, Chen TM, Cheng TY, Chen SL, Chen SG, Chou GH, et al. The comparison of early fluid therapy in extensive flame burns between inhalation and noninhalation injuries. Burns. 1998;24(7):671–5. https://doi.org/10.1016/s0305-4179(98)00092-8 .
Liu NT, Salinas J, Fenrich CA, Serio-Melvin ML, Kramer GC, Driscoll IR, et al. Predicting the proportion of full-thickness involvement for any given burn size based on burn resuscitation volumes. J Trauma Acute Care Surg. 2016;81(5):S144–9. https://doi.org/10.1097/TA.0000000000001166 .
Tan J, Zhou J, Li N, Yuan L, Luo G. A new resuscitation formula based on burn index provides more reliable prediction for fluid requirement in adult major burn patients. J Burn Care Res. 2021;42(5):962–7. https://doi.org/10.1093/jbcr/irab013 .
Saner FH, Pavlakovic G, Gu Y, Gensicke J, Paul A, Radtke A, et al. Effects of positive end-expiratory pressure on systemic haemodynamics, with special interest to central venous and common iliac venous pressure in liver transplanted patients. Eur J Anaesthesiol. 2006;23(9):766–71. https://doi.org/10.1017/S026502150600072X .
Kuiper JW, Groeneveld AB, Slutsky AS, Plotz FB. Mechanical ventilation and acute renal failure. Crit Care Med. 2005;33(6):1408–15. https://doi.org/10.1097/01.ccm.0000165808.30416.ef .
Bittner E, Sheridan R. Acute respiratory distress syndrome, mechanical ventilation, and inhalation injury in burn patients. Surg Clin North Am. 2023;103(3):439–51. https://doi.org/10.1016/j.suc.2023.01.006 .
Kumar AB, Andrews W, Shi Y, Shotwell MS, Dennis S, Wanderer J, et al. Fluid resuscitation mediates the association between inhalational burn injury and acute kidney injury in the major burn population. J Crit Care. 2017;38:62–7. https://doi.org/10.1016/j.jcrc.2016.10.008 .
Kremer T, Harenberg P, Hernekamp F, Riedel K, Gebhardt MM, Germann G, et al. High-dose vitamin c treatment reduces capillary leakage after burn plasma transfer in rats. J Burn Care Res. 2010;31(3):470–9. https://doi.org/10.1097/BCR.0b013e3181db5199 .
Fukui H, Iwahashi H, Endoh S, Nishio K, Yoshida Y, Hagihara Y, et al. Ascorbic acid attenuates acute pulmonary oxidative stress and inflammation caused by zinc oxide nanoparticles. J Occup Health. 2015;57(2):118–25. https://doi.org/10.1539/joh.14-0161-OA .
Du Z, Jia H, Liu J, Zhao X, Xu W. Effects of three hydrogen-rich liquids on hemorrhagic shock in rats. J Surg Res. 2015;193(1):377–82. https://doi.org/10.1016/j.jss.2014.06.051 .
Mitchell KB, Khalil E, Brennan A, Shao H, Rabbitts A, Leahy NE, et al. New management strategy for fluid resuscitation: quantifying volume in the first 48 hours after burn injury. J Burn Care Res. 2013;34(1):196–202. https://doi.org/10.1097/BCR.0b013e3182700965 .
Blumetti J, Hunt JL, Arnoldo BD, Parks JK, Purdue GF. The parkland formula under fire: is the criticism justified? J Burn Care Res. 2008;29(1):180–6. https://doi.org/10.1097/BCR.0b013e31815f5a62 .
Engrav LH, Colescott PL, Kemalyan N, Heimbach DM, Gibran NS, Solem LD, et al. A biopsy of the use of the baxter formula to resuscitate burns or do we do it like charlie did it? J Burn Care Rehabil. 2000;21(2):91–5. https://doi.org/10.1097/00004630-200021020-00002 .
Download references
Acknowledgements
We thanked Home for Researcher for language editing service.
Not applicable.
Author information
Shuao Xiao and Zeping Pan have contributed equally to this work.
Authors and Affiliations
Department of Plastic and Burn Surgery, Second Affiliated Hospital of Air Force Medical University, 569 Xinsi Road, Baqiao District, Xi’an, 710038, China
Shuao Xiao, Hang Li & Jinbin Ning
Department of Plastic and Burn Surgery, Joint Logistics Support Force of Chinese PLA, No. 927 Hospital Bao Yun Road, Puer, 665000, Yunnan, China
Zeping Pan & Hao Zhang
Department of Orthopedics, Western Theater Air Force Hospital of PLA, Chengdu, 610011, China
Yuheng Zhang
School of Basic Medicine, Fourth Military Medical University, 169 Changle West Rd, Xi’an, 710032, China
You can also search for this author in PubMed Google Scholar
Contributions
SX, ZP and JN designed the study and drafted the manuscript. HL, HZ and YZ collected assembled the data. SX and HZ performed the statistical analysis, HZ, TL, and JN critically supervised the project. All the authors read and approved the manuscript.
Corresponding authors
Correspondence to Tian Li , Hao Zhang or Jinbin Ning .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the leading institutional review board of the Second Affiliated Hospital of Air Force Medical University (#TDLL201905-32), institutional boards of Shaanxi Provincial People's Hospital, Xi'an Central Hospital, and the Yan'an University First Affiliated Hospital. It was conducted in accordance with the Helsinki Declaration of 1975 (revised in 2000). Data were collected from the patients’ medical records. The informed consent from each patient was waived, because this study was a retrospective research and patients involved in the study are anonymized.
Consent for publication
All authors gave approval of the final manuscript to be published.
Competing interests
All authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Xiao, S., Pan, Z., Li, H. et al. The impact of inhalation injury on fluid resuscitation in major burn patients: a 10-year multicenter retrospective study. Eur J Med Res 29 , 283 (2024). https://doi.org/10.1186/s40001-024-01857-w
Download citation
Received : 19 January 2024
Accepted : 23 April 2024
Published : 12 May 2024
DOI : https://doi.org/10.1186/s40001-024-01857-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Fluid resuscitation
- TMMU protocol
European Journal of Medical Research
ISSN: 2047-783X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Research article
- Open access
- Published: 10 May 2024
Total knee arthroplasty: does ultra-early physical therapy improve functional outcomes and reduce length of stay? A retrospective cohort study
- Lynn Thwin 1 ,
- Brian Rui Kye Chee 1 ,
- Yan Mei Yap 2 &
- Kelvin Guoping Tan 1
Journal of Orthopaedic Surgery and Research volume 19 , Article number: 288 ( 2024 ) Cite this article
159 Accesses
5 Altmetric
Metrics details
The Enhanced Recovery After Surgery (ERAS) Society recommends that after total knee arthroplasty (TKA), patients should be mobilized early. However, there is no consensus on how early physical therapy should be commenced. We aim to investigate whether ultra-early physical therapy (< 12 h postoperatively) leads to better outcomes.
This is a retrospective cohort study of 569 patients who underwent primary TKA from August 2017 to December 2019 at our institution. We compared patients who had undergone physical therapy either within 24 h or 24–48 h after TKA. Further subgroup analysis was performed on the < 24 h group, comparing those who had undergone PT within 12 h and within 12–24 h. The outcomes analyzed include the Oxford Knee Scoring System score, Knee Society Scores, range of motion (ROM), length of stay (LOS) and ambulatory distance on discharge. A student’s t test, chi-squared test or Fisher’s exact test was used where appropriate, to determine statistical significance of our findings.
LOS in the < 24 h group was shorter compared to the 24–48 h group (4.87 vs. 5.34 days, p = 0.002). Subgroup analysis showed that LOS was shorter in the ultra-early PT (< 12 h) group compared to the early PT (12–24 h) group (4.75 vs. 4.96 days, p = 0.009). At 3 months postoperatively, there was no significant difference in ROM, ambulatory distance or functional scores between the < 24 h group and 24–48 h group, or on subgroup analysis of the < 24 h group.
Patients who underwent physical therapy within 24 h had a shorter length of stay compared to the 24–48 h group. On subgroup analysis, ultra-early (< 12 h) physical therapy correlated with a shorter length of stay compared to the 12–24 h group (4.75 vs. 4.96 days, p = 0.009) - however, the difference is small and unlikely to be clinically significant. Ultra-early (< 12 h) physical therapy does not confer additional benefit in terms of functional scores, ROM or ambulatory distance. These findings reinforce the importance of early physical therapy after TKA in facilitating earlier patient discharge.
Introduction
Total knee arthroplasty (TKA) is the mainstay of treatment for late stage osteoarthritis, and is being performed with increasing frequency each year.
Multiple preventive strategies have been documented in the literature - surgical and nonsurgical - in an attempt to slow the progression of knee osteoarthritis [ 1 , 2 , 3 ]. However, with many countries facing an aging and more active population, the incidence of severe knee osteoarthritis requiring joint replacement continues to increase. [ 4 , 5 ]
The Enhanced Recovery After Surgery (ERAS) Society recommends that TKA patients should be mobilized as early as possible after surgery to aid quicker recovery [ 6 ]. Studies have suggested that early physical therapy helps to improve functional outcomes, range of motion (ROM) as well as in-hospital length of stay (LOS) [ 7 , 8 , 9 , 10 , 11 , 12 ]. In addition to improving functional outcomes, safely reducing the hospital LOS also helps with reducing healthcare costs as one of the main cost contributors in a TKA is the length of inpatient stay [ 13 , 14 ].
Early initiation of physical therapy (PT) post-op has been proposed as one of the ways to reduce LOS [ 7 , 15 ]. It has been shown that PT can be safely initiated as early as post operative day zero (POD 0) [ 15 ]. Some studies showed that early initiation of PT may allow a more efficient and productive PT session on subsequent days resulting in better ROM and functional outcomes [ 9 , 11 ]. Early initiation of PT can also reduce the development of complications such as deep vein thrombosis, pulmonary emboli, chest infections and urinary retention [ 16 ]. However, the definition of early PT varies from study to study. Some studies use the number of post-operative days in their definition, while others use the number of hours from the time of surgery.
