
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- < Back To Research Topics

Coronary Heart Disease Research
Language switcher.
For almost 75 years, the NHLBI has been at the forefront of improving the nation’s health and reducing the burden of heart and vascular diseases . Heart disease, including coronary heart disease, remains the leading cause of death in the United States. However, the rate of heart disease deaths has declined by 70% over the past 50 years, thanks in part to NHLBI-funded research. Many current studies funded by the NHLBI focus on discovering genetic associations and finding new ways to prevent and treat the onset of coronary heart disease and associated medical conditions.
NHLBI research that really made a difference
The NHLBI supports a wide range of long-term studies to understand the risk factors of coronary heart disease. These ongoing studies, among others, have led to many discoveries that have increased our understanding of the causes of cardiovascular disease among different populations, helping to shape evidence-based clinical practice guidelines.
- Risk factors that can be changed: The NHLBI Framingham Heart Study (FHS) revealed that cardiovascular disease is caused by modifiable risk factors such as smoking, high blood pressure , obesity , high cholesterol levels, and physical inactivity. It is why, in routine physicals, healthcare providers check for high blood pressure, high cholesterol, unhealthy eating patterns, smoking, physical inactivity, and unhealthy weight. The FHS found that cigarette smoking increases the risk of heart disease. Researchers also showed that cardiovascular disease can affect people differently depending on sex or race, underscoring the need to address health disparities.
- Risk factors for Hispanic/Latino adults: The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) found that heart disease risk factors are widespread among Hispanic/Latino adults in the United States , with 80% of men and 71% of women having at least one risk factor. Researchers also used HCHS/SOL genetic data to explore genes linked with central adiposity (the tendency to have excess body fat around the waist) in Hispanic/Latino adults. Before this study, genes linked with central adiposity, a risk factor for coronary heart disease, had been identified in people of European ancestry. These results showed that those genes also predict central adiposity for Hispanic/Latino communities. Some of the genes identified were more common among people with Mexican or Central/South American ancestry, while others were more common among people of Caribbean ancestry.
- Risk factors for African Americans: The Jackson Heart Study (JHS) began in 1997 and includes more than 5,300 African American men and women in Jackson, Mississippi. It has studied genetic and environmental factors that raise the risk of heart problems, especially high blood pressure, coronary heart disease, heart failure , stroke , and peripheral artery disease (PAD) . Researchers discovered a gene variant in African American individuals that doubles the risk of heart disease. They also found that even small spikes in blood pressure can lead to a higher risk of death. A community engagement component of the JHS is putting 20 years of the study’s findings into action by turning traditional gathering places, such as barbershops and churches, into health information hubs.
- Risk factors for American Indians: The NHLBI actively supports the Strong Heart Study , a long-term study that began in 1988 to examine cardiovascular disease and its risk factors among American Indian men and women. The Strong Heart Study is one of the largest epidemiological studies of American Indian people ever undertaken. It involves a partnership with 12 Tribal Nations and has followed more than 8,000 participants, many of whom live in low-income rural areas of Arizona, Oklahoma, and the Dakotas. Cardiovascular disease remains the leading cause of death for American Indian people. Yet the prevalence and severity of cardiovascular disease among American Indian people has been challenging to study because of the small sizes of the communities, as well as the relatively young age, cultural diversity, and wide geographic distribution of the population. In 2019, the NHLBI renewed its commitment to the Strong Heart Study with a new study phase that includes more funding for community-driven pilot projects and a continued emphasis on training and development. Read more about the goals and key findings of the Strong Heart Study.
Current research funded by the NHLBI
Within our Division of Cardiovascular Sciences , the Atherothrombosis and Coronary Artery Disease Branch of its Adult and Pediatric Cardiac Research Program and the Center for Translation Research and Implementation Science oversee much of our funded research on coronary heart disease.
Research funding
Find funding opportunities and program contacts for research on coronary heart disease.
Current research on preventing coronary heart disease
- Blood cholesterol and coronary heart disease: The NHLBI supports new research into lowering the risk of coronary heart disease by reducing levels of cholesterol in the blood. High levels of blood cholesterol, especially a type called low-density lipoprotein (LDL) cholesterol, raise the risk of coronary heart disease. However, even with medicine that lowers LDL cholesterol, there is still a risk of coronary heart disease due to other proteins, called triglyceride-rich ApoB-containing lipoproteins (ApoBCLs), that circulate in the blood. Researchers are working to find innovative ways to reduce the levels of ApoBCLs, which may help prevent coronary heart disease and other cardiovascular conditions.
- Pregnancy, preeclampsia, and coronary heart disease risk: NHLBI-supported researchers are investigating the link between developing preeclampsia during pregnancy and an increased risk for heart disease over the lifespan . This project uses “omics” data – such as genomics, proteomics, and other research areas – from three different cohorts of women to define and assess preeclampsia biomarkers associated with cardiovascular health outcomes. Researchers have determined that high blood pressure during pregnancy and low birth weight are predictors of atherosclerotic cardiovascular disease in women . Ultimately, these findings can inform new preventive strategies to lower the risk of coronary heart disease.
- Community-level efforts to lower heart disease risk among African American people: The NHLBI is funding initiatives to partner with churches in order to engage with African American communities and lower disparities in heart health . Studies have found that church-led interventions reduce risk factors for coronary heart disease and other cardiovascular conditions. NHLBI-supported researchers assessed data from more than 17,000 participants across multiple studies and determined that these community-based approaches are effective in lowering heart disease risk factors .
Find more NHLBI-funded studies on preventing coronary heart disease on the NIH RePORTER.

Learn about the impact of COVID-19 on your risk of coronary heart disease.
Current research on understanding the causes of coronary heart disease
- Pregnancy and long-term heart disease: NHLBI researchers are continuing the Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-be (nuMoM2b) study to understand the relationship between pregnancy-related problems, such as gestational hypertension, and heart problems. The study also looks at how problems during pregnancy may increase risk factors for heart disease later in life. NuMoM2b launched in 2010, and long-term studies are ongoing, with the goal of collecting high-quality data and understanding how heart disease develops in women after pregnancy.
- How coronary artery disease affects heart attack risk: NHLBI-funded researchers are investigating why some people with coronary artery disease are more at risk for heart attacks than others. Researchers have found that people with coronary artery disease who have high-risk coronary plaques are more likely to have serious cardiac events, including heart attacks. However, we do not know why some people develop high-risk coronary plaques and others do not. Researchers hope that this study will help providers better identify which people are most at risk of heart attacks before they occur.
- Genetics of coronary heart disease: The NHLBI supports studies to identify genetic variants associated with coronary heart disease . Researchers are investigating how genes affect important molecular cascades involved in the development of coronary heart disease . This deeper understanding of the underlying causes for plaque buildup and damage to the blood vessels can inform prevention strategies and help healthcare providers develop personalized treatment for people with coronary heart disease caused by specific genetic mutations.
Find more NHLBI-funded studies on understanding the causes of coronary heart disease on the NIH RePORTER.

Recent findings suggest that cholesterol-lowering treatment can lower the risk of heart disease complications in people with HIV.
Current research on treatments for coronary heart disease
- Insight into new molecular targets for treatment: NHLBI-supported researchers are investigating the role of high-density lipoprotein (HDL) cholesterol in coronary heart disease and other medical conditions . Understanding how the molecular pathways of cholesterol affect the disease mechanism for atherosclerosis and plaque buildup in the blood vessels of the heart can lead to new therapeutic approaches for the treatment of coronary heart disease. Researchers have found evidence that treatments that boost HDL function can lower systemic inflammation and slow down plaque buildup . This mechanism could be targeted to develop a new treatment approach for coronary heart disease.
- Long-term studies of treatment effectiveness: The NHLBI is supporting the International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial EXTENDed Follow-up (EXTEND) , which compares the long-term outcomes of an initial invasive versus conservative strategy for more than 5,000 surviving participants of the original ISCHEMIA trial. Researchers have found no difference in mortality outcomes between invasive and conservative management strategies for patients with chronic coronary heart disease after more than 3 years. They will continue to follow up with participants for up to 10 years. Researchers are also assessing the impact of nonfatal events on long-term heart disease and mortality. A more accurate heart disease risk score will be constructed to help healthcare providers deliver more precise care for their patients.
- Evaluating a new therapy for protecting new mothers: The NHLBI is supporting the Randomized Evaluation of Bromocriptine In Myocardial Recovery Therapy for Peripartum Cardiomyopathy (REBIRTH) , for determining the role of bromocriptine as a treatment for peripartum cardiomyopathy (PPCM). Previous research suggests that prolactin, a hormone that stimulates the production of milk for breastfeeding, may contribute to the development of cardiomyopathy late in pregnancy or the first several months postpartum. Bromocriptine, once commonly used in the United States to stop milk production, has shown promising results in studies conducted in South Africa and Germany. Researchers will enroll approximately 200 women across North America who have been diagnosed with PPCM and assess their heart function after 6 months.
- Impact of mental health on response to treatment: NHLBI-supported researchers are investigating how mental health conditions can affect treatment effectiveness for people with coronary heart disease. Studies show that depression is linked to a higher risk for negative outcomes from coronary heart disease. Researchers found that having depression is associated with poor adherence to medical treatment for coronary heart disease . This means that people with depression are less likely to follow through with their heart disease treatment plans, possibly contributing to their chances of experiencing worse outcomes. Researchers are also studying new ways to treat depression in patients with coronary heart disease .
Find more NHLBI-funded studies on treating coronary heart disease on the NIH RePORTER.

Researchers have found no clear difference in patient survival or heart attack risk between managing heart disease through medication and lifestyle changes compared with invasive procedures.
Coronary heart disease research labs at the NHLBI
- Laboratory of Cardiac Physiology
- Laboratory of Cardiovascular Biology
- Minority Health and Health Disparities Population Laboratory
- Social Determinants of Obesity and Cardiovascular Risk Laboratory
- Laboratory for Cardiovascular Epidemiology and Genomics
- Laboratory for Hemostasis and Platelet Biology
Related coronary heart disease programs
- In 2002, the NHLBI launched The Heart Truth® , the first federally sponsored national health education program designed to raise awareness about heart disease as the leading cause of death in women. The NHLBI and The Heart Truth® supported the creation of the Red Dress® as the national symbol for awareness about women and heart disease, and also coordinate National Wear Red Day ® and American Heart Month each February.
- The Biologic Specimen and Data Repository Information Coordinating Center (BioLINCC) facilitates access to and maximizes the scientific value of NHLBI biospecimen and data collections. A main goal is to promote the use of these scientific resources by the broader research community. BioLINCC serves to coordinate searches across data and biospecimen collections and provide an electronic means for requesting additional information and submitting requests for collections. Researchers wanting to submit biospecimen collections to the NHLBI Biorepository to share with qualified investigators may also use the website to initiate the application process.
- Our Trans-Omics for Precision Medicine (TOPMed) Program studies the ways genetic information, along with information about health status, lifestyle, and the environment, can be used to predict the best ways to prevent and treat heart, lung, blood, and sleep disorders. TOPMed specifically supports NHLBI’s Precision Medicine Activities.
- NHLBI population and epidemiology studies in different groups of people, including the Atherosclerosis Risk in Communities (ARIC) Study , the Multi-Ethnic Study of Atherosclerosis (MESA) , and the Cardiovascular Health Study (CHS) , have made major contributions to understanding the causes and prevention of heart and vascular diseases, including coronary heart disease.
- The Cardiothoracic Surgical Trials Network (CTSN) is an international clinical research enterprise that studies heart valve disease , arrhythmias , heart failure, coronary heart disease, and surgical complications. The trials span all phases of development, from early translation to completion, and have more than 14,000 participants. The trials include six completed randomized clinical trials, three large observational studies, and many other smaller studies.

Learn how heart disease may be different for women than for men.
Explore more NHLBI research on coronary heart disease
The sections above provide you with the highlights of NHLBI-supported research on coronary heart disease. You can explore the full list of NHLBI-funded studies on the NIH RePORTER .
To find more studies:
- Type your search words into the Quick Search box and press enter.
- Check Active Projects if you want current research.
- Select the Agencies arrow, then the NIH arrow, then check NHLBI .
If you want to sort the projects by budget size — from the biggest to the smallest — click on the FY Total Cost by IC column heading.
- Patient Care & Health Information
- Diseases & Conditions
- Coronary artery disease
Coronary artery disease is a common heart condition. The major blood vessels that supply the heart (coronary arteries) struggle to send enough blood, oxygen and nutrients to the heart muscle. Cholesterol deposits (plaques) in the heart arteries and inflammation are usually the cause of coronary artery disease.
Signs and symptoms of coronary artery disease occur when the heart doesn't get enough oxygen-rich blood. If you have coronary artery disease, reduced blood flow to the heart can cause chest pain (angina) and shortness of breath. A complete blockage of blood flow can cause a heart attack.
Coronary artery disease often develops over decades. Symptoms may go unnoticed until a significant blockage causes problems or a heart attack occurs. Following a heart-healthy lifestyle can help prevent coronary artery disease.
Coronary artery disease may also be called coronary heart disease.
- What is coronary artery disease? A Mayo Clinic cardiologist explains.
Stephen Kopecky, M.D., talks about the risk factors, symptoms and treatment of coronary artery disease (CAD). Learn how lifestyle changes can lower your risk.
{Music playing}
Stephen Kopecky, M.D., Cardiovascular Disease, Mayo Clinic: I'm Dr. Stephen Kopecky, a cardiologist at Mayo Clinic. In this video, we'll cover the basics of coronary artery disease. What is it? Who gets it? The symptoms, diagnosis and treatment. Whether you're looking for answers for yourself or someone you love, we're here to give you the best information available.
Coronary artery disease, also called CAD, is a condition that affects your heart. It is the most common heart disease in the United States. CAD happens when coronary arteries struggle to supply the heart with enough blood, oxygen and nutrients. Cholesterol deposits, or plaques, are almost always to blame. These buildups narrow your arteries, decreasing blood flow to your heart. This can cause chest pain, shortness of breath or even a heart attack. CAD typically takes a long time to develop. So often, patients don't know that they have it until there's a problem. But there are ways to prevent coronary artery disease, and ways to know if you're at risk and ways to treat it.
Who gets it?
Anyone can develop CAD . It begins when fats, cholesterols and other substances gather along the walls of your arteries. This process is called atherosclerosis. It's typically no cause for concern. However, too much buildup can lead to a blockage, obstructing blood flow. There are a number of risk factors, common red flags, that can contribute to this and ultimately lead to coronary artery disease. First, getting older can mean more damaged and narrowed arteries. Second, men are generally at a greater risk. But the risk for women increases after menopause. Existing health conditions matter, too. High blood pressure can thicken your arteries, narrowing your blood flow. High cholesterol levels can increase the rate of plaque buildup. Diabetes is also associated with higher risk, as is being overweight. Your lifestyle plays a large role as well. Physical inactivity, long periods of unrelieved stress in your life, an unhealthy diet and smoking can all increase your risk. And finally, family history. If a close relative was diagnosed at an early age with heart disease, you're at a greater risk. All these factors together can paint a picture of your risk for developing CAD .
What are the symptoms?
When coronary arteries become narrow, the heart doesn't get enough oxygen-rich blood. Remember, unlike most pumps, the heart has to pump its own energy supply. It's working harder with less. And you may begin to notice these signs and symptoms of pressure or tightness in your chest. This pain is called angina. It may feel like somebody is standing on your chest. When your heart can't pump enough blood to meet your body's needs, you might develop shortness of breath or extreme fatigue during activities. And if an artery becomes totally blocked, it leads to a heart attack. Classic signs and symptoms of a heart attack include crushing, substernal chest pain, pain in your shoulders or arms, shortness of breath, and sweating. However, many heart attacks have minimal or no symptoms and are found later during routine testing.
How is it diagnosed?
Diagnosing CAD starts by talking to your doctor. They'll be able to look at your medical history, do a physical exam and order routine blood work. Depending on that, they may suggest one or more of the following tests: an electrocardiogram or ECG, an echocardiogram or soundwave test of the heart, stress test, cardiac catheterization and angiogram, or a cardiac CT scan.
How is it treated?
Treating coronary artery disease usually means making changes to your lifestyle. This might be eating healthier foods, exercising regularly, losing excess weight, reducing stress or quitting smoking. The good news is these changes can do a lot to improve your outlook. Living a healthier life translates to having healthier arteries. When necessary, treatment could involve drugs like aspirin, cholesterol-modifying medications, beta-blockers, or certain medical procedures like angioplasty or coronary artery bypass surgery.
Discovering you have coronary artery disease can be overwhelming. But be encouraged. There are things you can do to manage and live with this condition. Reducing cholesterol, lowering blood pressure, quitting tobacco, eating healthier, exercising and managing your stress can make a world of difference. Better heart health starts by educating yourself. So don't be afraid to seek out information and ask your doctors about coronary artery disease. If you'd like to learn even more about this condition, watch our other related videos or visit Mayoclinic.org. We wish you well.
Symptoms may go unrecognized at first, or they may only occur when the heart is beating hard like during exercise. As the coronary arteries continue to narrow, less and less blood gets to the heart and symptoms can become more severe or frequent.
Coronary artery disease signs and symptoms can include:
- Chest pain (angina). You may feel pressure or tightness in your chest. Some people say it feels like someone is standing on their chest. The chest pain usually occurs on the middle or left side of the chest. Activity or strong emotions can trigger angina. The pain usually goes away within minutes after the triggering event ends. In some people, especially women, the pain may be brief or sharp and felt in the neck, arm or back.
- Shortness of breath. You may feel like you can't catch your breath.
- Fatigue. If the heart can't pump enough blood to meet your body's needs, you may feel unusually tired.
- Heart attack. A completely blocked coronary artery will cause a heart attack. The classic signs and symptoms of a heart attack include crushing chest pain or pressure, shoulder or arm pain, shortness of breath, and sweating. Women may have less typical symptoms, such as neck or jaw pain, nausea and fatigue. Some heart attacks don't cause any noticeable signs or symptoms.
When to see a doctor
If you think you're having a heart attack, immediately call 911 or your local emergency number. If you don't have access to emergency medical services, have someone drive you to the nearest hospital. Drive yourself only as a last option.
Smoking or having high blood pressure, high cholesterol, diabetes, obesity or a strong family history of heart disease makes you more likely to get coronary artery disease. If you're at high risk of coronary artery disease, talk to your health care provider. You may need tests to check for narrowed arteries and coronary artery disease.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
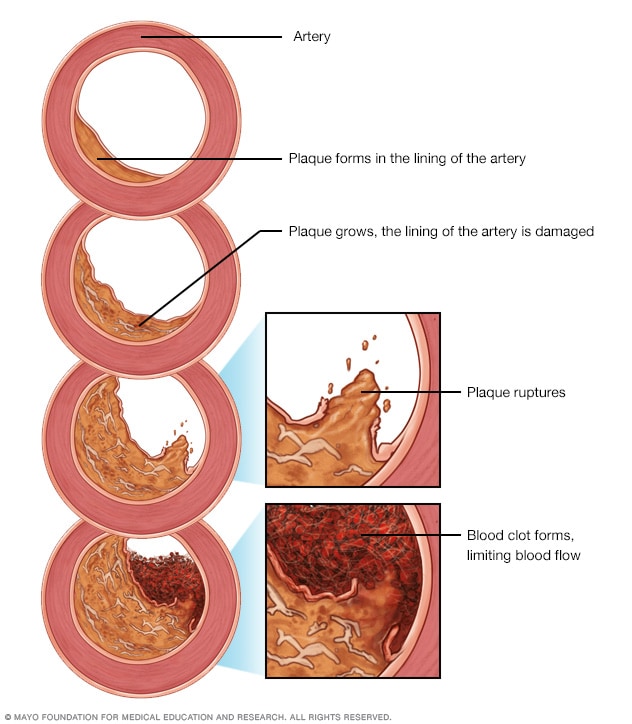
Development of atherosclerosis
If there's too much cholesterol in the blood, the cholesterol and other substances may form deposits called plaque. Plaque can cause an artery to become narrowed or blocked. If a plaque ruptures, a blood clot can form. Plaque and blood clots can reduce blood flow through an artery.
Coronary artery disease starts when fats, cholesterols and other substances collect on the inner walls of the heart arteries. This condition is called atherosclerosis. The buildup is called plaque. Plaque can cause the arteries to narrow, blocking blood flow. The plaque can also burst, leading to a blood clot.
Besides high cholesterol, damage to the coronary arteries may be caused by:
- Diabetes or insulin resistance
- High blood pressure
- Not getting enough exercise (sedentary lifestyle)
- Smoking or tobacco use
Risk factors
Coronary artery disease is common. Age, genetics, other health conditions and lifestyle choices can affect the health of the heart arteries.
Coronary artery disease risk factors include:
- Age. Getting older increases the risk of damaged and narrowed arteries.
- Sex. Men are generally at greater risk of coronary artery disease. However, the risk for women increases after menopause.
- Family history. A family history of heart disease makes you more likely to get coronary artery disease. This is especially true if a close relative (parent, sibling) developed heart disease at an early age. The risk is highest if your father or a brother had heart disease before age 55 or if your mother or a sister developed it before age 65.
- Smoking. If you smoke, quit. Smoking is bad for heart health. People who smoke have a significantly increased risk of heart disease. Breathing in secondhand smoke also increases the risk.
- High blood pressure. Uncontrolled high blood pressure can make arteries hard and stiff (arterial stiffness). The coronary arteries may become narrow, slowing blood flow.
- High cholesterol. Too much bad cholesterol in the blood can increase the risk of atherosclerosis. Bad cholesterol is called low-density lipoprotein (LDL) cholesterol. Not enough good cholesterol — called high-density lipoprotein (HDL) — also leads to atherosclerosis.
- Diabetes. Diabetes increases the risk of coronary artery disease. Type 2 diabetes and coronary artery disease share some risk factors, such as obesity and high blood pressure.
- Overweight or obesity. Excess body weight is bad for overall health. Obesity can lead to type 2 diabetes and high blood pressure. Ask your health care provider what a healthy weight is for you.
- Chronic kidney disease. Having long-term kidney disease increases the risk of coronary artery disease.
- Not getting enough exercise. Physical activity is important for good health. A lack of exercise (sedentary lifestyle) is linked to coronary artery disease and some of its risk factors.
- A lot of stress. Emotional stress may damage the arteries and worsen other risk factors for coronary artery disease.
- Unhealthy diet. Eating foods with a lot of saturated fat, trans fat, salt and sugar can increase the risk of coronary artery disease.
- Alcohol use. Heavy alcohol use can lead to heart muscle damage. It can also worsen other risk factors of coronary artery disease.
- Amount of sleep. Too little and too much sleep have both been linked to an increased risk of heart disease.
Risk factors often occur together. One risk factor may trigger another.
When grouped together, certain risk factors make you even more likely to develop coronary artery disease. For example, metabolic syndrome — a cluster of conditions that includes high blood pressure, high blood sugar, excess body fat around the waist and high triglyceride levels — increases the risk of coronary artery disease.
Sometimes coronary artery disease develops without any classic risk factors. Other possible risk factors for coronary artery disease may include:
- Breathing pauses during sleep (obstructive sleep apnea). This condition causes breathing to stop and start during sleep. It can cause sudden drops in blood oxygen levels. The heart must work harder. Blood pressure goes up.
- High-sensitivity C-reactive protein (hs-CRP). This protein appears in higher-than-usual amounts when there's inflammation somewhere in the body. High hs-CRP levels may be a risk factor for heart disease. It's thought that as coronary arteries narrow, the level of hs-CRP in the blood goes up.
- High triglycerides. This is a type of fat (lipid) in the blood. High levels may raise the risk of coronary artery disease, especially for women.
- Homocysteine. Homocysteine is an amino acid the body uses to make protein and to build and maintain tissue. But high levels of homocysteine may increase the risk of coronary artery disease.
- Preeclampsia. This pregnancy complication causes high blood pressure and increased protein in the urine. It can lead to a higher risk of heart disease later in life.
- Other pregnancy complications. Diabetes or high blood pressure during pregnancy are also known risk factors for coronary artery disease.
- Certain autoimmune diseases. People who have conditions such as rheumatoid arthritis and lupus (and other inflammatory conditions) have an increased risk of atherosclerosis.
Complications
Coronary artery disease can lead to:
- Chest pain (angina). When the coronary arteries narrow, the heart may not get enough blood when it needs it most — like when exercising. This can cause chest pain (angina) or shortness of breath.
- Heart attack. A heart attack can happen if a cholesterol plaque breaks open and causes a blood clot to form. A clot can block blood flow. The lack of blood can damage the heart muscle. The amount of damage depends in part on how quickly you are treated.
- Heart failure. Narrowed arteries in the heart or high blood pressure can slowly make the heart weak or stiff so it's harder to pump blood. Heart failure is when the heart doesn't pump blood as it should.
- Irregular heart rhythms (arrhythmias). Not enough blood to the heart can alter normal heart signaling, causing irregular heartbeats.
The same lifestyle habits used to help treat coronary artery disease can also help prevent it. A healthy lifestyle can help keep the arteries strong and clear of plaque. To improve heart health, follow these tips:
- Quit smoking.
- Control high blood pressure, high cholesterol and diabetes.
- Exercise often.
- Maintain a healthy weight.
- Eat a low-fat, low-salt diet that's rich in fruits, vegetables and whole grains.
- Reduce and manage stress.
Coronary artery disease care at Mayo Clinic
Living with coronary artery disease?
Connect with others like you for support and answers to your questions in the Heart & Blood Health support group on Mayo Clinic Connect, a patient community.
Heart & Blood Health Discussions

87 Replies Tue, May 14, 2024

130 Replies Mon, May 13, 2024

136 Replies Sun, May 12, 2024
- Ferri FF. Coronary artery disease. In: Ferri's Clinical Advisor 2022. Elsevier; 2022. https://www.clinicalkey.com. Accessed March 8, 2022.
- Coronary heart disease. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health-topics/coronary-heart-disease. March 8, 2022.
- Usatine RP, et al., eds. Coronary artery disease. In: Color Atlas and Synopsis of Heart Failure. McGraw Hill; 2019.
- Wilson PWF. Overview of the possible risk factors for cardiovascular disease. https://www.uptodate.com/contents/search. Accessed March 8, 2022.
- Masjedi MS, et al. Effects of flaxseed on blood lipids in healthy and dyslipidemic subjects: A systematic review and meta-analysis of randomized controlled trials. Current Problems in Cardiology. 2021; doi:10.1016/j.cpcardiol.2021.100931.
- Riaz H, et al. Association between obesity and cardiovascular outcomes: A systematic review and meta-analysis of mendelian randomization studies. JAMA Network Open. 2018; doi:10.1001/jamanetworkopen.2018.3788.
- Physical Activity Guidelines for Americans. 2nd ed. U.S. Department of Health and Human Services. https://health.gov/our-work/physical-activity/current-guidelines. Accessed March 8, 2022.
- Your guide to lowering your cholesterol with therapeutic lifestyle changes (TLC). National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health-topics/all-publications-and-resources/your-guide-lowering-cholesterol-therapeutic-lifestyle. Accessed March 24, 2022.
- Rethinking drinking. National Institute on Alcohol Abuse and Alcoholism. https://www.rethinkingdrinking.niaaa.nih.gov/. Accessed March 24, 2022.
- 2015-2020 Dietary Guidelines for Americans. U.S. Department of Health and Human Services and U.S. Department of Agriculture. https://health.gov/our-work/food-nutrition/2015-2020-dietary-guidelines/guidelines. Accessed March 24, 2022.
- Omega-3 supplements: In depth. National Center for Complementary and Integrative Health. https://www.nccih.nih.gov/health/omega3-supplements-in-depth. Accessed March 8, 2022.
- Mankad R (expert opinion). Mayo Clinic. April 28, 2020.
- Siscovick DS, et al. Omega-3 polyunsaturated fatty acid (fish oil) supplementation and the prevention of clinical cardiovascular disease: A science advisory from the American Heart Association. Circulation. 2017; doi:10.1161/CIR.0000000000000482.
- Barley. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed March 24, 2022.
- Black psyllium. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed March 24, 2022.
- Braswell-Pickering EA. Allscripts EPSi. Mayo Clinic. Feb. 10, 2022.
- Liao KP. Coronary artery disease in rheumatoid arthritis: Pathogenesis, risk factors, clinical manifestations, and diagnostic implications. https://www.uptodate.com/contents/search. Accessed March 8, 2022.
- What is coronary heart disease? National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health-topics/coronary-heart-disease Accessed March 8, 2022.
- Kannam JP, et al. Chronic coronary syndrome: Overview of care. https://www.uptodate.com/contents/search. Accessed March 8, 2022.
- Arnett DK, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019; doi:10.1161/CIR.0000000000000678.
- Aspirin use to prevent cardiovascular disease: Preventive medication. U.S. Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/uspstf/draft-recommendation/aspirin-use-to-prevent-cardiovascular-disease-preventive-medication. Accessed March 23, 2021.
- Zheng SL, et al. Association of aspirin use for primary prevention with cardiovascular events and bleeding events: A systematic review and meta-analysis. JAMA. 2019; doi:10.1001/jama.2018.20578.
- Cutlip D, et al. Revascularization in patients with stable coronary artery disease: Coronary artery bypass graft surgery versus percutaneous coronary intervention. https://www.uptodate.com/contents/search. Accessed March 24, 2022.
- Hypertension in Adults: Screening. U.S. Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/hypertension-in-adults-screening. Accessed March 24, 2022.
- How and when to have your cholesterol checked. U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/cholesterol/checked.htm. Accessed March 24, 2022.
- Blond psyllium. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed March 24, 2022.
- Oats. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed March 24, 2022.
- Garlic. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed March 24, 2022.
- Plant sterols. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed March 24, 2022.
- Ashraf H, et al. Use of flecainide in stable coronary artery disease: An analysis of its safety in both nonobstructive and obstructive coronary artery disease. American Journal of Cardiovascular Drugs. 2021; doi:10.1007/s40256-021-00483-9.
- Ono M, et al. 10-year follow-up after revascularization in elderly patients with complex coronary artery disease. Journal of the American College of Cardiology. 2021; doi:10.1016/j.jacc.2021.04.016.
- Coyle M, et al. A critical review of chronic kidney disease as a risk factor for coronary artery disease. International Journal of Cardiology: Heart & Vasculature. 2021; doi:10.1016/j.ijcha.2021.100822.
- Mankad R (expert opinion). Mayo Clinic. May 6, 2022.
- Angina treatment: Stents, drugs, lifestyle changes — What's best?
- Coronary artery disease FAQs
- Coronary artery disease: Angioplasty or bypass surgery?
- Coronary artery stent
- Drug-eluting stents
- Four Steps to Heart Health
Associated Procedures
- Cardiac catheterization
- Coronary angiogram
- Coronary angioplasty and stents
- Coronary artery bypass surgery
- Coronary calcium scan
- Echocardiogram
- Electrocardiogram (ECG or EKG)
- Stress test
News from Mayo Clinic
- Mayo Clinic Minute: Signs of coronary artery disease, how to reduce your risk Jan. 24, 2023, 04:15 p.m. CDT
- A History of Cancer, Coronary Artery Disease May Reduce Risk of Dementia Oct. 24, 2022, 02:45 p.m. CDT
Mayo Clinic in Rochester, Minnesota, has been recognized as one of the top Cardiology & Heart Surgery hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Overview of Coronary Artery Disease
- Pathophysiology |
- Risk Factors |
- Coronary Artery Anatomy |
- Treatment |
- Prevention |
Coronary artery disease (CAD) involves impairment of blood flow through the coronary arteries, most commonly by atheromas. Clinical presentations include silent ischemia, angina pectoris , acute coronary syndromes ( unstable angina , myocardial infarction ), and sudden cardiac death . Diagnosis is by symptoms, ECG, stress testing, and sometimes coronary angiography. Prevention consists of modifying reversible risk factors (eg, hypercholesterolemia, hypertension, physical inactivity, obesity, diabetes, smoking). Treatment includes medications and procedures to reduce ischemia and restore or improve coronary blood flow.
Coronary artery disease is the leading cause of death in both sexes, accounting for approximately one third of all deaths, and substantial numbers of these occur in low resource areas ( 1 ). Mortality from coronary artery disease is approximately 5 times higher in men than in women, but the mortality difference declines with age ( 2 ).
General references
1. Ralapanawa U, Sivakanesan R . Epidemiology and the Magnitude of Coronary Artery Disease and Acute Coronary Syndrome: A Narrative Review. J Epidemiol Glob Health 2021;11(2):169-177. doi:10.2991/jegh.k.201217.001
2. Bots SH, Peters SAE, Woodward M . Sex differences in coronary heart disease and stroke mortality: a global assessment of the effect of ageing between 1980 and 2010. BMJ Glob Health 2017;2(2):e000298. Published 2017 Mar 27. doi:10.1136/bmjgh-2017-000298
Etiology of Coronary Artery Disease
Usually, coronary artery disease is due to
Coronary artery atherosclerosis : Subintimal deposition of atheromas in large and medium-sized coronary arteries
Less often, coronary artery disease is due to
Coronary artery spasm (see Vasospastic Angina )
Vascular endothelial dysfunction can promote atherosclerosis and contribute to coronary artery spasm. Endothelial dysfunction is also recognized as a cause of angina in the absence of epicardial coronary artery stenosis or spasm (see Microvascular Angina ).
Rare causes include coronary artery embolism, dissection, aneurysm (eg, in Kawasaki disease ), and vasculitis (eg, in Takayasu arteritis ).
Pathophysiology of Coronary Artery Disease
Coronary atherosclerosis.
Coronary atherosclerosis is often irregularly distributed in different vessels but typically occurs at points of turbulence (eg, vessel bifurcations). As the atheromatous plaque grows, the arterial lumen progressively narrows, resulting in ischemia (often causing angina pectoris ). The degree of stenosis required to cause ischemia varies with oxygen demand.
Occasionally, an atheromatous plaque ruptures or splits. Reasons are unclear but probably relate to plaque morphology, plaque calcium content, and plaque softening due to an inflammatory process. Rupture exposes collagen and other thrombogenic material, which activate platelets and the coagulation cascade (see figure Pathways in Blood Coagulation ), resulting in an acute thrombus, which interrupts coronary blood flow and causes some degree of myocardial ischemia. The consequences of acute ischemia, collectively referred to as acute coronary syndromes (ACS), depend on the location and degree of obstruction and range from unstable angina, non–ST-segment elevation myocardial infarction (NSTEMI), to ST-segment elevation myocardial infarction (STEMI), which can result in transmural infarction, and other complications including malignant ventricular arrhythmias, conduction defects, heart failure, and sudden death.
Coronary artery spasm
Coronary artery spasm is a transient, focal increase in vascular tone, markedly narrowing the lumen and reducing blood flow; symptomatic ischemia ( vasospastic angina ) may result. Marked narrowing can trigger thrombus formation, causing infarction or life-threatening arrhythmia. Spasm can occur in arteries with or without atheroma.
In arteries without atheroma, basal coronary artery tone is probably increased, and response to vasoconstricting stimuli is probably exaggerated. The exact mechanism is unclear but may involve endothelial cell abnormalities of nitric oxide production or an imbalance between endothelium-derived contracting and relaxing factors.
In arteries with atheroma, the atheroma causes endothelial dysfunction, possibly resulting in local hypercontractility. Proposed mechanisms include loss of sensitivity to intrinsic vasodilators (eg, acetylcholine) and increased production of vasoconstrictors (eg, angiotensin II , endothelin, leukotrienes, serotonin, thromboxane) in the area of the atheroma. Recurrent spasm may damage the intima, leading to atheroma formation.
Use of vasoconstricting substances (eg, cocaine , nicotine ) and emotional stress also can trigger coronary spasm.
Coronary artery dissection
Coronary artery dissection is a rare, non-traumatic tear in the coronary intima with creation of a false lumen. Blood flowing through the false lumen expands it, which restricts blood flow through the true lumen sometimes causing coronary ischemia or infarction. Dissection may occur in atherosclerotic or non-atherosclerotic coronary arteries. Non-atherosclerotic dissection is more likely in pregnant or postpartum females and/or patients with fibromuscular dysplasia or other connective tissue disorders.
Risk Factors for Coronary Artery Disease
Risk factors for coronary artery disease are the same as risk factors for atherosclerosis :
Family history of early coronary artery disease (death from coronary artery disease in a first-degree relative prior to age 55 in males or age 65 in females)
High blood levels of low-density lipoprotein (LDL) cholesterol (see Dyslipidemia )
High blood levels of lipoprotein a
Low blood levels of high-density lipoprotein (HDL) cholesterol
Diabetes mellitus (particularly type 2)
Smoking (including secondhand exposure)
Physical inactivity
High level of apoprotein B (apo B)
High blood levels of C-reactive protein (CRP)
Smoking may be a stronger predictor of myocardial infarction in females ( 1 ). Genetic factors play a role, and several systemic disorders (eg, hypertension , hypothyroidism ) and metabolic disorders (eg, hyperhomocysteinemia ) contribute to risk. A high level of apo B may identify increased risk when total cholesterol or LDL level is normal ( 2, 3 ).
High blood levels of C-reactive protein indicate plaque instability and inflammation and may be a stronger predictor of risk of ischemic events than high levels of LDL ( 4 ). High blood levels of triglycerides and insulin (reflecting insulin resistance) may be risk factors, but data are less clear. CAD risk is also increased by a diet high in fat and calories and low in phytochemicals (found in fruits and vegetables), fiber, and vitamins C, D, and E; by a diet relatively low in omega-3 (n-3) polyunsaturated fatty acids (PUFAs—at least in some people); and by poor stress management.
Risk factor references
1. Prescott E, Hippe M, Schnohr P, Hein HO, Vestbo J . Smoking and risk of myocardial infarction in women and men: longitudinal population study. BMJ 1998;316(7137):1043-1047. doi:10.1136/bmj.316.7137.1043
2. Sniderman AD, Thanassoulis G, Glavinovic T, et al . Apolipoprotein B Particles and Cardiovascular Disease: A Narrative Review. JAMA Cardiol 2019 Dec 1;4(12):1287-1295. doi: 10.1001/jamacardio.2019.3780
3. Wilkins JT, Li RC, Sniderman A, Chan C, Lloyd-Jones DM . Discordance Between Apolipoprotein B and LDL-Cholesterol in Young Adults Predicts Coronary Artery Calcification: The CARDIA Study. J Am Coll Cardiol 2016;67(2):193-201. doi:10.1016/j.jacc.2015.10.055
4. Ridker PM, Lei L, Louie MJ, et al . Inflammation and Cholesterol as Predictors of Cardiovascular Events Among 13 970 Contemporary High-Risk Patients With Statin Intolerance. Circulation 2024;149(1):28-35. doi:10.1161/CIRCULATIONAHA.123.066213
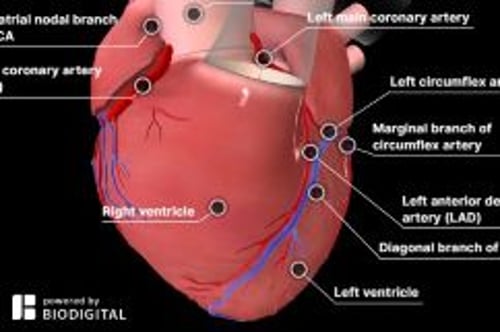
Coronary Artery Anatomy
The right and left coronary arteries arise from the right and left coronary sinuses in the root of the aorta just above the aortic valve orifice (see figure Arteries of the Heart ). The coronary arteries divide into large and medium-sized arteries that run along the heart’s surface (epicardial coronary arteries) and subsequently send smaller arterioles into the myocardium.
The left coronary artery begins as the left main artery and quickly divides into the left anterior descending (LAD), circumflex, and sometimes an intermediate artery (ramus intermedius). The LAD artery usually follows the anterior interventricular groove and, in some people, continues over the apex. This artery supplies the anterior septum (including the proximal conduction system) and the anterior free wall of the left ventricle (LV). The circumflex artery, which is usually smaller than the LAD artery, supplies the lateral LV free wall.