In addition, while many of the studies have concentrated on the LOS as well as safety aspects of early rehabilitation, only one study has looked at the functional outcomes associated with early PT [ 11 ]. The benefit for patients in terms of functional outcomes has not been adequately studied in the existing literature.
This study aims to investigate how the timing of physical therapy affects the functional outcomes as well as LOS of patients undergoing TKA.
This is a retrospective cohort study of 569 patients who underwent primary TKA between August 2017 and December 2019 at our institution. Institutional review board approval was obtained before performing this study (NHG DSRB 2020/00095). The data was prospectively collected from our institution’s existing knee registry.
The inclusion criteria comprises:
Patients who underwent unilateral TKA.
Patients who were discharged home.
Patients who commenced physical therapy within 48 h of their surgeries.
Patients who underwent unicompartmental knee arthroplasty, revision knee arthroplasty (for any cause), or bilateral total knee arthroplasty were excluded. Patients discharged to community rehabilitation centers were also excluded.
Patient demographics and surgical data were collected for all patients, including age, gender, body mass index (BMI), side (left or right), comorbidities and duration of operation.
All the patients were admitted to the hospital on the day of surgery. The length of stay was calculated from their date of admission to the date of discharge in terms of days. The timing of each case was determined by the availability of operative resources and the primary surgeon’s preference.
The TKAs were performed using medial parapatellar approaches. All the patients received either a peripheral nerve block or periarticular injection intra-operatively. The type of anesthesia was also recorded as spinal anesthesia or general anesthesia. After the surgery, all patients were first transferred to the post-anaesthesia care unit (PACU) and thereafter to the general wards for inpatient care.
Patients were selected for physical therapy based on availability of the physiotherapists and timing of the surgery. Patients who arrived in the ward from PACU after office hours commenced their physical therapy on the following day after their surgery. All patients received physical therapy within 48 h from the time of their respective surgeries.
The aims of physical therapy were the same regardless of whether it was commenced on the day of surgery or the subsequent days. The physical therapists determined the length and frequency of therapy sessions according to the needs of individual patients.
The patients were started on continuous passive motion (CPM) on the day of their surgery. The physical therapists would assist the patients to sit over the edge of bed, and also initiate active and active assisted knee range of motion (ROM) exercises. As the patients progressed, they would be taught transfers, started on gait training, stair climbing and activities of daily living exercises.
The patients were deemed safe for discharge after they were able to ambulate with a walking aid, clear ground level obstacles safely, have adequate pain control and a clean and dry surgical site.
The amount of distance covered on the day of discharge as well as their knee ROM were recorded.
Functional outcomes were measured using the Oxford Knee Score (OKS) and Knee Society Score (KSS) and KSS (function), and were collected until three months after the operation.
The time taken from the end of surgery to the start of physical therapy was recorded. During the analysis, the patients were grouped into those that commenced physical therapy within 24 h and 24–48 h after operation. The < 24 h group was also further subdivided to < 12 h and 12–24 h. We defined patients who received PT within 24 h as early PT and those who received within 12 h as ultra-early PT. Differences in outcomes were compared between < 24 h and 24–48 h groups, and a subgroup analysis of the < 24 h group was also performed to determine whether ultra-early physical therapy has an effect on the outcomes measured.
Statistical methods
Descriptive statistics of the demographic data and outcome variables were calculated. Numerical variables were presented as mean ± standard deviation or median (IQR) and Student’s t-test was used when appropriate. Categorical variables were presented as numbers and percentage and Chi-square test or Fisher Exact test was used when appropriate. A two tailed significance level of 0.05 was used for all the tests. All statistical analyses were conducted using IBM SPSS Statistics 19.
A total of 1312 patients underwent TKA during the specified period. Of these, 569 patients had unilateral surgery and were discharged home, and were hence included in the study. 478 patients underwent PT within 24 h and 91 patients within 48 h. There were no significant differences in age, gender, BMI and preoperative hemoglobin levels, pre op range of motion as well as functional scores between the two groups (Table 1 ).
There was no statistical significance between the groups with regards to co-morbidities (Table 2 ).
There was significant reduction in LOS in the < 24 h group compared to 24–48 h group (4.87 vs. 5.34 days, p = 0.002). There were no significant differences in other functional outcome measures between the 2 groups. (Tables 3 and 4 ). There was no increase in the complication rates between the two groups of patients.
A subgroup analysis was performed for the < 24 h group to determine whether patients who received ultra-early physical therapy (< 12 h) have shorter LOS as well as other functional outcomes compared to those who underwent early physical therapy (12–24 h). The ultra-early physical therapy group showed a shorter length of stay (4.75 vs. 4.96 days, p = 0.009). There was no significant difference in PROM, ambulatory distance at discharge and functional outcome between the ultra-early PT and early PT group (Table 5 ).
Early mobilization is an integral part of enhanced recovery after surgery (ERAS) [ 17 ]. The ERAS society recommends that patients should be mobilized as soon as possible after surgery - this helps to reduce the length of stay and counteract the adverse physiological effect of prolonged bed rest [ 6 ]. In current literature, studies have shown that early mobilization or rehabilitation after total knee arthroplasty improves functional outcomes as well as reduces the length of hospital stay [ 7 , 11 , 12 , 18 , 19 ].
Our study’s findings correlate with that of previous studies which have found that early mobilization on POD 0 following TKA leads to shorter LOS [ 13 , 15 , 20 ]. Chen et al. found in their prospective cohort study that patients who ambulated with PT on POD 0 had a shorter LOS than those patients who did not [ 15 ]. Similarly, Den Hertog et al’s randomized controlled trial showed that patients who were in a POD 0 fast-track rehabilitation program had a shorter LOS compared to standard rehabilitation programs in their randomized control trial [ 7 ]. In our study, all patients received PT within POD1. Patients in the ultra-early group received PT on POD0 while patients in the early (12–24 h) group and > 24 h group had PT on POD 1. Although both ultra-early and early physical therapy showed benefits in terms of LOS, our results show that there is diminishing benefits to ultra-early physical therapy (LOS: 4.75 vs. 4.96 days comparing < 12 h and 12–24 h) compared to that of early physical therapy (LOS: 4.87 vs. 5.34 days comparing < 24 h and 24–48 h). Although the ultra-early physical therapy (< 12 h) group showed a lower LOS compared to the 12–24 h group, the small difference (4.75 vs. 4.96 days) is unlikely to be clinically significant. In the healthcare setting where resources and manpower are finite and limited, it would be necessary to weigh the benefits of a slightly reduced LOS from ultra-early physical therapy against manpower and resource limitations.
In addition, the recorded mean LOS in our study is longer than what has been reported in previous literature (Bohl et al.: median of 32 h for POD0 PT and 31 h for POD1 PT; Chen et al.: mean of 2.8 days for POD0 PT and 3.7 days for POD1 PT). There are 2 main factors that could have contributed to our longer LOS, which are: the higher average age of our patients, and the difference in criteria for safe discharge by our physical therapists. The average age of our patients’ population (67.7 years) was several years older than patients in other studies (Bohl et al. 63.7 years, Chen et al. 62.3 years) [ 8 , 15 ]. This could contribute to slower recovery from the initial surgery as well as a slower rehabilitation process. Secondly, there is a strict criteria for safe discharge from the physical therapists at our institution. These include the ability to ambulate with a walking aid, clear ground level obstacles safely, achieve adequate pain control and a clean and dry surgical site. In the study by Bohl et al. 2019, there was no explicit criteria that was mentioned for safe discharge. An arbitrary term of being “cleared” by the physical therapist was used to denote when a patient was safe to be discharged from the acute hospital ward [ 8 ]. Chen et al’s study defined their discharge criteria, which included being able to ambulate 100ft and being able to climb up and down stairs. However, the amount of assistance required and the type of mobility aid required to achieve these discharge criteria were not mentioned. In addition, patients who were discharged to skilled nursing facilities and rehabilitation facilities were also included in their study. We have observed that in our local population, a significant percentage of patients have the expectation of only being discharged when they are close to independent ambulation. This would have a great impact on the LOS as a larger number of PT sessions would be needed to get these patients back to or close to their premorbid function.
Our data finds that at 3 months follow-up, there was no significant difference in change in OKS and KSS functional scores - differing from results from other studies in the current literature. Larsen et al. conducted a randomized controlled trial to investigate the effects of accelerated rehabilitation and physical therapy after arthroplasty. Their study involved a heterogenous group of 87 patients who had undergone either total hip arthroplasty (THA), total knee arthroplasty (TKA) or unicompartmental knee arthroplasty (UKA). They found that at 3 months follow-up, there was a significant gain in quality of life (QOL) using the EQ−5D score compared to baseline [ 11 ]. However, a subgroup analysis of TKA patients did not reveal any significant difference in the functional outcomes - it appears that their findings were skewed by significantly better results experienced by the THA patients who had undergone early physical therapy. Furthermore, the intervention group not only received earlier physical therapy, but they were also provided with pre-operative education and longer physical therapy sessions. Patients in the intervention group were also cohorted in the same ward. Thus, while Larsen et al’s study shows better functional outcomes after earlier intervention, it is difficult to isolate these effects to merely early initiation of physical therapy.
While other studies have found an increase in ROM with early initiation of physical therapy, our study did not find similar results [ 9 , 10 ]. Labraca et al’s randomized controlled trial had patients placed into two groups - those receiving physical therapy either before 24 h or after 24 h postoperatively. Patients who received physical therapy within 24 h showed significantly better LOS, ROM and gait scores. While our study found a similar correlation between earlier physical therapy and a shorter LOS, it did not find that earlier physical therapy led to increased ROM at discharge.
There are several strengths to our study. Firstly, the data was collected prospectively, which reduces the risk of recall bias. Secondly, other studies investigating the early initiation (POD 0 vs. POD 1) of PT mainly use LOS as an outcome factor. The present study not only uses LOS, but also compares the ROM, ambulation distance as well as early functional outcome score (3 months) to determine the difference in outcomes when PT is initiated ultra-early, early or after 24 h from surgery. Thirdly, our sample size ( n = 569, ultra-early PT n = 216, early PT n = 262, > 24 h n = 91) is relatively large when compared to other recent studies. Finally, our study isolates time to PT as the independent variable between treatment groups - other than this, there were no differences in intervention across treatment groups.
We recognise several limitations to our study. Firstly, the patients were not randomized and patients who were not well medically, not motivated to undergo PT or underwent surgeries later in the day were self-selected to be in the 12–24 h group or 24–48 h group. This might result in selection bias in the study. Secondly, our study focuses on patients who were discharged home. Over half of our TKA patients are discharged to subacute facilities for further rehabilitation prior to being discharged home - our study does not address the effects of earlier physical therapy on this significant patient population. Thirdly, LOS was defined as the time between admission and discharge at our institution. Besides the effects of earlier physical therapy, other non-related issues such as medical complications, patient preference and administrative discharge paperwork may also influence a patient’s length of stay and obscure the differences due to earlier physical therapy.
Our study shows that early commencement of physical therapy within 24 h is important in reducing the LOS (4.87 vs. 5.34 days comparing < 24 h and 24–48 h).
Ultra-early physical therapy (< 12 h) confers additional benefit in terms of length of stay (4.75 vs. 4.96 days, p = 0.009) compared to the 12–24 h group - however, the difference is small and unlikely to be clinically significant. Ultra-early (< 12 h) physical therapy does not confer additional benefit in terms of functional scores, ROM or ambulatory distance.
These findings reinforce the importance of early physical therapy after TKA in facilitating earlier patient discharge.
Where resources permit, physical therapy should be initiated on the day of operation, and ideally as soon as the patient returns to the ward.
Data availability
Data is provided within the manuscript or supplementary information files.
Roos EM, Arden NK. Strategies for the prevention of knee osteoarthritis. Nat Rev Rheumatol. 2016;12(2):92–101. https://doi.org/10.1038/nrrheum.2015.135 .
Article CAS PubMed Google Scholar
Khal AA, Peltier E, Choufani E et al. Tibia Valga Correction by Extraperiosteal Fibular Release in Multiple Exostosis Disease. Biomedicines. 2023;11(10):2841. Published 2023 Oct 19. https://doi.org/10.3390/biomedicines11102841 .
Geng R, Li J, Yu C, et al. Knee osteoarthritis: current status and research progress in treatment (review). Exp Ther Med. 2023;26(4):481. https://doi.org/10.3892/etm.2023.12180 . Published 2023 Aug 25.
Article CAS PubMed PubMed Central Google Scholar
Matsuoka H, Nanmo H, Nojiri S, Nagao M, Nishizaki Y. Projected numbers of knee and hip arthroplasties up to the year 2030 in Japan. J Orthop Sci. 2023;28(1):161–6. https://doi.org/10.1016/j.jos.2021.09.002 .
Article PubMed Google Scholar
Klug A, Gramlich Y, Rudert M, et al. The projected volume of primary and revision total knee arthroplasty will place an immense burden on future health care systems over the next 30 years. Knee Surg Sports Traumatol Arthrosc. 2021;29(10):3287–98. https://doi.org/10.1007/s00167-020-06154-7 .
Wainwright TW, Gill M, McDonald DA, et al. Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: enhanced recovery after surgery (ERAS®) Society recommendations. Acta Orthop. 2020;91(1):3–19. https://doi.org/10.1080/17453674.2019.1683790 .
den Hertog A, Gliesche K, Timm J, Mühlbauer B, Zebrowski S. Pathway-controlled fast-track rehabilitation after total knee arthroplasty: a randomized prospective clinical study evaluating the recovery pattern, drug consumption, and length of stay. Arch Orthop Trauma Surg. 2012;132(8):1153–63. https://doi.org/10.1007/s00402-012-1528-1 .
Article Google Scholar
Bohl DD, Li J, Calkins TE, et al. Physical therapy on Postoperative Day Zero following total knee arthroplasty: a Randomized, Controlled Trial of 394 patients. J Arthroplasty. 2019;34(7S):S173–S. 177.e1.
Labraca NS, Castro-Sánchez AM, Matarán-Peñarrocha GA, Arroyo-Morales M, Sánchez-Joya Mdel M, Moreno-Lorenzo C. Benefits of starting rehabilitation within 24 hours of primary total knee arthroplasty: randomized clinical trial. Clin Rehabil. 2011;25(6):557–66. https://doi.org/10.1177/0269215510393759 .
Lenssen AF, de Bie RA. Role of physiotherapy in peri-operative management in total knee and hip surgery [published correction appears in Injury. 2007;38(10):1224]. Injury. 2006;37 Suppl 5:S41-S43. https://doi.org/10.1016/S0020-1383(07)70011-6 .
Larsen K, Sørensen OG, Hansen TB, Thomsen PB, Søballe K. Accelerated perioperative care and rehabilitation intervention for hip and knee replacement is effective: a randomized clinical trial involving 87 patients with 3 months of follow-up. Acta Orthop. 2008;79(2):149–59. https://doi.org/10.1080/17453670710014923 .
Larsen K, Hansen TB, Thomsen PB, Christiansen T, Søballe K. Cost-effectiveness of accelerated perioperative care and rehabilitation after total hip and knee arthroplasty. J Bone Joint Surg Am. 2009;91(4):761–72. https://doi.org/10.2106/JBJS.G.01472 .
Tucker A, McCusker D, Gupta N, Bunn J, Murnaghan M. Orthopaedic Enhanced Recovery Programme for Elective hip and knee arthroplasty - could a Regional Programme be beneficial? Ulster Med J. 2016;85(2):86–91.
PubMed PubMed Central Google Scholar
Molloy IB, Martin BI, Moschetti WE, Jevsevar DS. Effects of the length of stay on the Cost of Total Knee and total hip arthroplasty from 2002 to 2013. J Bone Joint Surg Am. 2017;99(5):402–7. https://doi.org/10.2106/JBJS.16.00019 .
Article PubMed PubMed Central Google Scholar
Chen AF, Stewart MK, Heyl AE, Klatt BA. Effect of immediate postoperative physical therapy on length of stay for total joint arthroplasty patients. J Arthroplasty. 2012;27(6):851–6. https://doi.org/10.1016/j.arth.2012.01.011 .
Renkawitz T, Rieder T, Handel M, et al. Comparison of two accelerated clinical pathways–after total knee replacement how fast can we really go? Clin Rehabil. 2010;24(3):230–9. https://doi.org/10.1177/0269215509353267 .
Soffin EM, YaDeau JT. Enhanced recovery after surgery for primary hip and knee arthroplasty: a review of the evidence. Br J Anaesth. 2016;117(suppl 3):iii62–72. https://doi.org/10.1093/bja/aew362 .
Guerra ML, Singh PJ, Taylor NF. Early mobilization of patients who have had a hip or knee joint replacement reduces length of stay in hospital: a systematic review. Clin Rehabil. 2015;29(9):844–54. https://doi.org/10.1177/0269215514558641 .
Pua YH, Ong PH. Association of early ambulation with length of stay and costs in total knee arthroplasty: retrospective cohort study. Am J Phys Med Rehabil. 2014;93(11):962–70. https://doi.org/10.1097/PHM.0000000000000116 .
Smith TO, McCabe C, Lister S, Christie SP, Cross J. Rehabilitation implications during the development of the Norwich Enhanced Recovery Programme (NERP) for patients following total knee and total hip arthroplasty. Orthop Traumatol Surg Res. 2012;98(5):499–505. https://doi.org/10.1016/j.otsr.2012.03.005 .
Download references
The authors declare that no funding was obtained for this study.
Author information
Authors and affiliations.
Department of Orthopaedic Surgery, Tan Tock Seng Hospital, Singapore, Singapore
Lynn Thwin, Brian Rui Kye Chee & Kelvin Guoping Tan
Department of Physiotherapy, Tan Tock Seng Hospital, Singapore, Singapore
Yan Mei Yap
You can also search for this author in PubMed Google Scholar
Contributions
L.T., B.C. and Y.Y. contributed to the main manuscript text.L.T. and Y.Y. prepared the figures.K.T. oversaw the research idea and contributed to revisions.All authors reviewed the manuscript.
Corresponding author
Correspondence to Brian Rui Kye Chee .
Ethics declarations
Ethics approval and consent to participate.
Ethical Review Committee Statement was obtained for this study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Thwin, L., Chee, B.R.K., Yap, Y.M. et al. Total knee arthroplasty: does ultra-early physical therapy improve functional outcomes and reduce length of stay? A retrospective cohort study. J Orthop Surg Res 19 , 288 (2024). https://doi.org/10.1186/s13018-024-04776-y
Download citation
Received : 20 March 2024
Accepted : 02 May 2024
Published : 10 May 2024
DOI : https://doi.org/10.1186/s13018-024-04776-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Journal of Orthopaedic Surgery and Research
ISSN: 1749-799X
- Submission enquiries: [email protected]
Retrospective research: What are the ethical and legal requirements?
Affiliation.
- 1 Faculty of Business and Economics, University of Lausanne, and Faculty of Law, Geneva, Switzerland.