The dominant coronary artery refers to the one that gives rise to the posterior descending artery. Most people have right dominance: The right coronary artery passes along the atrioventricular (AV) groove over the right side of the heart; it supplies the sinus node (in 55%), right ventricle, and usually the AV node and inferior myocardial wall. About 10 to 15% of people have left dominance: The circumflex artery is larger and continues along the posterior AV groove to supply the posterior wall and AV node.
Arteries of the Heart
Treatment of Coronary Artery Disease
Medical therapy, including antiplatelet agents, lipid-lowering drugs (eg, statins), and beta-blockers
Percutaneous coronary intervention (PCI)
For acute thrombosis, sometimes fibrinolytic drugs
Coronary artery bypass grafting (CABG)
Treatment generally aims to reduce cardiac workload by decreasing oxygen demand and improving coronary artery blood flow, and, over the long term, to halt and reverse the atherosclerotic process. Coronary artery blood flow can be improved by percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG). An acute coronary thrombosis may sometimes be dissolved by fibrinolytic drugs .
Medical therapy
(See also Medications for Acute Coronary Syndromes .)
Medical management of patients with CAD depends on symptoms, cardiac function, and the presence of other disorders. Recommended therapy includes
Antiplatelet agents to prevent thrombus formation
Statins to lower LDL cholesterol levels
Beta-blockers to reduce symptoms of angina
Antiplatelet agents and statins improve short-term and long-term outcomes, probably by improving atheromatous plaque stability and endothelial function.
Beta-blockers reduce symptoms of angina by reducing heart rate and contractility and decreasing myocardial oxygen demand. Beta-blockers also reduce mortality post-infarction, especially in the presence of post-myocardial infarction (MI) LV dysfunction.
Calcium channel blockers are also helpful. They often are combined with beta-blockers in managing angina and hypertension but have not been proven to reduce mortality.
Nitrates modestly dilate coronary arteries and decrease venous return, decreasing cardiac work and relieving angina quickly. Longer acting nitrate formulations help decrease angina events but do not decrease mortality.
Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) are most effective at reducing mortality post MI in CAD patients with LV dysfunction ( 1, 2 ).
Little evidence exists to guide therapy for patients with endothelial dysfunction. Treatment is generally similar to that for typical large-vessel atherosclerosis, and some evidence suggests that use of beta-blockers may enhance endothelial function ( 3 ).
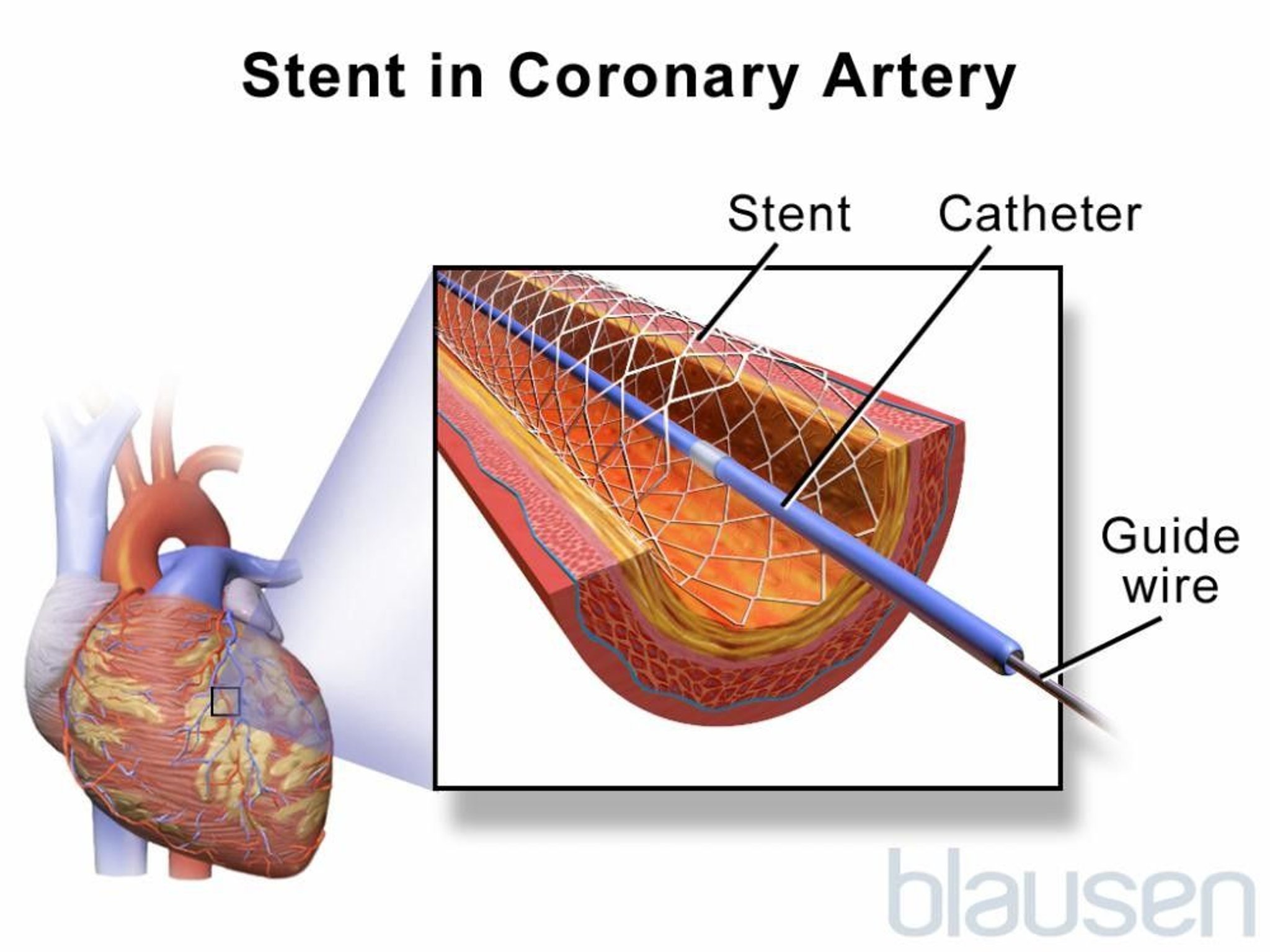
(See Percutaneous Coronary Interventions .)
PCI is indicated for patients with acute coronary syndrome (ACS) or with stable ischemic heart disease who have angina despite optimal medical therapy.
Drug-eluting stents, < 10% ( 4 ). Most PCI is done with stents, and most stents used in the United States are drug-eluting.
Patients without significant infarct or complications may return to work and usual activities usually within a few days after stent placement. However, cardiac rehabilitation is recommended for all patients.
In-stent thrombosis occurs because of the inherent thrombogenicity of metallic stents. Most cases occur within the first 24 to 48 hours. However, late stent thrombosis, occurring after 30 days and as late as ≥ 1 year (rarely), can occur with both bare-metal and drug-eluting stents, especially after cessation of antiplatelet therapy. Progressive endothelialization of the bare-metal stent occurs within the first few months and reduces the risk of thrombosis. However, the antiproliferative drugs released by drug-eluting stents inhibit this process and prolong the risk of thrombosis. Thus, patients who undergo stent placement are treated with various antiplatelet agents . The current standard regimen for patients with a bare-metal or drug-eluting stent consists of all of the following ( 5 ):
Glycoprotein IIb/IIIa inhibitors are not routinely used in stable patients (ie, no comorbidities, no acute coronary syndrome) having elective stent placement. They may be beneficial in some patients with an acute coronary syndrome but should not be considered routine. It is unclear whether it is beneficial to give glycoprotein IIb/IIIa inhibitors before arrival in the cardiac catheterization laboratory, but most national organizations do not recommend their use in this situation ( 5 ).
A statin is started after stent insertion, if one is not already being used because PCI by itself does not cure or prevent the progression of CAD. Statin therapy has been shown to improve long-term event-free survival ( 6 ). Patients who receive a statin before the procedure have a lower risk of periprocedural MI.
Overall, risks of undergoing PCI are comparable to those of CABG. Overall mortality rate is < 1%, but varies based on individual risk factors and tends to be similar to that of CABG; Q wave MI rate is < 1%. In < 1% of patients, intimal dissection causes obstruction requiring emergency CABG. Risk of stroke with PCI is lower than with CABG. A meta-analysis of 19 randomized trials reported a higher risk of stroke in patients undergoing CABG (1.2%) than PCI (0.34%,) at 30 days ( 7 ). Risk of bleeding is 1 to 2%.
(See Coronary Artery Bypass Grafting .)
CABG uses arteries (eg, internal mammary, radial) whenever possible, and if necessary, sections of autologous veins (eg, saphenous) to bypass diseased segments of the coronary arteries. At 1 year, about 85% of venous bypass grafts are patent, and after 5 years, one third or more are completely blocked. However, after 10 years, as many as 97% of internal mammary artery grafts are patent ( 8 ). Arteries also hypertrophy to accommodate increased flow. CABG is superior to PCI in patients with diabetes and in patients with multivessel disease amenable to grafting.
Coronary artery bypass grafting is typically done during cardiopulmonary bypass with the heart stopped; a bypass machine pumps and oxygenates blood. Risks of the procedure include stroke and MI. For patients with a normal-sized heart, no history of MI, good ventricular function, and no additional risk factors, risk is < 5% for perioperative MI, 1 to 2% for stroke, and ≤ 1% for mortality; risk increases with age, poor LV function, and presence of underlying disease. Operative mortality rate is 3 to 5 times higher for a second bypass than for the first.
After cardiopulmonary bypass, about 25 to 30% of patients develop cognitive dysfunction or behavioral changes, possibly caused by microemboli originating in the bypass machine ( 9 ). Cognitive or behavioral changes are more prevalent in older patients, prompting suspicion that these changes are most likely due to diminished "neuronal reserve," making older patients more susceptible to minor injuries incurred during cardiopulmonary bypass. Dysfunction ranges from mild to severe and may persist for weeks to years. To minimize this risk, some centers use a beating heart technique (off-pump CABG, which uses no cardiopulmonary bypass), in which a device mechanically stabilizes the part of the heart upon which the surgeon is working. However, long-term studies have failed to demonstrate lasting benefits of this approach in comparison to conventional on-pump CABG.
CAD may progress despite bypass surgery. Postoperatively, the rate of proximal obstruction of bypassed vessels increases. Vein grafts become obstructed early if thrombi form and later (several years) if atherosclerosis causes slow degeneration of the intima and media. Aspirin prolongs vein graft patency. Continued smoking has a profound adverse effect on patency. After CABG, a statin should be started or continued at maximally tolerated doses.
Treatment references
1. Indications for ACE inhibitors in the early treatment of acute myocardial infarction: systematic overview of individual data from 100,000 patients in randomized trials. ACE Inhibitor Myocardial Infarction Collaborative Group. Circulation 1998;97(22):2202-2212. doi:10.1161/01.cir.97.22.2202
2. Düsing R . Mega clinical trials which have shaped the RAS intervention clinical practice. Ther Adv Cardiovasc Dis 2016;10(3):133-150. doi:10.1177/1753944716644131
3. Peller M, Ozierański K, Balsam P, Grabowski M, Filipiak KJ, Opolski G . Influence of beta-blockers on endothelial function: A meta-analysis of randomized controlled trials. Cardiol J 2015;22(6):708-716. doi:10.5603/CJ.a2015.0042
4. Bønaa KH, Mannsverk J, Wiseth R, et al . Drug-Eluting or Bare-Metal Stents for Coronary Artery Disease. N Engl J Med 2016;375(13):1242-1252. doi:10.1056/NEJMoa1607991
5. Writing Committee Members, Lawton JS, Tamis-Holland JE, et al . 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines [published correction appears in J Am Coll Cardiol 2022 Apr 19;79(15):1547]. J Am Coll Cardiol 2022;79(2):e21-e129. doi:10.1016/j.jacc.2021.09.006
6. Grundy SM, Stone NJ, Bailey AL, et al : 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [published correction appears in Circulation 2019 Jun 18;139(25):e1182-e1186] [published correction appears in Circulation 2023 Aug 15;148(7):e5]. Circulation 139(25):e1082–e1143, 2019. doi:10.1161/CIR.0000000000000625
7. Palmerini T, Biondi-Zoccai G, Reggiani LB, et al : Risk of stroke with coronary artery bypass graft surgery compared with percutaneous coronary intervention. J Am Coll Cardiol 60(9):798–805, 2012. doi:10.1016/j.jacc.2011.10.912
8. Hillis LD, Smith PK, Anderson JL, et al : 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines [published correction appears in Circulation 2011 Dec 20;124(25):e957]. Circulation 124(23):e652–e735, 2011. doi:10.1161/CIR.0b013e31823c074e
9. Kulik A, Ruel M, Jneid H, et al : Secondary prevention after coronary artery bypass graft surgery: a scientific statement from the American Heart Association. Circulation 131(10):927–964, 2015. doi:10.1161/CIR.0000000000000182
Prevention of Coronary Artery Disease
The American Heart Association (AHA) recommends using the pooled cohort risk assessment equations to estimate lifetime and 10-year risk of atherosclerotic cardiovascular disease. The risk calculator is based on sex, age, race, total and high-density lipoprotein (HDL) cholesterol levels, systolic blood pressure (and whether blood pressure is being treated), diabetes, and smoking status ( 1 ).
Prevention of coronary artery disease involves modifying atherosclerosis risk factors :
Smoking cessation
Weight loss
Healthful diet
Regular exercise
Modification of serum lipid levels
Reduction of salt intake
Control of hypertension
Control of diabetes
Antihypertensive recommendations vary. In the United States, for patients who are at low risk ( < 10% 10-year risk) of atherosclerotic cardiovascular disease (ASCVD), antihypertensive therapy is recommended if blood pressure is > 130/80. In patients with coronary artery disease or whose risk of ASCVD is > 10%, antihypertensive medication is recommended for blood pressure > 130/80 mm Hg ( 2 ).
Modification of serum lipid levels (particularly with statins) may slow or even partially reverse the progression of CAD. Treatment goals have been modified. Instead of trying to achieve specific target low-density lipoprotein (LDL) cholesterol levels, patients are selected for treatment based on their risk of ASCVD. Lower risk patients with elevated LDL may not require statin treatment. Four higher risk patient groups have been identified in whom the benefit of statin therapy outweighs the risk of adverse events:
Patients with clinical ASCVD
Patients with LDL cholesterol ≥ 190 mg/dL ( ≥ 4.9 mmol/L)
Patients age 40 to 75 years with diabetes and LDL cholesterol levels of 70 to 189 mg/dL (1.8 to 4.9 mmol/L)
Patients age 40 to 75 years without diabetes, with LDL cholesterol levels of 70 to 189 mg/dL (1.8 to 4.9 mmol/L), and with ASCVD risk > 7.5%
Nicotinic acid or a fibrate may be added for patients with an HDL cholesterol level < 40 mg/dL ( < 1.03 mmol/L), although several trials have failed to demonstrate a lower risk of ischemia or slowed progression of atherosclerosis when medications are used to raise HDL ( 3 ).
≥ 60 years ( 4 ). It can be considered for patients aged 40 to 59 years whose 10-year risk of cardiovascular disease exceeds 10%, but absolute benefit is likely to be small.
Prevention references
1. Arnett DK, Blumenthal RS, Albert MA, et al : 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 74:1376–1414, 2019. doi: 10.1016/j.jacc.2019.03.009
2. Whelton PB, Carey RM, Aronow WS, et al : ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 71:e127–e248, 2018. doi: 10.1161/HYP.0000000000000066
3. AIM-HIGH Investigators, Boden WE, Probstfield JL, Anderson T, et al : Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med 365(24): 2255–2267, 2011. doi: 10.1056/NEJMoa1107579
4. US Preventive Services Task Force, Davidson KW, Barry MJ, et al : Aspirin Use to Prevent Cardiovascular Disease: US Preventive Services Task Force Recommendation Statement. JAMA 327(16):1577–1584, 2022. doi:10.1001/jama.2022.4983

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines
Coronary Heart Disease
What are the coronary arteries.
Coronary arteries supply blood to the heart muscle. Like all other tissues in the body, the heart muscle needs oxygen-rich blood to function, and oxygen-depleted blood must be carried away. The coronary arteries run along the outside of the heart and have small branches that supply blood to the heart muscle.
What are the different coronary arteries?
The 2 main coronary arteries are the left main and right coronary arteries.
Left main coronary artery (LMCA). The left main coronary artery supplies blood to the left side of the heart muscle (the left ventricle and left atrium). The left main coronary artery divides into branches:
The left anterior descending artery branches off the left coronary artery and supplies blood to the front of the left side of the heart.
The circumflex artery branches off the left coronary artery and encircles the heart muscle. This artery supplies blood to the lateral side and back of the heart.
Right coronary artery (RCA). The right coronary artery supplies blood to the right ventricle, the right atrium, and the SA (sinoatrial) and AV (atrioventricular) nodes, which regulate the heart rhythm. The right coronary artery divides into smaller branches, including the right posterior descending artery and the acute marginal artery.

Additional smaller branches of the coronary arteries include the obtuse marginal (OM), septal perforator (SP), and diagonals.
Why are the coronary arteries important?
Since coronary arteries deliver blood to the heart muscle, any coronary artery disorder or disease can reduce the flow of oxygen and nutrients to the heart, which may lead to a heart attack and possibly death. Atherosclerosis is inflammation and a buildup of plaque in the inner lining of an artery causing it to narrow or become blocked. It is the most common cause of heart disease.

What is coronary artery disease?
Coronary heart disease, or coronary artery disease (CAD), is characterized by inflammation and the buildup of and fatty deposits along the innermost layer of the coronary arteries. The fatty deposits may develop in childhood and continue to thicken and enlarge throughout the life span. This thickening, called atherosclerosis, narrows the arteries and can decrease or block the flow of blood to the heart.

The American Heart Association estimates that over 16 million Americans suffer from coronary artery disease--the number one killer of both men and women in the U.S.
What are the risk factors for coronary artery disease?
Risk factors for CAD often include:
High LDL cholesterol , high triglycerides levels, and low HDL cholesterol
High blood pressure (hypertension)
Physical inactivity
High saturated fat diet
Family history
Controlling risk factors is the key to preventing illness and death from CAD.
What are the symptoms of coronary artery disease?
The symptoms of coronary heart disease will depend on the severity of the disease. Some people with CAD have no symptoms, some have episodes of mild chest pain or angina, and some have more severe chest pain.
If too little oxygenated blood reaches the heart, a person will experience chest pain called angina. When the blood supply is completely cut off, the result is a heart attack, and the heart muscle begins to die. Some people may have a heart attack and never recognize the symptoms. This is called a "silent" heart attack.
Symptoms of coronary artery disease include:
Heaviness, tightness, pressure, or pain in the chest behind the breastbone
Pain spreading to the arms, shoulders, jaw, neck, or back
Shortness of breath
Weakness and fatigue
How is coronary artery disease diagnosed?
In addition to a complete medical history and physical exam, tests for coronary artery disease may include the following:
Electrocardiogram (ECG or EKG). This test records the electrical activity of the heart, shows abnormal rhythms (arrhythmias), and detects heart muscle damage.
Stress test (also called treadmill or exercise ECG). This test is given while you walk on a treadmill to monitor the heart during exercise. Breathing and blood pressure rates are also monitored. A stress test may be used to detect coronary artery disease, or to determine safe levels of exercise after a heart attack or heart surgery. This can also be done while resting using special medicines that can synthetically place stress on the heart.
Cardiac catheterization . With this procedure, a wire is passed into the coronary arteries of the heart and X-rays are taken after a contrast agent is injected into an artery. It's done to locate the narrowing, blockages, and other problems.
Nuclear scanning. Radioactive material is injected into a vein and then is observed using a camera as it is taken up by the heart muscle. This indicates the healthy and damaged areas of the heart.
Treatment for coronary heart disease
Treatment may include:
Modification of risk factors. Risk factors that you can change include smoking, high cholesterol levels, high blood glucose levels, lack of exercise, poor dietary habits, being overweight, and high blood pressure.
Medicines. Medicine that may be used to treat coronary artery disease include:
Antiplatelets. These decrease blood clotting. Aspirin, clopidogrel, ticlopidine, and prasugrel are examples of antiplatelets.
Antihyperlipidemics. These lower lipids (fats) in the blood, particularly low density lipid (LDL) cholesterol. Statins are a group of cholesterol-lowering medicines, and include simvastatin, atorvastatin, and pravastatin, among others. Bile acid sequestrants--colesevelam, cholestyramine and colestipol--and nicotinic acid (niacin) are other medicines used to reduce cholesterol levels.
Antihypertensives. These lower blood pressure. Several different groups of medicines work in different ways to lower blood pressure.
Coronary angioplasty. With this procedure, a balloon is used to create a bigger opening in the vessel to increase blood flow. Although angioplasty is done in other blood vessels elsewhere in the body, percutaneous coronary intervention (PCI) refers to angioplasty in the coronary arteries to permit more blood flow into the heart. PCI is also called percutaneous transluminal coronary angioplasty (PTCA). There are several types of PCI procedures, including:
Balloon angioplasty. A small balloon is inflated inside the blocked artery to open the blocked area.
Coronary artery stent. A tiny mesh coil is expanded inside the blocked artery to open the blocked area and is left in place to keep the artery open.
Atherectomy. The blocked area inside the artery is cut away by a tiny device on the end of a catheter.
Laser angioplasty. A laser used to "vaporize" the blockage in the artery.
Coronary artery bypass . Most commonly referred to as simply "bypass surgery" or CABG (pronounced "cabbage"), this surgery is often done in people who have chest pain (angina) and coronary artery disease. During the surgery, a bypass is created by grafting a piece of a vein above and below the blocked area of a coronary artery, enabling blood to flow around the blockage. Veins are usually taken from the leg, but arteries from the chest or arm may also be used to create a bypass graft. Sometimes, multiple bypasses may be needed to fully restore blood flow to all regions of the heart.
Find a Doctor
Specializing In:
- Coronary Angiography
- Cardiac Disease
- Cardiovascular Disease
At Another Johns Hopkins Member Hospital:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital
Find a Treatment Center
Find Additional Treatment Centers at:

Request an Appointment

Special Heart Risks for Men

A Heart-Healthy Eating Adventure

Diabetes Medications That Treat Heart Disease Too
Related Topics

Coronary Artery Disease (CAD)
- • Buildup of cholesterol or plaque that causes arteries to stiffen, narrow, and restrict blood flow
- • Symptoms may not be noticeable at first but include fatigue, chest pain, and/or shortness of breath
- • Treatments include heart transplantation, artificial heart implantation, and valve replacements
- • Involves Cardiology
- Cardiac Surgery
- Heart Disease Prevention
- Coronary Artery Bypass Graft (CABG)
- Coronary Artery CT Angiography
What causes coronary artery disease?
What are the symptoms of coronary artery disease, how is coronary artery disease diagnosed, how is coronary artery disease treated, what surgical procedures does yale medicine offer for the treatment of coronary artery disease, what makes yale medicine’s approach to the treatment of coronary artery disease unique.
There is a lot you can do to prevent coronary artery disease, which causes narrowing of the arteries and increases the risk of heart attack. It's the most common type of heart disease and the leading cause of death for both men and women in the United States.
Eating healthy, exercising, keeping your weight down, controlling your blood pressure and quitting smoking are all essential to preventing this condition.
If you do have risk factors—and they include family history—you should see a good cardiologist. Yale Medicine provides a full spectrum of clinical cardiovascular care, and our specialists have extensive experience with coronary artery disease. If you need surgery, we have renowned surgeons and the most advanced treatments available.
Coronary artery disease is caused by the gradual buildup of cholesterol or plaque, which makes the arteries stiffen and narrow. The result is reduced blood flow to the heart.
Multiple causes of coronary artery disease include:
- Genetics: Having a family history of heart disease
- Lifestyle: Eating unhealthy, high-fat foods and being sedentary
- Medical conditions: Including diabetes, high cholesterol and high blood pressure
Many people with heart disease have more than one of those risk factors.
People with coronary artery disease are at higher risk for a heart attack and other heart conditions that can be debilitating or even fatal. This leads to symptoms such as cardiac angina, the clinical term for shortness of breath and chest pain.
A sudden heart attack may be caused by a blood clot that forms on the surface of the plaque.
In its early stages, coronary artery disease may have no symptoms, though some people experience fatigue, chest pain or shortness of breath.
Doctors screen for heart disease during routine exams, asking questions about your personal and family history, taking blood samples to test cholesterol levels, and measuring your weight and blood pressure.
If a doctor has a reason to suspect you have heart disease, he or she may order additional tests. These can include an electrocardiogram, which measures electrical activity in the heart, or a stress test, which measures how well the heart works when stressed by physical activity.
Most people with coronary artery disease can be helped by one or several of three types of treatment. These are:
- Medication: Prescription drugs can counter the effects of heart disease, helping to keep risk factors including hypertension and cholesterol under control.
- Coronary stent: This is also called a percutaneous coronary intervention. A catheter is sent to the site of the blockage to open up the artery to restore blood flow.
- Heart surgery: A coronary artery bypass graft can reroute blood flow around a blocked artery.
Each of these treatments has advantages and disadvantages for patients. Surgery is generally reserved for patients who do not improve with the help of medication or stents or who can’t be effectively treated with those less-invasive methods.
Yale Medicine offers the full array of modern surgical treatments for all types of coronary artery disease. These include:
- Heart transplants
- Implantation of artificial hearts (called left ventricular assist devices, or LVAD )
- Mitral valve replacemen t and repair, for diseased heart valves
- Transcatheter Aortic Valve Replacement (called TAVR), an innovative treatment for patients with heart disease who are not strong enough for other types of heart surgery
Yale Medicine also offers surgical procedures to treat arrhythmia , hypertrophic cardiomyopathy , complex aortic aneurysm and other related issues.
Yale Medicine offers world-class expertise in treating all types of coronary artery disease with excellent outcomes.
Our doctors place a strong emphasis on multidisciplinary collaboration among cardiologists , interventional cardiologists, and cardiac surgeons .
Treatment planning for every high-risk patient with heart disease includes a formal collaborative discussion to evaluate all treatment options without any bias toward one specialty. This ensures that every patient benefits from input from specialists from several disciplines—a particular advantage for patients with complex heart disease.
Patients with heart disease who come to Yale Medicine for treatment can count on receiving cutting-edge therapies, using the latest, most innovative technologies and instrumentation.
Our cardiac surgeons’ clinical and basic research brings important advantages to patients, who have access to some of the newest technologies for the surgical treatment of heart disease.
Coronary Heart Disease, Myocardial Infarction, and Stroke — A Public Health Issue

Available for Download pdf icon [PDF – 3 MB]
Adults are living longer, and diseases of the heart and circulatory vessels are prevalent in this growing population of older adults. 1 Comorbid conditions along with cognition, sleep, physical balance and strength are factors that affect a person’s ability to function well and make disease management for people with coronary heart disease more challenging. 1,2 Maintaining functional abilities is critical for older adults from the perspective of overall health status, heart health, and chronic disease management. 1,2 Physical activity is key to preserving functional capacity and reducing frailty, which occurs more frequently in people with heart disease. 1,2 High blood pressure is an under-recognized contributing factor to premature disability and institutionalization and also key to preserving functional capacity. 3
Physical activity is important for maintaining heart muscle, vessel elasticity, reducing blood pressure levels and improving physical balance and strength. 1 It is foundational to chronic disease management programs and cardiac or stroke rehabilitation plans for improved mobility, fexibility and muscle strengthening. 1, 2
High blood pressure is a risk factor for coronary heart disease, myocardial infarction and stroke and is very common in older adults. 3 It is a leading cause of preventable illness and death. 3 Controlling high blood pressure is shown to reduce the risk of fatal myocardial infarctions and strokes. 3
Lowering blood pressure can be done safely with an established, monitored medication regime, physical activity and reduced sodium/salt intake. 3 Treating high blood pressure in older adults is a challenge due to other comorbid conditions, frailty, cognitive impairment and multiple medication use. 3
Coronary heart disease develops when major blood vessels supplying the heart with blood, oxygen and nutrients become damaged or blocked due to plaque build-up that limits blood flow. 4 Angina, a symptom of coronary heart disease, is chest pain or discomfort that occurs if an area of heart muscle is starved of oxygen-rich blood. 4 A heart attack occurs when the flow of oxygen-rich blood to a section of heart muscle suddenly becomes blocked and the heart can’t get oxygen and may damage heart muscle. 4 A stroke leads to death of brain cells due to lack of oxygen, caused by blockage of blood flow or rupture of a vessel to the brain. 4

Data for Public Health Action
As the older adult population continues to live longer, and diseases of the heart and circulatory vessels continue to increase, public health professionals are challenged to assist middle-aged and older adults in maintaining their functional capacity. Promoting chronic disease self-management through high blood pressure control, maintaining physical activity and a medication regime management is critical to older adult quality of life.

This brief examines the following questions:
- What percentage of adults report having coronary heart disease (CHD), including myocardial infarction and angina?
- What percentage of adults report having a stroke?
- What percentage of adults report being diagnosed with CHD, or a stroke, or both?
- What percentage of adults report being diagnosed with CHD, or a stroke, or both were taking high blood pressure medications?
- What percentage of adults report being diagnosed with CHD, or a stroke, or both were physically inactive, or had not exercised in the past month?
- What percentage of adults report being diagnosed with CHD, or a stroke, or both report good to excellent health or experienced 14 or more unhealthy days?
- What percentage of adults report being diagnosed with CHD, or a stroke, or both report having health care coverage and annual check-up?
- What percentage of adults report being diagnosed with CHD, or a stroke, or both report having two or more chronic diseases?
- What percentage of middle-aged and older adults report being diagnosed with CHD, or a stroke, or both self-report having subjective cognitive decline?
- What percentage of adults diagnosed with CHD, or a stroke, or both report being a caregiver by providing care or assistance to a friend or family member in the past 30 days or for two years or more?
The coronary heart disease and stroke data presented in this brief were collected from community-dwelling adults 45 years of age and older in 2015-2017 through the Behavioral Risk Factor Surveillance System (BRFSS).5 Questions related to coronary heart disease and stroke were administered in 50 states, the District of Columbia and two territories—Puerto Rico and Guam. Additional data reports can be generated and viewed through the CDC Healthy Aging Data Portal .
These data were examined in two age groups, adults 45-64 years and aged 65 years and older, as well as by sex, race and ethnicity, chronic disease status, and other demographic characteristics.
Characteristics of Middle-Aged and Older Adults with Coronary Heart Disease a
Figure 1: Adults Aged 45 years and Older Who Reported Having Coronary Heart Disease
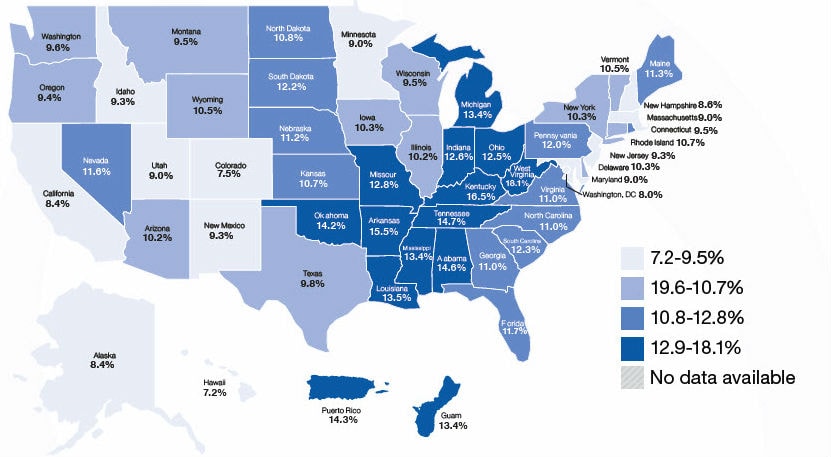
Has a doctor, nurse, or other health professional ever told you that you had any of the following: Ever told you had a heart attack, also called a myocardial infarction? Ever told you had angina or coronary heart disease?

- 7.1% adults aged 45 to 64 years reported having CHD compared with 17.0% of adults aged 65 years and older.
- 13.6% of men reported having CHD compared with 8.4% of women.
- The prevalence of CHD varied among racial/ethnic groups: 11.4% of whites, 10.0% of blacks/African Americans, 8.8% of Hispanics, and 6.3% of Asians and Pacifc Islanders.
- Prevalence of CHD was lower in adults with more years of formal education (10.9% with post high school education) compared with adults with few years of formal education (16.5% with less than a high school diploma).
a Respondents were classified as having coronary heart disease (CHD) if they reported having been told by a provider they had CHD. Respondents were also classified as having CHD if they reported having been told they had a heart attack (i.e., myocardial infarction) or angina.
Characteristics of Middle-Aged and Older Adults with a Stroke b
Figure 2: Adults Aged 45 years and Older Who Reported Having Had a Stroke
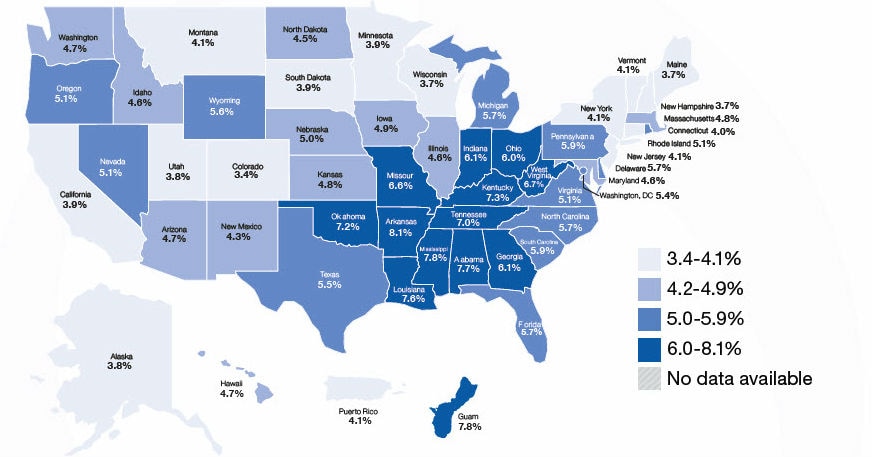
Has a doctor, nurse, or other health professional ever told you that you had a stroke?

- 3.7% adults aged 45 to 64 years reported having been told that they had a stroke compared with 7.6% of adults aged 65 years and older.
- 5.3% of men reported having been told that they had a stroke compared with 5.0% of women.
- The prevalence of stroke varied among racial/ethnic groups: 5.1% of whites, 7.5% of blacks/African Americans, 3.7% of Hispanics, and 2.9% of Asians and Pacifc Islanders.
- Prevalence of stroke was lower in adults with more years of formal education (5.1% with post high school education) compared with adults with few years of formal education (8.0% with less than a high school diploma).
b Respondents may also have been told they have CHD (not mutually exclusive).
Characteristics of Middle-Aged and Older Adults with Coronary Heart Disease, a or a Stroke, or Both
Figure 3: Adults Aged 45 years and Older Who Reported Having Had Coronary Heart Disease, or a Stroke, or Both

Has a doctor, nurse, or other health professional ever told you that you had any of the following: Ever told you had a heart attack, also called a myocardial infarction? Ever told you had angina or coronary heart disease? Ever told you had a stroke?