- PMID: 20349361
- DOI: 10.4414/smw.2010.13041
Retrospective research is conducted on already available data and/or biologic material. Whether such research requires that patients specifically consent to the use of "their" data continues to stir controversy. From a legal and ethical point of view, it depends on several factors. The main criteria to be considered are whether the data or the sample is anonymous, whether the researcher is the one who collected it and whether the patient was told of the possible research use. In Switzerland, several laws delineate the procedure to be followed. The definition of "anonymous" is open to some interpretation. In addition, it is debatable whether consent waivers that are legally admissible for data extend to research involving human biological samples. In a few years, a new Swiss federal law on human research could clarify the regulatory landscape. Meanwhile, hospital-internal guidelines may impose stricter conditions than required by federal or cantonal law. Conversely, Swiss and European ethical texts may suggest greater flexibility and call for a looser interpretation of existing laws. The present article provides an overview of the issues for physicians, scientists, ethics committee members and policy makers involved in retrospective research in Switzerland. It aims at provoking more open discussions of the regulatory problems and possible future legal and ethical solutions.
Publication types
- Research Support, U.S. Gov't, Non-P.H.S.
- Biomedical Research / ethics*
- Biomedical Research / legislation & jurisprudence*
- Ethics, Research*
- Guidelines as Topic
- Informed Consent / ethics
- Informed Consent / legislation & jurisprudence
- Presumed Consent / ethics
- Presumed Consent / legislation & jurisprudence
- Retrospective Studies*
- Switzerland
ORIGINAL RESEARCH article
Imaging response to immune checkpoint inhibitors in patients with advanced melanoma a retrospective observational cohort study.

- Tom Baker Cancer Centre, Calgary, Alberta, Canada
The final, formatted version of the article will be published soon.
Select one of your emails
You have multiple emails registered with Frontiers:
Notify me on publication
Please enter your email address:
If you already have an account, please login
You don't have a Frontiers account ? You can register here
The association between objective imaging response and first line immune checkpoint inhibitor (ICI) therapy regimes in advanced melanoma remains uncharacterized in routine practice.We conducted a multi-center retrospective cohort analysis of advanced melanoma patients receiving first line ICI therapy from August 2013-May 2020 in Alberta, Canada. The primary outcome was likelihood of RECIST v1.1 assessed objective imaging response between patients receiving antiprogrammed cell death protein 1 (anti-PD1) monotherapy and those receiving combination ipilimumabnivolumab. Secondary outcomes were identification of baseline characteristics associated with nonresponse and the association of imaging response with overall survival (OS) and time to next treatment (TTNT).Results: 198 patients were included, 41/198 (20.7%) had complete response, 86/198 (43.4%) had partial response, 23/198 (11.6%) had stable disease, and 48/198 (24.2%) had progressive disease. Median OS was not reached (NR) (95% CI 49.0-NR) months for complete responders, NR (95%CI 52.9-NR) months for partial responders, 33.7 (95%CI 15.8-NR) months for stable disease, and 6.4 (95%CI 5.2-10.1) months for progressive disease (log-rank p<0.001). Likelihood of objective imaging response remained similar between anti-PD1 monotherapy and ipilimumab-nivolumab groups (OR 1.95 95%CI 0.85-4.63, p=0.121).Elevated LDH level (OR 0.46; 95%CI 0.21-0.98, p=0.043), mucosal primary site (OR 0.14; 95%CI 0.03-0.48, p=0.003), and BRAF V600E mutation status (OR 0.31; 95%CI 0.13-0.72, p=0.007) were associated with decreased likelihood of response.No significant difference in likelihood of imaging response between anti-PD1 monotherapy and combination ipilimumab-nivolumab was observed. Elevated LDH level, mucosal primary site, and BRAF V600E mutation status were associated with decreased likelihood of response. Given that pivotal clinical trials of ipilimumab-nivolumab did not formally compare ipilimumab-nivolumab with nivolumab monotherapy, this work adds context to differences in outcomes when these agents are used. These results may inform treatment selection, and aid in counseling of patients treated with first-line ICI therapy in routine clinical practice settings.
Keywords: Melanoma, Immunotherapy, RECIST = Response Evaluation Criteria in Solid Tumors, Survival, prognosis
Received: 12 Feb 2024; Accepted: 13 May 2024.
Copyright: © 2024 Gupta, Stukalin, Meyers, Heng, Monzon, Cheng and Navani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Igor Stukalin, Tom Baker Cancer Centre, Calgary, T2N 4N2, Alberta, Canada Daniel E. Meyers, Tom Baker Cancer Centre, Calgary, T2N 4N2, Alberta, Canada Daniel Y. Heng, Tom Baker Cancer Centre, Calgary, T2N 4N2, Alberta, Canada Jose Monzon, Tom Baker Cancer Centre, Calgary, T2N 4N2, Alberta, Canada Tina Cheng, Tom Baker Cancer Centre, Calgary, T2N 4N2, Alberta, Canada Vishal Navani, Tom Baker Cancer Centre, Calgary, T2N 4N2, Alberta, Canada
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Secondary Menu

What was it like to go back through your career in this comprehensive way?
Through this process of organization, I became much more conscious of how each one of my series evolves. I work a lot in series I've developed over many years, and because I had to find the specific date in which everything happened, it certainly helped me understand how I think and how I make work.
I knew that I painted and I drew, but I actually had no idea that it was almost 70% of my practice. I have an actual quantitative way to demonstrate that through that database. Technically, that makes me a painter, even though I don't teach painting classes anymore. It's kind of fascinating.
For me, it was more like a desire. Part of my logic before we did the retrospective was: I want to be a painter, but I'm not. This whole process has made clear to me that I have been making work, it just hasn't been in the institutions of display.
Has looking back on your work changed how you're looking forward? Has it changed your approach to ongoing work?
Yeah, certainly. It's really making me feel like I can move on.
The exhibit includes 18 series that have been developed over many years. Of those 18, only like five or six had been exhibited thoroughly. I felt like the others were completed as artworks, but they were not out there. It's kind of like your children: It's not until they get a job or something that you feel like you’re done. You don't want them to be precarious and vulnerable. Now that I feel that they are out there in public view, I can really make works in a different way.
Ironically, even though I’ve had to obsessively think about the past for two years, now, I'm liberated from it.
Were there any things that you've been working on now that you recognized as you went back through your career — things that made you go, Oh, I've actually done this before?
I definitely am one of those artists that works a lot with continuity. Sometimes it's very obvious, like the Black Mirror series. Every time I make a new installation, there's common threads and common methods.

But my quasi-obsession with numbers and abstraction only became clear through this process. Throughout the pandemic, I was making a work called “2022,” and one of the works in the retrospective is this project called “Hexagonal Investigations” that I stopped around 20 years ago. For three or four years, I was obsessively working with a number of six. It really did let me see how nothing is new in a certain way. You just come at it from a very different perspective.
One thing that it also made very clear is that as you get more and more professional over the years — and this is going to sound a little bit sad — you get less time to play. The beauty of becoming a more established artist is that as you come up with an idea, you can actually execute it relatively fast, whereas in your first 10 or 20 years, you can sit on it because nobody has ever shown it or it takes you a decade to secure the funding for it.
While it's challenging in those first few years, the beauty of it is that you play a lot more.
You were born in Mexico, but you’ve lived in the United States for a long time. How does it feel to have your first retrospective exhibit taking place in Mexico?
Four or five years ago, I would have said it's going to take a decade or two longer for me to have a major show in Mexico. It was a very happy surprise to be doing the show not just in Mexico but through what effectively is the equivalent of the Smithsonian.
I've been kind of surprised what a Mexican show it is, having lived abroad for so many years. I don't think of myself as someone who makes artwork that only resonates in one place or another. But now that I'm seeing the catalog really come together, I realize the content makes a lot of sense in Mexico, so maybe it makes sense that the show was there.
There are works about the Mexican oil industry, which was nationalized decades ago and then privatized again. Stuff like that, I don't expect audiences abroad to really get the full meaning of the works, right?
What comes next for you?
I would say the main two things that came out of the pandemic and this period of extreme isolation were the retrospective and this body of work called “2022,” which was included in this major international exhibition called “Documenta 15” in collaboration with artists from Haiti that I've worked with since 2009. It has been postponed, so once I'm done with this retrospective, I’ll be freed to finish that.
In terms of new work, I was just invited to this major conference in Saudi Arabia called Future Culture Summit with all these really established museum directors, curators, fellow artists and thinkers. I'm really excited about just having this white space now before me to explore future collaborations. A few years ago, I would have felt like: No, that's going to be a distraction. Now I think I'm actually excited about not knowing exactly what I'm going to do in the next few years.
I'm also in the early stages of several projects I am producing in my role as director of the FHI Social Practice Lab and founder of Duke's Artistic Research Initiative . The generous support we received from the Mellon Foundation is allowing for new large-scale collaborations with great people like Sherrill Roland, Leonid Tsvetkov, Rashida Bumbray, Wanda Nanibush and Nicholas Mirzoeff, as well as a group of soon to be announced First Nations, Native American, indigenous contemporary artists, historians and thinkers.
- Mission Statement
- Diversity, Equity and Inclusion Initiatives
- Learning Outcomes
- Local Arts Links
- ARTHIST 345
- ARTHIST 383
- Art History
- Art History: Architecture
- Art History: Museum Theory & Practice
- Art History & Visual Arts
- Computational Media: Interdepartmental Major in Computer Science and Visual and Media Studies
- Visual Arts
- Visual & Media Studies
- Visual and Media Studies: Cinematic Arts
- Computational Media: Interdepartmental Minor in Computer Science and Visual and Media Studies
- Photography
- Cinematic Arts Minor
- Frequently Asked Questions
- How to Apply
- Where Our Students Go
- Capstone Projects
- Graduation with Distinction
- Global Education
- Independent Study & Research
- Senior Portfolio
- Undergrad Grants & Resources
- Student Funding
- Trinity Ambassadors
- Ph.D. in Art History & Visual Culture
- Ph.D. in Computational Media, Arts & Cultures
- MA in Computational Media
- MA in Digital Art History
- MFA in Experimental & Documentary Arts
- Financial Aid
- Meet Our Graduate Students
- Living in Durham
- MA in Digital Art History/Computational Media Students: 2015-2021
- PhD in Art History & Visual Culture Students: 2008-2021
- PhD in CMAC: Retrospective Booklet 2016-2021
- Advising Statement of Expectations
- Dissertation
- Independent Study
- Language Requirement
- Preliminary Exam
- Progress Toward the Degree
- Professional Development
- Historical & Cultural Visualization
- Cinematic Arts
- Computational Media, Arts & Cultures
- Fall 2024 Core Courses
- Primary Faculty
- Secondary Faculty
- Instructors, Adjunct and Visiting Faculty
- Emeriti Faculty
- Post Docs & Researchers
- Graduate Students
- Student Visual Arts Projects
- Faculty Visual Arts Projects
- Faculty Art History Projects
- Student Visual & Media Studies Projects
- Faculty Visual & Media Studies Projects
- Selected Faculty Books
- Related Programs
- Smith Warehouse Art Exhibition Space Request
- Alumni Profiles
- For Our Students
- Assisting Duke Students
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Can Acad Child Adolesc Psychiatry
- v.15(3); 2006 Aug
Language: English | French
A Methodology for Conducting Retrospective Chart Review Research in Child and Adolescent Psychiatry
Robin e. gearing.