- 9.6% adults aged 45 to 64 years reported being diagnosed with CHD, or a stroke, or both compared with 21.7% of adults aged 65 years and older.
- 16.8% of men reported having CHD, or a stroke, or both compared with 11.8% of women.
- The prevalence of CHD, or a stroke, or both varied among racial/ethnic groups: 14.8% of whites, 14.9% of blacks/African Americans, 11.2% of Hispanics, and 8.2% of Asians and Pacifc Islanders.
- Prevalence of CHD, or a stroke, or both was lower in adults with more years of formal education (11.7% of adults with post high school education) compared with adults with few years of formal education (21.2% of adults with less than a high school education).
- 30.5% of adults with CHD or a stroke, or both report living alone.
Health Status: Taking Medications for High Blood Pressure Among Adults with CHD or a Stroke, or Both
Figure 4: Adults Aged 45 years and Older with CHD, or a Stroke, or Both and Reported Taking High Blood Pressure Medicine
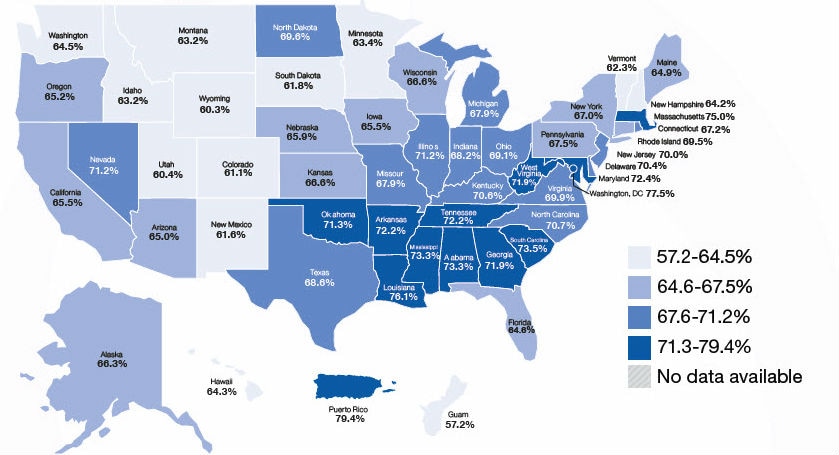
Has a doctor, nurse or other health professional ever told you that you have CHD, or a stroke, and or both and have high blood pressure? Are you currently taking medicine for your high blood pressure?

- 64.2% of adults aged 45 to 64 years diagnosed with CHD, or a stroke, or both reported taking high blood pressure medicine compared with 71.6% of adults aged 65 years and older.
- 68.4% of men with CHD, or a stroke, or both reported taking medications for high blood pressure compared with 68.6% of women with CHD, or a stroke, or both.
- The prevalence of CHD, or a stroke, or both and taking high blood pressure medications varied among racial/ethnic groups: 66.8% of whites, 79.9% of blacks/ African Americans, 66.0% of Hispanics, and 75.0% of Asians and Pacifc Islanders.
- Prevalence of adults with CHD, or a stroke or both and taking high blood pressure medicines was lower in adults with more than high school education (66.7%) compared with adults with less than a high school education (71.1%).
Health Status: Physical Activity
Figure 5: Adults Aged 45 years and Older Diagnosed with Coronary Heart Disease, or a Stroke, or Both Who Reported Participating in Physical Activity for 150 Minutes or More per Week in the Past Month
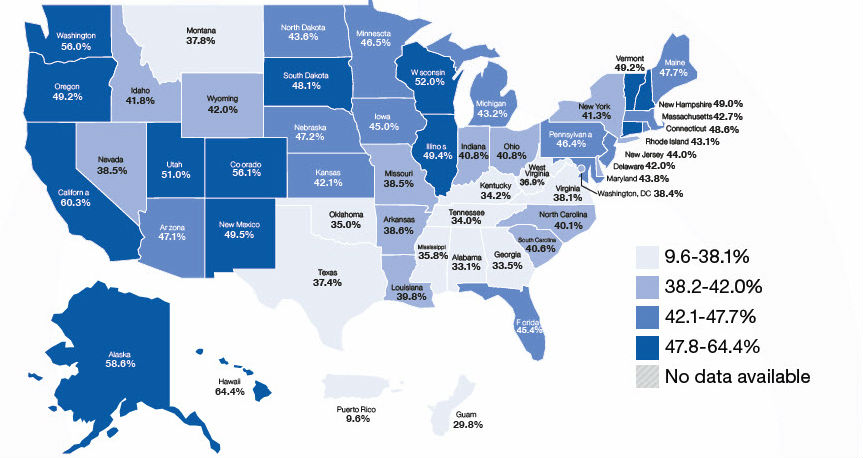
Being physically inactive can be a risk factor for increased complications for people diagnosed with coronary heart disease, or a stroke or both. Low and moderate levels of physical activity significantly reduce long-term risks for coronary heart disease deaths and assist with lowering high blood pressure. 6 The optimal amount of physical activity is moderate intensity aerobic exercise at least 150 minutes per week or 75 minutes per week of vigorous-intensity aerobic activity, for adults aged 45 years and older. 6
The physical activity measure identifies adults who participated in 150+ minutes (or vigorous equivalent minutes) of physical activity per week in past 30 days.
- 39.2% of adults aged 45-64 years diagnosed with CHD, or a stroke, or both reported participating in 150 minutes or more of physical activity per week compared with 46.3% of adults 65 years of age and older.
- 37.5% of women diagnosed with CHD, or a stroke, or both reported participating in 150 minutes or more of physical activity per week compared with 48.0% of men.
- The prevalence of adults participating in physical activity among adults diagnosed with CHD, or a stroke or both varied among racial/ethnic groups: 45.9% of whites, 32.9% of blacks/African Americans, 35.7% of Hispanics, and 50.7% of Asians and Pacifc Islanders.
- Prevalence of physical activity among adults diagnosed with CHD, or a stroke, or both was higher in adults with post high school education (50.8%) compared with adults with less than a high school education (32.7%).
Health Status: Health Care Coverage and Annual Check-ups
Figure 6: Adults Aged 45 years and Older Diagnosed with Coronary Heart Disease, or a Stroke, or Both, Who Had Health Insurance
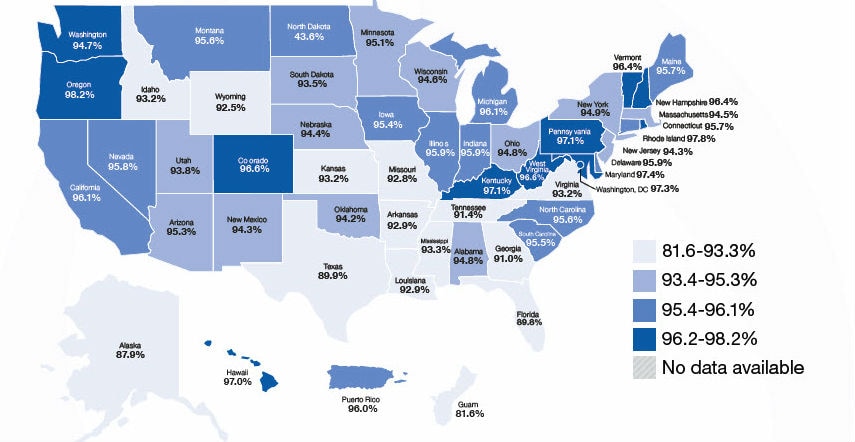
Do you have any kind of health care coverage, including health insurance, prepaid plans such as HMOs, or government plans such as Medicare, or Indian Health Service?
- 98.2% of adults aged 65 years and older diagnosed with CHD, or a stroke, or both reported having health care coverage compared with 88.9% of adults aged 45-64 years.
- The prevalence of having some form of health care coverage among persons having CHD or a stroke or both varied among racial/ethnic groups: 95.9% of whites, 90.8% of blacks/African Americans, 87.8% of Hispanics, and 89.8% of Asians and Pacific Islanders.
About how long has it been since you last visited a doctor for a routine check-up? Within the past year versus >12 months or never?
- 87.4% of adults diagnosed with CHD, or a stroke, or both reported having a routine check-up within the past year.
- 91.0% of adults aged 65 years and older diagnosed with CHD, or a stroke, or both reported having a routine check-up compared with 82.4% of adults aged 45-64 years.
Health Status: Excellent to Good Health and Unhealthy Days
Persons who have experienced coronary heart disease, or a stroke, or both may experience physical or mental limitations associated with their condition.
Would you say your health is Excellent, Very Good, Good, Fair or Poor? (Good to Excellent Health are data captured)

- 55.3% of adults diagnosed with CHD, or a stroke, or both aged 65 years and older reported their health as good to excellent compared with 43.6% of adults aged 45-64 years.
- Prevalence of adults with CHD, or a stroke, or both who reported their health as good to excellent was higher in adults with post high school education (59.3%) compared with adults with less than a high school education (33.6%).
Now thinking about your mental health, which includes stress, depression and problems with emotions, for how many days during the past 30 days was your mental health not good?
- 11.6% of adults diagnosed with CHD, or a stroke or both aged 65 years and older reported 14 or more mentally unhealthy days in the past month compared with 27.8% of adults aged 45-64 years.
- Prevalence of adults with CHD, or a stroke, or both experiencing 14 or more mentally unhealthy days was lower in adults with post high school education (14.7%) compared with adults with less than a high school education (25.7%).
Now thinking about your physical health, which includes physical illness and injury, for how many days during the past 30 days was your physical health not good?
- 28.7% of adults diagnosed with CHD, or a stroke, or both aged 65 years and older reported 14 or more physically unhealthy days in the past month compared with 39.2% of adults aged 45-64 years.
Health Status: Chronic Diseases
Figure 7: Adults Aged 45 years and older with Coronary Heart Disease, or a Stroke, or Both Who Reported Having Two or More Chronic Health Conditions
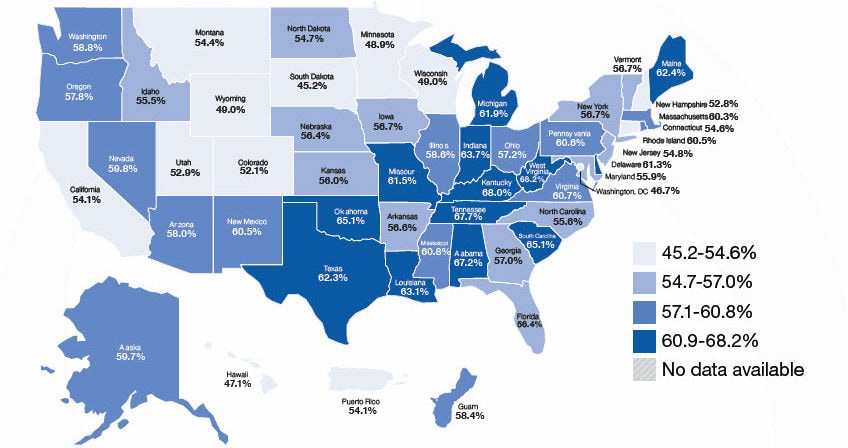
Has a doctor, nurse or other health professional ever told you that you had one of the following: a heart attack, angina or coronary heart disease, stroke, asthma (still have), cancer (skin, other types of cancer), COPD, arthritis, depressive disorder, kidney disease, diabetes?
Multiple chronic diseases (two or more) have been found to be associated with increased potential for functional diffculties. 1 As the number of chronic diseases increases, the management of these diseases becomes increasingly complex, which may lead to a greater need for assistance. 2
- 58.7% of adults diagnosed with CHD, or a stroke, or both reported having two or more other chronic diseases other than CHD or stroke.
- 57.3% adults aged 45 to 64 years diagnosed with CHD, or a stroke, or both report having at least two or more other chronic diseases compared with 59.7% of adults aged 65 years and older.
- 52.5% of men diagnosed with CHD, or a stroke, or both reported having at least two or more other chronic diseases compared to 66.4% of women.
- The prevalence of having at least two other chronic diseases among adults diagnosed CHD, or a stroke or both varied among racial/ethnic groups: 59.1% of whites, 57.2% of blacks/African Americans, 50.7% of Hispanics, and 47.2% of Asians and Pacifc Islanders.
- Prevalence of having at least two other chronic diseases among adults diagnosed with CHD, or a stroke, or both was lower in adults with post high school education (56.5%) compared with adults with less than a high school education (63.3%).
Health Status: Subjective Cognitive Decline
Figure 8: Percentage of Adults Aged 45 Years and Older with Coronary Heart Disease, or a Stroke, or Both Who had Subjective Cognitive Decline
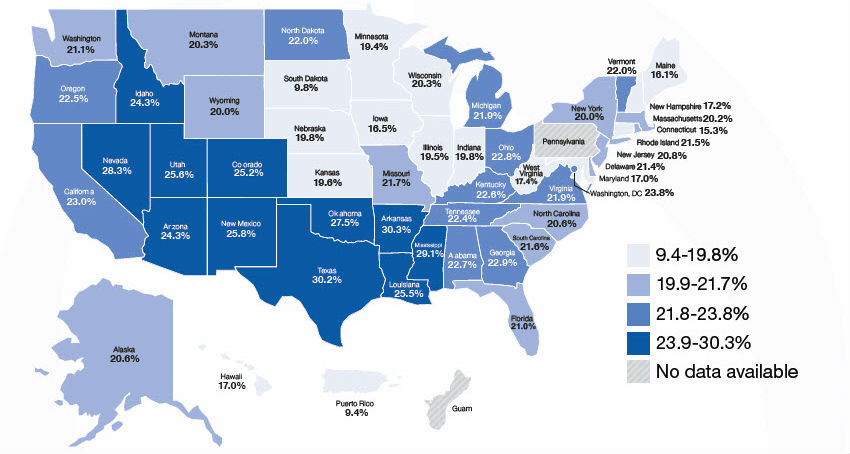
Coronary heart disease can lead to decreased cognitive function. 8 Subjective cognitive decline is the self-reported experience of worsening or more frequent confusion or memory loss within the past year. 7 Intensive blood pressure control may reduce the risk for cognitive decline.10 Cognitive decline can impact effective chronic disease self-management and successful activities of daily living. 8-10
During the past 12 months, have you experienced confusion or memory loss that is happening more often or is getting worse?
- 27.1% of adults aged 45-64 years diagnosed with CHD, or a stroke, or both reported subjective cognitive decline compared with 18.7% of adults 65 years of age and older.
- The prevalence of subjective cognitive decline among middle aged and older adults diagnosed with CHD, or a stroke, or both varied among racial/ethnic groups: 21.5% of whites, 23.1% of blacks/African Americans, 25.1% of Hispanics, and 7.1% of Asians and Pacifc Islanders.
- Prevalence of subjective cognitive decline among adults diagnosed with CHD, or a stroke, or both was lower in adults with post high school education (20.5%) compared with adults with less than a high school education (25.7%).
Prevalence of Coronary Heart Disease, or a Stroke, or Both Among Adult Caregivers
Figure 9: Adults Aged 45 years and Older with Coronary Heart Disease, or a Stroke, or Both Who Reported Being a Caregiver to Someone in the Past Month
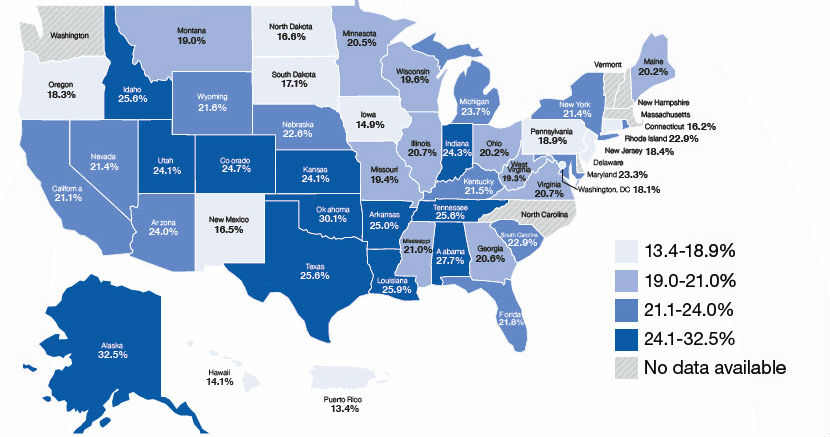
Persons who have experienced a heart attack or a stroke, or who have coronary heart disease (angina) may also be a caregiver for a friend or family member. Limitations associated with their own chronic health conditions can cause their caregiver role to become more challenging. 1, 2, 8-10
During the past 30 days, did you provide regular care or assistance to a friend or family member who has a health problem or disability?

Multiple chronic diseases (two or more) have been found to be associated with increased potential for functional difficulties. 1 As the number of chronic diseases increases, the management of these diseases becomes increasingly complex, which may lead to a greater need for assistance. 2
- 21.8% of adults diagnosed with CHD, or a stroke, or both reported providing care or assistance to friend or family member within the past 30 days.
- 36.9% of adult caregivers diagnosed with CHD, or a stroke, or both provided care for a friend or family member within the past 30 days for 20 or more hours per week.
For how long have you provided care for that person?
- 56.1% of adults diagnosed with CHD, or a stroke, or both reported providing care or assistance to friend or family member during the past two years.
Note: Caregiver and Subjective Cognitive Decline (SCD) estimates are based on data collected in 2015-2017 for states that asked these two modules, compared to other topics using only 2017 data.
Call to Action
Public health professionals can use existing data, such as that presented in this brief, to form action steps to assist the growing older population in maintaining heart health and functional capacity by collaborating with partners engaged in heart health, brain health, physical activity, healthy aging, and chronic disease self-management programs at the national, tribal, state, and local levels.
Key Strategies to improve heart, body, and brain health and reduce functional difficulties include:
- The Million Hearts Program—a national initiative with a network of partners focused on preventing 1 million heart attacks, strokes and other cardiovascular events by 2022. 5
- Engage middle aged and older adults diagnosed with coronary heart disease, myocardial infarction, or a stroke to engage in heart healthy behaviors to reduce and prevent hospitalizations or disability.
- Step it Up—a national initiative of the US Surgeon General’s Call to Action to Promote Walking and Walkable Communities. 11
- Increase messaging that emphasizes both the important role of caregivers and the importance of maintaining caregivers’ health and well-being.
- State Heart Disease and Stroke Prevention Programs—The State Public Health Actions to Prevent and Control Diabetes, Heart Disease and Stroke, a multifaceted initiative to improve heart and stroke health. 5
- American College of Preventive Medicine’s Educating Physicians on Benefts of BP Management to Reduce Cognitive Decline—a continuing education program for physicians.
- Educate health care professionals on the benefts of blood pressure management as a potential mechanism to reduce the future risk of cognitive decline and dementia.
- Encourage caregivers to get regular check-ups, use preventive services, and engage in self-care to maintain health.
- Ensure that persons, including caregivers, with a disability or chronic health conditions have access to self-management programs to maintain their health.
Technical Information
The Behavioral Risk Factor Surveillance System (BRFSS) is the nation’s premier system of health-related telephone surveys that collect state data about U.S. residents regarding their health-related risk behaviors, chronic diseases, and use of preventive services. Established in 1984 with 15 states, BRFSS now collects data in all 50 states as well as the District of Columbia and three U.S. territories. BRFSS completes more than 450,000 adult interviews each year, making it the largest and longest continuously conducted health survey system in the world.
The crucial information gathered through this state-based telephone surveillance system is used by national, state, and local public health agencies to identify populations that might be most at risk and to monitor the need for and the effectiveness of various public health interventions.
Although the BRFSS is a useful tool for assessing coronary heart disease and stroke in adult populations, it has some limitations: it excludes people who do not have telephones or are in institutions such as nursing homes; it may under represent people who are severely impaired because of the functional capacity required to participate in the survey; and responses to BRFSS are self-reported and therefore have not been confirmed by a healthcare provider. Despite these limitations, the BRFSS is a uniquely powerful tool to provide the prevalence of coronary heart disease and stroke and related issues among older community-dwelling U.S. adults, due to its large sample size and proven reliability and validity.
The BRFSS is administered and supported by the Division of Population Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. For more information, please visit https://www.cdc.gov/brfss .
- Forman DE, Arena R, Boxer R, et al. Prioritizing functional capacity as a principal end point for therapies oriented to older adults with cardiovascular disease: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2017;135:e894–e918. doi: 10.1161/CIR.0000000000000483
- Kleipool EE, Hoogendijk EO, Trappenburg MC, et al. frailty in older adults with cardiovascular disease: cause, effect or both?. Aging Dis . 2018;9(3):489-497. doi:10.14336/AD.2017.1125.
- Whelton PK, Carey, RM, Aronow WS, et al. 2017 high blood pressure clinical practice guideline: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol . 2018;17(19). doi: 10.1161/HYP.0000000000000066
- National Heart, Lung, and Blood Institute. Health Topics website. https://www.nhlbi.nih.gov/health-topics external icon . Accessed 16 January 2019.
- Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System website. https://www.cdc.gov/brfss . Accessed 16 January 2019.
- O’Keefe JH, O’Keefe EL, Lavie CJ. The goldilocks zone for exercise: not too little, not too much. Mo Med. 2018;115 (2):98-105.
- Taylor CA, Bouldin ED, McGuire LC. Subjective cognitive decline among adults aged ≥45 years — United States, 2015–2016. Rep . 2018;67:753–757. doi:10.15585/mmwr.mm6727a1
- Haring B, Leng X, Robinson J, et al. Cardiovascular disease and cognitive decline in postmenopausal women: results from the Women’s Health Initiative Memory Study. J Am Heart Assoc . 2013;2(6):e000369. Published 2013 Dec 19. doi:10.1161/JAHA.113.000369
- Lutski M, Weinstein G, Goldbourt U, Tanne D. Cardiovascular health and cognitive decline 2 decades later in men with preexisting coronary artery disease. Am J Cardiol . 2018;121(4):410–415. doi:10.1016/j.amjcard.2017.11.003
- The SPRINT MIND Investigators for the SPRINT Research Group. Effect of intensive vs standard blood pressure control on probable dementia: a randomized clinical trial. JAMA . 2019;321(6):553–561. doi:10.1001/jama.2018.21442 Note: Caregiver and Subjective Cognitive Decline (SCD) estimates are based on data collected in 2015-2017 for states that asked these two modules, compared to other topics using only 2017 data.
- Centers for Disease Control and Prevention. Step it Up! The Surgeon General’s Call to Action to Promote Walking and Walkable Communities website. https://www.cdc.gov/physicalactivity/walking/call-to-action/?s_cid=bb-dnpao-calltoaction-002
Disclaimer: The mark “CDC” is owned by the U.S. Department of Health and Human Services (HHS) and is used with permission. Use of this logo is not an endorsement by HHS or the Centers for Disease Control and Prevention (CDC) or any particular product, service, or enterprise.
To receive email updates about Alzheimer's Disease and Healthy Aging, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Search Menu
- Advance Articles
- Editor's Choice
- Braunwald's Corner
- ESC Guidelines
- EHJ Dialogues
- Issue @ a Glance Podcasts
- CardioPulse
- Weekly Journal Scan
- European Heart Journal Supplements
- Year in Cardiovascular Medicine
- Asia in EHJ
- Most Cited Articles
- ESC Content Collections
- Author Guidelines
- Submission Site
- Why publish with EHJ?
- Open Access Options
- Submit from medRxiv or bioRxiv
- Author Resources
- Self-Archiving Policy
- Read & Publish
- Advertising and Corporate Services
- Advertising
- Reprints and ePrints
- Sponsored Supplements
- Journals Career Network
- About European Heart Journal
- Editorial Board
- About the European Society of Cardiology
- ESC Publications
- War in Ukraine
- ESC Membership
- ESC Journals App
- Developing Countries Initiative
- Dispatch Dates
- Terms and Conditions
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, statistical analysis, supplementary data, declarations, data availability, ethical approval, pre-registered clinical trial number.
- < Previous
Artificial intelligence–based assessment of built environment from Google Street View and coronary artery disease prevalence
Zhuo Chen and Jean-Eudes Dazard contributed equally to the study.
Sadeer Al-Kindi and Sanjay Rajagopalan Co-senior authors.
- Article contents
- Figures & tables
- Supplementary Data
Zhuo Chen, Jean-Eudes Dazard, Yassin Khalifa, Issam Motairek, Sadeer Al-Kindi, Sanjay Rajagopalan, Artificial intelligence–based assessment of built environment from Google Street View and coronary artery disease prevalence, European Heart Journal , Volume 45, Issue 17, 1 May 2024, Pages 1540–1549, https://doi.org/10.1093/eurheartj/ehae158
- Permissions Icon Permissions
Built environment plays an important role in the development of cardiovascular disease. Tools to evaluate the built environment using machine vision and informatic approaches have been limited. This study aimed to investigate the association between machine vision–based built environment and prevalence of cardiometabolic disease in US cities.
This cross-sectional study used features extracted from Google Street View (GSV) images to measure the built environment and link them with prevalence of coronary heart disease (CHD). Convolutional neural networks, linear mixed-effects models, and activation maps were utilized to predict health outcomes and identify feature associations with CHD at the census tract level. The study obtained 0.53 million GSV images covering 789 census tracts in seven US cities (Cleveland, OH; Fremont, CA; Kansas City, MO; Detroit, MI; Bellevue, WA; Brownsville, TX; and Denver, CO).
Built environment features extracted from GSV using deep learning predicted 63% of the census tract variation in CHD prevalence. The addition of GSV features improved a model that only included census tract-level age, sex, race, income, and education or composite indices of social determinant of health. Activation maps from the features revealed a set of neighbourhood features represented by buildings and roads associated with CHD prevalence.
In this cross-sectional study, the prevalence of CHD was associated with built environment factors derived from GSV through deep learning analysis, independent of census tract demographics. Machine vision–enabled assessment of the built environment could potentially offer a more precise approach to identify at-risk neighbourhoods, thereby providing an efficient avenue to address and reduce cardiovascular health disparities in urban environments.

Extracted features from street view images via artificial intelligence (AI) demonstrate that 63% of the variation in coronary heart disease (CHD) prevalence can be explained by these environmental factors, highlighting the significant potential of this data in informing cardiovascular health assessments. AIC, Akaike information criterion; BIC, Bayesian information criterion; DSE, demographic and socio-economic; GSV, Google Street View; LMEM: linear mixed-effects model; LRT, likelihood ratio test.
See the editorial comment for this article ‘Artificial intelligence-enhanced exposomics: novel insights into cardiovascular health’, by R. Khera, https://doi.org/10.1093/eurheartj/ehae159 .
This cross-sectional study utilizes deep learning and machine vision to examine the association between the built environment and coronary heart disease at the neighbourhood level. Street view–based built environment factors, analysed using deep learning, explain a significant portion of coronary heart disease prevalence independently of socio-demographics. These findings have implications for targeted interventions, urban planning, and public health policies. Incorporating machine vision–enabled identification of urban features associated with cardiovascular risk can guide the creation of heart-healthy cities, reducing the burden of coronary artery disease and benefiting population health.
Coronary heart disease (CHD) accounts for over 50% of mortality from heart disease in the USA, responsible for nearly 400 000 deaths in 2020. 1 Despite advances in prevention and treatment over the past decade in the USA, 2 CHD remains the leading cause of death in the USA since 1950 with increasing evidence for non-conventional risk factors playing a larger than anticipated role than previously suspected. 1 , 3
Socioenvironmental factors are amongst the leading non-traditional risk factors increasingly implicated in CHD development. 4–6 These factors include social determinants such as race, income, education, and culture as well as the factors in the built environment and factors in the ambient environment such as noise, temperature, and air pollution, all of which have been shown to exert significant effects on CHD. 5–9
Large-scale integrated assessment of the environment at the neighbourhood level can facilitate rapid and complete assessment of its impact on CHD. Such data are however scarce, partly because of the costly and time-consuming nature of neighbourhood audits and inconsistent measurements and standards for data collection. Machine vision approaches such as Google Street View (GSV) have become an increasingly popular approach for virtual neighbourhood audits since its launch in 2007. Google Street View image coverage has been consistently expanding in recent years achieving almost full coverage in the USA. 10 Previous studies have shown GSV results are comparable with field assessments and have been used to assess the built environment features such as greenspace, 11 , 12 buildings, 13 and roads. 14
Google Street View images have gained popularity as a preferred data source for large-scale studies due to the widespread availability of this data set. It represents one of the largest repositories for machine vision–enabled assessments of extensive geographical areas, facilitated by standardized data collection approaches. Deep learning approaches such as convolutional neural networks (CNN) have been widely used in many studies and applications, given their excellent performance in tasks such as image classification, object detection, and image segmentation. 15 The use of such approaches to rapidly assess and extract built environment features from GSV images using deep learning can help facilitate integrated assessment and capture other aspects that may not be otherwise included. The goal of this study is to use GSV images to assess the built environment and use them to estimate CHD prevalence at the census tract level.
The University Hospitals Institutional Review Board exempted this cross-sectional study from review and the need for informed consent in accordance with 45 CFR §46, as the data were deidentified and thus not considered human participant research.
Data source for coronary heart disease
The prevalence of census tract CHD was obtained from the 2018 Centers for Disease Control and Prevention (CDC) Population Level Analysis and Community Estimates (PLACES), a project that provided chronic disease risk factors, health outcomes, and clinical preventive services. This project, a collaboration between the CDC Foundation and the Robert Wood Johnson Foundation, measures CHD prevalence using data (2015, 2016) from Behavioral Risk Factor Surveillance System (BRFSS), where people aged ≥18 are surveyed to report whether or not they have been told by a doctor, nurse, or other health professional that they had angina or CHD. We collected the CHD prevalence data for 789 census tracts in seven cities: Bellevue, WA; Brownsville, TX; Cleveland, OH; Denver, CO; Detroit, MI; Fremont, CA; and Kansas City, KS. For each city, we calculated the mean CHD prevalence and its interquartile range (IQR), showing the range within which the middle 50% of prevalence lies. The seven-city selection relies on population, disease burden, and geography, as outlined in the online supplementary material .
Google Street View data
Environment information was derived from ∼0.53 million GSV images for the seven cities (143 K for Detroit, 59 K for Kansas City, 70 K for Cleveland, 65 K for Brownsville, 38 K for Fremont, 35 K for Bellevue, and 120 K for Denver). The GSV images were downloaded via GSV static application programming interface (API) from 2020 to 2021. Google Street View API provides users with street-level panoramic imagery which captures the visual domain of pedestrians in thousands of cities worldwide. The GSV images of each census tract were downloaded in a grid pattern in the corresponding tract with an interval of 100 m. At each location where GSV images were retrieved, four images were gathered from different directions (i.e. the cardinal directions: N, E, S, and W), which composes a panoramic view of the surroundings at that location. When latitude and longitude coordinates are provided, the API searches within a 50 m radius for a photograph closest to this location. The API would not return any images if no available images could be found.
To process these images and gain environment information from them, a pre-trained deep CNN (DCNN) Places365 CNN 16 was used as the feature extractor to obtain the deep features of the image. Here, the deep features are the outputs of the deep layers in the hierarchy of the network. Compared with the shallow features in the shallow layers, these deep features represent the semantic information of the GSV images. Details of how the extraction was performed can be found in Supplementary data online , Figure S1 . We used Places365 CNN as the feature extractor because the images trained on Places365 CNN are more similar to that of GSV. Places365 CNN was trained on the subset of Places Database, which contains more than 10 million images consisting of 400+ unique scene categories such as towers, soccer fields, streets, swimming pools, and train station platforms. Compared with the ImageNet database, the diversity of environmental features found in the Places Database was believed to be representative of what is contained in GSV images. Through feature extraction, we obtained 4096 features representing the average built environment information for each census tract. It is noteworthy that Google emphasizes considering various factors, including weather conditions, in their image acquisition process. 10 Additionally, upon examination of our data set, only a very small proportion of the images were captured under conditions where only a limited amount of snow was present, with the observation that this has minimal influence on the computer vision algorithm.
Traditional demographics, socio-economic factors, and composite indices for social determinant of health
In addition to the GSV features, we obtained traditional demographic and socio-economic (DSE) factors: age (median), sex (male %), race (Black %), income (median $), and education (<high school %) from the 2018 American Community Survey 5-year estimates. 17 We also collected the established composite indices for social determinants of health (SDoH). Specifically, we considered three widely used SDoH indices: 2018 Social Deprivation Index (SDI), 18 2015 Area Deprivation Index (ADI), 19 and 2018 Social Vulnerability Index (SVI). 20 Social Deprivation Index, provided by Robert Graham Center, is a composite measure capturing seven demographic characteristics gathered from the American Community Survey to assess the overall socio-economic disparities at the area level. In contrast, ADI focuses on either the state or national level, ranking socio-economic (e.g. income, education, employment, and housing quality) disadvantage in those neighbourhoods. Additionally, CDC’s SVI provides insights into the vulnerability of communities by considering socio-economic status, housing, transportation, and other factors. These composite indices collectively contribute to a nuanced understanding of the SDoH in a neighbourhood.
Machine learning model using raw convolutional neural network–extracted features
We utilized three machine learning (ML) models to explore the association between the raw (4096) CNN-extracted features of GSV images and the tract-level CHD prevalence. The models for this analysis included extratrees regressor (ET), 21 random forest regressor (RF), 22 and light gradient boosted machine regressor (LGBM). 23 All models were estimated using a 10-fold cross-validation technique for a more robust result. For 10-fold cross-validation, the data set is split into 10 equal-sized subsets, and the model is trained on 9 subsets and tested on the remaining 1 subset. This process is repeated 10 times until all 10 subsets were used once as the testing set. R 2 values were reported as the model quality, quantifying the extent to which the CNN-extracted features of GSV images fit tract-level CHD prevalence. The performance of each model was also evaluated using the mean absolute error (MAE) and root mean squared error (RMSE).
Multilevel modelling with traditional demographics, socio-economic factors, and composite indices for social determinant of health
We analysed the effects of common DSE factors as well as CNN-extracted features of GSV images associated with the CHD. Details of this analysis are provided in the online supplementary material . Briefly, we followed an entirely supervised two-step modelling strategy. In the first step, a multivariate sparse partial least squares (SPLS) regression 24 was applied to the CNN-extracted features to reduce the dimensionality issue and the effect of noise on the error rates of our inferences. In the second step, we compare the effects of CNN-extracted features with recognized factors by building multilevel regression models allowing to account for both fixed and random effects. Specifically, linear mixed-effect regression models were fitted with the first few selected SPLS components augmented with DSE factors as well as other composite indices for SDoH, all treated here as fixed effects, and where city was treated as a random effect. The models were all adjusted for fixed effects including age, sex, race, income, and education. We then compared the regression estimates and goodness-of-fit measures between the reduced models and the combined linear mixed-effects models (LMEMs), where each set of independent variables enter simultaneously or individually. Two sets of three models were compared in this analysis: (i) a model containing both DSE factors and SPLS components (DSE + GSV model), (ii) a model with DSE factors alone (DSE model), and (iii) a model with the SPLS components alone (GSV model). Similarly, we compared three other models: (i) a model that incorporated the three SDoH indices alongside SPLS components (SDoH + GSV model), (ii) a model comprising only the three SDoH indices (SDoH model); and (iii) a model solely featuring the SPLS components (GSV model). In all comparisons, model performance was assessed using goodness-of-fit measures such as likelihood ratios tests (as it applied), Akaike information criterion (AIC) and Bayesian information criterion (BIC) criteria, as well as marginal and conditional R 2 values based on Nakagawa’s R 2 for mixed models. 25 For each model, we calculated the coefficient estimate of each variable with its standard error and confidence intervals (CI), the intraclass (within city) correlation coefficient (ICC) for the city random effects, the within-city random-effect residual variance (σ 2 ), and the between-city random-effect residual variance (τ 00 City ) to assess the reliability or consistency of the measurements. All P -values less than the α = 0.05 level were considered significant.
Features visualization using Grad-CAM
To understand the deep features of the GSV images that are associated with neighbourhood CHD prevalence, we identified the most influential GSV features contributing to the SPLS components. These top features were discerned by examining the magnitudes and signs of their coefficients in the SPLS regression model, thus helping to understanding how each feature is associated with CHD prevalence. Subsequently, we employed the Grad-CAM technique 26 to create the saliency map to highlight these prominent features in the original GSV images. This process provides certain explanations of what environmental features the CNN thinks to be associated with neighbourhood CHD prevalence.
In our study, we employed Python (version 3.8.10) for deep learning and ML tasks, utilizing packages such as PyTorch (version 1.8.2), fastai (version 2.6.3), and scikit-learn (version 1.0.2). For multilevel modelling, we used R (version 4.2.1), spls (version 2.2–3), and library lmer (version 1.1–35.1).
Seven cities revealed varying levels of CHD prevalence at the census tract level. In Bellevue, the median CHD prevalence (%) was 4.70 (IQR: 3.75–5.23), whereas in Brownsville, it was 7.70 (IQR: 6.48–8.63). Cleveland exhibited a median CHD prevalence of 8.70 (IQR: 7.35–10.00). Denver had a median CHD prevalence of 4.30 (IQR: 3.45–5.20), while Detroit’s median CHD prevalence was 8.55 (IQR: 7.40–9.80). Fremont displayed a median CHD prevalence of 3.70 (IQR: 3.35–4.10), and Kansas City reported a median CHD prevalence of 7.20 (IQR: 6.10–8.30).
Machine learning model results with raw convolutional neural network features
The 4096 CNN-extracted features from GSV images were able to explain more than 63% of the variance ( R 2 = 0.634) on the tract-level CHD prevalence in seven cities ( Figure 1 ). The three ML models had the similar performance, with the ET achieving the best result among all models with the lowest average MAE of 1.11 and RMSE of 1.58 (see Supplementary data online , Table S1 ). The actual estimate from CDC’s CHD prevalence and the model-predicted CHD prevalence were mapped for all census tracts in seven cities ( Figure 2 ). There was a good agreement between the actual estimates and predicted CHD prevalence across all census tracts in seven cities. We found a small number of extreme values that were underestimated by the models in certain census tracts of Detroit and Cleveland. The CHD prevalence of these underestimated census tracts was often more than 12%. When examining the CNN-extracted features using t-SNE, we noticed clustering of census tracts with similar values of CHD prevalence (see Supplementary data online , Figure S2 ).