1 Columbia University School of Social Work, New York, New York
Irfan A. Mian
2 Department of Psychiatry, The Hospital for Sick Children, Toronto, Ontario
3 Department of Psychiatry, Faculty of Medicine, University of Toronto, Ontario
4 Deputy Vice-Chancellor, RMIT University, Melbourne, Australia
Abel Ickowicz
Introduction.
Retrospective research has become largely undervalued and underutilized in child and adolescent psychiatry with the increasing singular focus on randomized control trials, despite the wealth of clinically relevant data available in historical medical records. In this paper a systematic and scientific approach to chart review research methodology for psychiatry is described.
Informed by available literature, a methodological stepwise approach for retrospective chart review was developed.
A nine step method aimed at maximizing benefits and minimizing limitations is discussed.
Conclusions
Retrospective chart review is an important methodology with distinct advantages and has the potential to provide psychiatry with valuable research opportunities. This method of study should not be lost in the field of psychiatry.
Résumé
La recherche rétrospective est sous-évaluée et sous-utilisée en psychiatrie de l’enfant et de l’adolescent, en dépit de la richesse des données cliniques pertinentes qui existent dans les dossiers médicaux. Cet article décrit une approche systématique et scientifique de la recherche en psychiatrie.
Méthode
Nous avons mis au point une méthode rétro-spective d’analyse des dossiers, documentée par la littérature existante.
Résultats
Nous présentons une méthode en neuf points destinée à maximiser les avantages et à minimiser les limites de l’analyse.
L’analyse rétrospective des dossiers est une méthodologie intéressante qui présente des avantages particuliers et peut offrir d’intéressantes possibilités de recherche en psychiatrie. Cette méthode d’étude ne devrait pas être perdue de vue en psychiatrie.
Retrospective research often requires the analysis of data that were originally collected for reasons other than research ( Hess, 2004 ; Jansen et al., 2005 ). This includes physician and nursing notes, ambulatory and emergency room reports, consultations, admission and discharge documentation, laboratory and diagnostic testing reports, and other clinical or administrative data.
For over eight decades, the systematic investigation of historical records has guided various clinical research ( Butler & Quinlan, 1958 ; Wu & Ashton, 1997 ). The scientific utilization of existing health records is common in epidemiological investigations ( Haley et al., 1980 ; Jansen et al., 2005 ), quality assessment and improvement studies ( Allison et al., 2000 ; Kirkorian, 1979 ), professional education and residency training ( Holmboe, Gross, & Hawkins, 1996 ; Neidich, 1990 ; Pan, Fergusson, Schweitzer., & Hebert, 2005 ), examination of inpatient care ( Ashton, Kuykendell, Johnson, Wray, & Wu, 1995 ; Wu & Ashton, 1997 ), and in clinical research ( Hellings, 2004 ; Rajeev, Srinath, Girimaji, Seshadri, & Singh, 2004 ; Staller, Kunwar, & Simionescu, 2005 ). Investigations using retrospective chart reviews or health record reviews have been reported to comprise 25% of all scientific articles in emergency medical journals ( Worster & Haines, 2004 ). In comparison, while a number of psychiatric studies have successfully extracted relevant data from systematic chart reviews ( Baldassano, Ghaemi, Chang, Lyman, & Lipari, 2004 ; Barzman et al., 2004 ; Bloch et al., 2005 ; Dworkin, 1987 ; Goldstein & Schwebach, 2004 ; Grant, 2005 ; Henderson et al., 2004 ; Marchand, Wirth, & Simon, 2004 ; Staller, 2004 ), its application is frequently limited and research findings questioned. Consequently, retrospective research is often undervalued and, hence, underutilized in psychiatry. The reluctance to use this research methodology may result from the lack of clear benefits of this approach; minimizing its recognized methodology maintains the limitations.
The advantages of conducting chart reviews include: a relatively inexpensive ability to research the rich readily accessible existing data; easier access to conditions where there is a long latency between exposure and disease, allowing the study of rare occurrences; and most importantly, the generation of hypotheses that then would be tested prospectively ( Hess, 2004 ; VonKoss Krowchuk, Moore, & Richardson, 1995 ; Wu & Ashton, 1997 ; Worster & Haines, 2004 ). However, the limitations of incomplete documentation, including missing charts, information that is unrecoverable or unrecorded, difficulty interpreting information found in the documents (e.g. jargon, acronyms, photocopies, and microfiches), problematic verification of information and difficulty establishing cause and effect, variance in the quality of information recorded by medical professionals ( Dworkin, 1987 ; Hess, 2004 ; Pan et al., 2005 ; VonKoss Krowchuk, 1995 ), have discouraged researchers from adopting this methodology. More developmental work is required to enhance its applicability ( Wu & Ashton, 1997 ). We have sought to address this gap in the literature by developing a methodology for conducting retrospective chart review research in psychiatry.
Methodological Guidelines
To extract data effectively and systematically from historical records requires a number of discrete steps.
Step One: Conception
The conception stage is comprised of two components: research formulation and a clinical scan. Research formulation involves the process of articulating the research questions followed by the generation of clear hypotheses. Outlining a research question and hypothesis enables investigators to determine feasibility of retrospective chart review, instead of considering an alternative methodology. Early linking of research methodology to the study’s proposed hypothesis facilitates an informed approach that assists decisions throughout the subsequent research stages.
The second conceptual component is conducting a clinical scan of the research question and hypothesis. Seeking out clinical expertise in this stage uncovers unanticipated benefits while identifying potential methodological barriers. The earlier an investigation seeks to incorporate wider input from others, the sooner the benefits of support, expertise, sample recruitment and promotion can be achieved. Despite its sound benefits, this step often receives less attention and is rarely recognized as a definitive step ( Hess, 2004 ).
Step Two: Literature Review
This stage involves a systematic review of the literature pertinent to the study’s area of focus, diagnoses, conditions, demographics, criteria, and populations. A review of the literature is a standard requirement for any research initiative, including retrospective chart reviews ( Findley & Daum, 1989 ; Hess, 2004 ; Jansen et al., 2005 ; Worster & Haines, 2004 ). The importance and process of conducting literature reviews is well established and it is not necessary to dwell on this step. However, it is important to note that an effective literature review requires searching several databases such as MEDLINE, PyschInfo, CINAHL, and EMBASE; it is also recommended that Boolean searches be conducted in each database. Librarians and information technologists in hospital and university libraries are valuable resources and should be consulted by investigators unfamiliar with conducting literature reviews. In addition to traditional published articles, conference proceedings and dissertations are worthy of consideration. An exhaustive literature review will provide the required background and will illuminate how other researchers operationalized key concepts or variables.
Step Three: Proposal Development
The development of a chart review research proposal comprises writing the research proposal and operationalization of the variables. Common to all research proposals, the construction of a research proposal must include an executive summary or abstract, introduction, literature review, research question and hypotheses, methodology (design, sample, instruments, and procedure), significance of the study, limitations, budget, references, and appropriate appendices. It is also important that retrospective chart review proposals be written with some consideration for future prospective studies ( Dworkin, 1987 ; Findley & Daum, 1989 ; VonKoss Krowchuk et al., 1995 ; Worster & Haines, 2004 ). Operationalization of the study variables in a review consists of two interconnected and iterative components. First, the study variables need to be defined; these variables are generally determined by the nature and focus of the investigation. Second, study variables are then reviewed in the literature to determine how other researchers have operationalized them in similar or related investigations. It is helpful to develop an appendix comprised of concise definitions and supported with citations of studies that have similarly used each variable.
Understanding the design of existing health records and how the data is recorded is of great importance. The following strategies will assist in this process. First, it has been recommended that researchers examine the flow of information, specifically from patient to health record ( Jansen et al., 2005 ) in order to identify established charting protocols, accepted processes of documentation, and the nature of standard documentation (e.g., emergency notes, diagnostic information, consultations, and discharge reports). Second, carefully inspect a few charts; three to five charts are recommended ( Findley & Daum, 1989 ; Smith, 1996 ). This will provide critical information on how the patient chart/health record is constructed and documented. Third, consult with site-specific clinicians to ascertain how patient information is recorded and documented in multi-site studies. A clear definition of the study variables and understanding of health records provide the essential base for researchers to development a standardized chart review data abstraction instrument.
Step Four: Data Abstraction Instrument
Organization, simplicity and clarity are essential criteria for the development of a uniform data abstraction instrument. Data collection should be organized in a logical order ( Smith, 1996 ), and when possible should parallel the flow of the information in the health record. Each variable needs a simple and unambiguous response section, where the abstractors can capture the required information. Internal validity and reproducibility of any retrospective study is significantly enhanced in the standardization of the data ( Jansen et al., 2005 ). This data abstraction instrument can be a paper or an electronic document ( Allison et al., 2000 ). A paper instrument has some advantages, notably cost effectiveness and easier application across multiple sites. However, an electronic version is more cost effective in large investigations, reduces input error (e.g., predetermined drop down categories), and allows for easier centralization and access to data.