Actual estimates (observed) and predicted CHD prevalence. A total of 789 census tracts in seven cities were analysed. Predicted CHD prevalence was from LGBM model trained using CNN-extracted features. The black dotted line represents the y = x line. Values are in percentage. CHD, coronary heart disease; CNN, convolutional neural network; LGBM, light gradient boosted machine

Maps of actual estimates (left) and predicted (right) CHD prevalence. The predicted CHD prevalence is obtained by averaging the results from 100 random trials based on k -fold cross-validation (with k = 10). Values are in percentage. Maps are not on the same scale. CHD, coronary heart disease
Comparison of Google Street View–sparse partial least square components with demographics and socio-economic factors
With SPLS, an optimal model was obtained with h = 6 SPLS components ( η = 0.6), yielding a model with 883 CNN-extracted features that explains R X Y 2 > 64.8% variance of CHD prevalence in the census tracts (see Supplementary data online , Figure S3 ). We found that the combined model (DSE + GSV) demonstrated a better goodness of fit, with statistically significant higher log-likelihood, lower AIC/BIC, and higher R 2 (conditional R 2 = 0.792) when compared with GSV and notably DSE model alone ( Table 1 ). The DSE model had lower AIC and BIC values, with a significant LRT, and higher R 2 when compared with the GSV model ( Table 1 ). Supplementary data online , Table S2 , presents the regression estimates and analysis of variance (ANOVA) results. Notably, four out of six GSV–SPLS components demonstrated statistical significance, while all DSE variables are statistically significant.
Model performance and comparison of linear mixed-effects models for coronary heart disease prevalence: Google Street View and demographic and socio-economic variables
Models: GSV, the LMEM with only the selected SPLS components (CHD: h = 6 obtained from the 4096 CNN features); DSE, the LMEM with only the demographics and socio-economic variables (city + sex + age + race + income + education); and GSV + DSE, the LMEM with both sets of independent variables from GSV and DSE.
LMEM, linear mixed-effects model; GSV, Google Street View; AIC, Akaike information criterion; BIC, Bayesian information criterion; LRT, likelihood ratio test.
Comparison of Google Street View–sparse partial least square components with social determinant of health indices
As expected, the LMEM that incorporates both GSV–SPLS components and SDoH indices, referred to as SDoH + GSV, achieved the best goodness of fit and overall performance. It exhibited the lowest AIC/BIC and the highest log-likelihood and marginal/conditional R 2 (conditional R 2 = 0.785), compared with GSV and notably SDoH model alone ( Table 2 ). Remarkably, the SDoH model performance was comparable with the GSV model with non-significant LRT ( P = .60), while AIC/BIC criteria and R 2 remained not significantly different. All three SDoH indices were statistically significant in the models, and the three GSV–SPLS components were statistically significant when adjusting for either DSE variables (see Supplementary data online , Table S2 ) or SDoH indices (see Supplementary data online , Table S3 ).
Model performance and comparison of linear mixed-effects models for coronary heart disease prevalence: Google Street View and social determinants of health indices
Models: GSV, the LMEM with only the selected SPLS components (CHD: h = 6 obtained from the full CNN features); SDoH, the LMEM with only the SDoH indices (SDI + SVI + ADI); and GSV + SDoH, the LMEM with both sets of independent variables from GSV and SDoH.
LMEM, linear mixed-effects model; GSV, Google Street View; AIC, Akaike information criterion; BIC, Bayesian information criterion; LRT, likelihood ratio test; SDOH, social determinants of health; SDI, Social Deprivation Index; SVI, Social Vulnerability Index; ADI, Area Deprivation Index.
Visualization of the most influential convolutional neural network–Google Street View features
Grad-CAM was utilized to visualize top CNN-extracted features identified from SPLS regression. The saliency maps generated by the Grad-CAM suggested that feature #2017, which seemed to highlight deteriorated buildings (suggesting neighbourhood blight), had a positive association with CHD prevalence ( Figure 3A ). Interestingly, other images for feature #2017 seemed to also highlight wooden utility poles (see Supplementary data online , Figure S4 ). Another feature (feature #458) that was positively associated with CHD was found to be highlighting road cracks as shown in Figure 3B . In contrast, feature #2873 in Figure 3C had a negative association with CHD prevalence, and its heatmap highlighted trees along the road. Feature #237, seeming to focus on well-built houses, also had a negative association with CHD prevalence ( Figure 3D ). More examples of Grad-CAM on the CNN-extracted GSV features are provided in the Supplementary data online , Figures S4–S8 , with ‘noises’.

Feature interpretations using Grad-CAMs. ( A and B ) Two pairs of GSV images (left) and their activation maps (right) for the features associated with higher CHD prevalence. ( C and D ) Two pairs of GSV images (left) and their activation maps (right) for the features associated with lower CHD prevalence. CHD, coronary heart disease; Grad-CAMs, gradient-weighted class activation mapping; GSV, Google Street View
While many epidemiological studies have examined associations between cardiovascular disease and individual built environmental features (e.g. greenspace, urban architecture, street connectivity, and food availability), our approach focused on machine vision–derived physical environment, relying on CNN and its related techniques to extract features.
Our results showed a strong model fit ( R 2 = 0.634), indicating that the raw CNN-extracted features from GSV images effectively predict CHD prevalence at the census tract level in seven cities ( Structured Graphical Abstract ). This indicated that the CNN-extracted features could capture neighbourhood features related to cardiovascular health. The predicted CHD prevalence using CNN-extracted features tended to be underestimated in certain areas compared with observed CHD prevalence especially in Detroit and Cleveland. This may be caused by the limited number of samples for these extreme values in the data set; the model may struggle to accurately distinguish and predict such rare occurrences. This may also suggest that certain CHD-related factors may either not be embedded in these environments at these locations or that perhaps features not captured by street view images, such as demographic factors, ambient factors, and other demographic and traditional variables, may play a much larger role in these environments.
Previous studies have used CNN to detect pre-defined built environmental features from GSV and found that dilapidated buildings and visible wires were associated with an increased risk of cardiovascular diseases. 27 , 28 Our approach employed a data-driven approach, taking the advantage of the knowledge that fully connected layers in the CNN contain condensed information of the input imagery that can be extracted and utilized for a variety of purposes. We utilized a pre-trained DCNN Places365 CNN, 16 so that the deep features from the CNN may be more representative of the built environment. One advantage of this approach is that pre-defined relevant features in the built environment are not required. The 4096-dimensional deep features embed all essential information of the built environment in the imagery so that we could retain relevant features as much as reasonably possible. Conversely, the disadvantage of using deep features from a pre-trained CNN is that it becomes difficult to identify corresponding physical features that impact CHD at the neighbourhood level. To alleviate this issue and provide certain interpretations of the deep features, we utilized Grad-CAM techniques to visualize the CHD-related features with a saliency map.
The results of multilevel modelling using demographics and socio-economic factors indicate that DSE variables were still better predictors of CHD prevalence than GSV features. One explanation is obviously the fact that physical environmental feature even if they represent a ‘meta’ framework for other mediators may not be sufficient to convey the risk conveyed by other factors which may be sparsely represented. However, by incorporating GSV features into the model with regular DSE variables, one could help improve the prediction of CHD prevalence at the neighbourhood level ( Table 1 ). Further comparisons between GSV features and existing SDoH indices reveal that GSV features can be on par with these established SDoH indices. Given the fact that these existing composite indices encompass a wild variety of social economic and environmental factors, our single-source GSV features offer a valuable and efficient perspective on the built environment’s potential impact on health outcomes. Our results further suggest that GSV features indeed may be helpful in highlighting specific built environment information related to CHD prevalence at the neighbourhood level as illustrated by Grad-CAM methods, which provided a potential way of identifying built environment information.
Grad-CAM highlighted several potential built environment features that are either associated with higher or lower CHD at the neighbourhood level. Deteriorated houses and roads are a feature of urban blight associated with higher CHD. This feature may in turn embody other features in the neighbourhood that drive cardiovascular risk, including lack of space for physical activity, 7 , 29 limited access to nutritionally balanced food, 30 and lack of access to health care. 31 Street greenery on the other hand was highlighted as associated with lower CHD prevalence. This agrees with previous studies that showed a robust association between green space and decreased cardiovascular risks. 32 , 33 It should be noted that some Grad-CAM results on a feature revealed different representations of built environment features. For instance, the feature that highlighted deteriorated houses also highlighted wooden utility poles in the images (see Supplementary data online , Figure S4 ). Other features may show combined physical features, an exemplified in Supplementary data online , Figure S8 , where it seemed to show an amalgamation of tree canopy and nearby sky. This analysis identifies potential environmental features correlated with CHD, but it is crucial to note that these correlations do not establish causality. It is possible that underlying factors such as socio-economic status, which might influence living conditions and health behaviours, play a significant role in these observed correlations.
Implications
Our study carries significant implications for the field of health research clinical practice. Firstly, we have pioneered the utilization of street view features in assessing cardiovascular risk, marking a novel approach that introduces new dimensions to our comprehension of the impact of the built environment on health. Furthermore, our research, while primarily conducted at the census tract level, holds the potential for analysis at an even more granular level, down to the level of individual patients. This extended analysis could yield highly precise and personalized insights into the intricate interplay between the built environment and individual health, thereby enabling tailored interventions and healthcare strategies. As we look ahead, future research in this field may explore advanced methods such as semantic segmentation to extract specific built environment features, including elements like green space, blue space, and sidewalks. This approach promises a more intricate understanding of how the environment influences cardiovascular health, offering an avenue for even more finely targeted interventions in public health.
Our findings also underscore the utility of such data in broadening our understanding of environmental influences on health. The associations identified between street view features and cardiovascular risk not only open avenues for generating new hypotheses but also serve as a valuable reference for shaping public health policies. These insights, while emphasizing correlations, guide us in identifying potential areas for intervention and in designing studies aimed at exploring causal relationships. This approach, therefore, contributes to a more informed and targeted strategy in public health planning, with a focus on mitigating cardiovascular risks associated with specific environmental factors.
Study limitations
There are multiple limitations of this study that should be noted. Firstly, the GSV images used in the study are only available along major streets and roads, and there are some populations who do not live in such neighbourhoods. However, given the fact that most population live around the urban neighbourhood where GSV are abundant, we believe this would not significantly affect the results for majority of census tracts. Further, although Places365 database contains 400+ unique scene categories, it may not include all features that can be found in the built environment. Small objects such as trash, other environmental pollutants, and physical domains that may translate into better urban quality of life may be difficult for computer vision techniques like CNN to detect in a GSV image. 34 It's important to note that interpreting Grad-CAM maps can involve a degree of speculation, and the visualizations may not always provide a definitive understanding of the exact features being detected by the model. Additionally, the census tracts with CHD prevalence data are from seven representative US cities of CDC PLACES data set and may not generalize to all census tracts in the USA, especially rural areas. 35 Future work is needed to examine the disparities of urban and rural areas and its cardiovascular-related built environment features.
Built environment impacts cardiovascular health outcome. In this study, we used GSV and a scene-pre-trained CNN to assess the built environment. We found CNN-extracted features explain significant portion of CHD prevalence at the census tract level. Compared with traditional DSE factors or composite indices for SDoH, GSV provides unique information that may relate to CHD such as buildings, greenspace, and roads as suggested by the activation maps from Grad-CAM technique. The outcomes of our study provide proof of concept for machine vision–enabled identification of urban network features associated with risk that in principle may enable rapid identification and targeting interventions in at-risk neighbourhoods to reduce cardiovascular burden.
Supplementary data are available at European Heart Journal online.
Disclosure of Interest
All authors declare no disclosure of interest for this contribution.
The data used in this analysis are publicly available. The analytic code can be made available upon request.
This work was funded by the National Institute on Minority Health and Health Disparities Award nos. P50MD017351 and 1R35ES031702-01 awarded to S.R.
Ethical approval was not required.
None supplied.
Tsao CW , Aday AW , Almarzooq ZI , Alonso A , Beaton AZ , Bittencourt MS , et al. Heart disease and stroke statistics—2022 update: a report from the American Heart Association . Circulation 2022 ; 145 : e153 – 639 . https://doi.org/10.1161/CIR.0000000000001052
Google Scholar
Health, United States, Annual Perspective, 2020–2021 [Internet]. National Center for Health Statistics (U.S.); 2022 [cited 2023 Feb 2]. Available from: https://stacks.cdc.gov/view/cdc/122044 .
Heron M , Anderson RN . Changes in the leading cause of death: recent patterns in heart disease and cancer mortality . NCHS Data Brief 2016 ; 254 : 1 – 8 . https://pubmed.ncbi.nlm.nih.gov/27598767/
Havranek EP , Mujahid MS , Barr DA , Blair IV , Cohen MS , Cruz-Flores S , et al. Social determinants of risk and outcomes for cardiovascular disease . Circulation 2015 ; 132 : 873 – 98 . https://doi.org/10.1161/CIR.0000000000000228
Al-Kindi SG , Brook RD , Biswal S , Rajagopalan S . Environmental determinants of cardiovascular disease: lessons learned from air pollution . Nat Rev Cardiol 2020 ; 17 : 656 – 72 . https://doi.org/10.1038/s41569-020-0371-2
Bhatnagar A . Environmental determinants of cardiovascular disease . Circ Res 2017 ; 121 : 162 – 80 . https://doi.org/10.1161/CIRCRESAHA.117.306458
Sallis JF , Floyd MF , Rodríguez DA , Saelens BE . Role of built environments in physical activity, obesity, and cardiovascular disease . Circulation 2012 ; 125 : 729 – 37 . https://doi.org/10.1161/CIRCULATIONAHA.110.969022
Liu J , Varghese BM , Hansen A , Zhang Y , Driscoll T , Morgan G , et al. Heat exposure and cardiovascular health outcomes: a systematic review and meta-analysis . Lancet Planet Health 2022 ; 6 : e484 – 95 . https://doi.org/10.1016/S2542-5196(22)00117-6
Rajagopalan S , Landrigan PJ . Pollution and the heart . N Engl J Med 2021 ; 385 : 1881 – 92 . https://doi.org/10.1056/NEJMra2030281
Google . Google Maps Street View. [cited 2023 Feb 2]. How Street View works and where we will collect images next. Available from: https://www.google.com/streetview/how-it-works/ .
Seiferling I , Naik N , Ratti C , Proulx R . Green streets − quantifying and mapping urban trees with street-level imagery and computer vision . Landsc Urban Plan 2017 ; 165 : 93 – 101 . https://doi.org/10.1016/j.landurbplan.2017.05.010
Lu Y . Using Google Street View to investigate the association between street greenery and physical activity . Landsc Urban Plan 2019 ; 191 : 103435 . https://doi.org/10.1016/j.landurbplan.2018.08.029
Kang J , Körner M , Wang Y , Taubenböck H , Zhu XX . Building instance classification using street view images . ISPRS J Photogramm Remote Sens 2018 ; 145 : 44 – 59 . https://doi.org/10.1016/j.isprsjprs.2018.02.006
Nagata S , Nakaya T , Hanibuchi T , Amagasa S , Kikuchi H , Inoue S . Objective scoring of streetscape walkability related to leisure walking: statistical modeling approach with semantic segmentation of Google Street View images . Health Place 2020 ; 66 : 102428 . https://doi.org/10.1016/j.healthplace.2020.102428
LeCun Y , Bengio Y , Hinton G . Deep learning . Nature 2015 ; 521 : 436 – 44 . https://doi.org/10.1038/nature14539
Zhou B , Lapedriza A , Khosla A , Oliva A , Torralba A . Places: a 10 million image database for scene recognition . IEEE Trans Pattern Anal Mach Intell 2018 ; 40 : 1452 – 64 . https://doi.org/10.1109/TPAMI.2017.2723009
Bureau UC . Census.gov . [cited 2023 Jun 29]. American Community Survey 5-year data (2009–2021). Available from: https://www.census.gov/data/developers/data-sets/acs-5year.html .
Robert Graham Center—Policy Studies in Family Medicine & Primary Care . Social Deprivation Index (SDI) [Internet]. 2018 [cited 2023 Jun 30]. Available from: https://www.graham-center.org/content/brand/rgc/maps-data-tools/social-deprivation-index.html .
Kind AJH , Buckingham WR . Making neighborhood-disadvantage metrics accessible—the neighborhood atlas . N Engl J Med 2018 ; 378 : 2456 – 8 . https://doi.org/10.1056/NEJMp1802313
Flanagan BE , Gregory EW , Hallisey EJ , Heitgerd JL , Lewis B . A social vulnerability index for disaster management . J Homel Secur Emerg Manag 2011 ; 8 :0000102202154773551792. https://doi.org/10.2202/1547-7355.1792
Geurts P , Ernst D , Wehenkel L . Extremely randomized trees . Mach Learn 2006 ; 63 : 3 – 42 . https://doi.org/10.1007/s10994-006-6226-1
Breiman L . Random forests . Mach learn 2001 ; 45 : 5 – 32 . https://doi.org/10.1023/A:1010933404324
Ke G , Meng Q , Finley T , Wang T , Chen W , Ma W , et al. Lightgbm: a highly efficient gradient boosting decision tree . Adv Neural Inf Process Syst 2017 ; 30 : 3149 – 3157 . https://papers.nips.cc/paper_files/paper/2017/hash/6449f44a102fde848669bdd9eb6b76fa-Abstract.html
Chun H , Keleş S . Sparse partial least squares regression for simultaneous dimension reduction and variable selection . J R Stat Soc Series B Stat Methodol 2010 ; 72 : 3 – 25 . https://doi.org/10.1111/j.1467-9868.2009.00723.x
Nakagawa S , Johnson PCD , Schielzeth H . The coefficient of determination R2 and intra-class correlation coefficient from generalized linear mixed-effects models revisited and expanded . J R Soc Interface 2017 ; 14 : 20170213 . https://doi.org/10.1098/rsif.2017.0213
Selvaraju RR , Cogswell M , Das A , Vedantam R , Parikh D , Batra D . Grad-CAM: visual explanations from deep networks via gradient-based localization . In: Proceedings of the IEEE International Conference on Computer Vision , 2017 , p. 618 – 26 .
Phan L , Yu W , Keralis JM , Mukhija K , Dwivedi P , Brunisholz KD , et al. Google Street View derived built environment indicators and associations with state-level obesity, physical activity, and chronic disease mortality in the United States . Int J Environ Res Public Health 2020 ; 17 : 3659 . https://doi.org/10.3390/ijerph17103659
Nguyen TT , Nguyen QC , Rubinsky AD , Tasdizen T , Deligani AHN , Dwivedi P , et al. Google Street View-derived neighborhood characteristics in California associated with coronary heart disease, hypertension, diabetes . Int J Environ Res Public Health 2021 ; 18 : 10428 . https://doi.org/10.3390/ijerph181910428
Chandrabose M , Rachele JN , Gunn L , Kavanagh A , Owen N , Turrell G , et al. Built environment and cardio-metabolic health: systematic review and meta-analysis of longitudinal studies . Obes Rev 2019 ; 20 : 41 – 54 . https://doi.org/10.1111/obr.12759
Gondi KT , Larson J , Sifuentes A , Alexander NB , Konerman MC , Thomas KS , et al. Health of the food environment is associated with heart failure mortality in the United States . Circ Heart Fail 2022 ; 15 : e009651 . https://doi.org/10.1161/CIRCHEARTFAILURE.122.009651
White-Williams C , Rossi LP , Bittner VA , Driscoll A , Durant RW , Granger BB , et al. Addressing social determinants of health in the care of patients with heart failure: a scientific statement from the American Heart Association . Circulation 2020 ; 141 : e841 – 63 . https://doi.org/10.1161/CIR.0000000000000767
Pereira G , Foster S , Martin K , Christian H , Boruff BJ , Knuiman M , et al. The association between neighborhood greenness and cardiovascular disease: an observational study . BMC Public Health 2012 ; 12 : 466 . https://doi.org/10.1186/1471-2458-12-466
Mitchell R , Popham F . Effect of exposure to natural environment on health inequalities: an observational population study . Lancet 2008 ; 372 : 1655 – 60 . https://doi.org/10.1016/S0140-6736(08)61689-X
Ross CE , Mirowsky J . Disorder and decay: the concept and measurement of perceived neighborhood disorder . Urban Aff Rev 1999 ; 34 : 412 – 32 . https://doi.org/10.1177/107808749903400304
Loccoh EC , Joynt MKE , Wang Y , Kazi DS , Yeh RW , Wadhera RK . Rural-urban disparities in outcomes of myocardial infarction, heart failure, and stroke in the United States . J Am Coll Cardiol 2022 ; 79 : 267 – 79 . https://doi.org/10.1016/j.jacc.2021.10.045
Author notes
- coronary arteriosclerosis
- artificial intelligence
- heart disease risk factors
- coronary heart disease
- neighborhood
- machine learning
- deep learning
- convolutional neural networks
- built environment
- census tract
Email alerts
Companion article.
- Artificial intelligence-enhanced exposomics: novel insights into cardiovascular health
Related articles in pubmed, citing articles via, looking for your next opportunity, affiliations.
- Online ISSN 1522-9645
- Print ISSN 0195-668X
- Copyright © 2024 European Society of Cardiology
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Perceived Interpersonal Racism in Relation to Incident Coronary Heart Disease Among Black Women
Affiliations.
- 1 Slone Epidemiology Center at Boston University, MA (S.S., J.R.P., Y.C.C., L.R.).
- 2 Cook County Health, Chicago, IL (M.B.).
- 3 The University of California at San Francisco (M.A.A.).
- 4 Boston University School of Public Health, MA (Y.C.C.).
- PMID: 38235551
- PMCID: PMC10926238 (available on 2025-02-13 )
- DOI: 10.1161/CIRCULATIONAHA.123.066471
Background: Racism is highly prevalent in the United States. Few data exist about whether perceived interpersonal racism is associated with risk of coronary heart disease (CHD).
Methods: We followed 48 305 participants in the Black Women's Health Study through biennial mailed and Internet-based health questionnaires from 1997, when they provided information on perceived interpersonal racism and were free of cardiovascular disease and cancer, until the end of 2019. We averaged participant responses to 5 validated questions about perceived interpersonal racism in everyday activities, such as "people act as if they think you are dishonest." We summed the positive responses to 3 questions about perceived racism in interactions that involved jobs, housing, and police; scores ranged from 0 (no to all) to 3 (yes to all). CHD cases were defined as nonfatal myocardial infarctions confirmed through medical records, fatal cases identified through the National Death Index, and self-reported revascularization events. We used Cox proportional hazard models adjusting for major confounders to estimate hazard ratios (HRs).
Results: During 22 years of follow-up, we identified 1947 incident CHD cases. For women who reported experiences of racism in employment, housing, or involving the police relative to women who reported no such experiences, the age-adjusted HR for CHD was 1.35 (95% CI, 1.13-1.61; P trend =0.006), and the multivariable HR for CHD was 1.26 (95% CI, 1.05-1.51; P trend =0.05). For women in the highest quartile of perceived interpersonal racism in daily life relative to women in the lowest quartile, the age-adjusted HR for CHD was 1.25 (95% CI, 1.07-1.46; P trend =0.006). After multivariable adjustment, the HR was attenuated and no longer statistically significant.
Conclusions: Perceived experiences of interpersonal racism in employment, in housing, and with the police were associated with higher incidence of CHD among Black women, whereas perceived racism in everyday life was not associated with higher risk.
Keywords: Black or African American; coronary disease; myocardial infarction; racism; women.
Publication types
- Research Support, N.I.H., Extramural
- Black People
- Coronary Disease* / epidemiology
- Myocardial Infarction* / epidemiology
- Risk Factors
- United States / epidemiology
- Women's Health
Grants and funding
- R01 CA058420/CA/NCI NIH HHS/United States
- R01 MD015085/MD/NIMHD NIH HHS/United States
- U01 CA164974/CA/NCI NIH HHS/United States
Study record managers: refer to the Data Element Definitions if submitting registration or results information.
Search for terms