Finally, researchers need to decide how the data will be managed, stored, and analyzed. While pen-and-paper systems can be developed, it is strongly recommended that a data abstraction software package be used ( Wu & Ashton, 1997 ). Several data abstraction software packages exist, such as Microsoft Access (Microsoft Corporation, Redmond, Wash) and MedQuest (Fu and Associates, Arlington, Va) ( Allison et al., 2000 ; Banks, 1998 ; Worster & Haines, 2004 ). These packages translate the data abstraction instrument into an electronic form that can be used for data input, quality control, and the management of the data (e.g. statistical analysis and reporting). Furthermore, these programs are widely available, inexpensive, and user friendly.
Step Five: Develop Protocols and Guidelines for Abstraction
For any data abstraction instrument it is essential to develop a coding manual that provides a clear set of protocols and guidelines to instruct the reviewers in the collection of data ( Findley & Daum, 1989 ; Hess, 2004 ; Wu & Ashton, 1997 ). This serves as a reference manual as to how the data will be abstracted from the health record. The manual should list each variable and explain how the variable will be captured in the data abstraction instrument, describe where the variables are located in the health record, and provide the required protocols to extract the data. Protocols with explicit criteria are designed to increase the inter-rater reliability of data abstraction ( Goldman, 1992 ; VonKoss Krowchuk et al., 1995 ). Consequently, protocols generally require revisions, specifically following the piloting of the study.
Step Six: Data Abstraction
To abstract data effectively it is essential to understand the specific requirements of each site to determine the procedures needed to select, train, and manage the study’s data abstractors. Every health care institution has an established set of guidelines, to which all studies must adhere. While many parallels exist across institutions for conducting a retrospective chart review, common differences among institutions are the procedures for chart procurement, retrieval rates, and access to patient charts. A number of considerations need to be taken in to account, such as who may access the charts (e.g., hospital employee), the available space provided to read the charts (few institutions allow charts to be removed), the site’s hours of operation and access, and policies regarding photocopying and use of institutional or personal computers. Any of these can potentially influence effective data abstraction and require clarity before study commencement.
Data abstractors need to be carefully selected and trained ( Allison et al., 2000 ; Pan et al., 2005 ; Wu & Ashton, 1997 ). It is preferable to select abstractors with experience in retrospective research or the area under investigation. It is also advantageous to select abstractors from health care professions, preferably with advanced levels of educations (e.g., Master’s Degree). To ensure inter-rater reliability it is imperative to have a minimum of two abstractors, but it has been recommended to have four ( Allison et al., 2000 ). It is important to determine how many abstractors are required and whether abstractors should be project based or site-specific. When possible it is preferable to use abstractors across sites rather than as on-site data collectors ( Jansen et al., 2005 , Jasperse & Ahmed, 1989 ). An alternative practice is to have one or two key abstractors train, assist, and audit site-specific data abstractors. A standard recommendation is that data abstractors remain blind to the study hypothesis to minimize “subjectivity in classification in relation to personal theories about the study’s aims” ( Worster & Haines, 2004 , p. 189).
Abstractors blind to the hypothesis decrease reviewer bias, specifically the possibility of their assessment being swayed by knowledge of others (e.g., investigators), concern over adversely effecting the study’s outcome, or interpreting their abstraction as too lenient or harsh ( Allison et al., 2000 ; Chaplan, Posner, & Cheney, 1991; Goldman, 1992 ; Wu & Ashton, 1997 ). Abstractors must become familiar with a health record, be aware where the information is located, and strive to remain objective ( Haley et al., 1980 ; Smith, 1996 ). Abstractors should be carefully trained with the data abstraction instrument and the accompanying protocols and guidelines. It has also been reported that the accuracy of reviewers increases when the individuals know they are being monitored ( Wu & Ashton, 1997 ). Finally it is important to the reliability of the investigation to determine the inter-rater reliability of both the data abstraction instrument and the individual data abstractors. This can be accomplished though a pilot investigation and/or random checks.
Finally, protocols are intended to resolve any ambiguous or conflicting data. It is important for abstractors to have established management procedures to resolve any conflict. Protocols may include scheduled meetings between abstractors to resolve data conflicts, access to research investigators for clarification, or the establishment of an independent adjudication committee for consultation ( Jansen et al., 2005 ; VonKoss Krowchuk, 1995 ).
Step Seven: Sample
Every retrospective chart review requires a statistical power analysis to determine the appropriate sample size. Calculating the appropriate sample size is a necessary component in all research proposals and is dependant on the statistical tests used in the study. Calculating sample size is beyond the scope of this article, but can be accessed in a literature review or through consultation with a biostatistician. A rule for quickly determining sample size is 10 cases (charts) per variable, in order to obtain results that are likely to be both true and clinically useful ( Sackett, Haynes, Guyatt, & Tugwell, 1991 ). While the literature generally holds ten events per predictor as an accepted norm (Findlay & Daum, 1989; Harrell, Lee, Machar, & Reichert, 1985 ; Sackett et al., 1991 ), others have suggested that it is acceptable to have a minimum of seven or five events per predictor ( Raykov & Wideman, 1995 ).
In conducting any retrospective chart review study, sampling refers to the method by which study cases or records are selected from the target population or database ( Worster & Haines, 2004 ). Three commonly used sampling methods in retrospective chart review are convenience, quota, and systematic sampling. In convenience sampling, the most common method, suitable cases are selected over a specific time frame; in quota sampling, a predetermined number of cases are sought from each site or diagnostic determinant; in systematic sampling, every ‘nth’ case is selected from the target population. Ascertaining the most appropriate sampling method depends on a number of factors including the importance of probability sampling, the epidemiological nature and prevalence of the specific condition, population availability, research budget, and time constraints.
The management of missing data poses methodological limitations in conducting chart review research ( Hellings, 2004 ; VonKoss Krowchuk et al., 1995 ). Rules about how missing data will be handled should be devised before data collection begins ( Wu & Ashton, 1997 ). In retrospective chart reviews, missing data can result in a hidden or non-response bias in the results, where cases with missing information may differ from the other cases ( Worster & Haines, 2004 ). Generally, managing missing values is treated either by the deletion of the case or variable, or imputing the missing value through averaging or maximum likelihood strategies ( Dworkin, 1987 ; Worster & Haines, 2004 ). In case or variable deletion, the entire case or variable is deleted from the analysis; however, this can reduce the sample size or may introduce a hidden bias ( Dworkin, 1987 ). Imputing missing responses through statistical analysis is more common in very large computerized databases ( Worster & Haines, 2004 ), and assumes that missing data are randomly absent. The most common maximum likelihood strategy is assigning the missing value as one response, such as with a “yes” or “no” question where the absence of a “yes” results in an immediate “no”.
There is no universal method for managing missing data, but it is imperative that researchers designing, implementing, and conducting retrospective chart review research develop protocols to address this issue. While the difficulties of missing data can often be specific to each investigation, strategies to manage this phenomenon can be garnered from anticipating common concerns associated with missing data. The most effective method to determine the development of any problems from missing data is to conduct a pilot study.
Step Eight: Ethics
It is not permissible to conduct a research study without ethics approval from an institutional review board. Therefore, it is an important step to obtain approval from the institutional review board(s) where the retrospective research will be conducted ( Hess, 2004 ). Further, it is increasingly becoming standard that researchers conducting retrospective studies publish their ethics board approval in the methods section ( Baldassano et al., 2004 ; Clayton & Thorne, 2000 ; Grant, 2005 ; Henderson et al., 2004 ; Preen, Holman, Lawrence, Baynham, & Semmens, 2004 ; Woogh, 2001 ). While the requirements for institutional review boards are standard, each board has their own protocols and policies for applicants. It is recommended that researchers contact the institution’s research ethics board coordinator, as they can provide valuable and time-saving site specific information and assistance. Any changes to the research protocols generally need to be submitted to the review board for an amended approval.
Step Nine: Pilot Study
A pilot study is essentially a small version of the proposed research. Pilot studies are critical in any study design ( Perry, 2001 ; Van Teijlingen & Hundley, 2002 ). These preliminary investigations typically lack the sample size that is needed to determine statistical significance to validate a hypothesis or evaluate an instrument ( Lydiard, 1991 ; Thompson & Spier, 1989 ), yet offer researchers valuable information. Specifically, pilot studies allow researchers to assess the feasibility of the planned investigation, determine the adequacy of the instrumentation, and evaluate any potential methodological pitfalls, such as data collection strategies ( Prescott & Soeken, 1989 ). Moreover, pilot studies provide investigators with an opportunity to evaluate the reliability of their data abstraction sheet ( Smith, 1996 ), clarify the data abstraction protocols, determine the frequency with which items are missing from the chart ( Wu & Ashton, 1997 ), provide information on the institution’s chart retrieval rates and the process of pulling charts, and evaluate any potential sampling concerns or impact resulting from inclusion and exclusion criteria ( Jansen et al., 2005 ).
In retrospective chart review investigations, a general recognized guideline for reliability is that pilot studies should target ten percent of the overall sample ( Gabel & Shindledecker, 1990 ; Wu & Ashton, 1997 ). In determining the actual pilot sample, the ten percent guideline needs to be adjusted to account for any concerns relating to the institution’s retrieval or availability rates and/or participant response rates if consent for their participation is required. When possible, it is preferable that pilot charts be randomly procured.
As described above, reliability is an important rationale for conducting a pilot study in this methodology. Inter-rater reliability is measured as a percentage of agreement when two or more abstractors collect data from the same chart ( Allison et al., 2000 ). A less frequently used form of reliability is intra-rater reliability, which involves that same abstractor collecting data from the same chart on two separate occasions. Depending on the variables’ level of measurement, a Cohen’s kappa (Kappa) rating or an intra-class correlation coefficient (ICC) can statistically measure the reliability. It is recommended that a minimum of 80% and preferably 95% reliability be achieved for important variables ( Allison et al., 2000 ; Rosen, 1995 ), and that variables with reliability below 70% be reassessed or re-operationalized.
A comprehensive and functional nine-step method for conducting retrospective chart review research in psychiatry has been developed. See, Table 1 : Methodological Steps: Conducting Retrospective Chart Review Research in Psychiatry.
Methodological Steps: Conducting Retrospective Chart Review Research in Psychiatry
The initial methodological steps begin with the conception of the retrospective research that facilitates the required literature review and subsequent proposal development. The middle steps centre on the development of a data abstraction instrument and necessary protocols and guidelines, which effectively guide the retrieval of data. The final methodological steps focus on the fundamental components of retrospective research, including data abstraction, sampling issues, ethics approval and conclude with the importance of conducting a pilot study. This nine-step model has sought to maximize benefits and minimize limitations of this methodology. Each step has highlighted components to improve the reliability and validity of this methodology, such as finding and accessing appropriate and accurate data, obtaining consistent information, improving inter-rater reliability, uniformly training data abstractors, and reducing bias. Further, this model has sought to address many of the limitations within this approach, including limiting potential abstraction and management errors, resolving ambiguous data, managing missing data, and calculating effective sample size.
The scientific and systematic investigation of existing health records is an important and valued methodology in health care research, specifically in epidemiology, quality assessment studies, and emergency medicine ( Worster & Haines, 2004 ; Wu & Ashton, 1997 ). Notwithstanding the recognized and considerable benefits of this methodology, retrospective research has been undervalued and underutilized in psychiatry and mental health disciplines. While there remain many notable limitations to retrospective chart review research, including incomplete or missing documentation, poorly recorded, and absent information, as a methodology it continues to offer numerous advantages.
This article has offered a clear nine-step approach for conducting retrospective chart review research that may assist researchers in psychiatry and mental health to access the benefits of this methodology and minimize its limitations. Following these nine steps will increase the scientific rigour through a standard process. This process guides the clinician researcher in the process of conception and development, definition of variables, and sampling issues. The strategies outlined for procurement and abstraction of data will assist in minimizing limitations and strengthen the reliability of the data. This methodology enables clinicians to effectively conduct research that can inform and add to their practice. Retrospective chart review is an important methodology with distinct advantages and has the potential to provide us with valuable research opportunities. This method of study should not be lost in the field of psychiatry.
- Allison JJ, Wall TC, Spettell CM, Calhoun J, Fargason CA, Kobylinski RW, Farmer R, Kiefe C. The art and science of chart review. Journal of Quality Improvement. 2000; 26 (3):115–136. [ PubMed ] [ Google Scholar ]
- Ashton CM, Kuykendell DH, Johnson ML, Wray NP, Wu L. The association between the quality of inpatient care and early readmission. Annals of Internal Medicine. 1995; 122 :415–421. [ PubMed ] [ Google Scholar ]
- Baldassano CF, Ghaemi SN, Chang A, Lyman A, Lipari M. Acute treatment of bipolar depression with adjunctive zonisamide: A retrospective chart review. Bipolar Disorders. 2004; 6 :432–434. [ PubMed ] [ Google Scholar ]
- Banks N. Designing medical record abstraction forms. International Journal of Qualitative Health Care. 1998; 10 :163–167. [ PubMed ] [ Google Scholar ]
- Barzman DH, DelBello MP, Kowatch RA, Gernert B, Fleck DE, Pathak S, Rappaport K, Delgado SV, Campbell P, Strakowski SM. The effectiveness and tolerability of aripiprazole for pediatric bipolar disordersd: A retrospective chart review. Journal of Child and Adolescent Psychopharmacology. 2004; 14 (4):593–600. [ PubMed ] [ Google Scholar ]
- Bloch Y, Ratzoni G, Sobol D, Mendlovic S, Gal G, Levkovitz Y. Gender differences in electro-convulsive therapy: A retrospective chart review. Journal of Affective Disorders. 2005; 84 :99–102. [ PubMed ] [ Google Scholar ]
- Butler JJ, Quinlan JW. Internal audit in the department of medicine of community hospital: 2 years’ experience. Journal of the American Medical Association. 1958; 167 :567–572. [ PubMed ] [ Google Scholar ]
- Caplan RA, Posner KL, Cheney FW. Effect of outcome of physician judgments of appropriateness of care. Journal of the American Medical Association. 1991; 265 :1957–1960. [ PubMed ] [ Google Scholar ]
- Clayton A, Thorne T. Diary data enhancing rigour: Analysis framework and verification tool. Journal of Advanced Nursing. 2000; 32 (6):1514–1521. [ PubMed ] [ Google Scholar ]
- Dworkin RJ. Hidden bias in the use of archival data. Evaluation and the Health Professions. 1987; 10 (2):173–185. [ PubMed ] [ Google Scholar ]
- Findley TW, Daum MC. Research in physical medicine and rehabilitation III: The chart review or how to use clinical data for exploratory retrospective studies. American Journal of Physical Medicine and Rehabilitation. 1989; 68 (3):150–157. [ PubMed ] [ Google Scholar ]
- Gabel S, Shindledecker R. Parental substance abuse and suspected child abuse/maltreatment predict outcome in children’s inpatient treatment. Journal of the American Academy of Child and Adolescent Psychiatry. 1990; 29 (6):919–924. [ PubMed ] [ Google Scholar ]
- Goldman RL. The reliability of peer assessments of quality of care. Journal of the American Medical Association. 1992; 267 :958–960. [ PubMed ] [ Google Scholar ]
- Goldstein S, Schwebach AJ. The comorbidty of pervasive developmental disorder and attention deficit hyperactivity disorder: Results of a retrospective chart review. Journal of Autism and Developmental Disorders. 2004; 34 (3):329–339. [ PubMed ] [ Google Scholar ]
- Grant JE. Outcome study of kleptomania patients treated with naltrexone: A chart review. Journal of Clinical Neuropharmacology. 2005; 28 (1):11–14. [ PubMed ] [ Google Scholar ]
- Haley RW, Hooton TM, Schoenfelder JR, Crossley KB, Quade D, Stanley RC, Culver DH. Effect of an infection surveillance and control program on the accuracy of retrospective chart review. American Journal of Epidemiology. 1980; 111 (5):543–555. [ PubMed ] [ Google Scholar ]
- Harrell FE, Lee KL, Machar DB, Reichert TA. Regressive models for prognostic prediction: Advantages, problems, and suggested solutions. Cancer Treatment Report. 1985; 69 (10):1071–1077. [ PubMed ] [ Google Scholar ]
- Hellings P. A rich source of clinical research data: Medical records and telephone logs. Journal of Pediatric Health Care. 2004; 18 (3):154–155. [ PubMed ] [ Google Scholar ]
- Henderson DC, Daley TB, Kunkel L, Rodrigues-Scott M, Koul P, Hayden D. Clozapine and hypertension: A chart review of 82 patients. Journal of Clinical Psychiatry. 2004; 65 (5):686–689. [ PubMed ] [ Google Scholar ]
- Hess DR. Retrospective studies and chart reviews. Respiratory Care. 2004; 49 (10):1171–1174. [ PubMed ] [ Google Scholar ]
- Holmboe E, Gross R, Hawkins R. Chart reviews for residents. Academic Medicine. 1996; 71 (11):1139. [ PubMed ] [ Google Scholar ]
- Jansen ACM, van Aalst-Cohen ES, Hutten BA, Buller HR, Kastelein JJP, Prins MH. Guidelines were developed for data collection from medical records for use in retrospective analyses. Journal of Clinical Epidemiology. 2005; 58 :268–274. [ PubMed ] [ Google Scholar ]
- Jasperse DM, Ahmed SW. The mid-Atlantic oncology program’s comparison of two data collection methods. Control Clinical Trials. 1989; 10 :282–289. [ PubMed ] [ Google Scholar ]
- Krikorian J. Quality control enhanced by chart review. Hospitals. 1979; 53 (21):97–98. [ PubMed ] [ Google Scholar ]
- Lydiard RB. Problems with reports of preliminary results. American Journal of Psychiatry. 1991; 148 (5):686. [ PubMed ] [ Google Scholar ]
- Marchand WR, Wirth L, Simon C. Quetiapine adjunctive and monotherapy for pediatric bipolar disorder: A retrospective chart review. Journal of Child and Adolescent Psychopharmacology. 2004; 14 (3):405–411. [ PubMed ] [ Google Scholar ]
- Neidich B. A method to facilitate student interest in research: Chart Review. Journal of Nursing Education. 1990; 29 (3):139–140. [ PubMed ] [ Google Scholar ]
- Pan L, Fergusson D, Schweitzer I, Hebert PC. Ensuring high accuracy of data abstracted from patient charts: The use of a standardized medical record as a training tool. Journal of Clinical Epidemiology. 2005; 58 (9):918–923. [ PubMed ] [ Google Scholar ]
- Perry SE. Appropriate use of pilot studies. Journal of Nursing Scholarship. 2001; 33 (2):107. [ PubMed ] [ Google Scholar ]
- Preen DB, Holman CD, Lawrence DM, Baynham NJ, Semmens JB. Hospital chart review provided more accurate comorbidity information than data from a general practitioner survey or an administrative database. Journal of Clinical Epidemiology. 2004; 57 (12):1295–1304. [ PubMed ] [ Google Scholar ]
- Prescott PA, Soeken KL. The potential uses of pilot work. Nursing Research. 1989; 38 (1):60–62. [ PubMed ] [ Google Scholar ]
- Rajeev J, Srinath S, Girimaji S, Seshadri S, Singh P. A systematic chart review of the naturalistic course and treatment of early-onset bipolar disorder in a child and adolescent psychiatry center. Comprehensive Psychiatry. 2004; 45 (2):148–154. [ PubMed ] [ Google Scholar ]
- Raykov T, Wideman KF. Issues in applied equation modeling research. Structural Equation Modeling. 1995; 2 :289–318. [ Google Scholar ]
- Rosen B. Fundamentals of biostatics. Belmont, CA: Wadsworth Publishing Company; 1995. [ Google Scholar ]
- Sackett DL, Haynes RB, Guyatt GH, Tugwell P. Clinical epidemiology: A basic science for clinical medicine. Boston, MA: Little, Brown & Company; 1991. [ Google Scholar ]
- Smith AJ. Chart reviews made simple. Nursing Management. 1996; 27 (8):33–34. [ PubMed ] [ Google Scholar ]
- Staller JA. Intramuscular ziprasidone in youth: A retrospective chart review. Journal of Child and Adolescent Psychopharmacology. 2004; 14 (3):590–592. [ PubMed ] [ Google Scholar ]
- Staller JA, Kunwar A, Simionescu M. Oxcarbazepine in the treatment of child psychiatric disorders: A retrospective chart review. Journal of Child and Adolescent Psychopharmacology. 2005; 15 (6):964–969. [ PubMed ] [ Google Scholar ]
- Thompson JW, Spier S. Quality of the psychiatric literature. American Journal of Psychiatry. 1989; 146 (11):1517. [ PubMed ] [ Google Scholar ]
- Van Teijlingen E, Hundley V. The Importance of Pilot Studies. Nursing Standard. 2002; 16 (4):33–36. [ PubMed ] [ Google Scholar ]
- VonKoss Krowchuk H, Moore ML, Richardson L. Using health records as sources of data for research. Journal of Nursing Measurements. 1995; 3 (1):3–12. [ PubMed ] [ Google Scholar ]
- Woogh C. Is schizophrenia on the decline in Canada? Canadian Journal of Psychiatry. 2001; 46 :61–67. [ PubMed ] [ Google Scholar ]
- Worster A, Haines T. Advanced statistics: Understanding medical record review (MRR) studies. Academic Emergency Medicine. 2004; 11 (2):187–192. [ PubMed ] [ Google Scholar ]
- Wu L, Ashton CM. Chart Review: A need for Reappraisal. Evaluation and Health Professions. 1997; 20 (2):145–163. [ PubMed ] [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
Retrospective studies are observational studies by necessity because they assess past events and it is impossible to perform a randomized, controlled experiment with them. However, they can be quicker and cheaper to complete, making them a good choice for preliminary research. Findings from a retrospective study can help inform a prospective ...