- Advanced Search
- See Studies by Topic
- See Studies on Map
- How to Search
- How to Use Search Results
- How to Find Results of Studies
- How to Read a Study Record

- Learn About Studies
- Other Sites About Studies
- Glossary of Common Site Terms

- Submit Studies to ClinicalTrials.gov PRS
- Why Should I Register and Submit Results?
- FDAAA 801 and the Final Rule
- How to Apply for a PRS Account
- How to Register Your Study
- How to Edit Your Study Record
- How to Submit Your Results
- Frequently Asked Questions
- Support Materials
- Training Materials

- Selected Publications
- Clinical Alerts and Advisories
- Trends, Charts, and Maps
- Downloading Content for Analysis

- ClinicalTrials.gov Background
- About the Results Database
- History, Policies, and Laws
- ClinicalTrials.gov Modernization
- Media/Press Resources
- Linking to This Site
- Terms and Conditions
- Search Results
- Study Record Detail

Cardiovascular-Renal Adverse Prognosis Assessment System for Coronary Heart Disease With Chronic Kidney Disease Based on Metabolomics (CRUISE-MET)
- Study Details
- Tabular View
- No Results Posted

Coronary heart disease (CHD) combined with chronic kidney disease (CKD) affects a substantial portion of the population and carries a significant disease burden, often leading to poor outcomes. Despite efforts to strictly control traditional risk factors, the efficacy in improving outcomes for patients with both CHD and CKD has been limited. Recent advancements in lipid metabolism research have identified new lipid metabolites associated with the occurrence and prognosis of CHD and CKD. Our preliminary trial has shown that levels of certain lipid metabolites, such as Cer(18:1/16:0), HexCer(18:1/16:0), and PI(18:0/18:1), are notably elevated in patients with CHD and reduced kidney function compared to those with relatively normal kidney function. This suggests that dysregulation of these non-traditional lipid metabolites may contribute to residual risk for adverse outcomes in these patients.
Furthermore, the emerging concept of "cardiovascular-kidney-metabolic syndrome" and the availability of new treatment options highlight the urgent need for a risk stratification tool tailored to modern management strategies and treatment goals to guide preventive measures effectively. To address this, we propose to conduct a prospective cohort study focusing on CHD combined with CKD. This study aims to comprehensively understand the clinical characteristics, diagnosis, treatment status, and cardiovascular-kidney prognosis in these patients. Through advanced metabolomics analysis, we seek to identify lipid metabolism profiles and non-traditional lipid metabolites associated with the progression of coronary artery disease in CHD-CKD patients. Leveraging clinical databases and metabolomics data, we will develop a robust risk prediction model for adverse cardiovascular-kidney outcomes, providing valuable guidance for clinical diagnosis, treatment decisions, and ultimately improving patient prognosis.

- Diagnostic Test: lipid metabolomics Extract 4 milliliters of fasting peripheral venous blood from enrolled patients for targeted lipid metabolism metabolomics research. Utilize a liquid chromatography-tandem mass spectrometry (LC-MS/MS) system to conduct metabolomics analysis on patient blood samples.
Cardiovascular adverse events includes Cardiovascular-related death, non-fatal myocardial infarction, non-fatal stroke, repeat revascularization, rehospitalization for heart failure.
- Cardiovascular events related to mortality: This includes 1) cardiovascular death; 2) death caused by stroke; 3) death resulting from cardiovascular surgery; 4) death from other cardiovascular causes.
- Cardiovascular death: During the follow-up period, this refers to death directly associated with documented myocardial infarction, heart failure, or arrhythmia. It also includes death events where the cause is unclear and not attributed to any other underlying conditions.
- Repeat revascularization is any unplanned repeat revascularization of either a target vessel or non-target vessel or CABG;
Renal composite endpoint event includes renal failure, renal-related death, or a decrease in eGFR >40% from baseline (confirmed by a second test 4 weeks later).
- Renal failure: End-stage kidney disease (ESKD) or eGFR persistently below 15 ml/min/1.73 m².
- End-stage kidney disease: Receiving renal replacement therapy (RRT), including hemodialysis/peritoneal dialysis, for more than 3 months, or undergoing kidney transplantation. Acute kidney injury (AKI) events leading to dialysis and death are also considered end-stage kidney disease (ESKD) events.
- Renal-related death: Meeting both of the following criteria: 1) The patient died during the follow-up period; 2) Despite the need for renal replacement therapy (RRT) due to their condition, it was not received;3)No other clear cause of death.
All-cause deaths includes cardiac death, vascular death and non-cardiovascular death.
- Cardiac death: any death due to proximate cardiac cause (eg, MI, low-output failure, fatal arrhythmia), unwitnessed death and death of unknown cause, and all procedure-related deaths, including those related to concomitant treatment, will be classified as cardiac death.
- Vascular death: caused by noncoronary vascular causes, such as cerebrovascular disease, pulmonary embolism, ruptured aortic aneurysm, dissecting aneurysm, or other vascular diseases.
- Non-cardiovascular death: any death not covered by the above definitions, such as death caused by infection, malignancy, sepsis, pulmonary causes, accident, suicide, or trauma
Collect 4 ml of fasting peripheral venous blood from enrolled patients. Fasting should commence at 22:00 the day before blood collection. The blood should be placed in EDTA anticoagulant tubes.
Within 2 hours after blood collection, plasma should be separated and stored for subsequent lipidomic analysis. This involves centrifuging at 3000 rpm for 10 minutes to separate the plasma. Transfer the upper layer of plasma into 200 ul/1.5 ml EP tubes, then store at -80°C for preservation.
Inclusion Criteria:
- Age 18-80 years old;
- Diagnosed with CHD during hospitalization through coronary angiography, including ST-segment elevation myocardial infarction (STEMI), non-ST-segment elevation acute coronary syndrome (NST-ACS), stable angina pectoris;
- Patients with clarified renal function status.;
CKD is defined as meeting one of the following criteria, with a duration of more than 3 months: eGFR < 60 ml/min/1.73 m² or eGFR ≥ 60 ml/min/1.73 m² and urinary albumin-to-creatinine ratio (uACR) ≥ 30 mg/g;
Exclusion Criteria:
- Pregnancy or lactation;
- Severe valve disease or severe mechanical complications requiring surgical intervention;
- Severe psychiatric illness or other reasons that impede follow-up compliance;
- Severe hematologic disorders or end-stage malignant tumors;
- Having undergone kidney transplantation or long-term maintenance dialysis;
- Severe liver disease (Child-Pugh class C);
- Received acute renal failure dialysis treatment within 12 weeks prior to screening for enrollment;
- Severe chronic lung disease requiring long-term mechanical ventilation support or awaiting lung transplantation;
- Life expectancy less than 1 year.
- For Patients and Families
- For Researchers
- For Study Record Managers
- Customer Support
- Accessibility
- Viewers and Players
- Freedom of Information Act
- HHS Vulnerability Disclosure
- U.S. National Library of Medicine
- U.S. National Institutes of Health
- U.S. Department of Health and Human Services

IMAGES
VIDEO
COMMENTS
Coronary Heart Disease (CHD) it is also know as Coronary Artery Disease. It happens when the blood vessels delivering to the heart develop blockage or are narrowed by plaque, which reduces the flow of the blood, oxygen and nutrients supplied to the heart. If this happens the person starts to feel chest pain (also known as angina pectoris) and ...
Heart disease, including coronary heart disease, remains the leading cause of death in the United States. However, the rate of heart disease deaths has declined by 70% over the past 50 years, thanks in part to NHLBI-funded research. Many current studies funded by the NHLBI focus on discovering genetic associations and finding new ways to ...
To celebrate the 200th anniversary of the New England Journal of Medicine, our essay focuses on the themes of coronary artery ... Factors of risk in the development of coronary heart disease ...
A family history of heart disease makes you more likely to get coronary artery disease. This is especially true if a close relative (parent, sibling) developed heart disease at an early age. The risk is highest if your father or a brother had heart disease before age 55 or if your mother or a sister developed it before age 65. Smoking.
Request an Appointment. 410-955-5000 Maryland. 727-767-8336 Florida. +1-410-502-7683 International. Coronary artery disease (also called coronary heart disease) is the number-one killer of both men and women in the United States, and it's the most common type of heart disease.
Coronary artery disease (CAD) involves impairment of blood flow through the coronary arteries, most commonly by atheromas. Clinical presentations include silent ischemia, angina pectoris, acute coronary syndromes (unstable angina, myocardial infarction), and sudden cardiac death. Diagnosis is by symptoms, ECG, stress testing, and sometimes ...
Introduction. The thesis of this essay is that the longstanding emphasis on cardiovascular disease (CVD) has at last yielded to a mounting force behind cardiovascular health (CVH), manifest in adoption by the American Heart Association (AHA) of its 2020 Impact Goal: "By 2020, to improve the CVH of all Americans by 20% while reducing deaths from CVDs and stroke by 20%." 1 It is proposed ...
Coronary artery disease (CAD) continues to pose a health challenge, impacting numerous individuals and placing strain on healthcare systems worldwide. The narrowing and blockage of arteries due to CAD can lead to complications like heart attacks and heart failure. Over time, dedicated efforts from researchers, professionals, and governments ...
Request an Appointment. 410-955-5000 Maryland. 855-695-4872 Outside of Maryland. +1-410-502-7683 International. Find a Doctor. A person with coronary heart disease has an accumulation of fatty deposits in the coronary arteries. These deposits narrow the arteries and can decrease or block the flow of blood to the heart.
No disease can have been so extensively studied. The work of recent years has yielded remarkable advances in our understanding, and in diagnostic and interventional cardiology, surgery, and pharmacology—effort well spent for a disease that carries such heavy social and economic costs. The clinical condition of coronary heart disease (CHD) presents as (i) angina, (ii) myocardial infarction ...
Figure 1. Stable coronary artery syndromes: different combinations of focal, diffuse, and microvascular coronary artery disease (CAD) contribute to myocardial ischaemia. Extreme forms of focal or diffuse coronary disease may result in discordant abnormalities of either fractional flow reserve (FFR) or coronary flow reserve (CFR), respectively.
Abstract. Ischemic heart disease (IHD) is the greatest single cause of mortality and loss of disability-adjusted life years worldwide, and a substantial portion of this burden falls on low- and middle-income countries (LMICs). Deaths from IHD and acute coronary syndrome (ACS) occur, on average, at younger ages in LMICs than in high-income ...
Coronary artery disease is caused by the gradual buildup of cholesterol or plaque, which makes the arteries stiffen and narrow. The result is reduced blood flow to the heart. Multiple causes of coronary artery disease include: Genetics: Having a family history of heart disease. Lifestyle: Eating unhealthy, high-fat foods and being sedentary.
Coronary Artery Disease. Coronary heart disease is the most common type of heart disease, killing 375,476 people in 2021. 2; About 1 in 20 adults age 20 and older have CAD (about 5%). 2; In 2021, about 2 in 10 deaths from CAD happen in adults less than 65 years old. 1;
High blood pressure is a risk factor for coronary heart disease, myocardial infarction and stroke and is very common in older adults. 3 It is a leading cause of preventable illness and death. 3 Controlling high blood pressure is shown to reduce the risk of fatal myocardial infarctions and strokes. 3. Lowering blood pressure can be done safely ...
Coronary artery disease is a condition in which there is an inadequate supply of blood and oxygen to the myocardium. It results from occlusion of the coronary arteries and results in a demand-supply mismatch of oxygen. It typically involves the formation of plaques in the lumen of coronary arteries that impede blood flow. It is the major cause of death in the US and worldwide. At the beginning ...
Introduction. Thought of broadly, the management of patients with stable coronary artery disease (CAD) involves significant complexity including the diagnosis of CAD, assessment of associated risk, treatment, and monitoring of symptoms during follow up. 1 To provide sufficient focus in this month's topic review in Circulation: Cardiovascular Quality and Outcomes, we have concentrated on the ...
Summary. Coronary artery disease (CAD) develops when plaque builds up in the coronary arteries and they become narrow or blocked. It can lead to a heart attack, but statins and other treatment ...
Ischemic heart disease represents a significant global burden of morbidity and mortality. While revascularization strategies are well defined in acute settings, there are uncertainties regarding chronic coronary artery disease treatment. Recent trials have raised doubts about the necessity of revascularization for "stable", chronic coronary syndromes or disease, leading to a shift towards ...
Heart disease is a major cause of death. In this article, learn about the different types, how to recognize the symptoms, and what treatment to expect. ... Coronary artery disease, also known as ...
These data have come to support what RCT has already shown. Coronary artery bypass grafting has, in fact, been shown to achieve better results than percutaneous coronary intervention (PCI) in the treatment of coronary disease independently from the SYNTAX score and the presence of left main or multivessel disease. 2
Pathophysiology of Coronary Heart Disease: As previously touched upon, Coronary Heart Disease is caused by a build up of fat deposits within the coronary arteries and more than 110,000 people in the UK die each year because of this condition. These fatty deposits or atheroma as they are medically termed are a mixture of cholesterol and other ...
Coronary heart disease (CHD) accounts for over 50% of mortality from heart disease in the USA, responsible for nearly 400 000 deaths in 2020. 1 Despite advances in prevention and treatment over the past decade in the USA, 2 CHD remains the leading cause of death in the USA since 1950 with increasing evidence for non-conventional risk factors ...
Background: Racism is highly prevalent in the United States. Few data exist about whether perceived interpersonal racism is associated with risk of coronary heart disease (CHD). Methods: We followed 48 305 participants in the Black Women's Health Study through biennial mailed and Internet-based health questionnaires from 1997, when they provided information on perceived interpersonal racism ...
The coronary heart disease studies were not restricted during the search by sample size because of the limited number of studies in selected countries. The study reviews the potential risk factors responsible for coronary heart disease globally. ... Duplicate articles and papers with incomplete information, like conference proceedings, were ...
This review focuses on the progress made in applying EECP to CHD cardiac rehabilitation globally, including a brief history of EECP, the working principle, etc, to help researchers grasp the research outline and gaps in the literature regarding EECP. Enhanced external counterpulsation (EECP) is a non-invasive, outpatient, pulsatile-assisted circulation technique that has been used in many ...
Hot line +662 011 3594. 20.00-8.00 (BKK Time) Contact Center +662 066 8888 and 1378. Rating score 0 of 10 , based on 0 vote (s) Heart-Center Heart-Disease. Coronary artery disease (CAD) is a major contributor to chronic heart failure (CHF) and a serious health concern.
Background: Diffuse coronary artery disease (CAD) impacts the safety and efficacy of percutaneous coronary intervention (PCI). Pathophysiological CAD patterns can be quantified using fractional flow reserve (FFR) pullbacks incorporating the pullback pressure gradient (PPG) calculation.
Coronary heart disease (CHD) combined with chronic kidney disease (CKD) affects a substantial portion of the population and carries a significant disease burden, often leading to poor outcomes. Despite efforts to strictly control traditional risk factors, the efficacy in improving outcomes for patients with both CHD and CKD has been limited. ...