Materials and Methods. We analyzed the data requirements of over 100 retrospective studies by mapping the selection criteria and study variables to data elements of two standard data dictionaries, one from the healthcare domain and the other from the clinical research domain. We also contacted study authors to validate our results.
A retrospective cohort study is a type of observational study that focuses on individuals who have an exposure to a disease or risk factor in common. Retrospective cohort studies analyze the health outcomes over a period of time to form connections and assess the risk of a given outcome associated with a given exposure. Note.
The study design used to answer a particular research question depends on the nature of the question and the availability of resources. In this article, which is the first part of a series on "study designs," we provide an overview of research study designs and their classification. The subsequent articles will focus on individual designs.
A retrospective study (by definition non-interventional) is a purely observational review and/or reassessment of database records with the aim of analyzing previous events of interest. The ethical and scientific standards for conducting biomedical research ...
One distinctive strength of observational studies-which are sometimes but not always retrospective-is the ability to obtain a large corpus of data from medical databases rapidly, as sometimes warranted by pressing health care policy and practice issues. Conclusion: Retrospective studies, often considered inferior to prospective, randomized, and ...
Here we provide 10 rules that serve as an end-to-end introduction to retrospective analyses of observational health care data. A running example of a COVID-19 study presents a practical implementation of each rule in the context of a specific treatment hypothesis.
Purpose. A first objective was to provide an overview of advantages and cautions around so-called retrospective clinical studies. A second objective was to provide guidelines for strong studies that can make a valid contribution to the clinical literature, whether these studies are prospective, retrospective, experimental, or observational.
A retrospective cohort study is a type of observational study that focuses on individuals who have an exposure to a disease or risk factor in common. Retrospective cohort studies analyse the health outcomes over a period of time to form connections and assess the risk of a given outcome associated with a given exposure. Retrospective cohort ...
It is the general experience of society that a rapid response to critical health situations can be key, and this requires sound scientific research and credible and complete data (Del Rio and Malani 2020, pp. 1339-1340). In this environment, retrospective research that uses data, including personal health data, previously provided for other ...
The rupture risk factors of mirror intracranial aneurysms: A systematic review and meta-analysis based on morphological and hemodynamic parameters. Huang Yong-Wei, Xiao-Yi Wang, Zong-Ping Li, Xiao-Shuang Yin. Propensity score-matched analysis of physician-controlled wire-guided cannulation as an effective technique against difficult cannulation ...
Retrospective Studies*. A thorough understanding of the pros and cons of the various study designs is critical to correct interpretation of their results. Retrospective studies are an important tool to study rare diseases, manifestations and outcomes. Findings of these studies can form the basis on which prospective studie ….
Limitations. Examples. FAQs. A retrospective study, sometimes called a historical cohort study, is a type of longitudinal study in which researchers look back to a certain point to analyze a particular group of subjects who have already experienced an outcome of interest. In a retrospective cohort study, the researcher identifies a group of ...
A retrospective study uses existing data that have been recorded for reasons other than research. A retrospective case series is the description of a group of cases with a new or unusual disease or treatment. With a case-control study, cases with and without the condition of interest are identified, …
Abstract. Looking back at 50 years of Journal of Consumer Research methods and interviewing some of the field's most respected methodologists, this article seeks to craft a core set of best practices for scholars in consumer research. From perennial issues like conceptual validity to emerging issues like data integrity and replicability, the advice offered by our experts can help scholars ...
The retrospective chart review (RCR), also known as a medical record review, is a type of research design in which pre-recorded, patient-centered data are used to answer one or more research questions [ 1 ]. The data used in such reviews exist in many forms: electronic databases, results from diagnostic tests, and notes from health service ...
A retrospective cohort study, also called a historic cohort study, is a longitudinal cohort study used in medical and psychological research. A cohort of individuals that share a common exposure factor is compared with another group of equivalent individuals not exposed to that factor, to determine the factor's influence on the incidence of a ...
Retrospective research is conducted on already available data and/or biologic material. Whether such research requires that patients specifically consent to the use of "their" data continues to stir controversy. From a legal and ethical point of view, it depends on several factors. The main criteria to be considered are whether the data or the ...
A retrospective study is an analysis that compares two groups of individuals. A case group and a control group. Both groups are similar, but the case group has a key factor that is being studied or investigated that the control group does not. It brings up key differences in individuals or groups of individuals based on some events/incidences.
Retrospective research, a component of health economics and outcomes research (HEOR), is needed throughout the product lifecycle to determine, demonstrate, and subsequently communicate the value of a product. Bringing together a unique and proven blend of deep therapeutic area domain expertise, scientific rigor, operational excellence, and access to unparalleled data assets, IQVIA can deliver ...
A retrospective study is one in which you look backwards at data that have already been collected or generated, to answer a scientific (usually medical) problem. Prospective studies are generally regarded as cleaner and more reliable, due to several shortcomings of retrospective studies: Some prospective studies have retrospective aspects.
Background It remains unclear whether additional fluid supplementation is necessary during the acute resuscitation period for patients with combined inhalational injury (INHI) under the guidance of the Third Military Medical University (TMMU) protocol. Methods A 10-year multicenter, retrospective cohort study, involved patients with burns ≥ 50% total burn surface area (TBSA) was conducted ...
Background The Enhanced Recovery After Surgery (ERAS) Society recommends that after total knee arthroplasty (TKA), patients should be mobilized early. However, there is no consensus on how early physical therapy should be commenced. We aim to investigate whether ultra-early physical therapy (< 12 h postoperatively) leads to better outcomes. Methods This is a retrospective cohort study of 569 ...
Retrospective research is conducted on already available data and/or biologic material. Whether such research requires that patients specifically consent to the use of "their" data continues to stir controversy. From a legal and ethical point of view, it depends on several factors. The main criteria to be considered are whether the data or the ...
Retrospective designs provide a vehicle for research using existing data but can be riddled with threats to both internal and external validity. Although a cause-and-effect relationship cannot be determined using retrospective studies, they are useful for providing preliminary data and in guiding the development of future prospective studies.
The association between objective imaging response and first line immune checkpoint inhibitor (ICI) therapy regimes in advanced melanoma remains uncharacterized in routine practice.We conducted a multi-center retrospective cohort analysis of advanced melanoma patients receiving first line ICI therapy from August 2013-May 2020 in Alberta, Canada.
Journal of Obstetrics and Gynaecology Research is a leading OBGYN journal publishing original research, case reports and reviews in obstetrics and gynecology. Abstract Aim In this study, we aimed to investigate patient characteristics, efficacy, prognostic factors, and safety of olaparib maintenance therapy for platinum-sensitive recurrent ...
The exhibit is a significant event for Lasch — a research professor of Art, Art History & Visual Studies — and the first retrospective of his career. Lasch has been teaching at Duke since 2002 and a practicing artist for over 30 years, producing both studio art and immersive community projects.
Background. Retrospective research often requires the analysis of data that were originally collected for reasons other than research (Hess, 2004; Jansen et al., 2005).This includes physician and nursing notes, ambulatory and emergency room reports, consultations, admission and discharge documentation, laboratory and diagnostic testing reports, and other clinical or administrative data.
Yes The details of the IRB/oversight body that provided approval or exemption for the research described are given below: The 5FU study (protocol-No: CESAR C-II-005, EudraCT-No; 2008-001515-37) with retrospective nature which was approved on 26.05.2008 by the ethics committee of the Albert-Ludwigs-Universitaet Freiburg, Freiburg, Germany.